Unlock your full potential by mastering the most common Laparoscopic Technology interview questions. This blog offers a deep dive into the critical topics, ensuring you’re not only prepared to answer but to excel. With these insights, you’ll approach your interview with clarity and confidence.
Questions Asked in Laparoscopic Technology Interview
Q 1. Explain the advantages of laparoscopic surgery compared to open surgery.
Laparoscopic surgery, also known as minimally invasive surgery, offers significant advantages over traditional open surgery. The key benefit lies in the smaller incisions. Instead of a large incision, laparoscopy uses several small punctures. This leads to several improvements:
- Reduced pain: Smaller incisions mean less tissue trauma, resulting in significantly less postoperative pain. Patients often require less pain medication and recover faster.
- Smaller scars: The small incisions leave behind much smaller and less noticeable scars compared to the large scars from open surgery.
- Shorter hospital stay: Because of less pain and faster recovery, patients typically spend less time in the hospital after laparoscopic procedures.
- Faster recovery time: Overall recovery is quicker, allowing patients to return to their normal activities sooner.
- Reduced risk of infection: Smaller incisions reduce the risk of infection, a significant complication of open surgery.
- Less blood loss: Precise instrument control minimizes bleeding during the procedure.
For example, a gallbladder removal (cholecystectomy) performed laparoscopically results in a much faster recovery than the same procedure done through open surgery. Patients often go home the same day or the next, whereas open cholecystectomy often requires a longer hospital stay.
Q 2. Describe the different types of laparoscopic instruments and their applications.
A wide array of instruments is used in laparoscopic surgery. These are broadly categorized based on their function:
- Graspers: These instruments help to grasp and manipulate tissues. Examples include Babcock forceps, atraumatic graspers, and Allison forceps. The choice depends on the tissue type and the procedure.
- Scissors: Used for cutting and dissecting tissue. Metzenbaum scissors and Mayo scissors are common examples, adapted for laparoscopic use with smaller, more maneuverable blades.
- Retractors: Hold back tissue to improve visibility of the surgical site. These can be simple, hand-held retractors or more sophisticated self-retaining retractors.
- Suction/Irrigation devices: These remove blood and fluids from the surgical field, maintaining a clear view and preventing excessive fluid accumulation. Often, these are combined into a single instrument.
- Energy devices: These provide energy for tissue dissection and hemostasis (stopping bleeding). These can include monopolar and bipolar electrosurgical devices, ultrasonic shears, and laser devices. The choice depends on the tissue type and the surgeon’s preference.
- Suturing devices: Laparoscopic suturing uses specialized needles and instruments for precise placement of sutures within a confined space. Endoscopic suturing devices, such as linear staplers, are also employed.
The application of each instrument is highly procedure-specific. For instance, during a laparoscopic appendectomy, graspers are used to manipulate the appendix, scissors for dissection, and energy devices for sealing blood vessels. The versatility of these instruments allows for complex procedures to be performed minimally invasively.
Q 3. What are the potential complications of laparoscopic surgery?
While laparoscopic surgery is generally safer than open surgery, potential complications exist. These can include:
- Injury to organs: Accidental damage to nearby organs during trocar insertion or instrument manipulation is a risk, though less frequent than in open surgery.
- Bleeding: While minimized, bleeding can occur, requiring additional measures to control it.
- Infection: Although less common than with open surgery, infection at the incision sites is still possible.
- Gas embolism: Air entering the bloodstream during the procedure is a rare but serious complication.
- Trocar site hernias: A weakness at the incision sites can result in a hernia, though this is less common with proper technique.
- Port site bleeding or hematoma: Bleeding around the insertion site of the trocars may cause swelling or pain.
- Conversion to open surgery: In certain cases, unforeseen complications might necessitate converting the procedure to open surgery.
Proper surgical technique, meticulous attention to detail, and appropriate patient selection significantly reduce these risks. Pre-operative planning and a skilled surgical team are crucial in minimizing these potential complications.
Q 4. How do you manage pneumoperitoneum during a laparoscopic procedure?
Pneumoperitoneum, the creation of artificial gas pressure in the abdominal cavity, is essential for laparoscopic surgery. It allows for better visualization and manipulation of organs. The process involves insufflating gas (usually carbon dioxide) into the abdomen using a Veress needle or an open technique. Careful management is critical:
- Pressure monitoring: Intra-abdominal pressure is constantly monitored using a pressure gauge to maintain optimal pressure levels and avoid excessive distension which could lead to complications.
- Gas flow rate control: The flow rate is adjusted to maintain the desired pressure, avoiding rapid inflation or deflation which can lead to injury.
- Insufflation port placement: Careful selection of the insufflation port site is crucial to avoid injury to organs.
- Gas type and flow: Carbon dioxide is usually the preferred gas due to its rapid absorption, but other gases may be used in specific scenarios. Flow should be monitored to avoid excessive accumulation.
