Every successful interview starts with knowing what to expect. In this blog, we’ll take you through the top Heart-Lung Transplantation interview questions, breaking them down with expert tips to help you deliver impactful answers. Step into your next interview fully prepared and ready to succeed.
Questions Asked in Heart-Lung Transplantation Interview
Q 1. Describe the process of donor organ selection for heart-lung transplantation.
Donor organ selection for heart-lung transplantation is a critical process that prioritizes the best possible match for the recipient while adhering to strict ethical guidelines. It’s a complex balancing act considering several factors.
- Blood type compatibility: The donor’s blood type must be compatible with the recipient’s, or at least compatible enough to bridge a potential mismatch with careful blood management strategies. ABO incompatibility is a major barrier.
- Size matching: The donor’s heart and lungs must be appropriately sized for the recipient to prevent strain and ensure proper function. This is assessed through various imaging techniques and is crucial to avoid post-operative complications.
- Organ function: The donor’s heart and lungs must be functioning optimally before procurement. Comprehensive testing assesses this, looking at things like blood pressure, oxygen saturation, and the absence of significant lung disease. This is assessed via various imaging and functional tests.
- Donor history: The donor’s medical history is meticulously reviewed to rule out any contraindications, such as infections, cancer, or other conditions that could compromise graft survival or cause rejection.
- Immunological matching: HLA (Human Leukocyte Antigen) typing is performed to assess the compatibility of the donor and recipient’s immune systems, aiming for the closest match possible to minimize the risk of rejection. The closer the match, the lower the risk of rejection, and the less intense immunosuppression needed.
- Distance and logistics: The geographical distance between the donor and recipient plays a significant role, impacting the viability of the organs. There is a strict time limit for organ preservation and transportation. Organs need to be procured and transported quickly to maintain viability
Imagine it like finding the perfect puzzle piece – all the elements must fit together seamlessly. A slight mismatch might still work, but a perfect fit significantly increases the chances of long-term success.
Q 2. Explain the different surgical techniques used in heart-lung transplantation.
Heart-lung transplantation involves a complex surgical procedure, and several techniques are employed depending on the patient’s specific condition and the surgeon’s preference. The core of the surgery remains consistent, however the approach can vary.
- Orthotopic transplantation: This is the most common technique, where the diseased heart and lungs are removed and replaced with the donor organs in their natural anatomical positions. This is the standard approach.
- En bloc transplantation: In this technique, the heart and lungs are removed and transplanted as a single unit. It’s usually considered when there is extensive involvement of the mediastinum (the area in the chest between the lungs) or complex pathology.
- Staged transplantation: Sometimes, a staged approach is used, where the heart is transplanted first, followed by lung transplantation later. This is mostly relevant in complex cases where the heart and lungs are individually assessed for suitability.
These techniques all aim to restore normal heart and lung function by replacing diseased organs with healthy ones. The specific approach used hinges on individual circumstances and requires advanced surgical expertise.
Q 3. What are the key physiological parameters monitored during and after a heart-lung transplant?
Continuous and meticulous monitoring of physiological parameters is crucial throughout the entire process of heart-lung transplantation, from the intraoperative phase to the long-term follow-up. This is done to ensure organ viability and identify potential complications early. This includes:
- Hemodynamic parameters: Heart rate, blood pressure, cardiac output, and central venous pressure are continuously monitored to assess the heart’s function and overall circulatory status.
- Respiratory parameters: Oxygen saturation (SpO2), arterial blood gases (ABGs), respiratory rate, and lung volumes are closely watched to evaluate lung function and gas exchange.
- Electrocardiogram (ECG): ECG monitoring is essential for detecting arrhythmias (irregular heartbeats), a common complication after transplantation.
- Laboratory tests: Blood tests, including complete blood counts, electrolytes, coagulation studies, and liver function tests, are performed regularly to assess organ function and identify signs of infection or rejection.
- Imaging studies: Chest X-rays, echocardiograms, and computed tomography (CT) scans may be used at different times to assess the status of the transplanted organs and identify any structural abnormalities or complications.
Think of this as a constant vigil – keeping a close watch to ensure everything is functioning smoothly and detect any problems as soon as they arise.
Q 4. How do you manage rejection in heart-lung transplant recipients?
Rejection is a major threat after heart-lung transplantation, where the recipient’s immune system attacks the transplanted organs. Managing it requires aggressive immunosuppression.
- Immunosuppressive medications: These medications suppress the immune system’s activity, reducing the risk of rejection. A common regimen includes combinations of medications such as corticosteroids, calcineurin inhibitors (cyclosporine, tacrolimus), and antiproliferative agents (azathioprine, mycophenolate mofetil). The dosage varies greatly depending on the patient’s specific condition and level of immunosuppression needed.
- Biopsies: Endomyocardial and lung biopsies are sometimes performed to assess the extent of rejection. These provide tissue samples for microscopic analysis that will help the physicians make informed therapeutic decisions.
