Every successful interview starts with knowing what to expect. In this blog, we’ll take you through the top Patient Advocacy and Education interview questions, breaking them down with expert tips to help you deliver impactful answers. Step into your next interview fully prepared and ready to succeed.
Questions Asked in Patient Advocacy and Education Interview
Q 1. Describe your experience developing and delivering patient education materials.
Developing patient education materials requires a multifaceted approach, prioritizing clarity, accessibility, and cultural sensitivity. I begin by thoroughly understanding the target audience’s health literacy level and learning styles. This involves analyzing the specific medical information needing dissemination and identifying any potential barriers to comprehension, such as complex terminology or low literacy levels.
My process typically involves:
- Needs Assessment: Identifying the key information patients need to know about their condition, treatment plan, and self-management strategies.
- Content Development: Writing clear, concise, and engaging materials using plain language, avoiding jargon. I often incorporate visuals such as diagrams, illustrations, and videos to improve comprehension.
- Material Design and Formatting: Using an accessible design that is easy to read and understand, considering font size, spacing, and layout. I ensure the materials are available in multiple formats (print, digital, audio) to cater to diverse learning preferences and disabilities.
- Pilot Testing: Testing the materials with a representative sample of the target audience to identify areas for improvement and ensure effectiveness before widespread distribution. I gather feedback on clarity, comprehension, and engagement.
- Distribution and Evaluation: Utilizing various channels for distribution, including the clinic, online platforms, and community outreach programs. Post-distribution evaluations help assess the impact of the materials on patient knowledge and behavior change.
For example, I once developed a series of short videos explaining diabetes management techniques, using simple language and visual aids. The videos proved highly effective, leading to a significant improvement in patient blood glucose control.
Q 2. How do you assess a patient’s health literacy level?
Assessing health literacy involves understanding a patient’s ability to understand and act on health information. It’s not simply about reading ability, but also encompasses their comprehension, numeracy skills, and ability to apply that knowledge to their own health.
I use a combination of methods:
- Informal Assessment: During conversations, I observe patients’ comprehension of medical terms and instructions. I gauge their ability to explain back their treatment plan in their own words.
- Validated Tools: Using standardized tools like the REALM (Rapid Estimate of Adult Literacy in Medicine) or the TOFHLA (Test of Functional Health Literacy in Adults) to objectively measure health literacy levels.
- Patient Self-Report: Asking patients about their comfort level with health information and their preferred learning methods. This provides insights into their confidence and learning preferences.
For instance, if a patient struggles to understand medication instructions, it might indicate a low health literacy level. I would then adjust my communication accordingly, using simpler language, visual aids, and repeat explanations until comprehension is confirmed.
Q 3. Explain your approach to addressing patient concerns and complaints.
Addressing patient concerns and complaints requires empathy, active listening, and a systematic approach. My approach centers around validating the patient’s feelings, investigating the issue thoroughly, and collaboratively finding a resolution.
I follow these steps:
- Active Listening: Allowing patients to fully express their concerns without interruption, demonstrating empathy and understanding.
- Clarification: Asking clarifying questions to fully grasp the nature and extent of the concern.
- Investigation: Gathering information from relevant sources, including medical records and healthcare providers, to understand the situation objectively.
- Collaboration: Working with the patient and healthcare team to develop a mutually agreeable solution. This may involve advocating for the patient’s needs with other members of the healthcare team.
- Follow-up: Checking in with the patient after the resolution to ensure they are satisfied with the outcome.
For example, if a patient complains about a medication side effect, I thoroughly document the complaint, discuss it with the prescribing physician, and explore alternative treatment options with the patient’s involvement.
Q 4. What strategies do you use to empower patients to actively participate in their care?
Empowering patients involves equipping them with the knowledge and skills to actively participate in their healthcare decisions. This means shifting from a passive recipient of care to an active partner in the process.
My strategies include:
- Shared Decision-Making: Involving patients in treatment plan discussions, explaining the risks and benefits of various options, and respecting their preferences.
- Skill-Building: Teaching patients self-management skills, such as medication management, symptom monitoring, and lifestyle modifications. I use practical demonstrations and role-playing to enhance understanding.
- Resource Provision: Connecting patients to reliable resources such as support groups, online educational materials, and community health programs.
- Advocacy: Championing patients’ needs and rights, ensuring they have access to appropriate care and information.
