Cracking a skill-specific interview, like one for Rheumatologic Rehabilitation, requires understanding the nuances of the role. In this blog, we present the questions you’re most likely to encounter, along with insights into how to answer them effectively. Let’s ensure you’re ready to make a strong impression.
Questions Asked in Rheumatologic Rehabilitation Interview
Q 1. Describe your experience managing patients with rheumatoid arthritis.
Managing rheumatoid arthritis (RA) requires a holistic approach encompassing medication management, physical therapy, and psychosocial support. My experience involves collaborating closely with rheumatologists to optimize medication regimens, tailoring them to individual patient needs and responses. I focus on assessing disease activity through measures like the Disease Activity Score (DAS28) and the Clinical Disease Activity Index (CDAI) to monitor treatment effectiveness. For instance, I recently worked with a patient whose RA was poorly controlled despite medication. By collaborating with her rheumatologist, we adjusted her treatment plan and incorporated specific exercises targeting her affected joints. This led to a significant reduction in pain and improved joint function, demonstrated by a decrease in her DAS28 score.
Beyond medication, a crucial aspect is functional rehabilitation. This includes targeted exercises to improve range of motion, strength, and endurance, alongside education on joint protection strategies and energy conservation techniques. I also incorporate ergonomic assessments to modify daily tasks and minimize joint stress. For example, I helped a patient adapt her kitchen setup to reduce strain on her hands and wrists while cooking.
Q 2. Explain your approach to patient education regarding disease management.
Patient education is central to successful RA management. My approach uses a combination of methods tailored to individual learning styles and preferences. I start with clear, concise explanations of the disease process, its impact on the body, and the rationale behind treatment plans. I use visual aids like diagrams and models to illustrate complex concepts. We discuss realistic goals and expectations, addressing concerns and anxieties about the condition.
I encourage active participation, encouraging patients to ask questions and express their concerns openly. I provide written materials summarizing key information, including exercise plans and joint protection strategies. I leverage technology by offering online resources and educational videos. Follow-up sessions are crucial to reinforce learning, address any emerging questions, and adjust the education plan based on patient progress and needs. For example, I created a personalized exercise booklet for a patient with limited literacy, using pictures and simple instructions to help them understand and perform the exercises.
Q 3. How do you assess a patient’s functional limitations in Rheumatology?
Assessing functional limitations in rheumatology involves a multi-faceted approach combining self-reported measures, observation, and objective assessments. Self-reported questionnaires, such as the Health Assessment Questionnaire (HAQ) and the Functional Assessment of Chronic Illness Therapy (FACIT)-Fatigue scale, provide valuable insights into a patient’s perceived limitations in daily activities.
Observation during functional tasks, such as getting dressed or walking, helps to identify difficulties and compensations. Objective assessments, including range of motion measurements (using goniometry), grip strength testing (using a dynamometer), and timed tests like the Timed Up and Go (TUG) test, provide quantifiable data on physical performance. Combining these methods offers a comprehensive understanding of a patient’s functional capacity and limitations, guiding the development of targeted rehabilitation interventions. For example, a patient with severe hand pain might score high on the HAQ and exhibit decreased grip strength during testing, indicating a significant functional limitation in daily tasks requiring dexterity.
Q 4. What therapeutic interventions are most effective for osteoarthritis pain?
Osteoarthritis (OA) pain management relies on a combination of pharmacological and non-pharmacological approaches. Non-pharmacological interventions often take precedence, focusing on weight management (if overweight or obese), regular low-impact exercise (such as walking or swimming), and physical therapy to improve joint mobility and strength.
Pharmacological interventions include topical analgesics (like NSAIDs creams), oral analgesics (such as acetaminophen), and, in some cases, oral NSAIDs or other disease-modifying osteoarthritis drugs (DMOADs). Intra-articular injections of corticosteroids or hyaluronic acid may be considered for short-term relief in severely affected joints. It is crucial to consider individual patient factors, comorbidities, and preferences when choosing the most appropriate treatment plan. For example, a patient with mild OA and limited mobility might benefit most from a program of supervised exercise and topical analgesics, while a patient with severe OA and significant pain might require a combination of oral analgesics and intra-articular injections alongside physical therapy.
Q 5. How do you incorporate patient-centered care into your Rheumatologic Rehabilitation practice?
Patient-centered care in rheumatologic rehabilitation emphasizes shared decision-making, respecting individual preferences, and tailoring interventions to meet specific needs and goals. I start each patient encounter by actively listening to understand their concerns, priorities, and expectations. This involves exploring their lifestyle, social support system, and perceived barriers to rehabilitation.
