Every successful interview starts with knowing what to expect. In this blog, we’ll take you through the top Interstitial Lung Disease Management interview questions, breaking them down with expert tips to help you deliver impactful answers. Step into your next interview fully prepared and ready to succeed.
Questions Asked in Interstitial Lung Disease Management Interview
Q 1. Describe the pathophysiology of idiopathic pulmonary fibrosis (IPF).
Idiopathic pulmonary fibrosis (IPF) is a chronic, progressive, and ultimately fatal interstitial lung disease of unknown cause. Its pathophysiology is complex and not fully understood, but it involves a cyclical process of epithelial injury, aberrant wound healing, and excessive extracellular matrix deposition. Imagine your lungs’ delicate air sacs (alveoli) getting repeatedly injured. Instead of healing properly, the body’s repair response goes haywire, leading to excessive scarring (fibrosis) that stiffens the lungs and hinders oxygen uptake.
- Epithelial Cell Injury: The process begins with damage to the alveolar epithelial cells, the lining of the air sacs. This damage can be triggered by various factors, although the exact cause remains elusive. Genetic predisposition and environmental exposures like silica dust or certain viruses are suspected contributors.
- Fibroblast Activation and Extracellular Matrix Deposition: Damaged epithelial cells release signals that activate fibroblasts, cells responsible for producing collagen and other components of the extracellular matrix. In IPF, fibroblasts become abnormally active, producing excessive amounts of collagen, leading to the characteristic fibrosis and thickening of the lung tissue.
- Immune System Dysregulation: The immune system plays a role, with both inflammatory and anti-inflammatory processes involved. An imbalance in these processes contributes to the ongoing tissue damage and fibrosis.
- Epithelial-Mesenchymal Transition (EMT): Epithelial cells can transform into myofibroblasts, cells that contribute significantly to fibrosis, further exacerbating the scarring process.
This vicious cycle of injury, inflammation, and fibrosis progressively worsens lung function, leading to shortness of breath, a dry cough, and ultimately respiratory failure.
Q 2. Differentiate between various types of interstitial lung diseases (ILDs).
Interstitial lung diseases (ILDs) encompass a broad spectrum of disorders characterized by inflammation and/or fibrosis affecting the interstitium – the supporting tissue between the alveoli and blood vessels. They are classified based on their underlying cause, clinical presentation, and imaging findings. Some key differentiations include:
- Idiopathic Pulmonary Fibrosis (IPF): A chronic, progressive fibrotic ILD of unknown cause, characterized by a specific pattern of fibrosis on HRCT.
- Non-specific Interstitial Pneumonia (NSIP): A pattern of ILD that can be either predominantly fibrotic or inflammatory, often with a better prognosis than IPF.
- Acute Interstitial Pneumonia (AIP): A rapidly progressive and life-threatening form of ILD with severe inflammation. Early diagnosis and aggressive treatment are crucial.
- Hypersensitivity Pneumonitis (HP): An inflammatory ILD triggered by an allergic reaction to inhaled antigens (e.g., mold, bird droppings). Identifying and eliminating the offending antigen is crucial for management.
- Sarcoidosis: A multisystem granulomatous disease that can affect the lungs, causing inflammation and sometimes fibrosis. It has a variable clinical course and may resolve spontaneously or require treatment.
- ILD associated with connective tissue diseases (e.g., rheumatoid arthritis, lupus): In these cases, ILD arises as a complication of the underlying autoimmune disease.
- Pneumoconiosis: ILD caused by inhalation of mineral dusts (e.g., silica, coal dust). The specific type depends on the inhaled dust.
Differentiating between these ILDs is crucial for appropriate management, as treatment strategies vary significantly.
Q 3. Explain the diagnostic approach to ILD, including imaging and pulmonary function tests.
Diagnosing ILD requires a multidisciplinary approach involving clinical evaluation, imaging studies, and pulmonary function tests (PFTs). It’s a process of exclusion, aiming to identify the specific type of ILD.
- Clinical History and Physical Examination: This includes a detailed assessment of symptoms (shortness of breath, cough, fatigue), risk factors (environmental exposures, family history), and physical findings (crackles on lung auscultation).
- High-Resolution Computed Tomography (HRCT) of the Chest: HRCT is the cornerstone of ILD imaging. It provides detailed images of the lung parenchyma, revealing patterns of interstitial lung changes characteristic of different ILDs (e.g., ground-glass opacities, honeycombing). This helps to differentiate between different types of ILDs, such as IPF and other interstitial lung diseases.
- Pulmonary Function Tests (PFTs): PFTs assess lung volumes, airflow, and gas exchange. In ILD, typical findings include reduced lung volumes (restrictive pattern), impaired diffusion capacity (DLCO), and decreased oxygen saturation. These tests quantitatively measure the severity of lung damage.
