Every successful interview starts with knowing what to expect. In this blog, we’ll take you through the top Critical Care and Ventilator Management interview questions, breaking them down with expert tips to help you deliver impactful answers. Step into your next interview fully prepared and ready to succeed.
Questions Asked in Critical Care and Ventilator Management Interview
Q 1. Describe the process of weaning a patient from mechanical ventilation.
Weaning from mechanical ventilation is a gradual process of transitioning a patient from ventilator support to spontaneous breathing. It’s a crucial step in critical care, requiring careful monitoring and individualized assessment. The goal is to safely remove the ventilator while ensuring adequate oxygenation and ventilation. Weaning is not a single event, but rather a dynamic process that may involve periods of progress and setbacks.
The process typically involves:
- Assessment of readiness: This includes evaluating respiratory parameters like respiratory rate, tidal volume, vital capacity, rapid shallow breathing index (RSBI), and oxygen saturation. We also assess the patient’s overall clinical status, including hemodynamic stability, level of consciousness, and presence of any underlying conditions that could impede weaning.
- Trial of spontaneous breathing: A common approach is to initiate spontaneous breathing trials (SBTs). This involves temporarily disconnecting the patient from the ventilator for a set period (typically 30-120 minutes), observing for signs of respiratory distress or hypoxemia. During SBTs, we closely monitor oxygen saturation, respiratory rate, heart rate, and work of breathing.
- Gradual reduction of ventilator support: If the SBT is successful, we gradually decrease the ventilator’s support, such as reducing the ventilator rate, increasing the pressure support, or switching to a less invasive mode, such as pressure support ventilation or synchronized intermittent mandatory ventilation (SIMV).
- Close monitoring: Throughout the weaning process, continuous monitoring of vital signs, arterial blood gases, and respiratory mechanics is essential to detect early signs of respiratory failure and adjust the weaning strategy as needed.
- Extubation: Once the patient demonstrates sustained spontaneous breathing and adequate oxygenation and ventilation, extubation can be considered. Post-extubation monitoring is crucial to prevent re-intubation.
For example, a patient recovering from pneumonia might start with several hours of SBTs with gradual decreases in ventilator support. If they tolerate this, then extubation would be considered. Conversely, a patient with severe ARDS may require a much slower and more cautious approach with prolonged periods of ventilator support and possibly utilizing different ventilator modes to support their breathing.
Q 2. What are the indications for initiating mechanical ventilation?
The decision to initiate mechanical ventilation is based on the patient’s inability to maintain adequate gas exchange (oxygenation and ventilation) and/or protect their airway. Indications are categorized into respiratory and non-respiratory reasons.
- Respiratory Failure: This is the primary indication, where the patient cannot maintain adequate oxygenation (hypoxemia, low PaO2) and/or ventilation (hypercapnia, high PaCO2). This can be caused by various conditions such as pneumonia, acute respiratory distress syndrome (ARDS), pulmonary edema, or neuromuscular weakness.
- Acute Respiratory Distress: This involves symptoms like increased work of breathing, severe dyspnea, and impending respiratory failure.
- Airway Protection: Mechanical ventilation is also indicated when a patient cannot protect their airway, such as in cases of altered mental status (e.g., coma, severe sepsis) or loss of airway reflexes. This is to prevent aspiration pneumonia.
- Respiratory Muscle Fatigue: In situations where respiratory muscles are too weak to support adequate breathing, mechanical ventilation assists in reducing the work of breathing. Examples include severe neuromuscular diseases (e.g., Guillain-Barré syndrome) or severe sepsis.
- Non-Respiratory Reasons: Although less common, other circumstances may necessitate mechanical ventilation, such as providing ventilatory support during major surgery (e.g., cardiac surgery) or severe traumatic brain injury management. These scenarios often aim at improving perfusion and oxygen delivery while allowing the patient’s body to focus on healing.
For instance, a patient presenting with severe pneumonia and hypoxemia despite supplemental oxygen would be a clear indication for initiating mechanical ventilation. Similarly, a patient in a coma after a head injury would require mechanical ventilation to maintain airway patency and ventilation. The decision requires a careful clinical assessment integrating multiple factors.
Q 3. Explain the difference between volume-controlled and pressure-controlled ventilation.
Both volume-controlled ventilation (VCV) and pressure-controlled ventilation (PCV) are modes of mechanical ventilation, but they differ in how they deliver breaths. Imagine inflating a balloon: VCV is like setting a target volume and the machine will deliver that volume, adjusting the pressure as needed. PCV is like setting a target pressure, and the machine delivers a breath until that pressure is reached, so the delivered volume varies.
- Volume-Controlled Ventilation (VCV): In VCV, the ventilator delivers a set tidal volume (the amount of air delivered with each breath) at a set respiratory rate. The ventilator adjusts the pressure needed to deliver that tidal volume. This is often preferred for patients who need precise control of tidal volume, such as those with acute lung injury where over-distension should be avoided.
- Pressure-Controlled Ventilation (PCV): In PCV, the ventilator delivers a breath to a set pressure for a pre-determined time. The volume delivered varies depending on the patient’s lung compliance (how easily the lungs expand). This mode is useful for patients with very stiff lungs (low compliance), as it helps avoid excessive pressures and potential lung injury. It also allows for more spontaneous breathing effort by the patient.
For example, in a patient with ARDS, PCV might be preferred to prevent over-distension of already injured lungs. In contrast, a patient with a normal respiratory system might tolerate VCV well, allowing for precise control of ventilation.
