Feeling uncertain about what to expect in your upcoming interview? We’ve got you covered! This blog highlights the most important Double Balloon Enteroscopy (DBE) interview questions and provides actionable advice to help you stand out as the ideal candidate. Let’s pave the way for your success.
Questions Asked in Double Balloon Enteroscopy (DBE) Interview
Q 1. Describe the indications for Double Balloon Enteroscopy (DBE).
Double Balloon Enteroscopy (DBE) is a sophisticated endoscopic technique used to visualize and treat lesions in the small bowel, a region traditionally difficult to access with conventional endoscopy. Its indications primarily revolve around investigating obscure gastrointestinal bleeding, diagnosing unexplained abdominal pain or iron deficiency anemia, and addressing suspected small bowel tumors or inflammatory conditions.
- Obscure gastrointestinal bleeding: When the source of bleeding cannot be identified through upper or lower endoscopy, DBE is crucial for pinpointing the bleeding site in the small bowel.
- Diagnosis of Crohn’s disease: DBE helps visualize and assess the extent of inflammation in the small bowel, particularly in patients with suspected Crohn’s disease.
- Polyps and tumors: DBE allows for the detection and removal (polypectomy) of small bowel polyps and the biopsy of suspicious tumors.
- Strictures: DBE can help evaluate and potentially treat small bowel strictures (narrowing).
- Foreign body retrieval: In cases of ingested foreign bodies that lodge in the small bowel, DBE can facilitate their safe removal.
Essentially, DBE is indicated when there’s a strong clinical suspicion of a small bowel pathology requiring direct visualization and potential intervention.
Q 2. What are the contraindications for DBE?
While DBE is a powerful tool, certain contraindications limit its use. These fall into several categories:
- Severe cardiovascular disease: The procedure is lengthy and requires significant sedation, posing risks for patients with unstable cardiac conditions.
- Uncontrolled coagulopathy: Patients with impaired blood clotting are at higher risk of bleeding complications during the procedure.
- Severe pulmonary disease: The prone position required for DBE can compromise respiration in patients with severe lung disease.
- Recent abdominal surgery or inflammation: Active inflammation or recent surgery increases the perforation risk significantly.
- Severe ascites (fluid in the abdomen): This can hinder visualization and increase the risk of complications.
- Inability to tolerate prolonged sedation: DBE is often lengthy, requiring a high level of sedation and analgesia. Patients unable to tolerate this are unsuitable candidates.
Careful evaluation of the patient’s overall health is crucial before proceeding with DBE. Thorough risk-benefit assessment is paramount.
Q 3. Explain the mechanism of the double balloon system in DBE.
The double balloon system is the core innovation of DBE, enabling access to the entire small bowel. It comprises a long, flexible endoscope with two inflatable balloons – one proximal and one distal – separated by a working channel.
Mechanism: The distal balloon is inflated to grip the bowel wall, while the proximal balloon secures the scope’s position higher up in the intestine. The endoscope is then advanced by inflation and deflation of the balloons, allowing for controlled intubation. The proximal balloon acts as an anchor, preventing slippage while the distal balloon acts as the propulsion mechanism. This allows for both antegrade (forward) and retrograde (backward) navigation within the small intestine.
Think of it like inch-worming through the small bowel, using the balloons for controlled grip and advancement. The working channel allows for the passage of biopsy forceps, polypectomy snares, and other instruments for diagnostic and therapeutic interventions.
Q 4. Detail the steps involved in performing a DBE procedure.
A typical DBE procedure involves several key steps:
- Preparation: This includes bowel cleansing (usually with polyethylene glycol solutions), intravenous access establishment, and monitoring of vital signs.
- Sedation and analgesia: Patients are placed under deep sedation and analgesia for their comfort and safety throughout the procedure.
- Intubation: The double balloon enteroscope is advanced through the mouth or nose, carefully navigating the small bowel using the inflation and deflation of the balloons. Experienced endoscopists carefully assess fluoroscopy images which can be extremely helpful during the process.
- Intestinal exploration and procedures: Once the target area is reached, diagnostic and therapeutic procedures are performed, including biopsy, polypectomy, or stricture dilation.
- Withdrawal of the endoscope: After the procedures are completed, the scope is withdrawn slowly and carefully.
- Post-procedure monitoring: Patients are closely monitored for any complications, such as bleeding or perforation, and receive appropriate post-procedure care.
The procedure’s duration can vary significantly, depending on the length of the small bowel involved and the complexity of the interventions performed.
Q 5. How do you manage bleeding complications during DBE?
