The thought of an interview can be nerve-wracking, but the right preparation can make all the difference. Explore this comprehensive guide to Cervical Cancer Screening interview questions and gain the confidence you need to showcase your abilities and secure the role.
Questions Asked in Cervical Cancer Screening Interview
Q 1. Explain the different types of cervical cancer screening tests and their indications.
Cervical cancer screening aims to detect precancerous lesions (cervical intraepithelial neoplasia, or CIN) before they progress to invasive cancer. Two main types of tests are used: Pap smears (cytology) and HPV (Human Papillomavirus) testing.
- Pap smear: This test examines cells collected from the cervix to identify abnormal cell changes. It’s a relatively simple procedure, but its sensitivity for detecting all high-grade precancerous lesions is lower than HPV testing.
- HPV testing: This test detects the presence of high-risk HPV types, which are the primary cause of cervical cancer. It’s more sensitive than Pap smears in detecting precancerous lesions, especially high-grade CIN. There are different types of HPV tests available, including those targeting specific high-risk genotypes (like HPV 16 and 18) or broader panels testing for multiple types.
- Combined testing (co-testing): This approach combines both Pap smear and HPV testing. It offers the highest sensitivity and specificity for detecting cervical cancer and its precursors.
Indications: Screening is typically recommended for women aged 21-65, with specific age-based recommendations and variations based on individual risk factors (like immunocompromise, history of CIN, or exposure to diethylstilbestrol (DES)). Women younger than 21 are generally not screened because of the low risk of developing precancerous lesions and higher frequency of false positives at this age. Screening guidelines may vary slightly based on the country and current recommendations.
Q 2. Describe the Bethesda System for reporting cervical cytology results.
The Bethesda System is a standardized reporting system for cervical cytology results. It provides a structured way to describe the findings of a Pap smear, ensuring consistency and clarity in communication between laboratories and clinicians. The system classifies findings into several categories, including:
- Negative for intraepithelial lesion or malignancy (NILM): This means no abnormal cells were detected.
- Atypical squamous cells of undetermined significance (ASCUS): Indicates some abnormal squamous cells but not enough to determine whether they’re cancerous or precancerous.
- Atypical squamous cells, cannot exclude HSIL (ASC-H): Indicates squamous cells with abnormal features suggesting high-grade squamous intraepithelial lesion (HSIL).
- Low-grade squamous intraepithelial lesion (LSIL): Indicates mild cellular abnormalities suggestive of CIN1.
- High-grade squamous intraepithelial lesion (HSIL): Indicates more significant cellular abnormalities suggestive of CIN2 or CIN3.
- Squamous cell carcinoma:Indicates the presence of invasive squamous cell carcinoma.
- Similar categories exist for glandular cells (e.g., AGC, endocervical adenocarcinoma).
The Bethesda System also includes descriptions of other findings such as inflammation, infection, and the presence of other cells.
Q 3. What are the limitations and advantages of Pap smears versus HPV testing?
Both Pap smears and HPV testing play vital roles in cervical cancer screening, but they have different strengths and weaknesses:
- Pap smear Advantages: Relatively inexpensive, widely available, readily interpretable in many cases, can sometimes detect other abnormalities besides precancerous cells.
- Pap smear Limitations: Less sensitive than HPV testing, especially for high-grade CIN, can produce false negatives and false positives.
- HPV testing Advantages: More sensitive than Pap smears for detecting high-grade CIN, can predict future risk of cancer, is useful for triage, enabling more efficient use of resources.
- HPV testing Limitations: More expensive than Pap smears in many settings, cannot directly identify severity of CIN, may yield false positive results (infection that clears on its own).
In practice, the optimal approach often involves combined testing or choosing the best screening strategy based on age, risk factors, and resource availability.
Q 4. Explain the role of colposcopy in cervical cancer screening.
Colposcopy is a procedure used to visualize the cervix using a specialized magnifying instrument (colposcope). It’s crucial in cervical cancer screening because it allows direct visualization of the cervix, facilitating the detection of lesions that may not be apparent on Pap smear or HPV testing. Acetic acid and Lugol’s iodine solutions can be applied to enhance visualization of abnormal tissue.
Role in screening: Colposcopy is typically performed when abnormal Pap smear or HPV test results are obtained. It helps to guide biopsies to obtain tissue samples for histopathological examination which definitively identifies and grades any precancerous or cancerous lesions. It is crucial in distinguishing benign changes from precancerous lesions.
Q 5. How do you interpret a positive HPV test result?
A positive HPV test result indicates the presence of high-risk HPV DNA. However, it’s important to remember that most women infected with high-risk HPV will clear the infection naturally without developing cervical cancer. Therefore, a positive HPV test alone does not necessarily mean cervical cancer or even precancerous lesions.
Interpretation and Management: A positive HPV result necessitates further investigation, typically through cytology (Pap smear) or colposcopy. The management strategy depends on the woman’s age, previous test results, and other risk factors. The goal is to identify any precancerous lesions and manage them appropriately, preventing progression to cancer.
Q 6. What are the management options for CIN lesions?
Cervical intraepithelial neoplasia (CIN) lesions represent abnormal cell growth on the cervix. Management depends on the grade of CIN (CIN1, CIN2, CIN3) and other factors, including patient age and overall health. Options include:
- Observation (watchful waiting): For low-grade lesions (CIN1), especially in younger women, the lesion may regress spontaneously, and repeat testing is necessary.
- Ablation or Excisional Procedures: These are often recommended for higher-grade lesions (CIN2, CIN3), such as Loop Electrosurgical Excision Procedure (LEEP), cold-knife conization, or laser ablation. These methods remove the abnormal tissue.