Q 4. How do you manage ventilator-associated pneumonia (VAP)?
Ventilator-associated pneumonia (VAP) is a serious complication of mechanical ventilation, characterized by a new onset pneumonia occurring more than 48 hours after endotracheal intubation. Prevention and early detection are critical to improve outcomes.
Management of VAP involves a multi-faceted approach:
- Prevention: The cornerstone of VAP management lies in robust preventive measures. This includes meticulous hand hygiene by healthcare providers, elevation of the head of the bed (HOB) to at least 30 degrees, daily sedation vacations, and early mobilization of the patient. Additionally, selective decontamination of the digestive tract and meticulous oral care are beneficial.
- Early detection: Close monitoring for signs and symptoms of pneumonia, including fever, increased white blood cell count, purulent secretions, and new or worsening infiltrates on chest X-ray, are vital. Early detection is crucial for initiating prompt treatment.
- Treatment: Treatment usually involves broad-spectrum antibiotics guided by cultures of respiratory secretions. The choice of antibiotics depends on the local microbiology data and the patient’s clinical condition. The duration of antibiotic treatment is typically 7-10 days, adjusted based on clinical response and cultures.
- Supportive Care: Supportive care is equally important and may involve oxygen therapy, airway clearance techniques (e.g., chest physiotherapy), and nutritional support. Management of any underlying conditions contributing to VAP should also be addressed.
For example, a patient developing a fever and a new infiltrate on chest X-ray two days after starting mechanical ventilation would necessitate a prompt evaluation for VAP and potentially empiric antibiotic therapy. Prevention strategies are essential to reduce the incidence of VAP within our critical care setting.
Q 5. What are the common complications of mechanical ventilation?
Mechanical ventilation, while life-saving, carries a risk of several complications. These can be broadly classified into respiratory and non-respiratory complications.
- Respiratory Complications: These are the most common and include VAP (as discussed above), barotrauma (lung injury due to high airway pressures), volutrauma (lung injury due to excessive tidal volumes), atelectasis (collapse of lung tissue), and oxygen toxicity. Pneumothorax (collapsed lung) and acute respiratory distress syndrome (ARDS) can also be worsened by mechanical ventilation.
- Cardiovascular Complications: Mechanical ventilation can impact cardiovascular function. Positive pressure ventilation can reduce venous return to the heart, leading to decreased cardiac output. Furthermore, it can lead to hemodynamic instability in patients already at risk.
- Gastrointestinal Complications: Stress ulcers, gastrointestinal bleeding, and ileus (bowel obstruction) are more common in mechanically ventilated patients. This is often related to the effects of sedation, immobility, and decreased blood flow to the gut.
- Neurological Complications: Patients on prolonged mechanical ventilation may experience delirium, cognitive dysfunction, and peripheral nerve injury. These complications are often multifactorial and may be influenced by the severity of the underlying illness and the duration of ventilation.
- Infection: In addition to VAP, other infections, such as bloodstream infections and urinary tract infections, are more frequent in patients requiring mechanical ventilation, partly due to the prolonged use of catheters and other invasive devices.
For instance, closely monitoring for signs of barotrauma such as worsening hypoxia or pneumothorax is crucial during high-pressure ventilation. Prophylactic measures, like stress ulcer prophylaxis, are utilized to minimize the risk of gastrointestinal complications.
Q 6. Describe your experience with different ventilator modes (e.g., SIMV, PCV, HFOV).
My experience encompasses a wide range of ventilator modes, each tailored to specific patient needs. Here’s a brief overview:
- Synchronized Intermittent Mandatory Ventilation (SIMV): This mode allows the patient to breathe spontaneously between ventilator breaths. It provides a set number of mandatory breaths at a set rate and volume, complemented by the patient’s spontaneous breaths. I find SIMV very useful during weaning, as it allows for gradual transfer of the work of breathing to the patient.
- Pressure-Controlled Ventilation (PCV): As previously mentioned, PCV delivers breaths to a set pressure. This is particularly useful for patients with very stiff lungs, preventing excessive pressures and potential lung injury. I often use PCV for patients with ARDS or other conditions where lung compliance is compromised.
- High-Frequency Oscillatory Ventilation (HFOV): HFOV delivers very small tidal volumes at high frequencies (often above 60 breaths per minute). This technique is employed primarily for patients with severe ARDS who are refractory to conventional ventilation strategies. HFOV can improve oxygenation and reduce lung injury in these severely ill patients. I have experience managing patients on HFOV, ensuring close monitoring of hemodynamics and lung mechanics.
I always choose a ventilator mode based on the individual patient’s clinical picture and respiratory mechanics. Each mode has strengths and weaknesses, and the appropriate selection is critical to optimizing patient outcomes.
Q 7. How do you assess the readiness of a patient for extubation?
Assessing readiness for extubation is a critical decision requiring careful evaluation of multiple parameters. We aim to minimize the risk of re-intubation, as it is associated with increased morbidity and mortality. A thorough assessment typically includes the following criteria:
- Respiratory System: This is the most important aspect. We assess parameters like respiratory rate (generally under 30 breaths per minute), tidal volume (adequate spontaneous breathing), vital capacity (typically >10-15 ml/kg), and rapid shallow breathing index (RSBI, generally <106 breaths/minute/liter). Oxygenation must be satisfactory with minimal or no supplemental oxygen required.
- Hemodynamic Stability: The patient’s cardiovascular system must be stable. Hypotension or significant arrhythmias can compromise spontaneous breathing after extubation.