Bleeding is a potential complication during DBE, particularly after polypectomy or biopsy. Management involves a stepwise approach:
- Immediate assessment: The severity of bleeding is assessed, usually through haemodynamic monitoring (blood pressure, heart rate).
- Endoscopic haemostasis: If the bleeding source is identified, various techniques can be employed, including epinephrine injection, coagulation with argon plasma, or clipping.
- Pharmacological intervention: Intravenous fluids and blood transfusions are given to support haemodynamics and replace blood loss.
- Surgical intervention: In cases of uncontrolled bleeding that cannot be managed endoscopically, urgent surgical intervention may be necessary.
Prophylactic measures like meticulous technique during polyp removal and careful patient selection can minimize the risk of bleeding.
Q 6. What are the potential perforation risks during DBE, and how are they mitigated?
Bowel perforation represents a serious complication of DBE, although the risk is relatively low in the hands of experienced endoscopists. Several factors increase the risk, including the presence of inflammation, strictures, or previous abdominal surgery.
Mitigation strategies include:
- Careful patient selection: Patients with significant risk factors should be carefully evaluated and alternative procedures considered.
- Meticulous technique: Careful balloon inflation and gentle manipulation of the endoscope minimize the risk of perforation.
- Fluoroscopic guidance: Use of fluoroscopy (real-time X-ray imaging) can provide valuable guidance and enhance the safety of the procedure.
- Early recognition and management: Immediate recognition of signs of perforation (abdominal pain, peritonitis) is crucial, requiring urgent surgical consultation and intervention.
Prevention is key; a cautious approach and skilled expertise are crucial in minimizing the risk of perforation.
Q 7. Discuss the role of sedation and analgesia in DBE.
Sedation and analgesia are integral to DBE, ensuring patient comfort and tolerance of a lengthy and potentially uncomfortable procedure. The depth of sedation is tailored to individual patient needs and risk profiles. Commonly used agents include propofol and midazolam for sedation, and fentanyl or remifentanil for analgesia.
Monitoring: Continuous monitoring of vital signs, including oxygen saturation, heart rate, blood pressure, and respiratory rate, is essential throughout the procedure. The use of pulse oximetry and capnography is also crucial. A dedicated anesthesia professional or trained nurse is essential for close monitoring and management of sedation.
The optimal level of sedation allows for patient comfort without compromising their respiratory or cardiovascular status, and ensures patient cooperation and successful procedure completion.
Q 8. How do you handle difficult intubation during DBE?
Difficult intubation during Double Balloon Enteroscopy (DBE) is a common challenge. It often stems from anatomical variations, such as severe angulations or strictures, or inadequate bowel preparation. My approach is multi-pronged and prioritizes patient safety.
- Careful Pre-procedural Assessment: A thorough review of the patient’s history, including prior abdominal surgeries and imaging studies (CT enterography, capsule endoscopy) helps anticipate potential difficulties.
- Strategic Intubation Techniques: I employ a combination of techniques, starting with gentle advancement of the endoscope, using controlled insufflation of air or CO2 to navigate difficult bends. If significant resistance is encountered, I may use hydro-dissection or carefully manipulate the balloons to negotiate the obstruction. The use of water or contrast for fluoroscopy guidance can be invaluable.
- Alternative Approaches: If intubation proves exceptionally challenging, I don’t hesitate to reassess and potentially utilize alternative techniques, such as switching to a different size or type of endoscope, or even terminating the procedure if deemed unsafe for the patient.
- Patient Positioning: Optimizing patient positioning (e.g., slight Trendelenburg, left lateral decubitus) can significantly aid intubation in certain scenarios.
For instance, I recently encountered a patient with extensive prior abdominal adhesions. Careful fluoroscopic guidance combined with strategic balloon inflation allowed successful navigation, preventing the need for premature procedure termination.
Q 9. Describe your experience with polypectomy and other therapeutic interventions during DBE.
Polypectomy and other therapeutic interventions during DBE are integral parts of my practice. The ability to perform these procedures extends the scope of DBE beyond simple diagnostic visualization.
- Polypectomy: I routinely perform snare polypectomy for lesions in the small bowel, using a variety of techniques depending on the size, location, and morphology of the polyp. This includes cold snare polypectomy for smaller lesions and hot snare polypectomy for larger ones. Hemoclips and argon plasma coagulation are employed for hemostasis as needed. Careful attention is paid to complete resection, minimizing the risk of recurrence or perforation.
- Other Interventions: Beyond polypectomy, I have experience with various other therapeutic procedures during DBE, such as Argon Plasma Coagulation (APC) for treating angiodysplasia, clipping of bleeding vessels, and the removal of foreign bodies. The choice of intervention is tailored to the specific clinical scenario.