- Positive Reinforcement: Recognizing and celebrating patients’ achievements in managing their health, boosting their confidence and motivation.
For instance, I might teach a patient with asthma how to use a peak flow meter and interpret the readings, giving them greater control over their condition.
Q 5. How do you navigate conflicting information or viewpoints among healthcare providers and patients?
Navigating conflicting information requires a careful, neutral approach that respects all viewpoints while prioritizing patient safety and well-being.
My approach is to:
- Facilitate Communication: Creating a safe space for open dialogue between the patient, healthcare providers, and family members.
- Clarify Discrepancies: Identifying the sources of conflicting information and assessing their reliability and validity.
- Present Evidence-Based Information: Sharing unbiased, research-based information to help clarify misunderstandings.
- Promote Shared Decision-Making: Guiding the patient to weigh the available information and make informed decisions aligned with their values and preferences.
- Document Everything: Maintaining a thorough record of discussions, decisions, and any actions taken to ensure accountability and transparency.
For example, if a patient receives conflicting advice from different specialists, I would facilitate a meeting between them, help the patient understand the different perspectives, and help them make an informed decision based on their personal needs and values.
Q 6. Describe a situation where you had to advocate for a patient’s rights.
I once advocated for a patient who was repeatedly denied access to a necessary medication due to insurance coverage issues. The patient had a chronic condition requiring this medication for survival, and the denial was causing significant distress and health deterioration.
My actions involved:
- Gathering Information: I meticulously collected all relevant medical records, insurance documents, and treatment plans to build a strong case.
- Communicating with Insurance Providers: I contacted the insurance company, explaining the medical necessity of the medication and outlining the potential consequences of denial. I used clear, concise language and provided substantial medical evidence to support my claim.
- Navigating Appeals Process: When the initial appeal was rejected, I assisted the patient in filing a formal appeal, providing further documentation and evidence.
- Seeking External Support: I contacted patient advocacy organizations for assistance in navigating the complex insurance system.
Ultimately, through persistent advocacy and collaboration with various stakeholders, we were able to secure coverage for the necessary medication, significantly improving the patient’s quality of life.
Q 7. How do you handle challenging or emotionally charged interactions with patients and families?
Handling challenging or emotionally charged interactions requires empathy, patience, and strong communication skills. It’s crucial to manage both the emotional and informational aspects of the interaction effectively.
My strategies include:
- Empathy and Validation: Acknowledging and validating the patient’s or family’s emotions, demonstrating understanding and support.
- Active Listening: Paying close attention to both verbal and non-verbal cues, allowing the individual to fully express their feelings.
- Clear and Calm Communication: Speaking in a clear, calm, and reassuring tone, avoiding jargon and complex medical terminology.
- Setting Boundaries: Establishing clear professional boundaries while maintaining a compassionate and supportive approach.
- Seeking Support: Knowing when to seek support from other members of the healthcare team, such as social workers or chaplains, to provide comprehensive care.
For instance, when a patient is grieving a loss or facing a difficult diagnosis, creating a safe space for their emotions and providing emotional support is as critical as providing medical information. I strive to connect patients with the appropriate resources to help them cope emotionally.
Q 8. How familiar are you with HIPAA regulations and patient confidentiality?
HIPAA (Health Insurance Portability and Accountability Act) regulations are fundamental to my practice. I’m intimately familiar with the Privacy Rule, which protects the confidentiality, integrity, and availability of Protected Health Information (PHI). This includes everything from a patient’s medical history and diagnoses to their insurance details and even their appointment times. My understanding encompasses the permitted disclosures of PHI, the requirements for obtaining authorization, and the necessary safeguards to prevent breaches. For example, I understand that PHI can be disclosed without authorization for treatment, payment, and healthcare operations, but even within these exceptions, strict limitations apply. I am meticulous about following HIPAA guidelines to ensure patient privacy, which includes secure data handling, password protection, and understanding the implications of any potential data breaches. I regularly participate in HIPAA compliance training to stay updated on the latest regulations and best practices.
Q 9. Describe your experience working with diverse patient populations.