Treatment plans are collaboratively developed, ensuring the patient feels empowered and involved in the process. Regular communication and feedback loops allow for adjustments to the plan based on patient progress and responses. For instance, a patient might prefer home-based exercises over clinic-based sessions; this preference is accommodated by designing a personalized home exercise program with regular check-ins. Empowering patients to take an active role in their care improves adherence and ultimately enhances the effectiveness of the rehabilitation process.
Q 6. Discuss the role of exercise therapy in managing inflammatory arthritis.
Exercise therapy plays a vital role in managing inflammatory arthritis, particularly in reducing pain, improving joint function, and increasing physical capacity. However, the type and intensity of exercise must be carefully tailored to the individual’s disease activity and functional status. During periods of high inflammation, low-impact activities, such as aquatic therapy or gentle range-of-motion exercises, are preferred.
As inflammation subsides, the program can gradually progress to incorporate more strength-training exercises and aerobic conditioning. It’s crucial to emphasize joint protection techniques to minimize stress on inflamed joints and prevent further damage. Examples include using proper body mechanics during daily activities and avoiding high-impact movements. Regular monitoring of pain levels and disease activity ensures the exercise plan remains safe and effective, preventing exacerbations. For example, a patient with active rheumatoid arthritis might start with aquatic therapy, followed by low-impact exercises, and finally progress to gentle strength training, always maintaining a close eye on pain levels and avoiding excessive joint strain.
Q 7. Describe your experience with assistive devices and adaptive techniques.
My experience with assistive devices and adaptive techniques involves a thorough assessment of a patient’s functional needs and limitations to identify appropriate solutions. This begins by identifying specific difficulties a patient encounters in their daily routines. For example, a patient with decreased hand dexterity might struggle with opening jars, while a patient with limited mobility might have trouble getting up from a chair.
Based on this assessment, I recommend and train patients on the use of various assistive devices, such as adaptive eating utensils, reachers, adaptive clothing fasteners, and mobility aids like walkers or canes. I also incorporate adaptive techniques into daily activities to facilitate easier and safer performance. For instance, I teach patients how to use adaptive strategies to get dressed without excessive joint stress, modifying techniques to reduce strain and protect their joints. Regular follow-up ensures the devices and techniques remain appropriate and effective, making necessary adjustments as the patient’s condition evolves or needs change.
Q 8. How do you measure and track patient progress in Rheumatologic Rehabilitation?
Measuring progress in rheumatologic rehabilitation is a multifaceted process requiring a blend of objective and subjective assessments. We utilize a variety of tools to track improvements.
- Functional Assessments: We use standardized questionnaires like the Health Assessment Questionnaire (HAQ) to quantify a patient’s ability to perform daily activities. Changes in HAQ scores over time reflect improvements in functional capacity. We also perform practical assessments, observing the patient’s range of motion, strength, and ability to perform specific tasks, such as dressing or walking. For example, I might time a patient completing a set of stairs at their first visit and compare it to subsequent visits.
- Pain Scales: Visual Analog Scales (VAS) and Numerical Rating Scales (NRS) allow patients to rate their pain levels, providing a quantitative measure of pain reduction. A patient might report pain at a 7/10 initially, and we track how this number changes as their treatment progresses.
- Laboratory Tests: While not directly measuring functional improvement, inflammatory markers like ESR and CRP can indirectly reflect disease activity and response to treatment. We track these to ensure the underlying disease process is improving.
- Patient-Reported Outcomes Measures (PROMs): These questionnaires delve into patient’s perceptions of their overall health, well-being, and quality of life. They provide valuable insights into the holistic impact of rehabilitation.
Tracking these measures over time allows for a comprehensive view of patient progress, enabling us to adjust treatment plans as needed. For instance, if a patient’s pain scores improve but their functional capacity remains stagnant, we might focus on strengthening exercises. Regular monitoring ensures that our interventions are effective and tailored to the individual patient’s needs.
Q 9. What are the common challenges faced by patients with lupus, and how do you address them?
Patients with lupus face a unique set of challenges due to the systemic nature of the disease. These challenges often intersect and impact quality of life significantly.
- Fatigue: Overwhelming fatigue is a hallmark symptom, impacting daily activities, work productivity, and social interactions. We address this through pacing strategies, energy conservation techniques, and referral to occupational therapy for adaptive strategies in daily life.
- Joint Pain and Inflammation: Arthritis is common, leading to pain, stiffness, and limited mobility. Joint protection education, physical therapy, and medication management are crucial aspects of care.
- Skin Manifestations: Lupus rashes can be painful, disfiguring, and psychologically distressing. We collaborate with dermatologists and offer emotional support.
- Organ Involvement: Lupus can affect various organs, including kidneys, lungs, and heart. We work closely with specialists like nephrologists and cardiologists to manage these complications.