- Bronchoalveolar Lavage (BAL): This procedure involves washing the airways to collect fluid and cells, which can provide information about the inflammatory response in the lungs. Analysis of this fluid helps characterize the type of inflammatory cells present, aiding in diagnosis.
- Surgical Lung Biopsy: In some cases, a surgical lung biopsy is needed to obtain a tissue sample for definitive diagnosis, particularly when imaging findings are ambiguous or when treatment decisions depend on a precise histological diagnosis.
The combination of these tests guides the clinician towards a specific diagnosis and helps formulate an appropriate treatment strategy.
Q 4. Discuss the role of high-resolution computed tomography (HRCT) in ILD diagnosis.
High-resolution computed tomography (HRCT) is indispensable in ILD diagnosis. It provides far greater detail than conventional chest X-rays, allowing visualization of the interstitial lung tissue. The characteristic patterns of interstitial changes seen on HRCT are crucial for differentiating between various types of ILDs.
- Identifying specific patterns: HRCT reveals patterns such as ground-glass opacities (areas of increased lung density), honeycombing (cystic spaces formed by the destruction of lung tissue), traction bronchiectasis (dilation of the airways due to lung scarring), and reticulation (a network of fine lines throughout the lung). These patterns are highly suggestive of specific ILDs. For instance, the presence of honeycombing is strongly associated with IPF.
- Assessing disease extent and severity: HRCT allows for a visual assessment of the extent and distribution of lung involvement, providing a measure of disease severity. This helps in staging the disease and monitoring its progression.
- Guiding biopsy decisions: HRCT can identify areas of characteristic lung involvement that may be suitable for biopsy, maximizing the yield of diagnostic information. This is particularly important if imaging findings are ambiguous.
While HRCT is a crucial tool, it’s important to remember it’s not definitive. It needs to be correlated with clinical findings, PFTs, and potentially a lung biopsy for a precise diagnosis.
Q 5. Interpret the results of a pulmonary function test suggestive of ILD.
Pulmonary function test results suggestive of ILD typically show a restrictive pattern, reflecting reduced lung volumes. This is because the fibrosis and inflammation in the lung tissue restrict lung expansion.
- Reduced Forced Vital Capacity (FVC): This indicates a decreased total amount of air that can be exhaled after a maximal inhalation. This finding reflects the overall limitation in lung expansion.
- Reduced Total Lung Capacity (TLC): This reflects the total volume of air the lungs can hold. This reduction indicates that the lungs cannot fully expand.
- Reduced Diffusing Capacity of the Lung for Carbon Monoxide (DLCO): This measurement reflects the efficiency of gas exchange across the alveolar-capillary membrane. A decreased DLCO indicates impaired gas exchange due to the thickened alveolar walls and decreased surface area for gas exchange.
- Normal or slightly reduced FEV1/FVC ratio: Unlike obstructive lung diseases (like asthma or COPD), the ratio of forced expiratory volume in one second (FEV1) to FVC is usually normal or only mildly reduced in ILD, distinguishing it from obstructive diseases.
The degree of reduction in these parameters reflects the severity of lung involvement. It’s important to remember that PFTs alone are not diagnostic of ILD but, in conjunction with HRCT and other clinical data, they contribute significantly to diagnosis and monitoring.
Q 6. Outline the current treatment guidelines for IPF.
Treatment for IPF aims to slow disease progression and improve quality of life. Currently, antifibrotic medications are the cornerstone of IPF management, along with supportive care measures.
- Antifibrotic Medications: Pirfenidone and nintedanib are the two FDA-approved antifibrotic agents for IPF. These medications work to reduce the progression of fibrosis in the lungs.
- Supportive Care: This includes oxygen therapy to alleviate hypoxemia, pulmonary rehabilitation to improve exercise capacity and quality of life, and management of symptoms such as cough and shortness of breath.
- Anti-inflammatory Therapy: While generally not the primary treatment for IPF, some patients may benefit from short courses of corticosteroids or other immunosuppressants if there’s a significant inflammatory component.
- Lung Transplantation: For patients with severe, rapidly progressing IPF who are not responding to medical therapy, lung transplantation may be considered, however, it is a major surgery with risks and complications.
Treatment decisions are individualized based on the patient’s disease severity, functional capacity, and overall health status. Regular monitoring is crucial to assess treatment response and adjust the therapeutic strategy as needed.
Q 7. Describe the mechanism of action of antifibrotic medications used in ILD.
The antifibrotic medications used in ILD, primarily pirfenidone and nintedanib, work through different mechanisms to reduce fibrosis, though the exact mechanisms are not fully elucidated.