- Neurological Status: An adequate level of consciousness is crucial for airway protection and effective cough. Patients should be alert and able to follow simple commands.
- Airway Secretion Clearance: Adequate cough strength is essential to clear secretions after extubation. Excessive secretions might indicate the need for further treatment before extubation.
- Other Factors: We consider factors such as underlying medical conditions, the patient’s overall clinical status, and the potential for future respiratory support needs. For example, a patient with a pre-existing neuromuscular disease might require a more prolonged weaning process.
Successfully extubating a patient requires a holistic approach. If the patient meets most of the above criteria, a spontaneous breathing trial (SBT) can be performed. If the SBT is successful, extubation is the next step. This patient specific evaluation is critical to ensure a safe and successful extubation.
Q 8. What are the signs and symptoms of respiratory distress?
Respiratory distress manifests as a spectrum of signs and symptoms indicating the body’s struggle to adequately oxygenate tissues. Early signs can be subtle, including increased respiratory rate (tachypnea), use of accessory muscles (like neck and shoulder muscles) to aid breathing, and nasal flaring. As distress worsens, more pronounced symptoms emerge such as retractions (the skin around the ribs and collarbone pulling inwards with each breath), grunting sounds on exhalation, and cyanosis (bluish discoloration of the skin and mucous membranes due to low oxygen levels). Patients may also exhibit restlessness, anxiety, and altered mental status due to hypoxia (low oxygen in the blood). In severe cases, respiratory failure ensues, characterized by inability to maintain adequate oxygenation and/or ventilation despite maximal effort.
- Example: A patient presenting with a respiratory rate of 30 breaths per minute, using their accessory muscles, and exhibiting nasal flaring would be considered to have early signs of respiratory distress.
- Example: A patient with marked retractions, grunting, and cyanosis is experiencing severe respiratory distress, requiring immediate intervention.
Q 9. Explain the concept of PEEP and its physiological effects.
PEEP, or Positive End-Expiratory Pressure, is a ventilator setting that maintains a positive pressure in the lungs at the end of exhalation. Instead of allowing the lungs to completely deflate, PEEP keeps some air in the alveoli (tiny air sacs in the lungs). This has several physiological effects:
- Improved Oxygenation: PEEP helps to recruit collapsed alveoli, opening them up for gas exchange and improving oxygenation. Think of it like inflating a slightly deflated balloon – it allows for better expansion and gas exchange.
- Increased Functional Residual Capacity (FRC): PEEP increases the volume of air remaining in the lungs at the end of exhalation. This larger FRC improves lung mechanics and reduces the work of breathing.
- Reduced Shunt: By improving alveolar recruitment, PEEP reduces the amount of blood flowing through areas of the lung that are not participating in gas exchange (shunt), further enhancing oxygenation.
- Potential Side Effects: While beneficial, high PEEP can also have negative consequences, such as barotrauma (lung injury from excessive pressure) or hemodynamic instability (affecting blood pressure and heart function). Therefore, PEEP levels must be carefully titrated to achieve the desired benefits while minimizing risks.
Clinical Application: PEEP is frequently used in patients with acute respiratory distress syndrome (ARDS) and other conditions characterized by hypoxemia to improve oxygenation and lung mechanics.
Q 10. How do you interpret arterial blood gas results in the context of mechanical ventilation?
Interpreting arterial blood gas (ABG) results in mechanically ventilated patients is crucial for guiding ventilator management. Key values include:
- PaO2 (Partial pressure of oxygen in arterial blood): Indicates the amount of oxygen dissolved in the blood. Low PaO2 (hypoxemia) suggests inadequate oxygenation, potentially requiring adjustments to FiO2 (fraction of inspired oxygen) or PEEP.
- PaCO2 (Partial pressure of carbon dioxide in arterial blood): Reflects the adequacy of ventilation. High PaCO2 (hypercapnia) suggests inadequate ventilation, potentially necessitating increased respiratory rate or tidal volume. Low PaCO2 (hypocapnia) may indicate hyperventilation, possibly due to pain, anxiety, or ventilator settings.
- pH (Blood acidity): Reflects the balance between acids and bases in the blood. Acidosis (low pH) can be respiratory (due to hypercapnia) or metabolic (due to other factors). Alkalosis (high pH) is usually associated with hyperventilation (hypocapnia) but also can be metabolic.
- HCO3- (Bicarbonate): A component of the blood’s buffering system; helps regulate pH. Changes in HCO3- often indicate metabolic disturbances.
Example: A patient with a PaO2 of 60 mmHg, PaCO2 of 55 mmHg, and pH of 7.25 indicates both hypoxemia and respiratory acidosis, suggesting the need for ventilator adjustments such as increased FiO2, PEEP, or respiratory rate.
Important Note: ABG interpretation must always be considered in the clinical context, taking into account the patient’s overall condition, other vital signs, and response to therapy.
Q 11. Describe your experience with managing patients with ARDS.
Managing patients with ARDS (Acute Respiratory Distress Syndrome) requires a multidisciplinary approach and close monitoring. My experience involves employing lung-protective ventilation strategies, including low tidal volumes, low respiratory rates, and the use of PEEP to optimize oxygenation while minimizing lung injury. I’m proficient in titrating ventilator settings based on ABG analysis and clinical assessment, focusing on minimizing ventilator-induced lung injury (VILI). I have experience with various modes of ventilation, including volume-controlled and pressure-controlled ventilation, as well as the use of recruitment maneuvers. Prone positioning, when indicated, is a significant component of management in severe cases, and I’m experienced in managing the challenges associated with it. Furthermore, meticulous attention is given to fluid management, as fluid overload can worsen ARDS. I have collaborated extensively with other specialists, including pulmonologists, intensivists, and respiratory therapists to provide comprehensive care, including the appropriate use of pharmacological interventions such as sedation and analgesia. Each patient’s approach is individualized based on the severity of their condition and overall clinical picture.