I have extensive experience working with diverse patient populations, spanning various age groups, socioeconomic backgrounds, ethnicities, and levels of health literacy. This experience has equipped me with a highly adaptable approach to patient advocacy and education. For instance, I’ve worked with elderly patients experiencing cognitive decline, requiring simplified explanations and visual aids. Conversely, I’ve also worked with younger patients who preferred interactive digital tools and more informal communication styles. My work with non-English speaking patients often involved utilizing translation services and culturally sensitive materials. I understand that cultural differences can significantly impact health beliefs and healthcare decisions. This experience has instilled in me a deep respect for individual differences and the importance of tailoring my approach to each individual’s specific needs and preferences.
Q 10. How do you adapt your communication style to meet individual patient needs?
Adapting my communication style is crucial. I begin by actively listening to understand the patient’s communication preferences, health literacy level, and any cultural or personal factors that might influence their understanding. For patients with limited health literacy, I use plain language, avoiding medical jargon. I often utilize visual aids like diagrams or charts. With patients who are anxious or apprehensive, I create a calm and reassuring environment, focusing on empathy and understanding. I might adjust my tone to be more formal or informal based on the patient’s preference. For those who prefer a more active role in their healthcare, I encourage questions and participation. For instance, with a patient struggling with a complex treatment plan, I might break down information into smaller, manageable chunks, checking for understanding at each step. This individualized approach ensures that patients feel heard, understood, and empowered to participate in their care.
Q 11. What resources do you utilize to stay current on best practices in patient advocacy and education?
Staying current requires a multi-faceted approach. I subscribe to professional journals like the Journal of Patient Education and Counseling and attend conferences and workshops organized by organizations like the Patient Advocate Foundation. I actively participate in online communities and forums focused on patient advocacy and education, exchanging best practices and insights with other professionals. I also track new legislation and guidelines related to patient rights and healthcare access. Websites of organizations like the Centers for Disease Control and Prevention (CDC) and the National Institutes of Health (NIH) are valuable resources for the latest research and evidence-based practices. Staying updated is essential to ensure I’m delivering the most effective and relevant support to my patients.
Q 12. How do you measure the effectiveness of your patient education programs?
Measuring effectiveness involves both quantitative and qualitative methods. Quantitative measures might include pre- and post-education assessments to gauge improvement in knowledge and understanding of a specific topic. For example, a pre- and post-test on diabetes management could reveal the impact of an educational program. We also track patient satisfaction through surveys or feedback forms. Qualitative measures involve gathering feedback through focus groups or individual interviews. This provides valuable insights into the patients’ experience and helps identify areas for improvement. For example, we might analyze feedback to assess the clarity of our materials, the effectiveness of our teaching methods, and the overall accessibility of our programs. By integrating both quantitative and qualitative data, we gain a comprehensive understanding of the program’s effectiveness and make necessary adjustments to maximize its impact.
Q 13. Describe your experience with electronic health records (EHRs) and patient portals.
I am proficient in using electronic health records (EHRs) and patient portals. EHRs provide a comprehensive view of a patient’s medical history, allowing me to tailor my advocacy efforts based on their specific circumstances. I understand how to navigate various EHR systems to access relevant information while strictly adhering to HIPAA regulations. Patient portals are invaluable tools for enhancing communication and engagement. I guide patients on how to access their health information through the portal, enabling them to actively participate in managing their health. I use the portal to securely exchange messages with patients, schedule appointments, and send important educational materials, ensuring seamless and efficient communication.
Q 14. How do you utilize technology to enhance patient engagement and communication?
Technology significantly enhances patient engagement. I use telehealth platforms for virtual consultations, making healthcare more accessible, particularly for patients with mobility issues or those living in remote areas. I create and share educational videos and infographics through platforms like YouTube or social media, ensuring information is easily accessible and engaging. I utilize email and text messaging to provide timely reminders, send educational materials, and facilitate communication between appointments. Secure messaging systems within patient portals also enable private and confidential communication. I even explore the use of mobile apps that support specific health conditions, enhancing patient self-management skills. The strategic use of technology allows me to reach a wider audience and offer personalized, convenient support.
Q 15. What is your experience with developing and implementing patient education programs?
Developing and implementing effective patient education programs requires a multifaceted approach. It starts with a thorough needs assessment to understand the specific knowledge gaps and learning styles of the target patient population. This might involve surveys, interviews, or focus groups. Then, I design programs using evidence-based practices, ensuring the information is accurate, accessible, and culturally appropriate. This often involves utilizing diverse formats like interactive workshops, printed materials, videos, and online resources, catering to different learning preferences.