One memorable case involved a patient with a large, pedunculated polyp in the distal ileum, successfully removed via snare polypectomy with minimal bleeding.
Q 10. Explain your approach to managing bowel preparation for DBE.
Adequate bowel preparation is paramount for successful DBE. I typically employ a split bowel prep regimen, ensuring optimal visualization of the small bowel.
- Oral Bowel Preparation: I usually prescribe a combination of polyethylene glycol (PEG) solutions and bisacodyl for complete cleansing of the colon and the proximal small bowel. The exact protocol is tailored to the patient’s individual tolerance and clinical situation, which might include modification for patients with renal impairment or other medical comorbidities.
- Dietary Restrictions: Clear liquid diet for 24-48 hours prior to the procedure is standard practice to minimize fecal residue. This may vary slightly depending on patient factors and the specific PEG solution utilized.
- Timing: The bowel prep is carefully timed to allow sufficient bowel cleansing without undue discomfort or dehydration. Usually the PEG solution is started the evening before the procedure.
For example, I might adapt the bowel preparation for an elderly patient with a history of renal insufficiency by modifying the amount of PEG solution used and carefully monitoring their fluid and electrolyte balance.
Q 11. What are the advantages and disadvantages of DBE compared to other endoscopic techniques?
DBE offers significant advantages over other endoscopic techniques, but it also has limitations.
- Advantages: DBE allows for visualization of the entire small bowel, enabling the diagnosis and treatment of conditions inaccessible to conventional colonoscopy or upper endoscopy. Its therapeutic capabilities make it valuable for polypectomy, hemostasis, and foreign body removal.
- Disadvantages: DBE is a more complex and technically demanding procedure than colonoscopy or upper endoscopy, requiring specialized training and expertise. It carries a higher risk of complications such as perforation, bleeding, and infection. The procedure can be lengthy and time-consuming, placing demands on both the patient and the endoscopist.
Choosing between DBE and other methods depends on the clinical question. For example, while capsule endoscopy provides excellent visualization of the small bowel, it lacks therapeutic capabilities and is not suitable for all patients.
Q 12. How do you assess the adequacy of bowel preparation before a DBE?
Assessing bowel preparation adequacy before DBE is crucial for procedural success. This is done through a combination of methods.
- Visual Inspection: Upon insertion of the endoscope, I visually inspect the colon and proximal small bowel for residual stool. Clear visualization of the bowel mucosa is the primary indicator of adequate preparation.
- Fluoroscopy: Fluoroscopy is helpful to assess the entire bowel, identifying any areas with retained fecal matter that may be difficult to visualize endoscopically. This is especially valuable in assessing the terminal ileum.
Inadequate bowel preparation necessitates either postponing the procedure to allow for a repeat bowel prep or using more aggressive cleansing techniques during the procedure itself, although this approach may be somewhat limited in its effectiveness.
Q 13. How would you address a patient’s anxiety before a DBE procedure?
Addressing patient anxiety before a DBE procedure is vital. I approach this through open communication, empathy, and a proactive strategy.
- Pre-procedural Education: I spend time explaining the procedure in detail, using clear and simple language, addressing the patient’s concerns and answering their questions honestly and thoroughly. This involves a discussion of the procedure’s benefits, risks, and potential complications.
- Medication: Mild anxiolytic medication can be prescribed for patients with significant anxiety, which is discussed and planned before the procedure.
- Supportive Environment: I encourage the patient to bring a support person to the procedure, providing reassurance and comfort. A calm and friendly demeanor from the medical team during the pre-procedural preparations is also key.
For example, I will often show patients images from previous DBE procedures (with appropriate patient privacy safeguards) to desensitize them to the visualization of the small bowel and make them feel more confident and comfortable.
Q 14. Describe your post-procedural care protocol for DBE patients.
Post-procedural care for DBE patients is crucial for preventing complications and ensuring a smooth recovery.
- Monitoring: Vital signs (heart rate, blood pressure, oxygen saturation) are closely monitored in the immediate post-procedure period. I observe for signs of perforation, bleeding, or infection.
- Pain Management: Analgesics are administered as needed to manage post-procedural discomfort, usually using standard anti-inflammatory medications.
- Hydration: I ensure adequate hydration, often intravenously immediately after the procedure, and then by oral route as the patient tolerates.
- Diet: A gradual return to a regular diet is encouraged, starting with clear liquids and advancing as tolerated.
- Follow-up: A follow-up appointment is scheduled to discuss results, address any concerns, and monitor for late complications.