- Cognitive Impairment: “Lupus fog,” a form of cognitive dysfunction, can affect memory, concentration, and decision-making. We work with neuropsychologists and encourage cognitive rehabilitation techniques.
Addressing these challenges requires a holistic approach, encompassing medical management, rehabilitation therapies, psychological support, and patient education. It’s about empowering patients to manage their symptoms and actively participate in their own care. For example, we might teach a patient with fatigue how to prioritize tasks, delegate responsibilities, and utilize assistive devices.
Q 10. Explain your understanding of joint protection techniques.
Joint protection techniques are crucial for managing pain, reducing inflammation, and preserving joint function in rheumatic diseases. They are strategies that aim to minimize stress on affected joints and prevent further damage.
- Positioning: Maintaining proper posture and avoiding prolonged periods in static positions helps to reduce strain on joints. For example, avoiding prolonged kneeling or bending helps protect knees.
- Body Mechanics: Learning to lift and carry objects correctly, using larger muscle groups instead of smaller, weaker ones, safeguards against joint stress.
- Adaptive Equipment: Using assistive devices such as reachers, jar openers, and adaptive clothing reduces strain on joints during daily tasks.
- Energy Conservation: Planning activities to minimize exertion and fatigue helps conserve joint energy. Breaking down tasks into smaller chunks or utilizing rest periods are effective strategies.
- Joint Rest: Allowing joints to rest during periods of flare-up or increased pain is vital.
We educate patients on these techniques, demonstrating proper methods through physical therapy sessions and providing tailored advice based on their individual needs and limitations. The goal is to empower patients to make conscious choices to protect their joints in all aspects of daily life. For instance, teaching a patient with rheumatoid arthritis to use a larger, lighter cutting knife to minimize wrist strain is a practical application of joint protection.
Q 11. How do you integrate interdisciplinary collaboration into patient care?
Interdisciplinary collaboration is the cornerstone of effective rheumatologic rehabilitation. The complexity of rheumatic diseases necessitates a multi-faceted approach.
- Rheumatologist: Manages the medical aspects of the disease, prescribing medications and monitoring disease activity.
- Physical Therapist: Focuses on improving strength, range of motion, and functional mobility through exercises and manual therapy.
- Occupational Therapist: Assists in adapting daily activities and work environments to minimize joint stress and enhance independence. They might suggest assistive devices or adaptive strategies for performing household tasks.
- Psychologist/Social Worker: Addresses the emotional and psychological impact of the disease, providing coping strategies and support for patients and their families.
- Other Specialists: Depending on the patient’s needs, other specialists like dermatologists (for skin involvement), nephrologists (for kidney involvement), and cardiologists (for heart involvement) may be involved.
Regular team meetings and shared decision-making processes ensure a unified and coordinated care plan tailored to each patient. We use electronic health records and shared platforms to facilitate communication and information sharing, ensuring everyone is informed and on the same page. A shared care plan fosters a sense of collaborative care which is reassuring for the patient.
Q 12. Describe your experience with different types of splints and bracing.
My experience encompasses a wide range of splints and braces, chosen based on the specific needs of each patient and the particular joint involved.
- Resting Splints: Used to immobilize joints during periods of inflammation or acute flares, promoting rest and reducing pain. Examples include wrist splints for carpal tunnel syndrome or elbow splints for epicondylitis.
- Functional Splints: Provide support and stability while allowing for some movement, facilitating functional use of the joint. These are often used for patients needing support while participating in daily activities.
- Dynamic Splints: Incorporate components that assist with range of motion exercises, helping to prevent joint contractures and improve mobility. For example, a dynamic splint could help improve finger extension after a stroke.
- Custom-Made Braces: Designed by orthotists to meet specific patient needs, offering tailored support and functionality. These may be used for severe joint instability or deformity.
I collaborate closely with orthotists to ensure the proper selection and fitting of these devices. Patient education is key, ensuring they understand how to properly use, maintain, and care for their splints and braces. We regularly assess the effectiveness of the devices and adjust them or replace them if necessary, to ensure optimal outcomes.
Q 13. What is your experience with managing medication side effects related to rheumatic diseases?
Managing medication side effects is a critical aspect of rheumatologic care, as many medications used to treat rheumatic diseases can have significant side effects.
- Gastrointestinal Issues: Nonsteroidal anti-inflammatory drugs (NSAIDs) can cause stomach upset, ulcers, and bleeding. We monitor patients closely, potentially using protective medications like proton pump inhibitors.
- Cardiovascular Risk: Some medications, such as corticosteroids, can increase the risk of cardiovascular events. We carefully weigh the benefits and risks, closely monitoring blood pressure and lipid levels.