For example, in a program addressing diabetes management, I might develop a series of short videos demonstrating proper insulin injection techniques, alongside a workbook with practical exercises and recipes for healthy eating. Following implementation, rigorous evaluation is crucial. This includes tracking attendance, assessing knowledge gains through pre- and post-tests, and gathering feedback through surveys or interviews to measure the program’s impact and make necessary adjustments.
I’ve successfully implemented numerous programs, including one for heart failure patients that reduced hospital readmissions by 15% through improved self-management skills. Another example involved creating a culturally sensitive program in Spanish for a predominantly Hispanic community, resulting in significantly improved medication adherence rates.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you identify and address health disparities within patient populations?
Addressing health disparities requires a deep understanding of the social determinants of health – factors like socioeconomic status, access to healthcare, education, and cultural beliefs that significantly impact health outcomes. I begin by identifying these disparities within a given patient population through data analysis (e.g., reviewing hospital discharge data, conducting community health assessments) and direct interaction with patients. For example, noticing a disproportionately high rate of uncontrolled hypertension among a specific ethnic group signals a need for targeted intervention.
Then, I design and implement culturally appropriate and accessible interventions to address the root causes of these disparities. This might involve collaborating with community organizations to provide transportation to appointments, translating materials into multiple languages, or offering education sessions in community centers. For instance, I worked on a project to increase colorectal cancer screening rates in a low-income community by partnering with local churches and offering free screening events. Crucially, patient engagement and empowerment are key – working *with* the community, rather than *for* it, ensures sustainability and effectiveness.
Q 17. Describe your experience in collaborating with interdisciplinary healthcare teams.
Effective patient advocacy necessitates seamless collaboration with interdisciplinary healthcare teams. I believe in a collaborative, communicative approach, actively participating in care team meetings, sharing relevant patient information, and advocating for patient needs. My experience includes working with physicians, nurses, social workers, pharmacists, and therapists. For instance, I collaborated with a physician to develop a shared decision-making tool for patients facing complex treatment choices. This involved incorporating the patient’s values and preferences into the treatment plan.
I also work closely with social workers to address social determinants of health that may impact treatment adherence. Effective communication is key; I use clear and concise language, ensuring everyone understands the patient’s needs and treatment goals. Regularly updating the team on a patient’s progress or challenges is crucial for maintaining cohesive and effective care.
Q 18. How do you build trust and rapport with patients and their families?
Building trust and rapport is foundational to effective patient advocacy. It starts with active listening – truly hearing the patient’s concerns and validating their feelings. I prioritize empathy and demonstrate genuine care for their well-being. This means making eye contact, using respectful and inclusive language, and taking the time to understand their individual circumstances.
I also build trust by being transparent and honest, explaining medical information in clear, understandable terms, and empowering patients to participate in their care decisions. A simple act like remembering details about a patient’s life or family during subsequent visits shows genuine interest and strengthens the relationship. For instance, remembering a patient’s grandchild’s name or asking about a recent family event can make a significant difference in fostering trust.
Q 19. How do you handle situations where a patient refuses treatment or medical advice?
When a patient refuses treatment or medical advice, my approach is to first understand the reason behind their refusal. This involves open and non-judgmental conversation, exploring their concerns, fears, and beliefs. It’s important to validate their feelings, even if I disagree with their decision. For example, a patient might refuse chemotherapy due to fear of side effects. Instead of pressuring them, I would explore their concerns and explain the benefits and risks of treatment clearly.
I would also involve other members of the healthcare team, such as a counselor or social worker, to address potential emotional or psychological barriers. Ultimately, respecting patient autonomy is paramount. While I can provide information and education, I cannot force a patient to accept treatment against their will. However, I can help them explore alternative options or provide resources that might support their decision.
Q 20. What is your experience with crisis intervention or support for patients and families?
My experience with crisis intervention includes supporting patients and families during difficult times, such as receiving a serious diagnosis, experiencing a medical emergency, or coping with loss. This involves providing emotional support, practical assistance, and connecting them with necessary resources. For example, if a family is struggling to cope with a loved one’s terminal illness, I might help them access hospice care, grief counseling, or support groups.