Example: I managed a patient with severe ARDS who required high levels of PEEP and prone positioning. Careful titration of these parameters, along with close monitoring of hemodynamics and oxygenation, resulted in improved lung mechanics and weaning from mechanical ventilation.
Q 12. What are the key parameters you monitor during mechanical ventilation?
During mechanical ventilation, several key parameters need constant monitoring. These include:
- Respiratory Rate and Tidal Volume: Essential indicators of ventilation adequacy. Changes in these parameters indicate a potential problem or response to treatment.
- Minute Ventilation (VE): The total volume of air moved in and out of the lungs per minute. It helps assess the overall effectiveness of ventilation.
- Arterial Blood Gases (ABGs): Provide vital information on oxygenation and ventilation, guiding ventilator adjustments.
- Oxygen Saturation (SpO2): Non-invasive measure of oxygenation, providing continuous monitoring.
- Heart Rate and Blood Pressure: Monitoring cardiovascular status is crucial, as mechanical ventilation can impact hemodynamics.
- End-tidal CO2 (EtCO2): Reflects alveolar CO2 levels, offering real-time information on ventilation. It’s often an early indicator of changes in ventilation.
- Peak Inspiratory Pressure (PIP) and Plateau Pressure: Reflects lung mechanics. High pressures can suggest over-distension and possible barotrauma.
- Compliance and Resistance: These values indicate how easily the lungs expand and how much airway resistance is present.
- Sedation Level: Patients should receive the minimum necessary sedation to facilitate optimal ventilator management and allow for timely weaning from mechanical ventilation.
Continuous monitoring of these parameters helps ensure patient safety and optimizes ventilation strategies.
Q 13. How do you troubleshoot ventilator alarms?
Troubleshooting ventilator alarms is critical for patient safety. The approach involves a systematic process:
- Identify the Alarm: Determine the type of alarm (high-pressure, low-pressure, apnea, low oxygen, etc.).
- Assess the Patient: Check the patient’s respiratory effort, breath sounds, oxygen saturation, and overall clinical status. Is the patient coughing, struggling, or exhibiting signs of distress?
- Check the Ventilator Connections and Settings: Ensure all connections are secure and that ventilator settings (tidal volume, respiratory rate, FiO2, PEEP) are appropriate and haven’t been accidentally altered.
- Look for Obstructions: Check for secretions or kinks in the endotracheal tube. If necessary, suction the airway gently.
- Evaluate Lung Mechanics: High-pressure alarms may indicate increased airway resistance or decreased lung compliance, necessitating adjustments in ventilator settings or treatment of underlying conditions.
- Address Underlying Issues: Alarms can be triggered by various factors such as pneumothorax, bronchospasm, or pulmonary edema. Addressing these underlying issues is paramount.
- Consult as needed: Don’t hesitate to consult with a respiratory therapist or physician if the alarm cannot be easily resolved.
Example: A high-pressure alarm may be caused by a kinked endotracheal tube or increased airway secretions, resolved by either removing the kink or suctioning the secretions. A low-pressure alarm might signal a disconnection, prompting immediate assessment and reconnection.
Q 14. Explain the difference between hypoxemia and hypercapnia.
Hypoxemia and hypercapnia are two distinct but related respiratory abnormalities:
- Hypoxemia: Refers to low oxygen levels in the arterial blood (low PaO2). It is a result of inadequate oxygen delivery to the lungs or impaired gas exchange in the alveoli. Symptoms may include shortness of breath, cyanosis, confusion, and altered mental status.
- Hypercapnia: Refers to elevated carbon dioxide levels in the arterial blood (high PaCO2). This usually indicates inadequate removal of CO2 from the lungs, often due to impaired ventilation. Symptoms can include headache, drowsiness, disorientation, and eventually, coma.
Key Differences: Hypoxemia primarily affects oxygenation, while hypercapnia affects carbon dioxide removal. They can occur together (e.g., in acute respiratory failure), or independently. Treatment approaches differ accordingly; hypoxemia is often addressed by increasing oxygen delivery, while hypercapnia requires improving alveolar ventilation.
Example: A patient with pneumonia may experience both hypoxemia (due to impaired gas exchange) and hypercapnia (due to reduced ventilation). Treatment would include oxygen therapy to address hypoxemia and potentially mechanical ventilation to improve ventilation and reduce hypercapnia.
Q 15. Describe your experience with different types of airway management (e.g., endotracheal intubation, tracheostomy).
Airway management is a critical skill in critical care, and my experience encompasses both endotracheal intubation and tracheostomy. Endotracheal intubation involves inserting a tube into the trachea through the mouth or nose to secure an airway and facilitate mechanical ventilation. I’m proficient in various techniques, including rapid sequence intubation for emergency situations and fiberoptic intubation for challenging anatomies. For example, I’ve successfully managed intubations in patients with limited neck mobility due to trauma or underlying disease. Tracheostomy, on the other hand, involves creating a surgical opening in the trachea to establish a long-term airway. I’ve participated in numerous tracheostomy procedures, both surgically and percutaneously, and have extensive experience managing the associated complications, such as bleeding, infection, and tube dislodgement. I also have experience with managing patients who require a change of tracheostomy tubes and assisting them with weaning from the tracheostomy tube. This often involves careful monitoring of the patient’s respiratory status and adjusting ventilation support as needed. Post-procedure care, including suctioning and airway hygiene, is also a routine part of my practice.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you assess and manage sedation in mechanically ventilated patients?