- Pirfenidone: The precise mechanism isn’t fully understood but is believed to involve multiple pathways. It may inhibit transforming growth factor-beta (TGF-β), a key cytokine involved in fibrosis. It also has anti-inflammatory and antioxidant properties, which may contribute to its overall benefit in slowing disease progression.
- Nintedanib: This is a tyrosine kinase inhibitor that targets multiple growth factors involved in fibrosis, including platelet-derived growth factor (PDGF), fibroblast growth factor (FGF), and vascular endothelial growth factor (VEGF). By inhibiting these growth factors, nintedanib aims to reduce the excessive production of extracellular matrix and the activation of fibroblasts, thereby slowing fibrosis.
Both medications aim to slow the progression of IPF, not reverse it. They are typically well-tolerated, although side effects can occur, which vary in frequency and severity. Regular monitoring for side effects is crucial.
Q 8. Discuss the potential side effects of antifibrotic agents.
Antifibrotic agents, while crucial in slowing the progression of Interstitial Lung Disease (ILD), can cause several side effects. These vary depending on the specific medication but generally fall into categories of gastrointestinal, dermatologic, and hepatic effects.
- Gastrointestinal: Nausea, vomiting, diarrhea, and abdominal pain are common, particularly in the early stages of treatment. For example, a patient might experience persistent nausea requiring adjustment of the medication dosage or timing.
- Dermatologic: Rash, pruritus (itching), and photosensitivity are potential skin-related side effects. We often counsel patients to use sunscreen liberally and report any skin changes immediately.
- Hepatic: Elevations in liver enzymes are a concern and necessitate regular liver function tests (LFTs). In some cases, treatment might need to be stopped or adjusted to prevent liver damage. We carefully monitor LFTs and adjust the treatment plan accordingly to minimize risk.
- Other: Less common but potentially serious side effects include increased risk of infection, myopathy (muscle weakness), and interstitial pneumonitis (inflammation of the lung tissue). Close monitoring and prompt intervention are vital if these occur.
It’s important to remember that these side effects are not inevitable. Many patients tolerate antifibrotic medications well. However, open communication between the patient and their healthcare team is crucial to manage any side effects effectively and ensure adherence to treatment.
Q 9. Explain the role of pulmonary rehabilitation in ILD management.
Pulmonary rehabilitation plays a vital role in improving the quality of life for ILD patients. It’s a comprehensive program that includes exercise training, education, and psychosocial support. Think of it as a personalized fitness plan designed to maximize lung function and overall well-being.
- Exercise Training: Tailored exercise programs, including aerobic exercises (like walking or cycling) and strength training, improve respiratory muscle strength and endurance, increasing the patient’s ability to perform daily activities.
- Education: Patients learn about their condition, medication management, breathing techniques, and energy conservation strategies. This empowers them to actively participate in their care.
- Psychosocial Support: Addressing the emotional and psychological impact of ILD is crucial. Support groups and counseling can provide emotional support and coping mechanisms to improve overall well-being.
For instance, a patient struggling with shortness of breath during everyday activities can learn breathing exercises and energy-conservation techniques through pulmonary rehabilitation, significantly improving their daily life.
Q 10. How do you counsel patients and their families about the prognosis of ILD?
Counseling patients and their families about the prognosis of ILD is a sensitive and challenging aspect of care. It requires empathy, honesty, and a tailored approach based on the individual’s disease severity and response to treatment.
We start by explaining the nature of ILD in simple terms, avoiding medical jargon. We then discuss the individual’s specific diagnosis and disease stage, explaining the potential trajectory of the disease. We use clear and realistic language, acknowledging the uncertainty inherent in predicting the future.
We always emphasize the importance of proactive management through medication, pulmonary rehabilitation, and lifestyle adjustments. We discuss treatment goals, focusing on improving quality of life rather than solely on extending life expectancy. We encourage patients to actively participate in decision-making and empower them to take control of their care.
Open communication and a supportive environment are vital. We encourage questions and offer resources such as support groups and palliative care services as needed. For example, with a patient facing a more advanced stage, we might introduce palliative care early to ensure comprehensive symptom management and emotional support.
Q 11. Describe the challenges in managing patients with advanced ILD.
Managing patients with advanced ILD presents numerous challenges. The disease’s progressive nature, coupled with significant respiratory compromise, necessitates a multidisciplinary approach.
- Respiratory Failure: As the disease progresses, patients may experience severe shortness of breath and require supplemental oxygen or even mechanical ventilation.
- Right Heart Failure (Cor Pulmonale): The increased pressure in the pulmonary arteries can lead to right heart failure, requiring specialized cardiac management.
- Infections: Patients with advanced ILD are at increased risk of infections due to impaired lung function and immune response.
- Symptom Management: Managing symptoms like dyspnea (shortness of breath), cough, and pain requires a nuanced approach, often involving multiple medications and interventions.