In cases of complications such as perforation, immediate surgical intervention may be necessary. Regular follow-up helps to promptly identify and manage any delayed complications.
Q 15. How do you interpret the findings of a DBE procedure?
Interpreting DBE findings requires a systematic approach, combining image analysis with clinical context. We start by assessing the quality of the procedure; was the entire designated small bowel segment visualized? Then, we meticulously examine the images for any abnormalities. This includes looking for:
- Polyps: Size, location, shape, and appearance (sessile or pedunculated) are all noted. Biopsy results are crucial for determining benignancy or malignancy.
- Ulcers: Their size, depth, and surrounding inflammation are assessed. We look for evidence of active bleeding or signs of malignancy.
- Strictures: The location, length, and severity of strictures are documented. Their cause needs to be investigated.
- Tumors: These are thoroughly evaluated for size, location, and involvement of surrounding structures. Biopsy is essential.
- Inflammation: The presence and extent of inflammation in the bowel wall are noted. This is key for diagnosing inflammatory bowel disease.
- Bleeding: The source and severity of any bleeding are identified and addressed appropriately.
Finally, a comprehensive report is generated, correlating the endoscopic findings with the patient’s clinical history and other investigations like imaging studies. For example, a patient presenting with iron-deficiency anemia might have a DBE revealing a small, bleeding angiodysplasia, previously undetectable by other means. The report would detail the location and character of the lesion, along with recommendations for management, such as endoscopic hemostasis or surgical intervention if needed.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What are the common complications of DBE and their management?
DBE, while a valuable tool, carries inherent risks. Common complications include:
- Perforation: This is a serious complication, requiring immediate intervention. It’s usually managed surgically, sometimes with a laparotomy or laparoscopic repair depending on the site and severity.
- Bleeding: Can occur during polypectomy or other therapeutic maneuvers. It’s usually managed endoscopically with techniques like injection of epinephrine or clips. Transfusion may be necessary in severe cases.
- Pancreatitis: This is rare but more likely in the context of manipulation near the papilla of Vater. Management focuses on supportive measures like bowel rest and fluid resuscitation.
- Infection: Post-procedure infections such as peritonitis can occur. Antibiotics are usually administered.
- Cardiovascular events: This is less frequent but patients with cardiac issues require close monitoring.
- Abdominal pain and distension: This can be managed with analgesics and bowel rest. Usually subsides within a few days.
Careful patient selection, meticulous technique, and close monitoring during and after the procedure are crucial in minimizing these risks. Pre-procedure evaluation focusing on cardiovascular health and coagulation status is also important. Post-procedural monitoring includes careful observation for signs of perforation like abdominal tenderness, fever, and tachycardia.
Q 17. Explain the role of fluoroscopy in DBE.
Fluoroscopy plays a vital role in DBE, essentially acting as a real-time X-ray imaging system. It allows visualization of the endoscope’s position and advancement within the bowel. This is especially important in navigating the complex anatomy of the small bowel, particularly during deep enteroscopy. Fluoroscopy aids in:
- Precise Endoscope Placement: It provides a clear picture of the endoscope’s location and orientation, allowing the endoscopist to accurately advance the scope through the intestines, helping to avoid unnecessary looping or looping of the small bowel.
- Detection of Perforation: Air leakage from the bowel is readily detectable on fluoroscopy and immediately indicates a potential perforation.
- Identification of Obstructions: Fluoroscopy can help identify anatomical obstructions or strictures hampering the passage of the endoscope.
- Guidance During Therapeutic Procedures: It helps in accurate placement of clips, injection of medication, and application of energy-based techniques like argon plasma coagulation.
For example, a patient with a suspected ileal stricture might be undergoing DBE. Fluoroscopy would clearly demonstrate the extent of the stricture, enabling the endoscopist to navigate the area carefully and possibly even perform dilatation if appropriate. The use of fluoroscopy in DBE is not without potential risks – like radiation exposure for both the patient and the physician. However the benefits significantly outweigh the risks. Appropriate shielding and limiting fluoroscopy time are critical.
Q 18. Describe your experience with different types of DBE equipment and accessories.
My experience encompasses a range of DBE equipment and accessories from various manufacturers. This includes endoscopes with different lengths and diameters, overtubes, balloon inflation systems, and accessories for therapeutic procedures such as polypectomy snares, argon plasma coagulation devices, and endoscopic mucosal resection (EMR) equipment.