- Monitoring for rejection: Regular blood tests, measuring the patient’s creatinine and other biomarkers, are used to detect signs of organ damage. An increase in creatinine can be a sign that the kidneys are starting to be affected, which could be associated with rejection.
- Treatment of rejection: If rejection is detected, high-dose corticosteroids are usually administered to suppress the immune response, sometimes along with other anti-rejection therapies, such as monoclonal antibodies. More targeted and refined therapies are constantly under research and development.
The goal is to find a delicate balance – suppressing the immune system enough to prevent rejection without leaving the recipient vulnerable to infections.
Q 5. Describe the common complications associated with heart-lung transplantation.
Heart-lung transplantation, while life-saving, carries a risk of various complications. These can occur during surgery, in the immediate postoperative period, or later on.
- Infection: Immunosuppressive drugs increase susceptibility to infections, which can range from mild to life-threatening. Pneumonia, bloodstream infections, and fungal infections are significant concerns.
- Rejection: As mentioned earlier, rejection is a major complication that can lead to organ failure if not managed effectively.
- Bleeding: Significant blood loss can occur during surgery or later due to anticoagulation therapy.
- Arrhythmias: Irregular heartbeats are common after heart transplantation.
- Primary graft dysfunction: This refers to poor function of the transplanted heart and lungs immediately after surgery, which can be life-threatening.
- Chronic rejection: This is a slower, more insidious form of rejection that can lead to gradual organ deterioration over time.
- Renal failure: Immunosuppressive drugs and other factors can lead to kidney dysfunction.
- Neurological complications: Stroke and other neurological issues are possible due to the complex nature of the surgery and circulatory implications.
Careful monitoring, prompt treatment, and a multidisciplinary approach are essential to manage these complications effectively.
Q 6. What are the indications for heart-lung transplantation?
Heart-lung transplantation is a complex procedure reserved for patients with end-stage heart and lung disease that’s refractory to other treatments. Several indications exist that mandate this high-risk yet life-saving intervention.
- Severe pulmonary hypertension: Untreatable high blood pressure in the lungs that significantly impairs the heart and lungs.
- Cystic fibrosis: A genetic condition leading to progressive lung damage and eventual respiratory failure.
- Interstitial lung disease: A group of conditions causing scarring and inflammation of the lung tissue.
- Severe congenital heart disease: Congenital heart defects that severely impair heart and lung function.
- Eisenmenger syndrome: A severe complication of congenital heart defects, where increased blood flow through the lungs results in severe pulmonary hypertension.
- Primary pulmonary hypertension: High blood pressure in the arteries of the lungs, often of unknown cause.
These conditions all share the common thread of progressive, life-threatening impairment of both heart and lung function. It’s only after exhausting other therapies that heart-lung transplantation becomes a viable option. The patient’s overall health, quality of life, and prognosis are also critically evaluated.
Q 7. Discuss the role of immunosuppression in heart-lung transplantation.
Immunosuppression plays a pivotal role in heart-lung transplantation to prevent rejection. Without it, the recipient’s immune system would recognize the transplanted organs as foreign and attack them, leading to organ failure.
- Goal: The primary goal of immunosuppression is to prevent the recipient’s immune system from mounting an attack against the transplanted organs while minimizing the risk of infection and other complications. It’s a balancing act.
- Medication regimen: A cocktail of medications is used, typically including corticosteroids, calcineurin inhibitors (like cyclosporine or tacrolimus), and antiproliferative agents (like azathioprine or mycophenolate mofetil). This is carefully tailored to the individual patient and their needs, always with the aim of minimizing the dose while maximizing the efficacy.
- Monitoring: Careful monitoring is required to adjust the dosage of immunosuppressants and detect any adverse effects. Blood tests to measure levels of the drugs, as well as tests to assess kidney and liver function are critical.
- Long-term implications: Long-term immunosuppression carries risks, such as increased susceptibility to infections, development of certain cancers, and kidney or liver damage. Life-long monitoring is necessary.
Immunosuppression is not a simple ‘one-size-fits-all’ approach; it’s a dynamic process that requires continuous adjustment based on the patient’s response and the evolving clinical picture. It’s a critical element in ensuring the long-term success of the transplant.
Q 8. How do you assess the functional status of a potential heart-lung transplant recipient?
Assessing the functional status of a potential heart-lung transplant recipient is a multi-faceted process requiring a comprehensive evaluation. We aim to determine the severity of their end-stage disease and their ability to tolerate the transplant procedure and subsequent immunosuppression. This involves a detailed history, physical examination, and numerous investigations.
- Cardiac Assessment: This includes echocardiography (to assess heart function), cardiac catheterization (to measure pressures and assess coronary arteries), and right heart catheterization (to evaluate pulmonary vascular resistance). We look for indicators like low ejection fraction, severe pulmonary hypertension, and irreversible heart damage.
- Pulmonary Assessment: Pulmonary function tests (PFTs) are crucial to measure lung volumes and gas exchange. High-resolution CT scans identify the extent of lung disease, and bronchoscopy may be performed for more detailed evaluation. We look for irreversible lung damage, severe hypoxemia (low blood oxygen), and evidence of significant airway disease.