- End-of-Life Care: Decisions about end-of-life care become increasingly important as the disease progresses, requiring sensitive discussions with the patient and family.
For example, we might need to coordinate care between pulmonologists, cardiologists, infectious disease specialists, and palliative care teams to manage the complex needs of a patient with advanced ILD.
Q 12. What are the indications for lung transplantation in ILD?
Lung transplantation is a potentially life-saving option for patients with advanced ILD who meet specific criteria. The primary indication is end-stage ILD refractory to medical therapy, meaning the disease is severely impairing lung function and is not responding to other treatments.
Specific criteria include:
- Severe respiratory failure despite optimal medical management
- Significant impairment of quality of life
- Suitable overall health status to undergo the rigorous procedure and post-transplant recovery
- Absence of contraindications such as severe cardiovascular disease or active infection.
Essentially, lung transplant is considered when the benefits of transplantation outweigh the risks of the procedure and the alternative is a poor prognosis with significantly diminished quality of life.
Q 13. How do you assess the suitability of a patient for lung transplantation?
Assessing a patient’s suitability for lung transplantation is a complex process involving a multidisciplinary team. The evaluation considers numerous factors to ensure that the patient has a reasonable chance of successful transplantation and long-term survival.
- Pulmonary Function Tests (PFTs): These assess the severity of lung damage and determine the patient’s eligibility.
- Cardiac Evaluation: A thorough cardiac workup rules out any significant heart disease that could compromise the outcome of the transplant.
- Infectious Disease Screening: Extensive screening is done to ensure the absence of any active infections.
- Psychosocial Evaluation: This assesses the patient’s psychological preparedness for the demands of transplantation and long-term immunosuppression.
- Oncological Evaluation: A thorough cancer screening is performed to exclude malignancy as a cause of the ILD.
The team weighs the potential benefits against the risks, including the surgical risks, the need for lifelong immunosuppression, and the possibility of rejection. Only patients who meet strict criteria and have a favorable risk-benefit profile are considered candidates.
Q 14. Explain the importance of oxygen therapy in ILD.
Oxygen therapy is a cornerstone of ILD management, particularly in patients with hypoxemia (low blood oxygen levels). It improves oxygen saturation, alleviates symptoms like shortness of breath, and can improve overall quality of life.
Oxygen therapy can be administered in several ways, from simple nasal cannulas to more complex systems like high-flow nasal cannulas or ventilators. The specific method depends on the severity of the hypoxemia and the patient’s individual needs.
For instance, a patient with significant shortness of breath at rest may benefit from continuous oxygen therapy at home, improving their ability to perform daily tasks. Even a moderate improvement in oxygen levels can significantly impact the patient’s well-being and reduce breathlessness.
Regular monitoring of blood oxygen levels is necessary to adjust oxygen therapy as needed. This ensures optimal oxygenation while minimizing potential side effects. The goal is to improve oxygenation without suppressing the patient’s drive to breathe, which can be detrimental in long term.
Q 15. Discuss the role of supportive care in managing ILD.
Supportive care in Interstitial Lung Disease (ILD) management is crucial, focusing on improving quality of life and managing symptoms rather than directly curing the underlying disease. It’s the cornerstone of care, often complementing disease-modifying therapies where available.
Oxygen Therapy: Supplemental oxygen is essential for patients experiencing hypoxemia (low blood oxygen levels), improving exercise tolerance and overall well-being. We carefully monitor oxygen saturation levels and adjust therapy as needed. For example, a patient with severe ILD might require continuous oxygen, while another with milder disease might only need it during exertion.
Pulmonary Rehabilitation: This comprehensive program involves exercise training, education, and psychological support. It helps patients improve their lung function, physical endurance, and quality of life. I’ve seen patients regain a significant amount of independence and reduce their dyspnea (shortness of breath) through dedicated pulmonary rehab.
Medication for Symptom Management: This can include bronchodilators to relax airway muscles and reduce breathlessness, cough suppressants, and medications to manage other symptoms like gastroesophageal reflux disease (GERD), which is often associated with ILD. Careful consideration of potential drug interactions is paramount.
Nutritional Support: Maintaining adequate nutrition is vital for patients with ILD, as the disease can lead to weight loss and malnutrition. Dietitian consultations can provide personalized dietary plans to maximize calorie intake and nutrient absorption. For instance, we might recommend small, frequent meals to avoid fatigue during eating.
Vaccination: Protecting patients from infections is critical. We strongly encourage influenza and pneumococcal vaccinations to minimize the risk of exacerbations.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Describe your experience in managing ILD-related complications.
My experience in managing ILD-related complications is extensive. These complications are often life-threatening and require prompt and decisive intervention.