Sedation management in ventilated patients is a delicate balance. The goal is to provide adequate sedation to improve patient comfort and tolerance of mechanical ventilation while minimizing adverse effects like prolonged mechanical ventilation, delirium, and increased risk of infection. My assessment includes a thorough review of the patient’s medical history, neurological status, and vital signs. I use validated sedation scales like the Ramsay Sedation Scale or Richmond Agitation-Sedation Scale (RASS) to objectively assess the level of sedation. Based on the assessment, I tailor the sedation regimen, often using a combination of medications such as propofol, dexmedetomidine, or opioids. I prioritize a multimodal approach, using non-pharmacological interventions such as noise reduction and environmental control to supplement medication. Continuous monitoring is crucial. I carefully monitor respiratory parameters, hemodynamics, and neurological function, adjusting the sedation level as needed. I also implement regular spontaneous breathing trials to assess the readiness for weaning from mechanical ventilation. For example, I might switch a patient from a continuous infusion of propofol to intermittent boluses, allowing for periods of spontaneous breathing to reduce the risk of prolonged sedation. This individualized approach ensures optimal patient comfort and safety while promoting timely extubation.
Q 17. What is your approach to managing a patient with a pneumothorax on a ventilator?
A pneumothorax, or collapsed lung, in a ventilated patient is a serious complication that requires immediate attention. My approach begins with confirming the diagnosis through chest x-ray or ultrasound. The management depends on the severity of the pneumothorax. For small pneumothoraces, observation may suffice, especially if the patient is hemodynamically stable and the pneumothorax is not progressing. Larger pneumothoraces, however, usually require intervention. This typically involves inserting a chest tube to re-expand the lung. The placement of a chest tube involves local anesthesia and careful selection of the insertion site to minimize complications. Following chest tube placement, I carefully monitor the patient’s respiratory parameters and chest tube drainage. It’s also important to note the placement of the chest tube in the appropriate location with proper lung expansion and drainage. If a patient remains unstable even with a chest tube, additional interventions, such as surgical repair, may be necessary. I often collaborate closely with thoracic surgery to determine the most appropriate approach for each individual case. Consistent monitoring is key, watching for signs of re-expansion pulmonary edema or recurrent pneumothorax.
Q 18. How do you manage a patient with a tension pneumothorax?
A tension pneumothorax is a life-threatening condition requiring immediate intervention. Unlike a simple pneumothorax, a tension pneumothorax causes a build-up of air in the pleural space, which compresses the lung and compromises cardiovascular function. Management involves immediate needle decompression, typically performed using a large-bore needle inserted into the second intercostal space in the mid-clavicular line. This rapidly relieves the pressure and improves the patient’s condition. After needle decompression, a chest tube is placed to maintain lung re-expansion and prevent recurrence. This is a true emergency; every second counts. I have experience in managing this situation in both the ICU and emergency department settings and understand the necessity of rapid and decisive action. The patient’s hemodynamic status needs constant monitoring after decompression. Post-procedure, the patient is monitored closely for signs of recurrence or complications associated with chest tube placement.
Q 19. Describe your experience with non-invasive ventilation (NIV).
Non-invasive ventilation (NIV) encompasses various techniques to support ventilation without the need for endotracheal intubation. My experience includes using various NIV modalities, such as continuous positive airway pressure (CPAP), bilevel positive airway pressure (BiPAP), and pressure support ventilation. I’ve used NIV in diverse patient populations, including those with acute exacerbations of COPD, acute respiratory distress syndrome (ARDS), and cardiogenic pulmonary edema. I’m skilled in selecting appropriate settings, troubleshooting equipment malfunctions, and educating patients and families about the use of NIV. For instance, I’ve successfully employed NIV to avoid intubation in patients with COPD exacerbations, improving their comfort and reducing the risk of associated complications from intubation. Successful NIV requires thorough patient assessment and selection of appropriate settings based on respiratory parameters and clinical picture.
Q 20. What are the advantages and disadvantages of NIV?
NIV offers several advantages over invasive ventilation, including a reduced risk of ventilator-associated pneumonia (VAP), improved patient comfort and ability to communicate, and earlier mobilization and rehabilitation. However, NIV also has limitations. It may be ineffective in patients with severe respiratory compromise, altered consciousness, or excessive secretions. It also requires patient cooperation, which can be a challenge in some cases. Furthermore, NIV can lead to complications such as skin breakdown from mask pressure, gastric distension, and hemodynamic instability if improperly managed. Choosing between NIV and invasive ventilation is a critical decision, carefully weighed against patient-specific factors and clinical judgment. For example, a patient with a severe exacerbation of COPD who is alert and cooperative might benefit greatly from NIV, avoiding the need for intubation. Conversely, a patient with severe ARDS and altered consciousness would likely require invasive ventilation.
Q 21. How do you select appropriate ventilator settings for different patient populations?