- Systemic Evaluation: We assess other organ systems for dysfunction, including liver, kidneys, and neurological status. Blood tests reveal overall health, infection, and clotting function. Psychological evaluation is crucial to assess the patient’s ability to adhere to the complex post-transplant regimen.
- Matching: Finally, we assess the recipient’s compatibility with potential donor organs, considering blood type, size, and HLA (Human Leukocyte Antigen) matching to minimize the risk of rejection.
For instance, a patient with severe cystic fibrosis and severe pulmonary hypertension requiring significant supplemental oxygen would require a comprehensive assessment to determine their suitability for a heart-lung transplant. We carefully weigh the benefits and risks, considering their overall health and likelihood of a successful outcome.
Q 9. Explain the different types of immunosuppressant drugs used.
Immunosuppressant drugs are essential after heart-lung transplantation to prevent organ rejection. We utilize a combination of agents to minimize side effects while maximizing efficacy. These drugs broadly fall into several categories:
- Calcineurin Inhibitors: Tacrolimus and cyclosporine are cornerstone drugs, preventing T-cell activation and subsequent rejection. They are potent but have side effects like nephrotoxicity (kidney damage), neurotoxicity, and hyperglycemia (high blood sugar).
- Antimetabolites: Azathioprine and mycophenolate mofetil inhibit DNA synthesis in lymphocytes, reducing immune activity. Side effects include bone marrow suppression and gastrointestinal issues.
- mTOR Inhibitors: Sirolimus and everolimus block mTOR signaling, a key pathway in T-cell activation. They are often used in combination with calcineurin inhibitors to reduce their toxicity.
- Corticosteroids: Prednisone provides strong anti-inflammatory effects in the early post-transplant period, reducing inflammation and the risk of acute rejection. Long-term use is associated with significant side effects such as osteoporosis, hyperglycemia, and weight gain.
- Belatacept: This newer agent selectively blocks T-cell co-stimulation, reducing immunosuppression-related side effects compared to traditional regimens.
The choice and combination of immunosuppressants are individualized based on the patient’s risk factors, other medical conditions, and response to treatment. Careful monitoring of blood levels and potential side effects is vital.
Q 10. What are the long-term complications of heart-lung transplantation?
Heart-lung transplant recipients face several long-term complications, many stemming from the immunosuppression required to prevent rejection. These include:
- Infection: Immunosuppression significantly increases susceptibility to infections, ranging from common colds to life-threatening opportunistic infections like cytomegalovirus (CMV) and Pneumocystis jirovecii pneumonia.
- Rejection: Despite immunosuppression, some degree of rejection is common. This can be acute (early after transplant) or chronic (developing gradually over time), requiring adjustments to immunosuppression or even re-transplantation.
- Cardiovascular Disease: Patients may develop coronary artery disease, heart failure, or arrhythmias, often due to the transplant procedure or medications.
- Renal Dysfunction: Many immunosuppressants are nephrotoxic, potentially leading to kidney damage requiring dialysis or transplantation.
- Diabetes Mellitus: Steroids and other immunosuppressants can cause or worsen diabetes.
- Malignancy: Long-term immunosuppression increases the risk of developing certain cancers, such as lymphoma and skin cancer.
- Neurological Complications: Some immunosuppressants can cause neurological issues, such as tremor, headache and cognitive impairment.
Regular monitoring, proactive infection control, and careful management of immunosuppression are crucial to mitigate these long-term risks.
Q 11. Describe your experience with managing post-operative pain in heart-lung transplant patients.
Managing post-operative pain in heart-lung transplant recipients is crucial for their recovery and overall well-being. It requires a multimodal approach, addressing both the incisional pain and the pain related to chest tubes and other procedures.
- Analgesics: We initially use intravenous opioids for effective pain control in the immediate post-operative period. This is gradually transitioned to oral analgesics like opioids, NSAIDs (nonsteroidal anti-inflammatory drugs), and acetaminophen, carefully considering potential drug interactions with immunosuppressants.
- Regional Anesthesia: Techniques like epidural analgesia can provide excellent pain relief with fewer systemic side effects, particularly beneficial in the early post-operative phase.
- Non-pharmacological Interventions: These include relaxation techniques, breathing exercises, and patient education to promote coping mechanisms and reduce anxiety. Physical therapy plays a vital role in mobilizing patients and regaining strength and mobility, thereby reducing pain.
- Patient-Controlled Analgesia (PCA): PCA pumps allow patients to self-administer analgesics, providing greater control and reducing anxiety, leading to better pain management.
We tailor the analgesic regimen based on individual needs, considering factors such as comorbidities, drug allergies, and response to treatment. Regular pain assessments are critical to ensure adequate pain control and prevent chronic pain development.
Q 12. How do you manage infections in heart-lung transplant recipients?