Acute Exacerbations: I’ve managed numerous acute exacerbations, often requiring hospitalization, intravenous corticosteroids, and close monitoring of respiratory function. Early recognition and aggressive management are key to improving outcomes. One memorable case involved a patient who presented with sudden worsening dyspnea and hypoxemia; prompt intervention with high-flow oxygen and intravenous corticosteroids prevented respiratory failure.
Pulmonary Hypertension: This serious complication requires careful monitoring and management with medications like pulmonary vasodilators. We often collaborate with cardiologists to optimize treatment strategies. I’ve worked closely with cardiologists to tailor treatment plans based on individual patient needs, improving their quality of life and extending survival.
Infections: ILD patients are at increased risk of respiratory infections, which can trigger exacerbations. Prompt diagnosis and treatment with appropriate antibiotics are crucial. Careful monitoring for signs and symptoms is essential for early intervention.
Cardiac Complications: ILD can impact cardiac function, requiring collaboration with cardiologists for comprehensive management. Careful monitoring of cardiac parameters is necessary.
Psychological Impact: The chronic nature of ILD can significantly affect patients’ mental health. We regularly assess patients for anxiety and depression and offer appropriate support or referral to mental health professionals. Incorporating psychological support into the treatment plan significantly improves patient compliance and overall well-being.
Q 17. How do you approach a patient with suspected ILD but inconclusive diagnostic findings?
When a patient presents with suspected ILD but inconclusive diagnostic findings, a careful and systematic approach is essential. This often involves a process of elimination and careful consideration of other possible diagnoses.
Thorough History and Physical Examination: This helps identify potential risk factors and clinical clues, guiding further investigations. We obtain detailed information about symptoms, exposure to environmental factors (e.g., dust, asbestos), family history, and any other relevant medical conditions.
High-Resolution Computed Tomography (HRCT) Scan of the Chest: This is the most important imaging modality for ILD, though it’s not always definitive. We look for characteristic patterns suggestive of different types of ILD. However, HRCT findings can sometimes be nonspecific and require additional testing.
Pulmonary Function Tests (PFTs): These tests assess lung volumes and airflow, providing valuable information about the extent and severity of lung involvement. Typical findings include restrictive or mixed restrictive/obstructive patterns. However, PFTs alone cannot diagnose ILD.
Blood Tests: We perform various blood tests to rule out other conditions and screen for autoimmune diseases frequently associated with ILD. This might include autoantibody testing and inflammatory markers.
Bronchoscopy with Bronchoalveolar Lavage (BAL): In selected cases, we might perform a bronchoscopy to obtain a sample of lung tissue for analysis (transbronchial biopsy) or fluid from the alveoli (BAL). This can help determine the underlying cause of ILD, but carries risks and isn’t always conclusive.
Surgical Lung Biopsy: This is considered when other diagnostic methods are inconclusive. It involves obtaining a tissue sample for detailed pathological examination, providing the most definitive diagnosis. This is an invasive procedure and the last resort due to its risks.
Ultimately, the diagnostic approach is tailored to each patient, taking into account their clinical presentation, risk factors, and the availability of resources.
Q 18. Discuss your familiarity with current research and clinical trials in ILD.
I maintain a strong awareness of the latest research and clinical trials in ILD. This involves actively participating in professional societies, attending conferences, and regularly reviewing relevant medical literature.
Novel Therapeutics: I’m familiar with ongoing research into novel therapies targeting various mechanisms involved in ILD pathogenesis, including antifibrotic agents and immunomodulators. Many clinical trials are evaluating these new treatments for various forms of ILD.
Biomarkers: Research into identifying specific biomarkers to aid in early diagnosis, prognosis, and treatment monitoring is actively progressing. This could revolutionize ILD management in the future.
Personalized Medicine: The field is moving toward a more personalized approach, tailoring treatment strategies to individual patients based on their specific genetic profile and disease characteristics. This area is very active in research.
Genetic Studies: Significant progress is being made in understanding the genetic basis of ILD, identifying susceptibility genes and providing insights into disease mechanisms.
Keeping abreast of these developments allows me to provide my patients with the most up-to-date and effective treatment options.
Q 19. How do you stay updated on the latest advancements in ILD management?
Staying updated on advancements in ILD management is a continuous process. I utilize several strategies to ensure my knowledge remains current.
Membership in Professional Organizations: Active participation in organizations like the American Thoracic Society (ATS) and the European Respiratory Society (ERS) provides access to cutting-edge research, guidelines, and educational materials.
Regular Review of Medical Literature: I consistently review peer-reviewed journals, such as the American Journal of Respiratory and Critical Care Medicine and the European Respiratory Journal, to stay informed about new findings.
Attendance at Conferences and Meetings: I regularly attend national and international conferences to learn about the latest research and treatment approaches directly from leading experts in the field.