- Bone Loss: Corticosteroids can contribute to osteoporosis. We monitor bone density, often recommending calcium and vitamin D supplements or other bone-protecting medications.
- Infections: Immunosuppressive medications increase susceptibility to infections. We educate patients about infection prevention strategies and monitor for signs of infection.
- Neurological Effects: Some medications can cause peripheral neuropathy or other neurological problems. Regular neurological examinations help detect these complications early.
Proactive monitoring and prompt intervention are crucial. We develop strategies to minimize side effects and work collaboratively with patients to manage any that occur. Open communication between patients and the medical team is crucial for early detection and timely management. For example, if a patient is experiencing significant gastrointestinal discomfort from NSAIDs, we might consider switching to a different medication or adding gastrointestinal protection.
Q 14. How do you differentiate between different types of arthritis?
Differentiating between various types of arthritis requires a thorough history, physical examination, and often, laboratory testing and imaging studies. Key features to consider include:
- Joint Involvement: Some arthritides are localized to specific joints (e.g., osteoarthritis of the knees), while others are systemic (e.g., rheumatoid arthritis, which can affect many joints).
- Inflammation: The presence or absence of inflammation is crucial. Rheumatoid arthritis is an inflammatory disease, while osteoarthritis is primarily degenerative.
- Symptoms: Pain, stiffness, swelling, redness, and warmth are common symptoms, but their pattern and severity vary across different arthritides.
- Laboratory Tests: Rheumatoid factor (RF) and anti-citrullinated protein antibodies (ACPA) are blood tests that can help diagnose rheumatoid arthritis. Other blood tests may be used to rule out other conditions.
- Imaging Studies: X-rays, ultrasound, and MRI can reveal joint damage, inflammation, and other characteristics that aid in diagnosis. For example, X-rays might show joint space narrowing in osteoarthritis.
A thorough evaluation helps differentiate between osteoarthritis (degenerative joint disease), rheumatoid arthritis (inflammatory autoimmune disease), psoriatic arthritis (associated with psoriasis), lupus (a systemic autoimmune disease), and gout (caused by uric acid crystal deposition). It is important to consider the whole clinical picture for an accurate diagnosis and appropriate treatment.
Q 15. Describe your approach to pain management in Rheumatologic Rehabilitation.
My approach to pain management in rheumatologic rehabilitation is multifaceted and highly individualized, prioritizing a biopsychosocial model. This means we consider not only the physical pain but also the psychological and social factors impacting the patient’s experience.
We start with a thorough assessment, including a detailed pain history, physical examination, and functional assessment. This helps us understand the type, location, intensity, and impact of the pain on the patient’s daily life. Based on this, we develop a personalized plan encompassing several strategies:
- Pharmacological Management: This might involve working closely with the patient’s rheumatologist to optimize medication regimens, including NSAIDs, analgesics, and potentially disease-modifying antirheumatic drugs (DMARDs) or biologics.
- Physical Therapy: This is crucial for improving joint mobility, muscle strength, and overall function. We utilize various modalities, as discussed later.
- Occupational Therapy: This focuses on adapting daily activities to minimize pain and maximize independence. For example, we might suggest assistive devices or modify workspaces.
- Psychological Interventions: Managing the psychological impact of chronic pain is vital. This may involve cognitive behavioral therapy (CBT) to address negative thought patterns and coping strategies, or relaxation techniques like mindfulness and meditation.
- Education and Self-Management: Empowering patients with knowledge about their condition and self-management techniques is key to long-term success. This includes understanding pain flares, pacing activities, and recognizing warning signs.
For example, I recently worked with a patient with rheumatoid arthritis experiencing significant hand pain. We implemented a program combining low-impact exercises, hand splinting at night, and CBT to manage her anxiety related to pain flares. This integrated approach resulted in a significant reduction in her pain and improved functional capacity.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you adapt treatment plans for patients with comorbidities?
Managing comorbidities is crucial in rheumatologic rehabilitation. Many patients with rheumatic diseases also have conditions like diabetes, heart disease, or osteoporosis. Ignoring these can lead to adverse outcomes. My approach involves:
- Thorough Assessment: A comprehensive medical history is essential to identify all existing conditions. This includes reviewing medication lists and discussing any limitations imposed by comorbidities.
- Interprofessional Collaboration: Close collaboration with other specialists like cardiologists, endocrinologists, or pulmonologists is vital to ensure the treatment plans are coordinated and safe. For instance, if a patient has heart disease, high-intensity exercise might be contraindicated.
- Individualized Treatment Plans: The treatment plan must adapt to the patient’s unique combination of conditions. Exercise intensity, frequency, and type must be carefully considered to avoid exacerbating comorbidities. For example, a patient with diabetes might need more frequent blood glucose monitoring during intensified exercise.