Selecting appropriate ventilator settings is a complex process that requires careful consideration of the patient’s respiratory physiology, disease severity, and overall clinical status. It is not a one-size-fits-all approach. I tailor ventilator settings based on factors like the patient’s age, underlying medical conditions, and the severity of respiratory failure. For instance, patients with acute respiratory distress syndrome (ARDS) require a different approach than those with chronic obstructive pulmonary disease (COPD). I use arterial blood gas analysis and respiratory mechanics to guide my decisions, focusing on maintaining adequate oxygenation and ventilation while minimizing lung injury. I start by setting tidal volume and respiratory rate, aiming for eucapnia (normal CO2 levels) and adequate oxygenation. Positive end-expiratory pressure (PEEP) is adjusted to recruit collapsed alveoli and improve oxygenation without over-distending the lungs. I closely monitor the patient’s response to these settings and make adjustments as necessary. In some cases, I utilize advanced ventilation strategies like lung-protective ventilation to minimize ventilator-induced lung injury. For ARDS, I might use a lower tidal volume strategy and higher PEEP to optimize gas exchange while protecting the lungs. Regular monitoring of the patient’s respiratory status and adjustments based on that is key to optimized ventilator management.
Q 22. What are the ethical considerations in managing critically ill patients?
Ethical considerations in critical care are paramount and often involve navigating complex situations with significant uncertainty. We must constantly balance the patient’s best interests with their autonomy, family wishes, and resource allocation. This involves:
- Informed Consent: Ensuring patients or their surrogates understand the risks, benefits, and alternatives to proposed treatments, even when time is limited. This may involve simplifying complex medical information into easily digestible terms. For example, explaining the pros and cons of mechanical ventilation to a family member facing a difficult decision.
- Beneficence and Non-maleficence: Acting in the patient’s best interest while minimizing harm. This often requires careful weighing of the potential benefits of aggressive treatments against their potential side effects and burdens. For example, a patient with end-stage disease might benefit more from comfort measures rather than aggressive life-sustaining treatments.
- Justice and Resource Allocation: Fairly distributing limited resources, like ICU beds or ventilators, especially during crises. This requires a system of prioritization based on objective criteria and ethical principles, prioritizing those with the highest chance of survival and avoiding discriminatory practices.
- End-of-Life Care: Respecting patient wishes regarding life-sustaining treatments through advanced directives or discussions with family. This includes honest conversations about prognosis and respecting decisions to forgo life-sustaining measures.
Ethical decision-making often involves interdisciplinary discussions with physicians, nurses, social workers, chaplains, and ethics committees, ensuring a holistic approach to patient care and respecting all voices in the decision-making process.
Q 23. Describe your experience with hemodynamic monitoring in the ICU.
Hemodynamic monitoring is essential for managing critically ill patients. My experience encompasses the use of various methods, including arterial lines (allowing continuous blood pressure and blood gas sampling), central venous catheters (providing access for fluid administration and monitoring central venous pressure), and pulmonary artery catheters (though their use has decreased with evolving evidence, I have experience with their application in selected patients to assess cardiac output and pulmonary pressures). I’m proficient in interpreting the data obtained from these monitoring devices and adjusting treatment strategies based on these parameters. For example, I’ve used CVP measurements to guide fluid resuscitation and avoid fluid overload, recognizing that its usefulness is limited in certain conditions.
I’m also experienced in using less invasive monitoring techniques, such as echocardiography (both transthoracic and transesophageal), which offer valuable insights into cardiac function and hemodynamic status without the risks associated with invasive lines. I understand the limitations of each technique and use a multimodal approach to get a comprehensive picture of a patient’s hemodynamic status. This holistic approach is crucial for accurate assessment and effective treatment.
Q 24. How do you manage a patient with a sudden drop in blood pressure?
A sudden drop in blood pressure, or hypotensive shock, is a life-threatening emergency requiring immediate action. My approach follows a structured algorithm focusing on identifying the underlying cause and initiating appropriate therapy simultaneously.
- ABCDE Approach: First, I ensure the patient’s airway, breathing, and circulation are addressed. This might involve securing the airway, providing supplemental oxygen, and initiating intravenous access.
- Identify the Cause: Simultaneously, I rapidly assess potential causes, which could include hypovolemia (fluid loss), cardiac dysfunction (heart failure, arrhythmias), sepsis (infection-induced shock), anaphylaxis, or neurogenic shock. Rapid assessment involves history-taking, focused physical exam, and immediate lab testing (blood tests, lactate).
- Fluid Resuscitation: For hypovolemic shock, rapid fluid resuscitation with crystalloid solutions (e.g., normal saline or Ringer’s lactate) is the cornerstone of treatment. The response to fluid is closely monitored. If this fails to improve blood pressure, other causes must be considered.
- Vasopressors: If fluid resuscitation is insufficient, vasopressor medications (e.g., norepinephrine, dopamine) may be necessary to increase blood pressure. The selection and dose depend on the underlying cause and hemodynamic profile.
- Further Investigations: Further investigations, such as echocardiography, to assess cardiac function and other specific investigations (e.g. blood cultures for sepsis) guide further management.
The management of hypotensive shock is highly individualized and relies on prompt identification of the underlying cause and rapid intervention, emphasizing teamwork and close collaboration with other members of the ICU team.
Q 25. Describe your experience with managing patients with sepsis.
Sepsis management is a complex process requiring a prompt and aggressive approach. My experience involves managing patients across the spectrum of sepsis severity, from early sepsis to septic shock. I follow the Surviving Sepsis Campaign guidelines, prioritizing early recognition and treatment.