I’ve worked with both video and non-video endoscopes. Video endoscopes give superior image quality and allow for better real-time assessment of the bowel lining. The choice of equipment depends on the specific clinical scenario, patient anatomy, and the suspected pathology. For instance, longer endoscopes might be needed for deep small bowel lesions while shorter ones might suffice for lesions in the proximal small bowel. The flexibility of the endoscope needs to be carefully considered as well. Accessories used in therapeutic interventions also vary with the specific situation. Experience with various types of equipment allows for a more flexible and adaptable approach to DBE procedures.
For instance, I prefer one brand’s balloon inflation system for its ease of use and precise pressure control, another’s polypectomy snare for its maneuverability and strength. Adapting to different equipment is very important. It’s about choosing the best tools to handle each case.
Q 19. How do you manage a suspected perforation during a DBE?
Suspected perforation during DBE is a surgical emergency. Management involves immediate cessation of the procedure. The primary steps include:
- Immediate assessment: Closely monitor vital signs (heart rate, blood pressure, oxygen saturation). Assess for signs of peritonitis (abdominal rigidity, guarding, rebound tenderness).
- Fluid resuscitation: Initiate intravenous fluids to maintain hemodynamic stability.
- Broad-spectrum antibiotics: Administer prophylactic antibiotics to prevent infection.
- Surgical consultation: Immediately consult a surgical team for evaluation and potential intervention.
- Imaging studies: Obtain abdominal X-rays or a CT scan to confirm the diagnosis and assess the extent of perforation.
- Surgical intervention: Surgical repair is generally necessary, often involving laparotomy or laparoscopic techniques.
The approach depends on the location and severity of the perforation. Small perforations might be managed conservatively with close monitoring and bowel rest, but most cases necessitate surgical repair to prevent peritonitis and other life-threatening complications. Post-operative care includes intensive monitoring, continued antibiotic treatment, and nutritional support. Careful documentation and follow-up are essential.
Q 20. What are the key differences between single-balloon and double-balloon enteroscopy?
The key difference lies in the number of balloons. Single-balloon enteroscopy (SBE) utilizes a single balloon to advance the scope through the intestinal lumen, while DBE employs two separate balloons – one for advancement and another for distal traction/anchoring. This crucial difference impacts several aspects:
- Intubation Depth: DBE typically allows for deeper intubation into the small bowel compared to SBE, significantly increasing the reach and diagnostic/therapeutic potential.
- Technique: SBE relies on a more ‘push-and-pull’ technique, whereas DBE involves controlled advancement with distal anchoring and intubation.
- Procedure Duration: DBE procedures generally take longer than SBE procedures.
- Technical complexity: DBE is technically more demanding than SBE, requiring more skill and experience from the endoscopist.
- Complications: While both have similar potential complications, the deeper reach and longer duration of DBE can increase the risk in some cases.
In essence, while SBE is a valuable tool for reaching the proximal small bowel, DBE provides superior access and facilitates the exploration of the entire small bowel, making it ideal for examining deep-seated lesions or conditions affecting the distal small bowel. Choosing between SBE and DBE is largely determined by factors such as the location of the suspected lesion, clinical indication, and the endoscopist’s experience and expertise.
Q 21. What is your experience with advanced therapeutic techniques using DBE (e.g., argon plasma coagulation, endoscopic mucosal resection)?
I have extensive experience in utilizing advanced therapeutic techniques during DBE. Argon plasma coagulation (APC) is frequently used for hemostasis of bleeding lesions (e.g., angiodysplasias) or for treating inflammatory lesions. APC’s precise application and minimal thermal injury makes it well suited for the delicate environment of the small bowel.
Endoscopic mucosal resection (EMR) is another technique I regularly employ for the removal of polyps or superficial tumors. It allows for en bloc resection and histological examination. EMR requires careful planning and execution, particularly within the small bowel, and is dependent on the lesion characteristics. I also have experience with other techniques, such as band ligation, polypectomy, and dilatation of strictures depending on the clinical need and the patient’s health status.
The choice of technique is individualized, considering lesion characteristics, patient factors (e.g., coagulation status), and the technical feasibility. For example, a large sessile polyp may necessitate piecemeal EMR, whereas smaller pedunculated polyps might be effectively removed using polypectomy. Post-procedure monitoring following therapeutic interventions is critical, paying close attention to bleeding, perforation, or other complications. Detailed documentation is essential, including procedural details, any complications encountered, and the final pathology report. Success in these advanced techniques depends on a combination of technical skill, appropriate equipment, and thorough post-procedure care.
Q 22. Explain your understanding of the anatomy relevant to DBE.