- Medication Interactions: Careful monitoring for drug interactions between medications for rheumatic disease and those for comorbidities is paramount to avoid complications.
For instance, I recently worked with a patient who had both rheumatoid arthritis and congestive heart failure. We collaborated with her cardiologist to design a low-impact exercise program that improved her joint mobility without stressing her heart.
Q 17. What are the potential complications associated with prolonged immobility in Rheumatologic patients?
Prolonged immobility in rheumatologic patients can lead to a cascade of serious complications:
- Muscle Atrophy and Weakness: Lack of movement causes muscles to waste away, leading to weakness, reduced functional capacity, and increased risk of falls.
- Joint Contractures: Stiffening of the joints due to prolonged inactivity, making movement painful and restricted.
- Osteoporosis: Immobility reduces bone density, increasing the risk of fractures.
- Cardiovascular Complications: Reduced activity contributes to cardiovascular problems like decreased cardiac output and increased risk of blood clots.
- Respiratory Problems: Immobility can lead to reduced lung capacity and increased risk of pneumonia.
- Pressure Sores: Prolonged pressure on the skin can cause skin breakdown and ulcers.
- Depression and Anxiety: Inability to participate in activities can worsen mental health.
Imagine a patient with severe rheumatoid arthritis who limits movement due to pain. Without intervention, this could lead to severe joint contractures, muscle atrophy, and reduced quality of life. Our goal is to prevent these complications through early mobilization and exercise programs tailored to their limitations.
Q 18. Discuss your experience with different modalities of physical therapy, such as ultrasound and electrical stimulation.
I have extensive experience using various physical therapy modalities. The choice of modality depends on the specific condition, the patient’s response, and the treatment goals.
- Ultrasound: Uses high-frequency sound waves to penetrate tissues, increasing blood flow and reducing inflammation. It’s often used for managing pain and swelling in specific joints. For instance, ultrasound can be beneficial for treating tendonitis associated with rheumatoid arthritis.
- Electrical Stimulation: Uses electrical currents to stimulate muscles, improving strength and reducing pain. Different types of electrical stimulation exist, including transcutaneous electrical nerve stimulation (TENS) for pain relief and neuromuscular electrical stimulation (NMES) for muscle strengthening. TENS can be particularly helpful for managing pain during flares of inflammatory arthritis.
- Other Modalities: Other modalities like heat and cold therapy, manual therapy, and therapeutic exercise are also frequently used in conjunction with ultrasound and electrical stimulation to create a comprehensive treatment plan.
I always ensure that the patient understands the purpose and potential side effects of each modality. For instance, before applying ultrasound, I explain the sensation the patient should expect and monitor them for any discomfort.
Q 19. How do you address patient anxiety and depression related to chronic rheumatic diseases?
Chronic rheumatic diseases significantly impact mental health, often leading to anxiety and depression. Addressing these aspects is integral to comprehensive care.
- Psychological Screening: Regular screening for depression and anxiety using standardized tools is essential.
- Referral to Mental Health Professionals: When necessary, referral to a psychologist or psychiatrist is crucial for appropriate management of mental health conditions. This can involve therapy, medication, or both.
- Psychoeducation: Educating patients and their families about the emotional impact of chronic illness helps them cope more effectively. Understanding that anxiety and depression are common and treatable is vital.
- Stress Management Techniques: Teaching relaxation techniques such as deep breathing, progressive muscle relaxation, or mindfulness meditation can help manage stress and improve mental well-being.
- Support Groups: Connecting patients with support groups can provide a sense of community and shared experience, reducing feelings of isolation.
For example, I recently referred a patient with lupus who was experiencing significant depression to a psychologist specializing in chronic illness. This intervention significantly improved her emotional state and her adherence to her physical therapy regimen.
Q 20. Describe your experience with patients who have fibromyalgia.
Fibromyalgia is a chronic condition characterized by widespread pain, fatigue, and sleep disturbances. Managing fibromyalgia requires a holistic approach focusing on symptom management and improving quality of life.
- Multimodal Treatment: Treatment involves a combination of strategies, including exercise, medication, and psychological interventions. Exercise should be low-impact and gradually increased to avoid exacerbation of symptoms.
- Pain Management Strategies: Techniques like CBT, mindfulness, and relaxation exercises help manage pain and improve sleep quality.
- Medication: Medications may include analgesics, antidepressants, and anticonvulsants, depending on the patient’s symptoms.
- Graded Exercise Therapy: A gradual increase in physical activity helps build endurance and improve function, while pacing activities prevents symptom exacerbation.
- Sleep Hygiene: Addressing sleep disturbances is crucial, as poor sleep often worsens symptoms. This might involve sleep studies and behavioral interventions.