Managing infections in heart-lung transplant recipients is paramount, as they are at significantly increased risk due to immunosuppression. Our approach emphasizes both prevention and prompt treatment.
- Prophylactic Measures: This includes vaccinations against common infections (e.g., influenza, pneumococcus), antiviral medications (e.g., ganciclovir for CMV prophylaxis), and antifungal prophylaxis (depending on risk factors). Strict adherence to hand hygiene and isolation precautions is essential.
- Early Recognition and Treatment: We carefully monitor patients for signs and symptoms of infection, including fever, cough, shortness of breath, and changes in lab values. Rapid diagnostic testing is crucial to identify the causative pathogen and initiate targeted therapy promptly. This might involve blood cultures, sputum cultures, or other relevant diagnostic tests.
- Antimicrobial Stewardship: We use antimicrobial agents judiciously, ensuring appropriate selection and dosage to minimize resistance development. Close monitoring of response and potential toxicity is paramount.
- Supportive Care: In addition to antimicrobial therapy, supportive care measures may include intravenous fluids, oxygen therapy, and respiratory support as needed.
A multidisciplinary approach, involving infectious disease specialists, pulmonologists, and intensivists, is often necessary to manage complex or severe infections. For example, the management of a CMV infection might involve antiviral medication, supportive care, and adjustment of immunosuppression.
Q 13. What is your approach to patient education for heart-lung transplant recipients and their families?
Patient education is integral to successful outcomes in heart-lung transplantation. We implement a comprehensive program addressing various aspects of post-transplant care.
- Pre-transplant Education: We discuss the procedure, recovery process, potential complications, medication regimens, and lifestyle modifications. This helps patients and their families understand what to expect and prepare for the challenges ahead.
- Post-transplant Education: We provide detailed instruction on medication administration, signs and symptoms of rejection and infection, dietary guidelines, exercise recommendations, and the importance of adherence to follow-up appointments.
- Support Groups: Connecting patients with support groups provides valuable peer-to-peer support, addressing emotional and psychological challenges.
- Written Materials and Resources: We provide patients with written materials, pamphlets, and access to online resources to reinforce key concepts and address questions that may arise between visits.
We emphasize clear communication, using plain language and visual aids to make complex information easily understandable. Involving family members in the education process is crucial, as they play a key role in supporting the patient’s adherence to the post-transplant regimen.
Q 14. Describe the challenges of managing patients with multiple organ system failure after heart-lung transplant.
Managing patients with multiple organ system failure after heart-lung transplantation presents significant challenges requiring a highly coordinated, multidisciplinary approach. These patients often require intensive care support.
- Identifying and Addressing Underlying Causes: We meticulously investigate the cause of organ dysfunction, which may involve rejection, infection, medication side effects, or other complications. Prompt diagnosis and treatment are essential.
- Hemodynamic Support: Patients may require inotropic support (medications to improve heart contractility) and/or mechanical circulatory support (e.g., extracorporeal membrane oxygenation or ECMO) to maintain adequate organ perfusion.
- Respiratory Support: Mechanical ventilation and other respiratory support modalities may be necessary to manage respiratory failure.
- Renal Replacement Therapy: Dialysis may be needed if kidney function is severely impaired.
- Immunosuppression Management: The immunosuppression regimen may need adjustments based on the severity of rejection and other factors.
- Supportive Care: This includes nutritional support, electrolyte balance correction, and other measures to maintain organ function and patient stability.
The management of such patients necessitates close collaboration among the transplant team, intensivists, and specialists from other fields (e.g., nephrology, infectious diseases). The decisions require careful consideration of risks and benefits for each therapeutic intervention, given the patients’ frailty.
Q 15. How do you identify and manage cardiac arrhythmias in post-transplant patients?
Cardiac arrhythmias are a significant concern after heart-lung transplantation, often stemming from the surgery itself, rejection, or underlying heart disease. Management begins with continuous electrocardiogram (ECG) monitoring. We meticulously identify arrhythmias using ECG, Holter monitoring, and implantable cardiac event recorders (ICERs). Common arrhythmias include atrial fibrillation, ventricular tachycardia, and bradycardia. Treatment varies depending on the severity and type of arrhythmia. For example, atrial fibrillation might be managed with rate control medication like beta-blockers or digoxin, potentially including rhythm control with antiarrhythmic drugs or cardioversion. More serious ventricular arrhythmias may require antiarrhythmic drugs, implantable cardioverter-defibrillators (ICDs), or even catheter ablation. Bradycardia often necessitates the use of a pacemaker. Careful electrolyte management is crucial, as imbalances can trigger or worsen arrhythmias. We closely monitor patients for signs of electrolyte abnormalities and adjust treatment accordingly. For example, low potassium levels (hypokalemia) can increase the risk of arrhythmias.
Imagine it like this: the heart is a finely tuned instrument. Post-transplant, it’s adjusting to a new organ, and that can cause some erratic beats. We use a variety of tools to listen to the heart’s rhythm and make adjustments, like a conductor fine-tuning an orchestra.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What is your experience with extracorporeal membrane oxygenation (ECMO) in the context of heart-lung transplantation?