Understanding the anatomy relevant to Double Balloon Enteroscopy (DBE) is crucial for successful and safe procedure execution. DBE allows visualization and intervention in the small bowel, an area notoriously difficult to access with traditional endoscopy. Therefore, a thorough knowledge of the small bowel’s structure, including its length, its various segments (duodenum, jejunum, ileum), its relationship to adjacent organs (like the colon and stomach), and the presence of anatomical landmarks like the ligament of Treitz, is essential. The procedure also involves navigating the cecum and ascending colon during antegrade DBE and the transverse and descending colon during retrograde DBE. A strong understanding of the vascular supply and lymphatic drainage of these areas is also important for managing potential complications like bleeding or perforation. It’s not just about the small bowel itself; it’s also about understanding the surrounding structures to anticipate and avoid potential challenges during the procedure.
For example, recognizing the ligament of Treitz is vital during antegrade DBE as it marks the transition between the duodenum and jejunum, guiding the navigation of the endoscope. Similarly, being aware of the location of the ileocecal valve is essential for safe passage during both antegrade and retrograde procedures. Knowing the anatomical variations is also important. Not all individuals have the same anatomical features, and variations in the small bowel’s length and position can require adapted techniques. In essence, mastering the anatomy sets the stage for a smooth and effective DBE procedure.
Q 23. How do you ensure patient safety during a DBE procedure?
Patient safety is paramount in DBE. My approach involves several key elements. Firstly, a comprehensive patient history and physical examination are essential to assess the risk factors and suitability for the procedure. This includes evaluation of their cardiovascular and respiratory status, as well as identifying any potential bleeding disorders or allergies to medications. Preoperative bowel preparation, often with a low-residue diet and laxatives, is crucial to ensure optimal visualization. Secondly, meticulous monitoring during the procedure is vital. This includes continuous monitoring of vital signs (heart rate, blood pressure, oxygen saturation), careful observation for any signs of distress, and maintaining adequate sedation and analgesia. The sedation is carefully titrated to ensure comfort and cooperation without compromising respiratory function. We use pulse oximetry and capnography for respiratory monitoring. Regular assessment of fluid balance is also vital. Thirdly, using appropriate endoscopy techniques that minimize risk is key. This means careful advancement and withdrawal of the endoscope to avoid perforation or bowel injury. The use of appropriate inflation pressures in the balloons is critical and strictly adhered to. Regular endoscopic images are reviewed throughout the process. Fourthly, having a robust plan for managing complications, including perforation, bleeding, and adverse reactions to sedation, is paramount. We ensure necessary resuscitation equipment, including fluids, blood, and medications, is readily available. Finally, post-procedure monitoring is crucial. Patients are observed in a recovery room and followed up to assess any complications like pain, bleeding or infection.
Q 24. What is your approach to troubleshooting technical difficulties during a DBE?
Troubleshooting technical difficulties during a DBE procedure requires a systematic approach. The first step is to identify the specific problem. Is it difficulty in advancing the endoscope? Is it a problem with balloon inflation or deflation? Or is the image quality poor? Then a systematic approach begins based on the type of problem encountered. For instance, if the endoscope is stuck, gentle manipulation with adjustments in angulation and pressure, using the appropriate balloon inflation, is attempted first. If this fails, imaging techniques like fluoroscopy may be employed to visualize the position of the endoscope and identify the obstruction. If there’s a problem with balloon inflation or deflation, the integrity of the balloons and the functionality of the inflation/deflation system are checked. Sometimes simply changing the inflation medium may resolve the issue. Poor image quality could be due to inadequate bowel preparation, excess air or fluid in the bowel, or problems with the endoscope’s camera system. This requires carefully reviewing the bowel preparation and making adjustments based on what was observed during the procedure. In cases where the problem cannot be resolved easily, the procedure may need to be temporarily paused or even terminated to avoid risking patient safety. Documenting all interventions and troubleshooting steps is extremely important. Experience plays a significant role in rapidly identifying and effectively managing technical issues. Regular training and maintenance of equipment are essential preventative measures.
Q 25. Describe your experience with documenting DBE procedures.
Accurate and comprehensive documentation is integral to good patient care and legal protection. My approach involves meticulously documenting every aspect of the procedure, starting from the pre-procedure assessment and consent to the post-procedure recovery. The documentation includes: patient demographics, medical history, indication for the procedure, pre-procedure preparation details, the type of DBE performed (antegrade, retrograde, or double-balloon enteroscopy), detailed descriptions of the endoscopic findings (including the location, size, and nature of any lesions), any biopsies performed, details of all therapeutic interventions, the amount and type of sedation and analgesia used, intraoperative vital signs, any complications encountered, and the post-procedure management plan. High-quality images (stills and videos) are acquired and included as part of the report. I use structured reporting systems to ensure consistency and completeness of the documentation. The medical record should ideally be a comprehensive and easily accessible record, capable of being understood by other healthcare providers. The patient’s post-procedure recovery and any significant findings from subsequent follow-up appointments are also meticulously documented. These records serve as a crucial reference for future management, research, and quality assurance.