I’m trained in crisis intervention techniques, including active listening, de-escalation, and providing immediate emotional support. This may include helping patients and families process their emotions, develop coping mechanisms, and access mental health resources. In urgent situations, I work closely with other members of the healthcare team to ensure the patient’s immediate safety and well-being. Collaboration with social workers, chaplains, and mental health professionals is vital in these scenarios.
Q 21. How do you prioritize tasks and manage your time effectively in a fast-paced healthcare setting?
Effective time management in a fast-paced healthcare setting relies on organization and prioritization. I utilize tools like electronic health records (EHRs) and task management software to track my workload, schedule appointments, and set reminders. I prioritize tasks based on urgency and importance, focusing on time-sensitive issues and those with the greatest impact on patient well-being. This might involve using a prioritization matrix, categorizing tasks as urgent/important, important/not urgent, etc.
I also practice efficient communication, using concise language and minimizing unnecessary meetings. Delegation is also crucial when appropriate; I’m able to assign tasks to other team members when possible to maximize efficiency. Regularly reviewing my schedule and adjusting it as needed helps maintain balance and prevents feeling overwhelmed. Regular breaks and self-care practices are also essential for preventing burnout and maintaining effectiveness.
Q 22. Describe your experience with cultural competency and sensitivity in patient care.
Cultural competency in patient care involves understanding and respecting the diverse cultural backgrounds, beliefs, and practices of patients. It’s about recognizing that healthcare isn’t a one-size-fits-all approach. My experience includes extensive training in health disparities, implicit bias, and cross-cultural communication. I’ve worked with patients from various ethnicities, religious backgrounds, and socioeconomic statuses, learning to adapt my communication style and approach to effectively meet their individual needs.
For example, I worked with a patient from a community where direct eye contact is considered disrespectful. Understanding this cultural nuance allowed me to build rapport by subtly adjusting my communication style. In another instance, I had to work closely with a family who had strong spiritual beliefs that influenced their approach to healthcare decisions. By actively listening to their concerns and integrating their beliefs into the care plan, we were able to achieve a much better outcome.
This involves not just understanding different cultures but also being self-aware of my own biases and actively working to overcome them. I regularly participate in continuing education focusing on cultural competency to maintain and expand my knowledge in this crucial area of patient care.
Q 23. How familiar are you with different learning styles and teaching methods?
Understanding diverse learning styles is paramount in patient education. People learn differently; some are visual learners, preferring diagrams and charts, while others are auditory learners, responding better to verbal explanations and discussions. Some are kinesthetic learners, who learn best through hands-on activities.
My approach involves utilizing a variety of teaching methods to cater to these different styles. For instance, I use visual aids like infographics and videos for visual learners, provide detailed verbal instructions and engage in open discussions for auditory learners, and incorporate interactive exercises or demonstrations for kinesthetic learners. I also employ a combination of techniques, ensuring that information is presented in multiple formats to maximize comprehension and retention.
Adapting to individual learning needs might mean simplifying complex medical jargon, using analogies and real-life examples to make concepts easier to grasp, or providing written materials to supplement verbal explanations. Regularly assessing a patient’s understanding and providing tailored feedback is critical to effective education.
Q 24. Describe a time you had to resolve a conflict between a patient and a healthcare provider.
I once had to mediate a conflict between a patient who felt unheard and a physician who felt frustrated by the patient’s lack of adherence to the treatment plan. The patient, an elderly woman with limited health literacy, felt overwhelmed by the physician’s explanations and didn’t fully understand her medication regimen. The physician, in turn, felt the patient wasn’t taking her health seriously.
My approach involved active listening to both parties, acknowledging their perspectives and concerns without judgment. I helped the patient re-explain her concerns, clarifying the areas of misunderstanding. I then worked with the physician to simplify the explanation of the treatment plan, incorporating visual aids and written instructions. We also discussed alternative communication strategies to ensure the patient felt comfortable expressing her concerns and asking questions.
Ultimately, we developed a collaborative care plan that addressed both the patient’s concerns and the physician’s goals. This involved regular check-ins, a simplified medication schedule, and arranging for translation services to ensure clear communication. The resolution demonstrated the importance of clear communication, empathy, and collaborative problem-solving in addressing patient-provider conflicts.
Q 25. How do you utilize data and analytics to improve patient outcomes and satisfaction?