I frequently work with patients with fibromyalgia, focusing on building a personalized program that addresses their specific symptoms and limitations. It’s vital to build trust and understanding, acknowledging the challenges they face and supporting their self-management efforts.
Q 21. How do you assess patient adherence to prescribed treatment plans?
Assessing patient adherence to prescribed treatment plans is crucial for effective rehabilitation. I employ several strategies:
- Regular Follow-up Appointments: Scheduled appointments provide opportunities to monitor progress, address concerns, and make adjustments to the plan as needed.
- Patient Diaries or Logs: Asking patients to keep track of their exercise sessions, medication adherence, and pain levels helps identify areas needing improvement.
- Communication and Education: Clear communication about the treatment plan and its rationale is crucial. Addressing any misconceptions or concerns promotes better adherence.
- Goal Setting: Collaboratively setting realistic and achievable goals empowers patients and motivates them to adhere to their plans.
- Motivational Interviewing: Utilizing motivational interviewing techniques helps identify barriers to adherence and supports the patient in finding solutions.
- Technology: Using wearable technology to track activity levels and other relevant data can provide valuable feedback and improve adherence.
For example, I utilize patient diaries to track exercise adherence in patients with rheumatoid arthritis. When adherence is low, we discuss potential barriers, adjust the plan together, and develop strategies to overcome the obstacles, thereby increasing their likelihood of achieving their goals.
Q 22. What is your experience with home modifications and home health care?
Home modifications and home health care are crucial components of comprehensive rheumatologic rehabilitation. My experience encompasses assessing the home environment for safety hazards and recommending modifications to improve accessibility and independence for patients with rheumatic conditions. This includes suggesting adaptations such as grab bars in bathrooms, ramps for wheelchair access, and modifications to kitchen layouts for easier movement. I also collaborate with home health agencies to coordinate the provision of necessary services, like physical therapy, occupational therapy, and personal care assistance, ensuring a seamless transition from the clinical setting to the patient’s home. For example, I recently worked with a patient with severe rheumatoid arthritis who found it difficult to use the stairs. We collaborated to install a stair lift, dramatically improving her mobility and quality of life. Furthermore, I regularly liaise with occupational therapists to ensure the proper adaptive equipment is provided and used correctly within the home environment. This holistic approach significantly improves patient outcomes and reduces hospital readmissions.
Q 23. What is your experience with ergonomic assessments and workplace modifications?
Ergonomic assessments and workplace modifications are essential for managing rheumatic conditions and preventing work-related exacerbations. My experience involves conducting thorough assessments of the patient’s workstation, identifying potential ergonomic risk factors such as poor posture, repetitive movements, and awkward working positions. I then develop and implement tailored modifications, which might include adjusting chair height and angles, providing ergonomic keyboard and mouse setups, or recommending alternative work techniques. In one case, I worked with a data entry clerk with carpal tunnel syndrome secondary to rheumatoid arthritis. After a comprehensive ergonomic assessment, we implemented changes that included a split keyboard, adjustable monitor stand, and frequent rest breaks. This resulted in a significant reduction in her pain and improved her work productivity. I believe in educating employers about the importance of providing a supportive work environment for employees with rheumatic diseases. Creating an open communication channel and ensuring collaboration between the patient, employer, and the rehabilitation team is critical for successful workplace integration.
Q 24. How do you handle difficult or non-compliant patients?
Handling difficult or non-compliant patients requires a patient-centered approach that prioritizes understanding and collaboration. I begin by actively listening to their concerns, validating their feelings, and exploring the reasons behind their non-compliance. It’s crucial to understand that non-compliance often stems from underlying factors such as pain, fear, lack of knowledge, or practical barriers. I use motivational interviewing techniques to build rapport and encourage self-management. For instance, if a patient is struggling to adhere to their exercise regimen, I would collaborate with them to develop a tailored program that addresses their specific needs and limitations. This might involve adjusting the intensity and duration of exercises, incorporating rest periods, or offering alternative exercises they find more enjoyable. If necessary, I would involve family members or caregivers in the treatment plan to provide support and encouragement. Ultimately, the goal is to create a therapeutic alliance based on trust and mutual respect, leading to improved adherence and better outcomes. Documentation is key, recording any challenges, the strategies used, and the patient’s response to those strategies. This aids in ongoing assessment and adjustments to the treatment plan.
Q 25. Explain your knowledge of the latest advancements in Rheumatologic Rehabilitation.