- Post-operative management: Gas is released at the end of the procedure, and any residual gas is absorbed naturally. Post-operative discomfort may be managed with appropriate pain relief strategies.
Careful management of pneumoperitoneum is paramount in ensuring patient safety and procedural success. It’s a dynamic process that demands constant monitoring and adjustment based on the individual patient’s physiology and the surgical procedure.
Q 5. Explain the principles of trocar placement and insertion.
Trocar placement is a critical step in laparoscopic surgery. The goal is to safely introduce the instruments into the abdominal cavity while minimizing the risk of injury to organs. The process generally follows these principles:
- Careful planning: Pre-operative imaging (ultrasound or CT scan) may be used to aid in the selection of optimal trocar sites.
- Safe entry points: Trocar insertion points are chosen to avoid major blood vessels, nerves, and organs. Anatomical landmarks are used for guidance.
- Open versus closed technique: The open technique involves making a small incision, exposing the peritoneum, and then inserting the trocar under direct vision. The closed technique uses a Veress needle to create a pneumoperitoneum before trocar insertion, which is less direct.
- Optimal trocar angle: The angle of trocar insertion must be optimized to minimize the risk of injury to underlying structures.
- Continuous monitoring: Intra-abdominal pressure is constantly monitored during trocar insertion.
- Verification of trocar placement: After trocar insertion, visual inspection may be required to ensure there are no organ injuries.
Careful consideration of these principles ensures that trocar placement is performed safely and efficiently, setting the stage for a successful laparoscopic procedure. An incorrect placement can have serious consequences, making careful planning and skillful execution paramount.
Q 6. Describe your experience with laparoscopic suturing techniques.
Laparoscopic suturing requires specialized techniques and instruments due to the limited space and restricted access. My experience encompasses several approaches:
- Endoloop technique: Using an endoloop device to place a suture around tissue without requiring the threading of a needle. This is particularly useful for ligation of vessels or closing defects.
- Intracorporeal knot-tying: This method involves tying sutures within the abdominal cavity using specialized instruments such as the Roeder knot pusher. It requires significant dexterity and precision.
- Extracorporeal knot-tying: Sutures are passed through tissue intracorporeally, and then tied outside the abdominal cavity. This method is easier to learn than intracorporeal knot-tying.
- Use of absorbable sutures: Preference is often given to absorbable sutures, as these reduce the need for suture removal post-operatively.
- Various suturing patterns: Several patterns, including simple interrupted, continuous, and running sutures, are used based on the specific requirements of the tissue and the surgical procedure.
Proficiency in laparoscopic suturing techniques is essential for safe and efficient minimally invasive surgery. Continuous practice and familiarity with various suturing instruments are key to mastering these techniques. For example, during a laparoscopic cholecystectomy, I often utilize the endoloop technique for cystic duct ligation, minimizing the risk of bleeding and simplifying the procedure.
Q 7. How do you handle unexpected bleeding during a laparoscopic procedure?
Unexpected bleeding during a laparoscopic procedure necessitates a rapid and decisive response. The steps taken depend on the severity and location of the bleeding:
- Identify the source: Careful observation and exploration of the surgical field are essential to identify the bleeding source.
- Control the bleeding: Techniques include applying pressure directly to the bleeding site, using electrosurgery (monopolar or bipolar) for coagulation, or applying clips or sutures to seal blood vessels.
- Suction/Irrigation: Maintaining clear visibility is crucial. Suction is used to clear blood, and irrigation with saline solution helps visualize the area.
- Retraction: If needed, retractors are employed to provide a better view of the bleeding source.
- Consider advanced techniques: If the bleeding is significant or uncontrolled, more advanced techniques such as angiographic embolization may be required.
- Conversion to open surgery: In rare cases, if bleeding is uncontrollable and threatens the patient’s safety, conversion to open surgery might be necessary.
Prompt recognition and efficient management of bleeding are essential to ensure patient safety. A thorough understanding of haemostasis techniques and the ability to quickly adapt to unforeseen circumstances are vital aspects of laparoscopic expertise. I’ve encountered instances of unexpected bleeding during laparoscopic procedures, and the quick identification of the source and implementation of appropriate hemostatic measures has consistently ensured positive outcomes.
Q 8. Explain your knowledge of laparoscopic energy sources (e.g., monopolar, bipolar).
Laparoscopic surgery relies on various energy sources to cut, coagulate, and dissect tissue. The two primary types are monopolar and bipolar electrosurgery.
Monopolar electrosurgery uses a single electrode to deliver high-frequency electrical current to the tissue. The current passes through the tissue to a grounding pad placed on the patient’s skin, completing the circuit. This method is effective for cutting and coagulation but carries a risk of burns or unintended tissue damage if not used carefully. Think of it like a single-wire light switch – the current flows through one path.