- Early Goal-Directed Therapy: This involves rapid assessment, obtaining blood cultures before antibiotic administration, and initiating broad-spectrum antibiotics within the first hour of suspicion. I utilize lactate measurements as an important indicator of tissue perfusion and guide fluid resuscitation, aiming for adequate tissue oxygenation.
- Source Control: Identifying and addressing the source of infection is critical, whether it’s pneumonia, urinary tract infection, or an intra-abdominal abscess. This may involve surgical intervention or other specific interventions like source removal or drainage.
- Hemodynamic Optimization: Maintaining adequate blood pressure and organ perfusion is essential, often requiring fluid resuscitation and vasopressors as previously described. Continuous monitoring of hemodynamic parameters is crucial.
- Organ Support: If organ dysfunction develops, I provide appropriate support, such as mechanical ventilation, renal replacement therapy (dialysis), or other forms of organ-specific support.
- Monitoring and Adjustment: Close monitoring of vital signs, organ function, and inflammatory markers is necessary. Treatment strategies must be adjusted based on the patient’s response and ongoing assessment.
Successful sepsis management relies on a multidisciplinary approach involving infectious disease specialists, surgeons, and other specialists as needed.
Q 26. What is your approach to managing a patient with acute kidney injury?
Acute kidney injury (AKI) management focuses on identifying the underlying cause, supporting kidney function, and preventing further damage. My approach involves a thorough evaluation, including assessment of urine output, serum creatinine levels, and other renal function markers.
- Identify the Cause: The first step is to determine the cause of AKI (pre-renal, intra-renal, or post-renal). This involves assessing volume status, blood pressure, medications (nephrotoxic drugs), and imaging if indicated.
- Fluid Management: For pre-renal AKI (caused by decreased blood flow to the kidneys), careful fluid resuscitation is critical, titrated to maintain adequate urine output and blood pressure. For other forms of AKI, fluid management might be more restricted to prevent fluid overload.
- Nephrotoxic Drug Avoidance: Minimizing exposure to nephrotoxic drugs and adjusting or discontinuing these when possible is crucial.
- Renal Replacement Therapy (RRT): In cases of severe AKI requiring RRT (hemodialysis or continuous renal replacement therapy), the timing and modality of treatment depend on the severity of AKI, fluid overload, and electrolyte disturbances. I have extensive experience with different types of RRT.
- Supportive Care: Close monitoring of electrolytes, acid-base balance, and other potential complications, such as hyperkalemia, is vital. Supportive therapies are provided as needed.
AKI management is a dynamic process requiring regular reassessment and adjustment of treatment based on the patient’s clinical status and laboratory results.
Q 27. How do you manage pain and anxiety in critically ill patients?
Managing pain and anxiety in critically ill patients is crucial for their comfort, recovery, and overall outcome. My approach involves a multimodal strategy, utilizing both pharmacological and non-pharmacological interventions.
- Pharmacological Management: This includes analgesics (opioids, non-opioid analgesics) and anxiolytics (benzodiazepines, propofol). The choice of medication and dosage depend on the patient’s condition and response to treatment. I use sedation protocols to carefully titrate medication while avoiding oversedation. Pain assessments use validated pain scales such as the numeric rating scale (NRS) or the critical-care pain observation tool (CPOT).
- Non-Pharmacological Interventions: These include techniques like relaxation exercises, music therapy, repositioning, and environmental modifications to minimize noise and light. Providing emotional support and involving family members in care significantly reduces anxiety.
- Sedation Management: I employ strategies to minimize sedation, promoting early mobilization and reducing the duration of mechanical ventilation. Daily sedation interruptions are often used to assess patient comfort and readiness for weaning.
- Delirium Management: Early detection and management of delirium, a common complication in critically ill patients, is paramount. This often involves environmental modifications, pharmacological interventions if necessary, and early mobilization.
A key aspect of my approach is individualizing pain and anxiety management based on the patient’s specific needs and preferences, recognizing that the most effective approach often involves a combination of strategies.
Q 28. Describe your experience with advanced cardiac life support (ACLS).
I have extensive experience in Advanced Cardiac Life Support (ACLS), having participated in numerous ACLS courses and actively utilizing these skills in the ICU. My experience encompasses managing various cardiac arrests, including those resulting from arrhythmias (ventricular fibrillation, pulseless ventricular tachycardia) and cardiac arrest secondary to other conditions (e.g., hypovolemia, tension pneumothorax, tamponade).
- Teamwork and Leadership: ACLS is a team-based approach, and I’m comfortable leading the resuscitation team, delegating tasks efficiently, and maintaining clear communication throughout the process.
- Rhythm Recognition and Interpretation: Rapid and accurate interpretation of electrocardiograms (ECGs) is critical. I can effectively identify various cardiac rhythms and initiate appropriate interventions.
- Defibrillation and Cardioversion: I am proficient in performing defibrillation and cardioversion, ensuring safety protocols are followed meticulously.
- Advanced Life Support Medications: I’m experienced in administering various medications used in ACLS, including epinephrine, amiodarone, and vasopressin, following established guidelines.
- Post-Resuscitation Care: ACLS doesn’t end with return of spontaneous circulation (ROSC). I’m experienced in providing post-resuscitation care, including targeted temperature management and neuroprotective strategies.
My ACLS experience underscores the importance of continuous learning and training, ensuring that my skills remain up to date and that I can effectively manage life-threatening cardiac emergencies. Regular participation in simulation training maintains my proficiency in a low-stakes setting.