Continuing Medical Education (CME) Activities: I actively participate in CME programs to obtain continuing education credits and enhance my knowledge and skills.
Collaboration with Colleagues: Regular discussions and collaboration with colleagues in pulmonology and related specialties ensure a multidisciplinary approach and facilitate knowledge sharing.
Q 20. Describe a challenging case involving ILD management and how you approached it.
One challenging case involved a young woman with rapidly progressive ILD of unknown etiology. Initial investigations including HRCT and PFTs revealed severe restrictive lung disease, but bronchoscopy with BAL and transbronchial biopsy were inconclusive.
The challenge was the rapid progression of her disease, despite aggressive supportive care. We explored various diagnostic possibilities, including autoimmune disorders and genetic testing. Eventually, after a period of several months and through collaboration with a multidisciplinary team, a surgical lung biopsy was performed, revealing a rare form of ILD requiring a highly specialized treatment plan. This case highlighted the importance of persistence in diagnosis and close collaboration with other specialists to ultimately identify and implement the best course of action. The patient responded well to the tailored treatment, and her progress showcased the power of multidisciplinary collaboration and comprehensive patient care.
Q 21. What are your strengths and weaknesses related to ILD management?
My strengths in ILD management include a deep understanding of the complexities of the disease, a comprehensive approach to diagnosis and treatment, and the ability to effectively collaborate with multidisciplinary teams. I am adept at interpreting complex diagnostic data and tailoring treatment strategies to individual patients. My strong communication skills allow for effective patient and family education, fostering trust and adherence to treatment plans.
My area for ongoing development is staying current with the ever-expanding body of research on the genetic underpinnings of ILD and applying the latest genomic knowledge to refine diagnostic and therapeutic strategies. I am actively addressing this by pursuing advanced training in genomic medicine and collaborating with researchers in this field.
Q 22. How do you collaborate with other healthcare professionals in managing ILD?
Managing Interstitial Lung Disease (ILD) is a highly collaborative effort. I work closely with a multidisciplinary team, including pulmonologists, respiratory therapists, nurses, physiotherapists, dieticians, and often specialists like cardiologists or rheumatologists, depending on the patient’s specific needs.
- Pulmonologists: They provide expertise in diagnosing and managing ILD, often leading the treatment plan.
- Respiratory Therapists: They play a crucial role in assessing respiratory function, administering oxygen therapy, and educating patients on breathing techniques.
- Nurses: Provide vital patient education, administer medications, and monitor for potential complications.
- Physiotherapists: Help improve lung function and overall physical fitness through tailored exercise programs.
- Dieticians: Provide nutritional guidance to support optimal lung health and manage any associated weight loss.
- Other Specialists: If the ILD is related to another condition (like rheumatoid arthritis or scleroderma), collaboration with these specialists is essential for holistic care.
Regular team meetings, shared patient portals, and detailed communication through progress notes in the EHR ensure everyone is informed and working towards the same goals. For example, if a patient experiences a sudden decline in their oxygen saturation levels, I immediately consult the respiratory therapist for adjustments to oxygen therapy and the nurse for a comprehensive assessment.
Q 23. Describe your experience with electronic health records (EHRs) in managing ILD patients.
Electronic Health Records (EHRs) are indispensable in managing ILD patients. I use the EHR to track vital signs, pulmonary function test results (like FVC and DLCO), imaging data (HRCT scans), medication records, and progress notes. This allows for a comprehensive longitudinal view of each patient’s disease progression.
The EHR’s features facilitate efficient communication. For instance, I can quickly share imaging results and laboratory reports with other members of the healthcare team, ensuring timely interventions. The integrated messaging system facilitates prompt communication with patients and other healthcare professionals. Moreover, I can utilize EHR functionalities to monitor patients remotely, checking on key metrics and providing appropriate support.
However, challenges exist. Data entry can be time-consuming, and the sheer volume of information can sometimes be overwhelming. Ensuring data accuracy and integration with other systems is critical for seamless workflow. The EHR also necessitates careful management of patient privacy and data security.
Q 24. How do you ensure patient safety and quality of care in ILD management?
Patient safety and quality of care are paramount in ILD management. We achieve this through a multi-pronged approach:
- Regular Monitoring: Closely monitoring vital signs, oxygen saturation levels, and respiratory function allows for early detection of exacerbations or adverse effects from medications.
- Evidence-Based Practice: We adhere to the latest evidence-based guidelines for diagnosing and treating ILD, ensuring optimal outcomes and minimizing potential risks.
- Medication Management: Careful medication reconciliation, including education on potential side effects and interactions, helps reduce medication errors and adverse reactions.
- Patient Education: Empowering patients with knowledge about their disease, treatment options, and potential complications helps improve adherence and self-management skills.