Bipolar electrosurgery uses two electrodes, one delivering current and the other returning it. The current flows only between the two electrodes, reducing the risk of burns and improving precision. It’s like using a small, focused lamp instead of a floodlight; it allows for more targeted energy delivery. Bipolar is generally preferred for delicate tissues and where minimizing collateral damage is crucial, such as during surgeries near major blood vessels.
Other energy sources used in laparoscopy include ultrasonic energy (e.g., Harmonic scalpel) which uses high-frequency vibrations to cut and coagulate tissue, and laser energy which offers precise cutting and ablation capabilities, offering distinct advantages for specific surgical situations.
Q 9. How do you use laparoscopic visualization systems effectively?
Effective laparoscopic visualization is paramount for successful surgery. This relies on a high-quality camera system, proper insufflation (filling the abdominal cavity with gas to create space), and skilled camera manipulation. The surgeon must be able to smoothly and precisely maneuver the camera to get optimal views. Poor visualization can lead to errors, increased operative time, and even patient injury.
I use a systematic approach, starting with a thorough initial survey of the surgical field to assess the anatomy and identify landmarks. During the procedure, I constantly adjust the camera angle and zoom level to maintain optimal visualization of the operative area. I also use various laparoscopic instruments, such as retractors, to improve visibility as needed. This often involves coordination with surgical assistants to optimize the field.
Understanding the limitations of the system is also important. For instance, it’s impossible to ‘feel’ the tissue in the same way as in open surgery, so we rely heavily on visualization to guide our actions and avoid injuries to adjacent structures. I’ve found that consistent practice and a keen awareness of the camera’s capabilities are crucial to develop proficiency and safety.
Q 10. Describe your experience with different laparoscopic surgical approaches (e.g., transabdominal, transvaginal).
My experience encompasses a wide range of laparoscopic approaches. Transabdominal approaches are the most common and involve accessing the abdominal cavity through small incisions in the abdomen. This allows for a broad range of procedures, from appendectomy to complex colorectal resections. The approach can be tailored based on the specific procedure and the surgeon’s preference (e.g., single-port or multi-port techniques).
Transvaginal approaches are used for procedures involving the pelvic organs, particularly in gynecological surgery. This approach minimizes abdominal scarring and offers advantages in specific situations. However, it has limitations in terms of access and visualization compared to a transabdominal approach. The choice between approaches depends critically on factors including the surgical indication, patient anatomy, and the surgeon’s expertise.
I’m proficient in various approaches including the use of natural orifices for surgery (NOTES) and single-incision laparoscopic surgery (SILS), which aim to minimize surgical trauma and improve cosmetic outcomes. Choosing the optimal approach requires careful pre-operative planning and assessment of the individual patient’s characteristics.
Q 11. What is your experience with robotic-assisted laparoscopic surgery?
I have extensive experience with robotic-assisted laparoscopic surgery (RALS). RALS combines the minimally invasive benefits of laparoscopy with the enhanced dexterity and precision offered by robotic surgical systems (e.g., da Vinci Surgical System). The system provides a magnified, high-definition 3D view, allowing for more precise dissection and manipulation of tissues. The robotic arms offer greater range of motion than the human hand, facilitating complex procedures.
In my experience, robotic surgery is particularly advantageous in procedures requiring intricate movements and high precision, such as complex urological or gynecological procedures. The improved visualization and dexterity lead to reduced trauma, shorter hospital stays, and better patient outcomes in many cases. However, it’s important to acknowledge the higher cost and longer setup times associated with robotic surgery. The learning curve for robotic surgery is steeper, requiring dedicated training and practice.
Q 12. How do you ensure patient safety during laparoscopic procedures?
Patient safety is my utmost priority. I follow a multi-layered approach to ensure safety throughout the laparoscopic procedure. This begins with thorough pre-operative evaluation, including a complete medical history, physical examination, and appropriate blood work. I carefully explain the risks and benefits of the procedure to the patient and obtain informed consent.
During the procedure, continuous monitoring of vital signs (heart rate, blood pressure, oxygen saturation) is crucial. Maintaining proper pneumoperitoneum (the gas pressure in the abdominal cavity) is essential to prevent complications such as hypercarbia or gas embolism. Careful dissection techniques and meticulous hemostasis (control of bleeding) are essential to minimize the risk of injury to blood vessels or other organs.
The use of appropriate energy sources and meticulous attention to detail significantly reduce the chance of complications such as burns or perforations. A well-coordinated surgical team, including experienced nurses and assistants, plays a key role in patient safety. Post-operative monitoring and timely intervention are also crucial to identify and address any potential complications.
Q 13. Describe the process of setting up a laparoscopic surgical field.
Setting up a laparoscopic surgical field requires meticulous attention to detail and adherence to strict sterile protocols. The process begins with ensuring the operating room is appropriately prepared, including the availability of all necessary equipment and instruments. The surgeon and surgical team scrub their hands and arms and don sterile gowns and gloves. The patient is positioned and prepped with an antiseptic solution.