Rheumatologic rehabilitation is constantly evolving. Recent advancements include the increased use of telehealth for remote monitoring and rehabilitation, providing greater accessibility and convenience for patients. Furthermore, there’s significant focus on personalized medicine, utilizing genetic and biomarker information to tailor treatment plans and predict individual responses to therapy. Advances in biologic therapies have also dramatically altered the course of many rheumatic diseases, impacting rehabilitation goals and strategies. For example, the use of biologics often leads to improved function and reduced pain, enabling patients to participate in more intensive rehabilitation programs. Moreover, the incorporation of virtual reality (VR) and augmented reality (AR) technologies offers novel approaches to pain management and functional training. VR can be used to simulate real-life activities, helping patients practice and build confidence in performing tasks at home or in the workplace. Finally, there’s growing research into the use of artificial intelligence (AI) to analyze patient data, predict disease progression, and personalize treatment strategies.
Q 26. Describe your experience with outcome measures and their relevance in Rheumatology.
Outcome measures are essential for evaluating the effectiveness of rheumatologic rehabilitation interventions and tracking patient progress. They provide objective data to assess improvements in various aspects such as pain, function, physical activity, and quality of life. Commonly used outcome measures include the Health Assessment Questionnaire (HAQ), the Disease Activity Score 28 (DAS28), and the Patient-Reported Outcomes Measurement Information System (PROMIS) questionnaires. In my experience, selecting appropriate outcome measures depends on the specific rheumatic condition and the goals of the rehabilitation program. I use these measures at baseline, during the course of treatment, and at follow-up appointments to monitor response to therapy and guide clinical decision-making. For instance, tracking a patient’s HAQ score can demonstrate improvement in their daily living activities following an occupational therapy intervention. Regular assessment using these measures not only helps demonstrate the value of rehabilitation services but also allows for timely adjustments to the treatment plan based on the patient’s response. The use of validated and reliable outcome measures ensures that we’re collecting high-quality data that can be used for research and to improve patient care.
Q 27. How do you ensure patient safety during treatment sessions?
Patient safety is paramount in all treatment sessions. I adhere to strict protocols to ensure a safe environment. This begins with a thorough assessment of the patient’s physical capabilities and limitations before commencing any intervention. I modify exercises and activities as needed to accommodate the patient’s functional status and pain levels, avoiding any movements that could exacerbate their condition. I provide clear instructions and demonstrate proper techniques to prevent injuries. The treatment area is kept clean and free of hazards, and appropriate equipment is used according to manufacturer’s instructions. For patients with reduced mobility or balance problems, assistive devices are used as necessary, and close supervision is provided. I regularly monitor the patient’s vital signs and pain levels throughout the session, and I’m prepared to address any adverse events promptly. Open communication with the patient is vital; I encourage them to report any discomfort or unusual sensations immediately. Patient education is key; I empower patients to actively participate in ensuring their safety by understanding their limits and communicating their needs effectively. This proactive approach fosters a safe and effective therapeutic environment.
Q 28. Describe your experience with working within a multidisciplinary team in a Rheumatology setting.
Effective rheumatologic rehabilitation necessitates a collaborative approach involving a multidisciplinary team. My experience includes working closely with rheumatologists, physiatrists, physical therapists, occupational therapists, nurses, and social workers. We utilize regular team meetings to coordinate treatment plans, share information, and address any challenges. For example, the rheumatologist might provide information about the disease activity and medication management, while the physical therapist focuses on improving physical function, and the occupational therapist addresses daily living tasks. The social worker provides support with psychosocial issues, and nurses aid in monitoring and managing any complications. This integrated approach allows us to provide comprehensive and patient-centered care. Effective communication is crucial; we use electronic health records and regular team meetings to ensure seamless information exchange. Collaborative case conferences allow us to share our observations, discuss challenges and adjust the treatment plan as needed, ultimately leading to better outcomes and improved patient satisfaction. This integrated, team-based approach is vital for providing the best possible care to patients with complex rheumatological conditions.
Key Topics to Learn for Rheumatologic Rehabilitation Interview
- Musculoskeletal Anatomy & Physiology: Understanding joint structure, function, and the impact of rheumatic diseases on these systems. This includes the intricacies of synovial joints, cartilage, and bone.
- Rheumatic Disease Pathophysiology: Developing a strong grasp of the underlying mechanisms of common rheumatic conditions like rheumatoid arthritis, osteoarthritis, lupus, and fibromyalgia. This includes understanding inflammation, autoimmunity, and pain pathways.
- Therapeutic Exercise & Modalities: Knowing the application of various therapeutic interventions such as range of motion exercises, strengthening programs, joint protection techniques, and the use of modalities like heat, cold, and electrical stimulation.
- Assistive Devices & Adaptive Strategies: Familiarity with the selection, fitting, and training of patients in the use of assistive devices like canes, walkers, and adaptive equipment for daily living activities.
- Patient Assessment & Goal Setting: Mastering the process of comprehensive patient evaluation, including functional assessments, pain scales, and the development of individualized treatment plans aligned with patient goals.