- Infection Prevention: Implementing stringent infection control protocols to reduce the risk of pneumonia, a serious complication of ILD.
- Risk Assessment and Prevention: Proactive identification and mitigation of risks such as falls and malnutrition are crucial to prevent complications and improve quality of life.
For example, we carefully monitor patients on immunosuppressants for signs of infection and promptly intervene with appropriate treatment. We also conduct regular fall risk assessments for our elderly patients to provide assistive devices or modify their environment to enhance safety.
Q 25. How do you address ethical considerations in the treatment of ILD patients?
Ethical considerations in ILD management are complex and multifaceted. Key aspects include:
- Informed Consent: Ensuring patients fully understand their diagnosis, treatment options, potential benefits, risks, and alternatives before making decisions.
- Beneficence and Non-Maleficence: Striving to do good and avoid harm by carefully weighing the potential benefits and risks of each treatment.
- Justice and Equity: Ensuring fair and equitable access to high-quality care for all patients, regardless of their socioeconomic background or other factors.
- Confidentiality: Protecting patient privacy and maintaining confidentiality throughout the course of treatment.
- End-of-Life Care: Addressing the emotional and physical needs of patients nearing the end of life and supporting their families.
A difficult ethical dilemma arises when considering high-cost therapies with uncertain long-term benefits. In these cases, transparent discussions with the patient and their family about the benefits, risks, and costs are paramount, enabling a shared decision-making process based on their values and preferences. I always involve the ethics committee when facing challenging ethical situations.
Q 26. Discuss your approach to shared decision-making with ILD patients.
Shared decision-making is central to my approach with ILD patients. I believe that patients should be active participants in their care. I start by providing clear and concise information about their diagnosis, prognosis, and treatment options in a way they can understand.
I then encourage patients to share their preferences, concerns, and goals. This information is vital in tailoring a treatment plan that aligns with their individual needs and values. For example, a patient might prioritize maintaining their quality of life, even if it means accepting a slightly higher risk of disease progression. Understanding this preference helps in collaboratively selecting the most appropriate course of action.
I use decision aids, such as shared decision-making tools or brochures, to facilitate the process. We discuss the pros and cons of different treatments, including potential side effects and lifestyle implications. Ultimately, the treatment plan is a collaborative agreement, respecting patient autonomy and shared responsibility for achieving the best possible outcomes.
Q 27. What are the common causes of acute exacerbations in ILD, and how do you manage them?
Acute exacerbations of ILD are a significant concern, often leading to hospitalization and increased mortality. Common causes include:
- Infection: Pneumonia is a major trigger, often requiring aggressive antibiotic treatment.
- Medication Side Effects: Certain medications can exacerbate underlying lung inflammation.
- Environmental Factors: Exposure to pollutants or allergens can trigger an exacerbation.
- Unknown Causes: In some cases, the precise cause remains unclear.
Management of acute exacerbations is multifaceted and may include:
- Supplemental Oxygen: To improve oxygenation.
- Antibiotics: If an infection is present.
- Corticosteroids: To reduce inflammation.
- Bronchodilators: To help open the airways.
- Mechanical Ventilation: In severe cases requiring respiratory support.
Early recognition of symptoms (like increased shortness of breath, cough, and fever) is crucial. Prompt medical attention and aggressive treatment can significantly improve outcomes.
Q 28. Describe your understanding of the impact of ILD on patients’ quality of life.
ILD significantly impacts patients’ quality of life. The progressive nature of the disease, coupled with breathlessness, fatigue, and cough, can profoundly affect their physical functioning, emotional well-being, and social participation.
Many patients experience reduced exercise capacity and difficulty performing daily activities. This can lead to social isolation, anxiety, and depression. The uncertainty surrounding the disease’s progression and the potential for life-threatening complications can also significantly impact their mental health. Therefore, a holistic approach to management is crucial, incorporating psychological support, pulmonary rehabilitation, and strategies to enhance their overall quality of life. Regular assessments using validated quality-of-life questionnaires provide a quantifiable measure of the impact of the disease and the effectiveness of interventions.
For example, we might refer a patient to a support group to connect with others facing similar challenges and provide emotional support. Pulmonary rehabilitation programs help patients improve their exercise capacity and regain independence in daily tasks. We also encourage the use of assistive devices and discuss strategies for effective symptom management.
Key Topics to Learn for Interstitial Lung Disease Management Interview
- Disease Pathophysiology: Understanding the diverse range of ILDs, their underlying mechanisms, and the common pathways of inflammation and fibrosis.
- Diagnostic Approaches: Mastering the interpretation of pulmonary function tests (PFTs), high-resolution computed tomography (HRCT) scans, and bronchoalveolar lavage (BAL) findings in diagnosing ILD.