Extracorporeal membrane oxygenation (ECMO) is a life-support system that temporarily takes over the functions of the heart and lungs. In heart-lung transplantation, ECMO can be invaluable in several situations. Pre-transplant, it can stabilize critically ill patients awaiting a suitable donor organ, allowing them to bridge the time until transplantation. Post-transplant, ECMO can provide support if the transplanted heart and lungs fail to function adequately, buying time for recovery or addressing complications such as primary graft dysfunction. I have extensive experience using ECMO in both pre- and post-transplant scenarios. For instance, I successfully used ECMO to support a patient with severe primary graft dysfunction following a heart-lung transplant, allowing the transplanted organs time to recover and ultimately preventing the need for re-transplantation. The decision to use ECMO is complex, carefully weighing the risks and benefits based on patient factors, severity of organ failure, and the availability of resources.
Think of ECMO as a temporary bridge, supporting the patient until the transplanted organs can fully take over their functions. It’s a powerful tool, but we only deploy it when absolutely necessary.
Q 17. Explain your approach to ventilator management in post-transplant patients.
Ventilator management in post-heart-lung transplant patients is critical due to their vulnerable respiratory status. Our approach focuses on weaning the patient from the ventilator as quickly and safely as possible. We begin with a lung-protective ventilation strategy, using low tidal volumes and moderate positive end-expiratory pressure (PEEP) to minimize lung injury. We closely monitor oxygenation, carbon dioxide levels, and respiratory mechanics using blood gas analysis and respiratory parameters. We tailor the ventilator settings based on the patient’s individual response, gradually reducing ventilator support as they demonstrate improved respiratory function. This often involves a combination of spontaneous breathing trials and synchronized intermittent mandatory ventilation (SIMV). We actively look for signs of weaning readiness, such as adequate oxygenation, reduced work of breathing, and stable hemodynamics. Weaning is a progressive process, and setbacks can occur; adjustments are made as needed based on the patient’s response.
It’s like carefully teaching a bird to fly—we gradually reduce the support until it can fly on its own. We have to monitor closely and be ready to adjust our support if the bird struggles.
Q 18. Describe your experience with the use of advanced imaging techniques (e.g., echocardiography, CT scans) in the evaluation and management of heart-lung transplant patients.
Advanced imaging plays a vital role throughout the heart-lung transplant journey. Echocardiography is fundamental, allowing us to assess cardiac function, valve function, and the presence of rejection or other complications. Transthoracic echocardiography (TTE) is performed routinely, while transesophageal echocardiography (TEE) provides a more detailed view when necessary. Computed tomography (CT) scans are valuable for evaluating the lungs, identifying pulmonary complications like infection or rejection, and assessing vascular structures. Magnetic resonance imaging (MRI) is occasionally used for more detailed evaluation of cardiac structures and function. For example, early detection of rejection using these imaging techniques is crucial for initiating timely treatment and improving patient outcomes. A patient presenting with reduced cardiac output after transplant might undergo a TTE to evaluate for issues like pericardial effusion or rejection. A suspected pulmonary infection might lead to a CT scan to confirm the diagnosis and guide treatment.
These imaging techniques are our eyes into the heart and lungs. They provide detailed pictures that guide our decisions and allow for early detection of potential problems.
Q 19. How do you assess the effectiveness of immunosuppression?
Assessing immunosuppression effectiveness is crucial to prevent rejection while minimizing the risk of infection and other complications. We use a multi-pronged approach. Blood tests measure blood levels of immunosuppressant drugs (therapeutic drug monitoring), ensuring appropriate levels are maintained. Biopsies of the transplanted organs are performed periodically to assess for signs of rejection, both cellular and humoral. We also closely monitor the patient for clinical signs of rejection such as fever, shortness of breath, or decreased exercise tolerance. Other lab tests include complete blood counts (CBC) and liver and kidney function tests, as immunosuppressants can affect these organs. We regularly adjust the immunosuppression regimen based on these assessments, striving to maintain a balance between effective immunosuppression and minimizing side effects.
Imagine a tightrope walker—we need to keep them balanced between two dangers: rejection (falling to one side) and infection/toxicity (falling to the other). We constantly monitor and adjust the safety net (immunosuppression) to keep them stable.
Q 20. What are the ethical considerations in heart-lung transplantation?
Heart-lung transplantation raises complex ethical considerations. Organ allocation is a major one, requiring fair and equitable distribution of scarce resources. This involves careful consideration of medical urgency, patient prognosis, and factors like geographic location and blood type. Informed consent is another critical aspect, ensuring the patient fully understands the risks, benefits, and alternatives to transplantation. Transparency and open communication with patients and their families are essential. Furthermore, ongoing ethical dilemmas might arise concerning treatment decisions, resource allocation, and quality of life issues as patients navigate the post-transplant journey. The ethical principles of beneficence (acting in the patient’s best interest), non-maleficence (avoiding harm), autonomy (respecting patient choices), and justice (fair resource allocation) guide our decision-making process.