- Pain Management Strategies: Understanding various approaches to managing pain in rheumatic conditions, including pharmacological interventions, non-pharmacological techniques (e.g., relaxation, mindfulness), and interdisciplinary collaboration.
- Rehabilitation Program Planning & Implementation: Ability to design, implement, and progress rehabilitation programs based on individual patient needs, considering factors like disease severity, functional limitations, and patient motivation.
- Outcome Measurement & Evaluation: Understanding the importance of tracking patient progress using standardized outcome measures and evaluating the effectiveness of interventions. This includes interpreting data and making adjustments to treatment plans as needed.
- Interprofessional Collaboration: Highlighting the importance of working effectively with other healthcare professionals (physicians, nurses, occupational therapists, etc.) to provide holistic patient care.
Next Steps
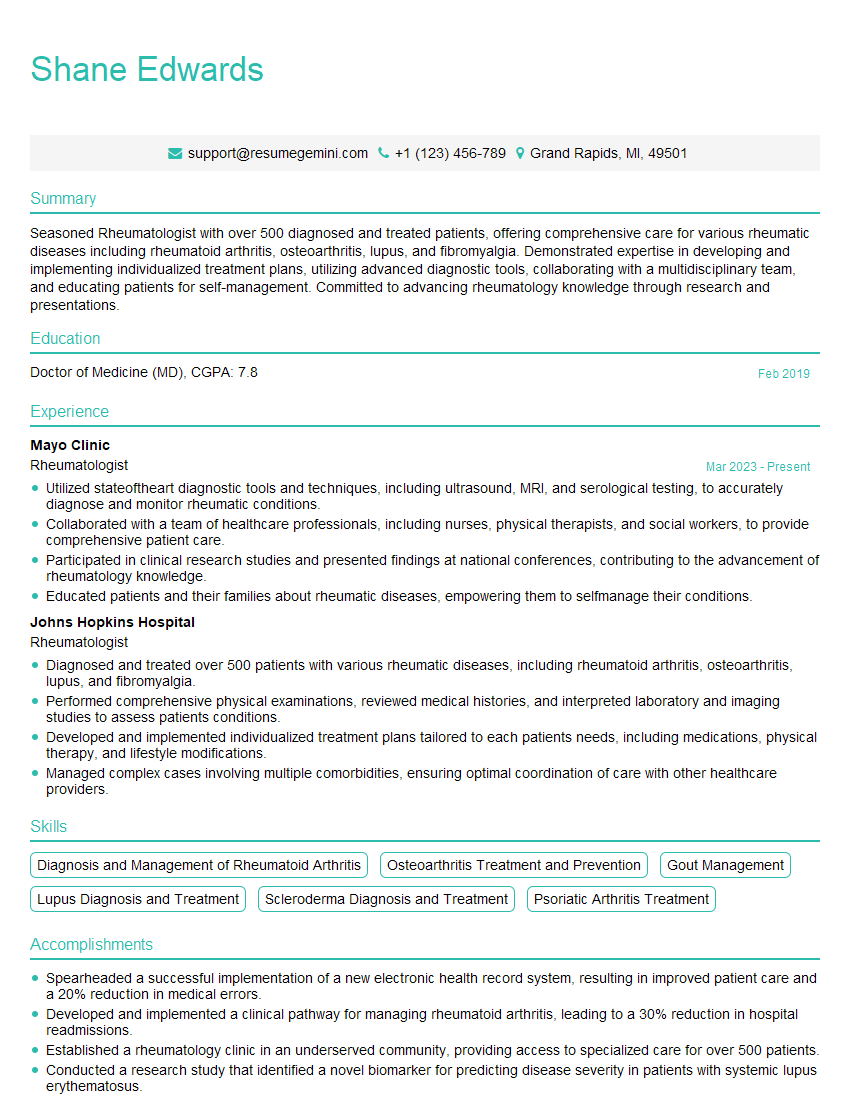
Mastering Rheumatologic Rehabilitation principles is crucial for career advancement in this rapidly evolving field. It demonstrates a strong understanding of patient care and positions you as a valuable asset to any team. To maximize your job prospects, creating an ATS-friendly resume is paramount. ResumeGemini is a trusted resource that can help you build a professional resume that highlights your skills and experience effectively. Examples of resumes tailored to Rheumatologic Rehabilitation are available to guide you, ensuring your application stands out.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hi, I have something for you and recorded a quick Loom video to show the kind of value I can bring to you.
Even if we don’t work together, I’m confident you’ll take away something valuable and learn a few new ideas.
Here’s the link: https://bit.ly/loom-video-daniel
Would love your thoughts after watching!
– Daniel
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.