- Treatment Strategies: Familiarize yourself with current guidelines and evidence-based treatments, including anti-fibrotic therapies, immunosuppressants, and supportive care.
- Practical Application: Case Studies: Practice analyzing clinical scenarios, formulating differential diagnoses, and developing personalized treatment plans for patients with various ILD subtypes.
- Monitoring Disease Progression: Learn to interpret clinical and imaging data to assess treatment response and identify disease progression.
- Patient Communication and Counseling: Develop skills in effectively communicating complex medical information to patients and their families, addressing their concerns and providing emotional support.
- Research and Emerging Therapies: Stay updated on the latest research findings and emerging therapies in the field of ILD management. Understanding clinical trials and their methodologies is beneficial.
- Ethical Considerations: Be prepared to discuss ethical dilemmas related to patient care, resource allocation, and end-of-life decisions in the context of ILD.
Next Steps
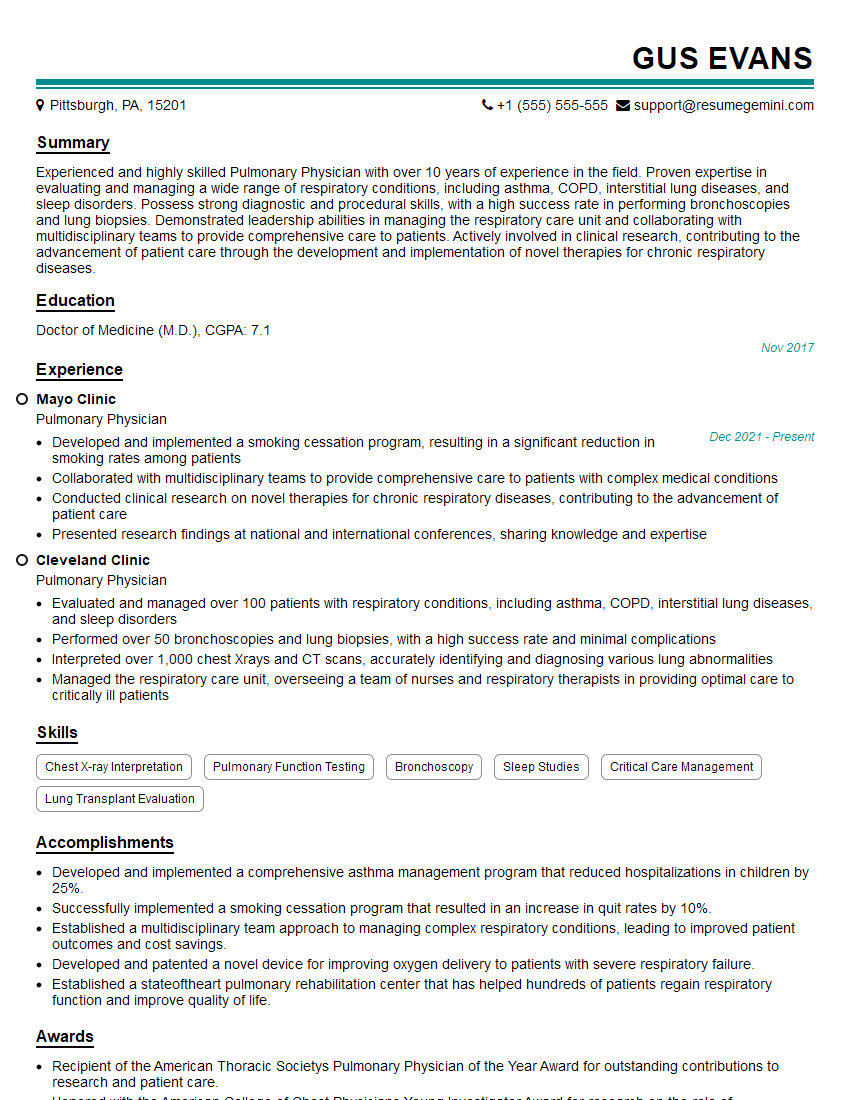
Mastering Interstitial Lung Disease Management significantly enhances your career prospects, opening doors to specialized roles and leadership opportunities within respiratory medicine. A strong resume is crucial for showcasing your expertise and securing your ideal position. To maximize your job search success, create an ATS-friendly resume that highlights your relevant skills and experience. ResumeGemini is a trusted resource for building professional, impactful resumes. Leverage their tools and resources to craft a compelling resume that showcases your qualifications. Examples of resumes tailored to Interstitial Lung Disease Management are available to help guide you.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hi, I have something for you and recorded a quick Loom video to show the kind of value I can bring to you.
Even if we don’t work together, I’m confident you’ll take away something valuable and learn a few new ideas.
Here’s the link: https://bit.ly/loom-video-daniel
Would love your thoughts after watching!
– Daniel
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.