It’s a delicate balancing act, ensuring that resources are used fairly and that each patient’s wishes and well-being are prioritized.
Q 21. Discuss the importance of psychosocial support for heart-lung transplant recipients.
Psychosocial support is integral to the successful outcome of heart-lung transplantation. The procedure is physically and emotionally demanding, often leaving patients with anxieties about rejection, medications, and the long-term impact on their lives. We provide comprehensive support through a multidisciplinary team including psychologists, social workers, and nurses specializing in transplantation. This support encompasses emotional counseling to address anxiety and depression, practical assistance with medication management and lifestyle adjustments, and facilitating social connections with other transplant recipients. Support groups offer a vital platform for sharing experiences and fostering mutual support. The goal is to improve patient adherence to the treatment plan, enhance quality of life, and increase the likelihood of long-term success. For example, providing access to support groups where transplant recipients can share their experiences and learn coping mechanisms can significantly reduce stress and improve their adjustment to the post-transplant life.
Think of it as building a strong foundation of support to help the patient thrive, not just survive, after transplantation. Emotional well-being is just as important as physical recovery.
Q 22. Explain the role of rehabilitation in heart-lung transplant recovery.
Rehabilitation after a heart-lung transplant is absolutely crucial for a successful recovery. It’s not just about getting stronger physically; it’s about restoring a patient’s overall quality of life. Think of it like this: the transplant is the engine, but rehabilitation is the fuel and the driver that gets the engine running smoothly and efficiently.
Physical Therapy: This focuses on building strength, improving endurance, and regaining mobility. Patients often start with simple exercises and gradually progress to more challenging activities. For example, a patient might begin with walking short distances and eventually work up to climbing stairs or even light jogging.
Occupational Therapy: This helps patients regain the skills needed for daily living, such as dressing, bathing, and preparing meals. It focuses on adapting tasks to accommodate any physical limitations and promoting independence.
Respiratory Therapy: This is critical because the new lungs need to function optimally. Techniques like deep breathing exercises, airway clearance, and breathing treatments are employed to improve lung function and prevent infections. We often use incentive spirometers to help patients take deep breaths and expand their lungs.
Cardiac Rehabilitation: This component focuses on improving the heart’s function and overall cardiovascular health through supervised exercise and education about heart-healthy lifestyle changes, such as diet and stress management. This is key, as the transplanted heart needs to be supported by a healthy lifestyle.
Psychological Support: The emotional and psychological impact of a heart-lung transplant is significant. Counseling and support groups are vital for patients and their families to cope with the stress, anxieties, and adjustments required after surgery.
The length and intensity of rehabilitation vary depending on individual needs and responses to treatment. However, it’s a continuous process that extends beyond the initial hospital stay and involves ongoing monitoring and adjustment of the rehabilitation plan as the patient progresses.
Q 23. How do you manage the financial aspects of heart-lung transplantation for patients?
Managing the financial aspects of heart-lung transplantation is a significant challenge. The costs associated with the procedure, including surgery, hospitalization, medications (immunosuppressants are lifelong and expensive!), and ongoing care, are substantial. We work closely with patients and their families to navigate this complex landscape.
Insurance Coverage: We explore all available insurance options, working with the patient’s insurance company to ensure coverage for the transplant and subsequent care. This often involves extensive pre-authorization processes.
Financial Assistance Programs: We help patients identify and apply for financial assistance programs offered by hospitals, pharmaceutical companies, and charitable organizations. These programs can significantly reduce out-of-pocket expenses.
Fundraising Initiatives: In some cases, we may support the patient’s efforts in organizing fundraising initiatives to help cover costs.
Social Work Support: Our social workers play a vital role in connecting patients and families with resources and navigating the complexities of healthcare financing. They offer guidance on budgeting, navigating insurance claims, and exploring financial assistance options.
Open and honest communication with the patient and family about the financial implications is crucial from the outset. Early identification of potential financial barriers allows us to develop a comprehensive strategy to minimize financial stress and ensure patients receive the necessary care.
Q 24. Describe your experience with various types of heart-lung transplant rejection.
Heart-lung transplant rejection is a serious complication that can occur at any time after surgery. It happens when the recipient’s immune system attacks the transplanted organs. There are different types, broadly categorized by timing:
Hyperacute Rejection: This is rare and occurs within minutes to hours of transplantation. It’s usually due to pre-existing antibodies against the donor organs. It’s a medical emergency requiring immediate intervention, including removal of the transplanted organs.
Acute Rejection: This is more common and can occur within the first few months or even years post-transplant. It presents with symptoms such as fever, shortness of breath, decreased exercise tolerance, and changes in lung function or heart performance. Treatment typically involves high-dose corticosteroids and other immunosuppressant medications.
Chronic Rejection: This is a gradual process occurring over months or years, leading to progressive damage to the transplanted organs. This manifests as slow deterioration of function with subtle symptoms, making early detection challenging. Treatment options are limited, and the outcome may be less favorable.