Data and analytics play a vital role in improving patient outcomes and satisfaction. By tracking key metrics such as patient adherence to treatment plans, readmission rates, and patient satisfaction scores, we can identify areas needing improvement. For example, we might analyze data to determine if certain patient populations are experiencing higher readmission rates, which could indicate a need for improved discharge planning or follow-up care.
Analyzing patient feedback surveys can reveal areas where patients feel underserved, such as inadequate communication or lack of emotional support. This data allows us to target interventions, develop more effective education programs, and tailor services to meet specific patient needs.
I use this data to develop evidence-based strategies for improving care. This involves using statistical software to analyze trends, identifying correlations between factors affecting patient outcomes, and using this insight to guide decision-making. For instance, if data shows a correlation between poor medication adherence and lack of access to transportation, then implementing a medication delivery service might significantly improve outcomes.
Q 26. How do you identify and address barriers to patient access and care?
Identifying barriers to patient access and care requires a multifaceted approach. This includes understanding socioeconomic factors like insurance coverage, transportation, and language barriers. It also involves recognizing healthcare system-related issues, such as long wait times, lack of specialized services, or limited provider availability in certain geographic areas.
My strategy for addressing these barriers involves actively collaborating with community organizations, healthcare providers, and policymakers. This might involve connecting patients with financial assistance programs, arranging transportation, or providing translation services. I also advocate for policy changes that improve access to care, such as expanding insurance coverage or increasing funding for community health clinics.
For instance, I helped implement a program that provided free transportation to patients who lacked reliable transportation to their appointments. This simple intervention significantly improved appointment attendance and overall treatment outcomes. Furthermore, actively engaging with policymakers to discuss the unique needs of underserved communities and proposing solutions is crucial for systematic change.
Q 27. How do you ensure the accuracy and reliability of patient information?
Ensuring the accuracy and reliability of patient information is paramount. This involves adhering to strict privacy regulations like HIPAA, utilizing secure electronic health record systems, and employing double-checking procedures to ensure data entry accuracy.
I regularly audit patient records to identify and correct errors. I emphasize the importance of clear, concise, and complete documentation to all healthcare team members. When discrepancies arise, I use a methodical process to investigate and resolve the issue, documenting the steps taken and the outcome.
Furthermore, I promote a culture of accountability and transparency within the healthcare team, encouraging open communication and collaboration to minimize errors and maintain the integrity of patient information. Education on data privacy regulations and best practices for data handling is an ongoing process.
Q 28. What is your approach to continuous professional development in patient advocacy and education?
Continuous professional development is crucial in the ever-evolving field of patient advocacy and education. My approach involves a multi-pronged strategy focused on staying abreast of the latest research, best practices, and technological advancements in healthcare.
This includes attending conferences and workshops, participating in online courses, and engaging in professional networking opportunities. I actively seek out mentorship from experienced professionals and participate in peer-review discussions to learn from others’ experiences and refine my own skills. I also dedicate time to self-directed learning, researching areas of interest and keeping up-to-date with relevant publications and literature.
Maintaining certifications and pursuing advanced qualifications are also part of my commitment to lifelong learning. Continuous professional development allows me to remain proficient in my practice, and most importantly, to offer the best possible care and support to my patients.
Key Topics to Learn for Patient Advocacy and Education Interview
- Understanding Patient Needs & Communication Styles: Learn to effectively assess diverse patient needs and tailor your communication approach accordingly, considering cultural, linguistic, and emotional factors.
- Developing Educational Materials: Explore best practices for creating clear, concise, and engaging patient education materials, including brochures, videos, and presentations, that are easily understood and accessible.
- Health Literacy & Patient Empowerment: Understand the concept of health literacy and its impact on patient outcomes. Learn strategies to empower patients to actively participate in their healthcare decisions.
- Advocacy Skills & Techniques: Master the art of effective advocacy, navigating the healthcare system to ensure patients receive appropriate care, access resources, and have their voices heard.
- Ethical Considerations & Confidentiality: Explore the ethical dilemmas faced in patient advocacy and education, and understand the importance of maintaining patient confidentiality and privacy.
- Collaboration & Teamwork: Learn the importance of effective collaboration with healthcare professionals, family members, and other stakeholders to provide holistic patient care and support.
- Program Evaluation & Improvement: Understand how to measure the effectiveness of patient education programs and use data to make improvements and drive better patient outcomes.