Next, the laparoscopic ports are placed. The number and location of the ports vary depending on the procedure. These locations are chosen carefully to provide optimal access and visibility while minimizing the risk of injury to major organs. Each port site is meticulously disinfected and draped to maintain a sterile field.
The laparoscope is then introduced into the abdominal cavity. The pneumoperitoneum is established using a Veress needle or open technique, allowing the surgeon to inflate the abdomen with carbon dioxide to create working space. Once the pneumoperitoneum is established, the other instruments are introduced through the remaining ports.
Throughout the setup, sterility is paramount. Any breach of sterile technique must be immediately addressed. Consistent adherence to these procedures is crucial for minimizing the risk of surgical site infections and other complications.
Q 14. Explain the importance of proper sterilization and disinfection in laparoscopic surgery.
Proper sterilization and disinfection are critical in laparoscopic surgery to prevent surgical site infections (SSIs), a serious complication that can lead to prolonged hospital stays, increased morbidity, and even mortality. The risk of SSIs is higher in laparoscopic procedures due to the creation of multiple small incisions.
Sterilization refers to the complete elimination of all microorganisms from an object. This is usually achieved through autoclaving (high-pressure steam sterilization) or ethylene oxide gas sterilization for instruments that cannot withstand high heat. Disinfection involves reducing the number of microorganisms to a safe level, often achieved using chemical disinfectants.
All instruments, laparoscopic ports, and other equipment used in laparoscopic surgery must be properly sterilized before each procedure. Surgeons and surgical staff must maintain strict sterile technique throughout the operation to prevent contamination. Post-operative care, including proper wound care, contributes to minimizing SSI risk. Adherence to these rigorous processes significantly reduces the risk of infections and improves patient safety.
Q 15. How do you troubleshoot common technical issues during a laparoscopic procedure?
Troubleshooting technical issues during a laparoscopic procedure requires a systematic approach. It’s crucial to remember patient safety is paramount. My process typically involves:
- Identify the problem: Is the camera blurry? Are the instruments malfunctioning? Is there insufflation failure? Precisely defining the issue is the first step.
- Check the basics: This often involves verifying connections, power sources, and gas flow. A simple loose connection can cause significant problems. For example, a sudden drop in insufflation pressure might be due to a leak in the pneumoperitoneum system – I’d systematically check all connections and the trocar sites.
- Systematic troubleshooting: If the problem persists, I’d move to a more detailed investigation. This might involve checking the camera’s cable, the light source, or the instrument’s articulation mechanisms. Sometimes, it’s a simple matter of repositioning the camera or adjusting the light intensity.
- Seek assistance: If the problem is beyond my immediate expertise or if it poses a risk to the patient, I will not hesitate to call for help from the surgical team, the anesthesia team, or biomedical engineering.
- Document everything: Meticulous documentation of the problem, the troubleshooting steps, and the resolution (or lack thereof) is essential for quality assurance, learning, and potential future investigations.
For example, I once experienced a sudden loss of camera image during a cholecystectomy. After checking the basic connections, I discovered a problem with the camera head itself, requiring a quick switch to a backup camera. The procedure was delayed minimally thanks to a systematic approach and our well-rehearsed protocols.
Career Expert Tips:
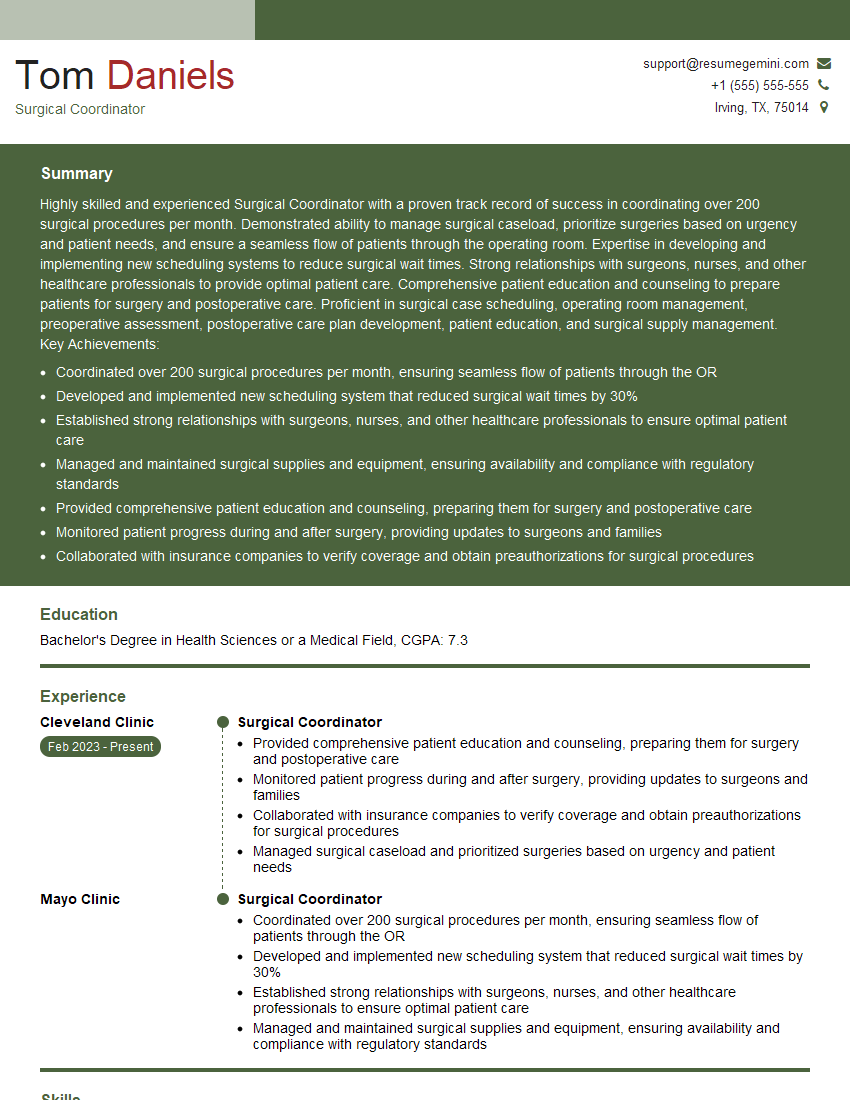
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Describe your experience with various laparoscopic cameras and their features.