Key Topics to Learn for Critical Care and Ventilator Management Interview
- Physiology of Respiratory Failure: Understanding the underlying mechanisms of respiratory distress, including acute respiratory distress syndrome (ARDS), and different types of respiratory failure.
- Mechanical Ventilation Modes: A thorough grasp of various ventilation modes (e.g., volume control, pressure control, pressure support) and their appropriate applications based on patient physiology and clinical needs. Practical application: Being able to explain the rationale behind choosing a specific mode for a given patient scenario.
- Ventilator Settings and Parameters: Mastering the interpretation and adjustment of key ventilator parameters like tidal volume, respiratory rate, PEEP, FiO2, and airway pressure. Practical application: Troubleshooting ventilator alarms and adjusting settings based on arterial blood gas analysis.
- Weaning from Mechanical Ventilation: Understanding the process of weaning patients from mechanical ventilation, including readiness assessment, weaning protocols, and managing complications.
- Monitoring and Assessment: Proficiently interpreting arterial blood gases (ABGs), chest x-rays, and other diagnostic tools to assess respiratory status and guide ventilator management. Practical application: Describing how changes in ABGs would influence ventilator settings.
- Complications of Mechanical Ventilation: Knowledge of potential complications such as ventilator-associated pneumonia (VAP), barotrauma, volutrauma, and strategies for prevention and management.
- Advanced Ventilator Techniques: Familiarity with advanced techniques such as high-frequency ventilation, extracorporeal membrane oxygenation (ECMO), and prone positioning.
- Ethical and Legal Considerations: Understanding ethical dilemmas related to end-of-life decisions and resource allocation in critical care, as well as legal aspects of patient care.
- Teamwork and Communication: Highlighting experience with effective communication within a multidisciplinary critical care team.
Next Steps
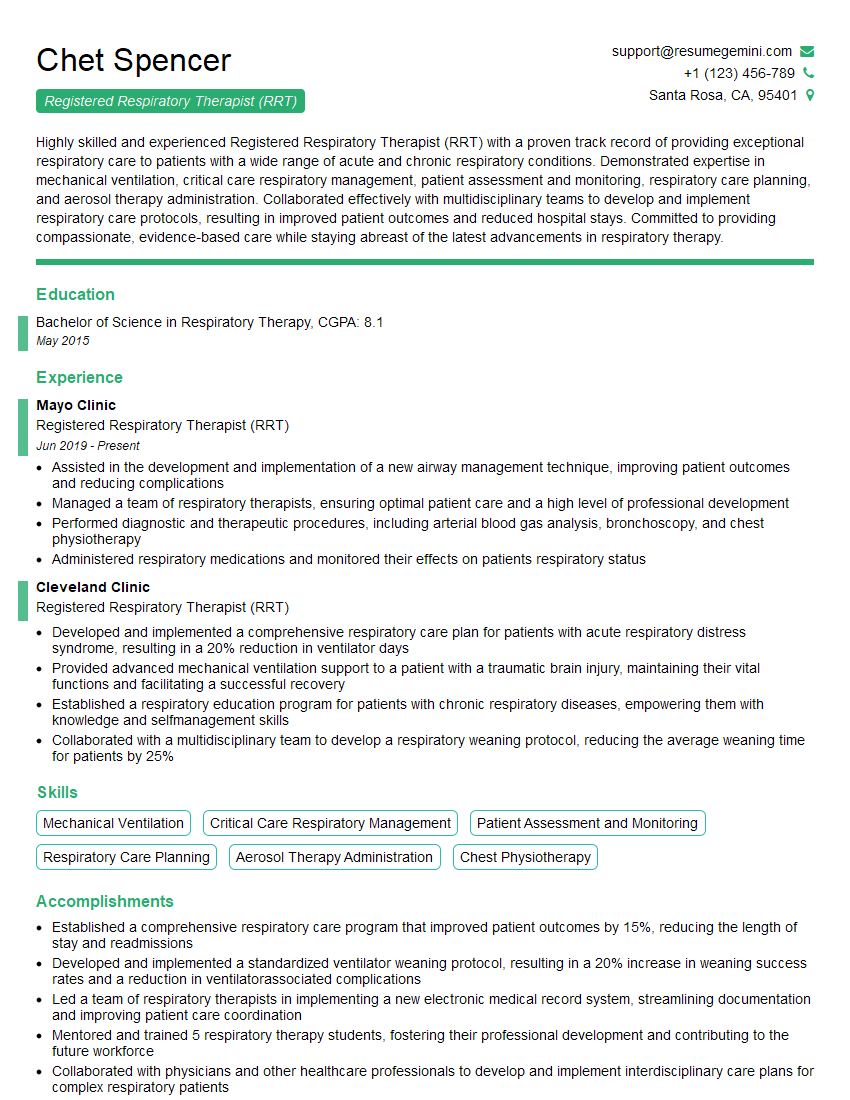
Mastering Critical Care and Ventilator Management significantly enhances your career prospects, opening doors to specialized roles and leadership opportunities within intensive care units. An ATS-friendly resume is crucial for getting your application noticed by recruiters. To make your resume stand out and showcase your expertise effectively, we recommend using ResumeGemini. ResumeGemini offers a powerful toolset to build professional, impactful resumes, and provides examples of resumes tailored to Critical Care and Ventilator Management to help guide your application process. Invest in your future – create a resume that reflects your exceptional skills and experience.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
To the interviewgemini.com Webmaster.
Very helpful and content specific questions to help prepare me for my interview!
Thank you
To the interviewgemini.com Webmaster.
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.