Q 26. How do you manage a patient who experiences a reaction to sedation during DBE?
Managing a patient experiencing a reaction to sedation during DBE requires immediate attention and a coordinated response. The first step involves recognizing the signs and symptoms of the reaction, which can range from mild (e.g., nausea, vomiting, hypotension) to severe (e.g., respiratory depression, cardiac arrhythmias). Once a reaction is recognized, the sedation is immediately stopped, and the patient’s airway is assessed and secured if necessary. Oxygen is administered, and monitoring is intensified. Depending on the severity, treatment may range from supportive care (e.g., oxygen, intravenous fluids) to more aggressive measures such as administering medications to counteract the sedative effects or to treat hypotension or arrhythmias. We maintain close communication with anesthesiology or critical care for severe reactions. The patient’s vital signs are closely monitored, and if necessary, the patient is transferred to the intensive care unit (ICU) for close monitoring and treatment. Post-procedure, we carefully review the events leading up to the reaction to understand what triggered it and to prevent similar events in future cases. Documentation of the reaction, treatment provided, and subsequent recovery is crucial for further analysis and risk management.
Q 27. What are the current research advancements and future trends in DBE?
Research in DBE is constantly evolving, focusing on improving safety, efficacy, and expanding its applications. Current advancements include the development of advanced imaging techniques, such as narrow-band imaging (NBI) and chromoendoscopy, to improve lesion detection and characterization. There’s growing research on minimally invasive methods for therapeutic interventions such as polyp removal and hemostasis. There is also significant work being done on improving the design and functionality of the enteroscope itself. For example, improved balloon designs for better maneuverability are being developed. Another area of focus is the development of advanced software for improved image processing and navigation during DBE. Future trends may include the integration of artificial intelligence (AI) for automated lesion detection, robotic-assisted DBE for improved precision, and the development of novel endoscopic techniques to improve visualization and access to previously inaccessible areas of the small bowel. Personalized approaches, using patient-specific information to tailor the procedure, are likely to become more prevalent. Research also continues to focus on the clinical application of DBE to a broader spectrum of indications and on extending long-term follow-up data to better evaluate outcomes.
Q 28. Describe a challenging DBE case you have encountered and how you handled it.
One challenging case involved a patient with suspected Crohn’s disease presenting with recurrent abdominal pain and weight loss. During the antegrade DBE, the endoscope encountered significant angulations and strictures in the terminal ileum. The strictures were so tight that advancing the endoscope became incredibly difficult, creating a considerable risk of perforation. To overcome this, we employed several strategies. First, we used gentle and controlled inflation of the balloons to avoid causing excessive pressure and potential injury. Second, we carefully adjusted the position and angle of the endoscope, using fluoroscopy to assist in navigation. Third, we utilized water irrigation to clear any fecal matter or debris that might have been contributing to the obstruction. Despite these measures, we were still faced with challenges. We carefully documented the difficulty in advancing the endoscope in addition to all attempts at advancing it. The procedure was stopped multiple times to allow the patient to rest. Ultimately, we successfully navigated the strictures, visualized extensive inflammation and ulcerations in the terminal ileum, consistent with Crohn’s disease, and obtained crucial biopsies for histopathological confirmation. The patient made a full recovery following the procedure. This case highlighted the importance of meticulous technique, patience, and the ability to adapt strategies during challenging DBE procedures.
Key Topics to Learn for Double Balloon Enteroscopy (DBE) Interview
- Indications and Contraindications: Master the criteria for selecting patients suitable for DBE and understanding when it’s not the appropriate procedure. Consider the advantages and disadvantages compared to other endoscopic techniques.
- Procedure Technique: Thoroughly understand the step-by-step process, including balloon inflation/deflation, advancement techniques, and handling of potential complications. Practice explaining the procedure clearly and concisely.
- Advanced Techniques and Applications: Familiarize yourself with specialized DBE applications, such as polypectomy, stricture dilation, and stent placement. Be prepared to discuss your experience and comfort level with these techniques.
- Complications and Management: Understand potential complications (perforation, bleeding, etc.) and the strategies for their prevention and management. This demonstrates a crucial aspect of patient safety awareness.