The diagnosis of rejection often involves a combination of clinical symptoms, blood tests (to measure organ-specific enzymes and immune markers), and biopsy of the heart and/or lungs. Early recognition and prompt treatment are vital to prevent irreversible damage and improve long-term outcomes. I’ve seen many cases where early intervention has been lifesaving, emphasizing the importance of vigilance and quick response to any concerning changes in the patient’s condition.
Q 25. What is your understanding of the latest advancements in heart-lung transplantation?
The field of heart-lung transplantation is constantly evolving. Recent advancements focus on improving patient outcomes and minimizing complications.
Improved Immunosuppression Protocols: We are constantly refining immunosuppression strategies to reduce rejection risk while minimizing side effects. New medications with fewer adverse effects are constantly emerging, and personalized medication regimes are becoming more common based on genetic factors.
Minimally Invasive Surgical Techniques: The development of minimally invasive surgical techniques aims to reduce trauma, blood loss, and recovery time. This reduces the risk of complications and allows for quicker rehabilitation.
Improved Organ Preservation Techniques: Advances in organ preservation techniques have extended the time organs can be stored, increasing the availability of suitable donor organs and expanding the pool of potential recipients.
Bioengineering and Regenerative Medicine: Research into bioengineering and regenerative medicine holds immense potential to create functional replacement tissues and organs, potentially addressing the shortage of donor organs. Though still in its early stages, this area holds exciting possibilities for the future of heart-lung transplantation.
These advancements are continually improving the success rates and long-term survival of heart-lung transplant recipients, enhancing quality of life and offering hope to those in need of this life-saving procedure.
Q 26. Describe your experience with managing a patient experiencing primary graft dysfunction.
Primary graft dysfunction (PGD) is a devastating complication that can occur immediately following a heart-lung transplant. It involves the failure of the transplanted organs to function normally in the early post-transplant period. It’s essentially a situation where the organs aren’t performing as they should even though there’s no evidence of rejection.
Managing PGD requires aggressive, multifaceted treatment. It’s a critical situation that requires intensive care and close monitoring. We typically utilize the following approaches:
Mechanical Support: This might involve the use of an extracorporeal membrane oxygenation (ECMO) machine to temporarily support the heart and lungs while the transplanted organs try to recover. ECMO acts as an external heart and lung, providing essential support until the organs regain function.
Inotropic and Vasopressor Support: Medications that strengthen the heart’s contractions and raise blood pressure are administered to maintain adequate circulation.
Respiratory Support: This might involve mechanical ventilation (a ventilator to assist breathing) and other respiratory treatments to improve oxygenation and gas exchange.
Immunosuppression Optimization: While PGD is not a rejection, careful management of immunosuppression is crucial to help minimize further organ damage. We frequently adjust medications based on the patient’s response.
Close Monitoring and Vigilance: Continuous monitoring of vital signs, blood tests, and imaging studies is crucial to assess the patient’s condition and the effectiveness of the interventions.
The outcome of PGD is highly variable. Some patients recover completely, while others may experience long-term complications or even death. The challenge lies in identifying early warning signs and aggressively treating the underlying causes of organ dysfunction to give patients the best chance of survival.
Q 27. What is your experience with the use of bioprosthetic versus mechanical valves in heart-lung transplantation?
The choice between bioprosthetic and mechanical valves in heart-lung transplantation depends on several factors, including the patient’s age, overall health, and the specific needs of the recipient. Both have advantages and disadvantages.
Bioprosthetic Valves: These valves are made from animal tissues (usually porcine or bovine). They don’t require lifelong anticoagulation (blood thinners) medication, which reduces the risk of bleeding complications. However, they have a limited lifespan (typically 10-15 years) and may require replacement later on. This is a significant factor, especially in younger patients.
Mechanical Valves: These valves are made from durable materials like metal and plastic. They have a much longer lifespan, potentially lasting a lifetime. However, they require lifelong anticoagulation therapy to prevent blood clots from forming on the valve surface, increasing the risk of bleeding complications. This is a significant consideration, as uncontrolled bleeding could be a life-threatening event.
The decision is made on a case-by-case basis. For younger patients with a longer life expectancy, a mechanical valve might be preferable due to its durability, even with the need for lifelong anticoagulation. Older patients, or those with a higher bleeding risk, might be better suited for a bioprosthetic valve, despite its shorter lifespan, to minimize the risks associated with anticoagulation therapy. We always involve the patient and family in this decision-making process, making sure they fully understand the pros and cons of each option and choosing the option that best aligns with their individual circumstances and preferences.
Key Topics to Learn for Heart-Lung Transplantation Interview
- Pre-transplant Evaluation: Understanding the selection criteria for candidates, including physiological assessment, psychological evaluation, and social support systems. Practical application: Analyzing patient data to determine suitability for transplantation.