I have extensive experience with various laparoscopic cameras, ranging from older 2D systems to the latest 3D and 4K high-definition cameras. Key features I consider include:
- Image quality: Resolution, clarity, and color reproduction are critical for accurate visualization of anatomical structures. 4K cameras offer significantly improved detail compared to older systems.
- Camera control: The ease of manipulating the camera— its articulation, zoom, and focus – directly impacts the efficiency and precision of the surgery. Ergonomic camera controls are essential to minimize operator fatigue.
- Lighting: Adequate illumination is crucial. Modern cameras often offer adjustable light intensity and different light settings to optimize visualization in different surgical fields.
- Integration with other systems: Seamless integration with other components of the laparoscopic system, including the monitor and recording devices, is important for smooth workflow.
- Sterilization capabilities: The camera and its components must be compatible with appropriate sterilization methods, ensuring a safe and sterile surgical environment.
For instance, I’ve found that 3D cameras significantly improve depth perception, particularly during complex procedures like colorectal surgery. The enhanced visualization translates directly into greater precision and reduced complications.
Q 17. How do you manage patient positioning during laparoscopic surgery?
Patient positioning during laparoscopic surgery is critical for optimal surgical access, minimizing complications, and ensuring patient safety. It involves a collaborative effort between the surgical team, the anesthesia team, and the operating room nurses.
Factors influencing positioning include:
- Surgical approach: The specific surgical technique and the location of the operative site determine the optimal position. For example, a cholecystectomy might require a supine position with the patient’s right shoulder elevated, whereas a splenectomy may involve a left lateral decubitus position.
- Patient factors: The patient’s age, body habitus, and any pre-existing conditions must be considered. Patients with respiratory or cardiovascular compromise might require special attention to their positioning.
- Equipment considerations: The operating table and the specialized positioning aids must be adjusted appropriately to provide adequate access for the surgeon and to prevent pressure injuries.
- Preventing injury: Proper padding, positioning aids, and continuous monitoring are crucial to prevent nerve palsies, pressure sores, and other positioning-related complications.
Before initiating any procedure, a thorough assessment of the patient is performed, and the optimal position is meticulously planned and executed. Continuous monitoring and adjustments throughout the procedure are vital for patient comfort and safety.
Q 18. What is your understanding of the limitations of laparoscopic surgery?
Laparoscopic surgery, while offering many advantages, has certain limitations:
- Limited tactile feedback: The lack of direct tactile sensation compared to open surgery can make it challenging to assess tissue characteristics and perform delicate maneuvers. This is overcome to some extent by specialized instruments, but remains a limitation.
- Steeper learning curve: Mastering laparoscopic techniques requires extensive training and practice, significantly steeper than open surgery techniques for many procedures.
- Two-dimensional view: Traditional laparoscopy uses a two-dimensional image, potentially distorting the three-dimensional anatomy. 3D cameras mitigate this but don’t completely eliminate it.
- Inability to deal with extensive adhesions: Severe adhesions can make laparoscopic access challenging or impossible, necessitating conversion to open surgery.
- Potential for complications: Though relatively infrequent, complications such as trocar site hernias, bleeding, and visceral injury can occur.
- Suitability of patient: Not all patients are suitable candidates for laparoscopic surgery; obese patients or those with severe co-morbidities may present challenges.
Understanding these limitations is crucial for making informed decisions about the surgical approach and ensuring patient safety. These limitations are frequently weighed against the advantages of laparoscopy, such as reduced pain, smaller incisions and faster recovery times, to reach the best possible outcome for each patient.