- Cultural Competency & Sensitivity: Develop an understanding of diverse cultural beliefs and practices related to healthcare and how to adapt your approach to effectively work with patients from different backgrounds.
- Technology & Patient Engagement: Explore how technology can be leveraged to enhance patient education and engagement, including telehealth platforms and digital health tools.
- Problem-Solving & Conflict Resolution: Develop skills in addressing challenges and conflicts that may arise in patient advocacy situations, utilizing effective problem-solving strategies.
Next Steps
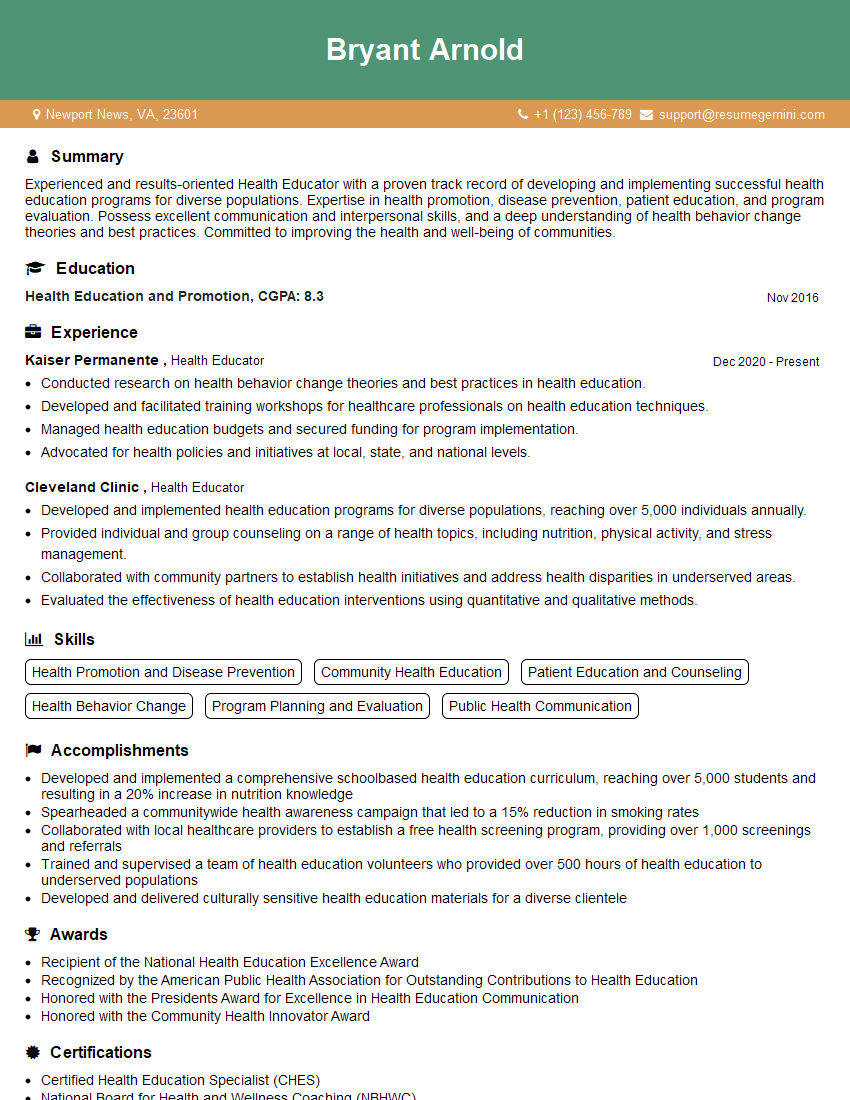
Mastering Patient Advocacy and Education is crucial for career advancement in healthcare. It demonstrates your commitment to patient-centered care and positions you as a valuable asset to any healthcare team. To significantly improve your job prospects, creating an ATS-friendly resume is essential. ResumeGemini is a trusted resource to help you build a professional and impactful resume that highlights your skills and experience. ResumeGemini provides examples of resumes tailored to Patient Advocacy and Education, helping you showcase your qualifications effectively and land your dream job.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hi, I have something for you and recorded a quick Loom video to show the kind of value I can bring to you.
Even if we don’t work together, I’m confident you’ll take away something valuable and learn a few new ideas.
Here’s the link: https://bit.ly/loom-video-daniel
Would love your thoughts after watching!
– Daniel
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.