- Surgical Techniques: Familiarize yourself with the intricacies of the procedure, including various surgical approaches and the management of potential intraoperative complications. Practical application: Troubleshooting potential surgical challenges and proposing solutions.
- Immunosuppression Strategies: Mastering the principles of immunosuppression, including the selection of appropriate agents, monitoring of drug levels, and management of adverse effects. Practical application: Developing personalized immunosuppression protocols for individual patients.
- Post-transplant Management: Comprehensive understanding of post-operative care, including monitoring for rejection, infection management, and long-term follow-up. Practical application: Developing a plan to prevent and manage common post-transplant complications.
- Organ Allocation and Ethics: Grasping the ethical considerations and allocation processes involved in heart-lung transplantation. Practical application: Justifying the selection of recipients based on established criteria.
- Advanced Imaging Techniques: Understanding the role of various imaging modalities (CT, MRI, etc.) in assessing organ viability and diagnosing post-transplant complications. Practical application: Interpreting imaging results to inform clinical decision-making.
- Disease Management (e.g., Pulmonary Hypertension, Congenital Heart Disease): Deep dive into the specific diseases necessitating heart-lung transplantation and their impact on the surgical approach and post-transplant care. Practical application: Discussing specific disease characteristics in a case study scenario.
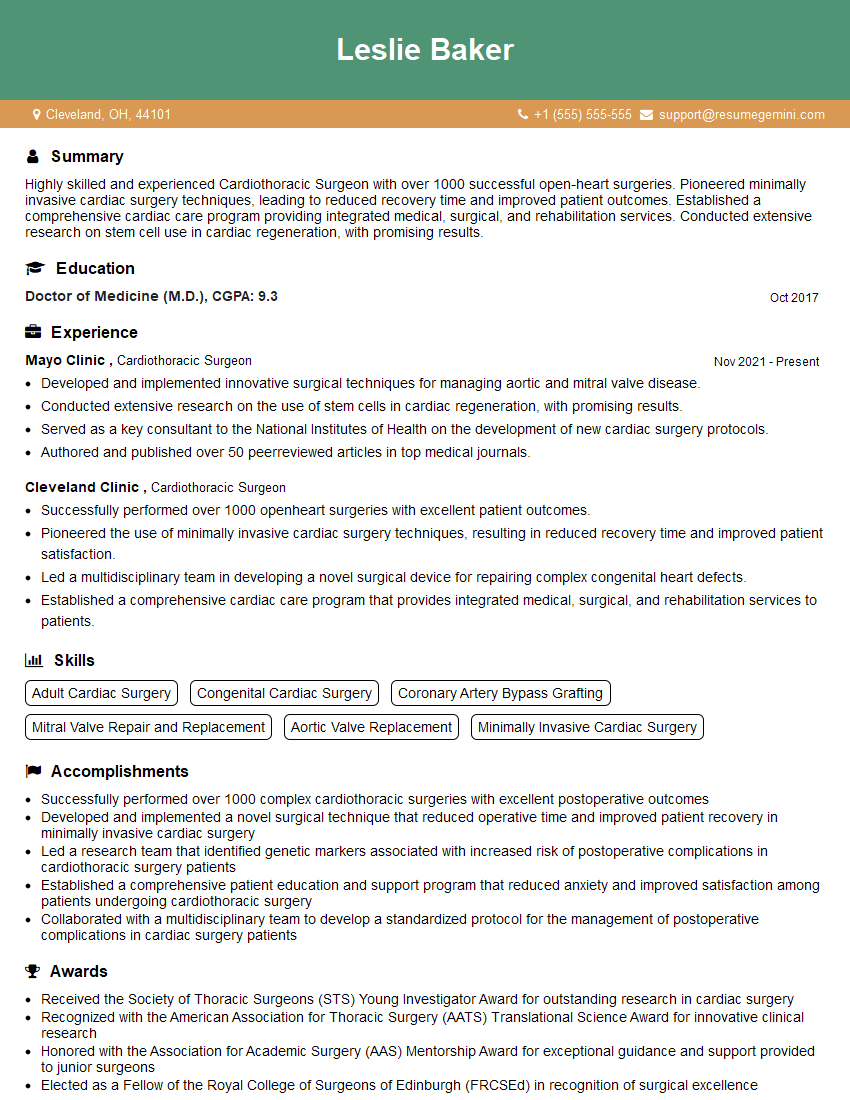
Next Steps
Mastering the complexities of Heart-Lung Transplantation significantly enhances your career prospects within the field of cardiothoracic surgery and organ transplantation. A strong understanding of these concepts positions you for leadership roles and opens doors to exciting research opportunities. To further strengthen your application, creating an ATS-friendly resume is crucial for maximizing your chances of securing an interview. ResumeGemini is a trusted resource that can help you build a professional and impactful resume tailored to the specifics of your experience. Examples of resumes tailored to Heart-Lung Transplantation are available to guide you.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
To the interviewgemini.com Webmaster.
Very helpful and content specific questions to help prepare me for my interview!
Thank you
To the interviewgemini.com Webmaster.
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.