Q 19. Explain the role of the surgical team in laparoscopic procedures.
The surgical team in laparoscopic procedures is a highly coordinated group, each member playing a vital role:
- Surgeon: Leads the procedure, manipulates instruments, and makes critical decisions.
- First Assistant: Assists the surgeon with instrument handling, retraction, and other tasks, significantly improving efficiency.
- Second Assistant (often scrub nurse): Responsible for maintaining instrument sterility, managing supplies, and assisting with other needs.
- Anesthesiologist: Monitors and manages the patient’s vital signs, maintains anesthesia, and addresses any complications related to anesthesia.
- Circulating Nurse: Manages the overall operating room environment, ensures the sterility of supplies, assists with patient positioning, and manages patient records.
Effective teamwork, communication, and clear roles are critical for successful laparoscopic procedures. The surgical team operates as a single unit, each member relying on and supporting the others. Any breakdown in communication or teamwork can lead to inefficiencies and potentially compromise patient safety.
Q 20. How do you communicate effectively with the surgical team during a laparoscopic case?
Effective communication is paramount during laparoscopic procedures. I utilize a combination of strategies:
- Clear and concise language: I use precise terms to describe the surgical field, instrument movements, and any observed complications. Avoiding jargon whenever possible ensures everyone understands.
- Regular updates: I provide regular updates to the surgical team, especially about critical steps, changes in the surgical plan, or any unexpected findings. This keeps everyone informed and prepared for potential adjustments.
- Non-verbal communication: Effective non-verbal communication, including gestures and facial expressions, plays a significant role in coordinating movements and conveying information quickly.
- Active listening: I actively listen to the contributions of team members, encouraging feedback and discussion. This fosters collaboration and helps to identify potential problems early.
- Designated roles and responsibilities: Establishing clear roles and responsibilities for each team member minimizes confusion and ensures everyone knows their part. This reduces redundancy and ensures efficient workflow.
For example, I always confirm instrument placement and actions with the first assistant, verbally or through hand signals, before undertaking critical steps. This shared awareness prevents errors and safeguards patient safety.
Q 21. Describe your experience with laparoscopic retrieval of specimens.
Retrieving specimens during laparoscopic surgery involves specialized techniques to ensure the specimen’s integrity and avoid complications:
- Specimen bag placement: A sterile specimen bag is introduced into the abdominal cavity early in the procedure. This facilitates easy retrieval.
- Endobag technique: An endobag— a specialized retrieval bag—is used to contain the specimen within the abdominal cavity before retrieval. This minimizes spillage and contamination.
- Endoscopic retrieval devices: Specialized retrieval devices, such as grasping forceps or retrieval nets, are used to carefully extract the specimen from the body.
- Closing the port site: Once the specimen is retrieved, the port site is meticulously closed with sutures or clips, preventing bleeding and hernia formation.
- Specimen labeling and handling: The retrieved specimen is carefully labeled, documented, and handed over to the pathology department, ensuring appropriate handling and analysis.
I’ve found that meticulous attention to detail during specimen retrieval is critical for accurate pathological diagnosis and helps to avoid complications like seeding of tumor cells or infections. For instance, in a laparoscopic appendectomy, it’s crucial to ensure the entire appendix, including the appendiceal base, is within the retrieval bag to avoid leaving behind any tissue which might lead to complications. The proper handling and labelling are vital for clear communication with the pathology department.
Q 22. What is your familiarity with different types of laparoscopic ports?
Laparoscopic ports are essential for minimally invasive surgery. They’re essentially small incisions through which specialized instruments and a camera are inserted into the abdominal cavity. Different types cater to various surgical needs and anatomical considerations.
- Pneumatic Ports: These are the most common, using a blunt trocar to create the port. The gas insufflation helps expand the abdominal cavity for better visualization.
- Hassons Ports: These use an open technique where a small incision is made and the trocar is then inserted under direct vision, minimizing the risk of visceral injury, particularly in areas with dense vascularity. This is often favored in situations where there’s a higher risk of bowel or vascular damage.
- Veress Needles: These are used for initial insufflation of the abdomen before port placement. They are crucial for creating pneumoperitoneum. They are extremely important because they can cause significant injury if placed incorrectly. Proper placement is extremely important in preventing injury to bowel or major vasculature.
- Specialized Ports: These include ports with valves to control gas flow, ports with built-in irrigation systems, and ports designed for specific instruments like robotic surgery. For example, robotic surgery often uses specialized ports that allow for articulation of the robotic arms.
Choosing the right port depends on factors like the surgical procedure, patient anatomy, and surgeon preference. For example, a Hasson trocar is often preferred for the initial port placement in cases of obese patients, as direct visualization decreases the likelihood of damage to the abdominal wall.
Q 23. How do you handle challenging anatomical variations during laparoscopic surgery?