- Imaging and Interpretation: Develop the ability to interpret images obtained during DBE and correlate them with clinical findings. Practice explaining your diagnostic reasoning.
- Post-procedure Care and Follow-up: Understand the importance of post-procedure monitoring and patient education. Be prepared to discuss appropriate follow-up care and potential complications.
- Equipment and Technology: Demonstrate familiarity with different types of DBE equipment and their functionalities. Understanding the nuances of the technology shows technical proficiency.
- Ethical and Legal Considerations: Be prepared to discuss ethical considerations related to informed consent and patient autonomy within the context of DBE.
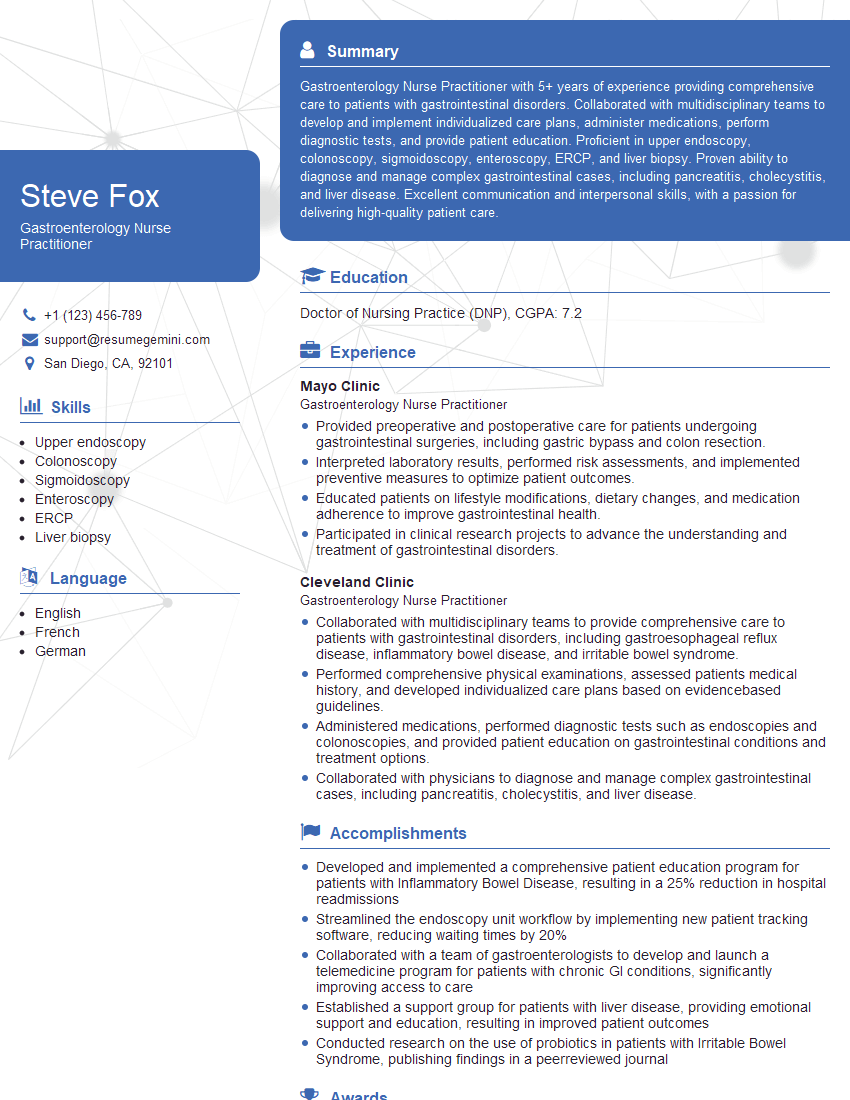
Next Steps
Mastering Double Balloon Enteroscopy (DBE) significantly enhances your career prospects in gastroenterology and related fields. It opens doors to specialized roles and advanced clinical opportunities. To maximize your chances of landing your dream job, crafting a compelling and ATS-friendly resume is crucial. ResumeGemini is a trusted resource that can help you build a professional and impactful resume, tailored to highlight your DBE expertise. Examples of resumes tailored specifically to Double Balloon Enteroscopy (DBE) roles are available to guide you. Invest in your future – create a resume that showcases your skills and experience effectively.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hi, I have something for you and recorded a quick Loom video to show the kind of value I can bring to you.
Even if we don’t work together, I’m confident you’ll take away something valuable and learn a few new ideas.
Here’s the link: https://bit.ly/loom-video-daniel
Would love your thoughts after watching!
– Daniel
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.