Challenging anatomical variations are a common occurrence in laparoscopic surgery. Successful navigation requires a blend of advanced surgical skills, pre-operative planning, and adaptability.
My approach involves a multi-step process:
- Pre-operative Imaging: Thorough review of CT scans, MRIs, or ultrasounds helps identify potential anatomical variations such as adhesions, anatomical distortions (eg. due to previous surgeries or tumors), or unusual vascular arrangements. This allows me to plan the port placement strategy and anticipate potential difficulties.
- Careful Port Placement: Strategic placement of ports, avoiding areas of known vascularity and potential adhesion formations, is critical. This may involve using alternative port placement positions or techniques as compared to a standard technique. We often use open techniques (Hasson) to minimize risks in challenging scenarios.
- Intraoperative Flexibility: I remain flexible during the procedure, adapting my approach as needed. If unexpected adhesions are encountered, I might use instruments to gently dissect them or switch to different instruments better suited to the specific anatomical challenge.
- Advanced Techniques: Sometimes, advanced techniques like laparoscopic ultrasound or indocyanine green (ICG) fluorescence imaging are beneficial. ICG fluorescence imaging can help to delineate vascular anatomy and reduce the risk of injury during dissection.
- Collaboration and Consultation: When dealing with complex cases with significant anatomical variations, consulting with senior surgeons or specialists is crucial. Sometimes, it is also safer to convert to an open procedure to avoid complications.
For example, in a patient with significant prior abdominal surgeries leading to dense adhesions, a careful, step-wise dissection with meticulous attention to vascular structures is required. The Hasson technique is often favored for initial port placement in these cases. Open dissection, while longer, is safer than blindly entering the abdomen with the risk of causing a major injury to a visceral structure.
Q 24. Explain your understanding of post-operative care for laparoscopic surgery patients.
Post-operative care for laparoscopic surgery patients is crucial for a successful outcome and minimizing complications. It focuses on managing pain, preventing infections, and monitoring for potential complications.
- Pain Management: Appropriate analgesia is administered, often involving a multimodal approach that combines various medications to target different pain mechanisms. Patients are taught effective pain management strategies and encouraged to mobilize early on.
- Infection Control: Regular monitoring of the surgical sites and prompt treatment of any signs of infection are vital. Prophylactic antibiotics are often administered, and wound care instructions are given to patients.
- Wound Care: Careful attention is paid to proper wound care and assessing for signs of infection or leakage.
- Bowel Function Monitoring: Post-operative ileus (delayed bowel function) is a common complication. We carefully monitor bowel sounds and manage any issues accordingly using methods like bowel rest or encouraging dietary modification.
- Early Mobilization: Encouraging early mobilization aids in respiratory function and reduces the risk of thromboembolic events, such as deep vein thrombosis (DVT).
- Discharge Planning: A comprehensive discharge plan ensures that patients are provided with all the necessary instructions for wound care, medication management, and follow-up appointments.
For instance, if a patient develops a fever post-operatively, prompt evaluation is crucial to exclude an infection and initiate timely treatment. Similarly, monitoring bowel function and addressing early signs of ileus, such as abdominal distension, can prevent complications like bowel obstruction.
Q 25. What is your approach to preventing surgical site infections in laparoscopic surgery?
Preventing surgical site infections (SSIs) is a top priority in laparoscopic surgery. My approach is multi-faceted and involves strict adherence to established protocols and best practices:
- Pre-operative Patient Preparation: Pre-operative skin preparation is meticulously performed, adhering to recommended guidelines. This often involves showering with an antiseptic solution and then applying chlorhexidine gluconate to the surgical site.
- Sterile Technique in the Operating Room: Maintaining a strictly sterile environment in the operating room is paramount. This includes meticulous surgical hand hygiene and appropriate gowning and gloving protocols.
- Appropriate Antibiotic Prophylaxis: Judicious use of prophylactic antibiotics is critical, ensuring appropriate timing and choice of antibiotic based on the surgical procedure and patient factors.
- Minimizing Operation Time: Shorter operation times reduce the risk of infection. Careful surgical planning and efficient techniques are vital.
- Maintaining Normothermia: Maintaining appropriate patient temperature can help boost the immune response and reduce infection risk.
- Post-Operative Wound Care: Meticulous post-operative wound care follows established best practices. Patients are educated on proper wound care to avoid any potential contamination.
For example, in high-risk patients, such as those with diabetes, we may implement additional measures, such as using a specialized adhesive surgical dressing, to minimize SSI risk.
Q 26. How do you stay current with the latest advancements in laparoscopic technology?
Staying current with advancements in laparoscopic technology is essential for providing optimal patient care. I utilize several strategies:
- Continuing Medical Education (CME): I actively participate in CME activities, including attending conferences, workshops, and webinars focused on laparoscopic surgery and related fields.
- Professional Societies: Membership in professional surgical societies provides access to the latest research, guidelines, and opportunities for networking with peers and experts.
- Peer-Reviewed Journals: Regularly reading peer-reviewed journals keeps me updated on the latest research findings and technological advancements.
- Online Resources: Reputable online resources provide access to a vast amount of information on the subject.
- Collaboration with Colleagues: Regularly discussing cases and sharing experiences with colleagues, both within and outside my own institution, can help expand my knowledge base and introduce new approaches.
For instance, I regularly attend the annual meetings of the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) and follow journals such as the Journal of the American College of Surgeons (JACS).
Q 27. Describe your experience working with different laparoscopic platforms (e.g., da Vinci, etc.).
I have significant experience working with various laparoscopic platforms, including the da Vinci Surgical System and other advanced laparoscopic instruments. Each platform has its own strengths and weaknesses.
My experience with the da Vinci system includes performing complex procedures with its robotic capabilities. The enhanced dexterity and precision offered by the da Vinci system are invaluable in intricate surgical settings. For example, the da Vinci’s wristed instruments allow for greater maneuverability in confined spaces, facilitating minimally invasive procedures that might otherwise be more challenging with traditional laparoscopy. However, it is important to acknowledge the limitations that the da Vinci system presents as well including cost and the learning curve associated with its operation.
My experience with conventional laparoscopic platforms has provided me with proficiency in a wide range of procedures. I’m adept at using various laparoscopic instruments and maintaining precision and control, ensuring optimal outcomes for the patient. I find that the combination of experience with both robotic surgery and conventional techniques allows me to make informed decisions on whether to use robotic or conventional techniques for any particular surgical scenario.
Q 28. Explain your understanding of the ethical considerations related to laparoscopic surgery.
Ethical considerations are paramount in laparoscopic surgery. They guide my practice in several crucial ways:
- Informed Consent: Patients must be fully informed about the procedure, including potential benefits, risks, and alternatives. This includes discussion of potential complications such as bleeding, infection, and the possibility of needing to convert to an open procedure.
- Patient Autonomy: Respecting the patient’s autonomy and preferences is paramount. The patient’s decisions should always be central to the decision-making process.
- Beneficence and Non-maleficence: The principle of beneficence requires that I act in the patient’s best interest, aiming for the best possible outcome. Non-maleficence involves minimizing the potential harm or risk to the patient.
- Justice and Equity: Ensuring equitable access to laparoscopic surgery, regardless of socio-economic status or other factors, is crucial.
- Continuous Learning: Maintaining competency and remaining updated on best practices is essential in ensuring high-quality care. Continuing education on new advancements and techniques helps to remain up-to-date on surgical safety and best practices.
For instance, in cases where there’s uncertainty about the best course of action, I fully discuss all possible treatment options with the patient and their family. If the decision is in favor of open surgery after initially planning for a laparoscopic procedure, it is communicated transparently and the patient and their family are fully involved in the decision-making process.
Key Topics to Learn for Your Laparoscopic Technology Interview
- Instrumentation and Equipment: Understanding the various instruments, cameras, and ancillary devices used in laparoscopic procedures. This includes their functionality, limitations, and maintenance.
- Surgical Techniques: Mastering the core principles of minimally invasive surgery, including trocar placement, tissue dissection, suturing, and energy sources. Consider different surgical approaches and their applications.
- Imaging and Visualization: A thorough grasp of laparoscopic imaging systems, image interpretation, and troubleshooting potential visualization issues during procedures.
- Safety and Complications: Familiarize yourself with potential complications, risk mitigation strategies, and emergency management protocols in laparoscopic surgery. Understanding safety protocols is crucial.
- Surgical Planning and Case Selection: Knowledge of patient assessment, procedure planning, and appropriate selection of patients for laparoscopic procedures. Discuss the advantages and limitations compared to open surgery.
- Advanced Laparoscopic Techniques: Explore specialized procedures such as robotic-assisted laparoscopy or single-incision laparoscopic surgery (SILS). Highlighting knowledge of emerging technologies shows initiative.
- Troubleshooting and Problem-Solving: Prepare to discuss how you would approach common challenges encountered during laparoscopic procedures, such as bleeding, instrument malfunction, or unexpected anatomical variations.
Next Steps: Elevate Your Career with Laparoscopic Technology Expertise
Mastering laparoscopic technology opens doors to exciting career opportunities and positions you at the forefront of minimally invasive surgical advancements. To maximize your job prospects, it’s crucial to present your skills effectively. Creating an ATS-friendly resume is essential for getting your application noticed by recruiters and hiring managers. This is where ResumeGemini can help. ResumeGemini provides a trusted platform for building professional resumes, ensuring your qualifications shine through. We offer examples of resumes tailored specifically to the Laparoscopic Technology field to guide you in creating a compelling application that showcases your unique skills and experience. Take the next step toward your dream career—build your resume with ResumeGemini today!
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
To the interviewgemini.com Webmaster.
Very helpful and content specific questions to help prepare me for my interview!
Thank you
To the interviewgemini.com Webmaster.
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.