The choice of procedure depends on factors such as lesion size, location, and patient-specific circumstances. Regular follow-up is essential after treatment to ensure complete lesion removal and to monitor for recurrence.
Q 7. Describe the process for managing abnormal cervical cytology results.
Management of abnormal cervical cytology results follows a structured approach, often starting with repeat Pap smears and/or HPV testing. This allows for assessment of whether the abnormality was transient or persistent.
Abnormal Results: If an abnormality persists or worsens, further investigation is needed using colposcopy and biopsy to assess the nature of the abnormal cells. Depending on the diagnosis, management strategies will be implemented. Low-grade lesions can be managed with observation or treatment, while high-grade lesions typically require excisional or ablative treatment. Invasive cancer will require treatment as dictated by clinical staging and other factors.
Importance of Follow-Up: Ongoing follow-up is vital to assess treatment response and detect any recurrences. Regular screening is also crucial even after treatment to ensure early detection of any new abnormalities.
Q 8. What are the risk factors for cervical cancer?
Cervical cancer, thankfully a largely preventable disease, arises from persistent infection with high-risk types of Human Papillomavirus (HPV). Several factors increase a woman’s risk. Think of it like this: some factors directly contribute to HPV infection or its persistence, while others weaken the body’s ability to fight it off.
- HPV Infection: This is the most significant risk factor. Exposure to high-risk HPV types (like 16 and 18) is crucial for cervical cancer development. Multiple sexual partners or early onset of sexual activity increases exposure risk.
- Smoking: Smoking impairs the immune system, making it harder to clear HPV infections. It also directly damages cervical cells.
- Weakened Immune System: Conditions like HIV/AIDS compromise the body’s ability to fight off HPV, increasing the risk of progression to cancer.
- Long-term use of Oral Contraceptives: While the link is debated, some studies suggest a slightly elevated risk with prolonged use.
- Multiple Pregnancies: Multiple pregnancies can lead to hormonal changes that might affect cervical cells.
- Early age at first full-term pregnancy: Women who have their first full-term pregnancy before age 17 are at higher risk.
- Exposure to Diethylstilbestrol (DES): DES, a synthetic estrogen, was given to pregnant women decades ago; daughters of women who took DES have an increased risk of cervical abnormalities.
- Low socioeconomic status: Access to healthcare, including screening, is often limited in lower socioeconomic groups, leading to delayed diagnosis.
Understanding these risk factors allows us to tailor prevention strategies and screening recommendations for individual patients.
Q 9. Discuss the role of vaccination in cervical cancer prevention.
Vaccination against HPV is a cornerstone of cervical cancer prevention. The HPV vaccine protects against the high-risk types of HPV that cause the vast majority of cervical cancers. It’s like giving the body a head start in the fight against this virus.
The vaccine is most effective when given before sexual activity, typically recommended for girls and boys aged 11-12. However, it can still be beneficial for older individuals who haven’t been vaccinated or haven’t completed the series. The vaccine doesn’t cure existing infections but prevents new ones, significantly reducing the risk of developing cervical cancer in the future. Several vaccines are available, offering protection against multiple HPV types.
While the vaccine is highly effective, it doesn’t offer 100% protection, emphasizing the continued importance of regular screening.
Q 10. Explain the importance of follow-up after an abnormal screening test.
Follow-up after an abnormal cervical cancer screening test is crucial because it determines the next steps in managing the patient. An abnormal result doesn’t automatically mean cancer, but it signifies the need for further investigation to rule out precancerous lesions or cancer itself.
The follow-up procedure depends on the nature of the abnormality. It may involve repeat Pap tests, HPV testing, colposcopy (a visual examination of the cervix using a magnifying instrument), or a cervical biopsy. Prompt follow-up helps to detect and treat any precancerous lesions before they progress to cancer, greatly improving the chances of a positive outcome.
Delaying follow-up significantly increases the risk of delayed diagnosis and treatment, potentially leading to more invasive procedures and a poorer prognosis. Consistent communication and patient education are essential to ensure timely follow-up.
Q 11. What are the ethical considerations related to cervical cancer screening?
Ethical considerations in cervical cancer screening are multifaceted and crucial. They include:
- Informed Consent: Patients must fully understand the procedure, its benefits, risks, and alternatives before undergoing screening. This includes potential false positives and the emotional distress associated with abnormal results.
- Confidentiality: Maintaining strict confidentiality of patient information is paramount, adhering to all relevant privacy regulations.
- Equity and Access: Ensuring equitable access to screening services regardless of socioeconomic status, race, ethnicity, or geographic location is ethically vital.
- Resource Allocation: Efficient and ethical allocation of resources to maximize the impact of screening programs is essential.
- Balancing individual autonomy with public health goals: The goal is to promote population-level health improvements while respecting individual preferences and autonomy regarding healthcare decisions.
- Overdiagnosis and overtreatment: Screening can lead to the detection of lesions that may never have progressed to cancer. Ethical considerations arise when deciding on the best course of action in these scenarios.
Navigating these ethical dilemmas requires careful consideration, balancing individual rights with population-wide benefits.
Q 12. How do you counsel patients about cervical cancer screening?
Counseling patients about cervical cancer screening involves a sensitive and personalized approach. I always begin by explaining the importance of screening in preventing cervical cancer. I use plain language and visual aids to explain the procedure, emphasizing its simplicity and minimal discomfort.
I address common concerns and misconceptions, such as the fear of pain or embarrassment. I discuss the different types of screening tests (Pap smear, HPV test, and their combination) and explain their benefits and limitations. I also discuss the implications of both normal and abnormal results, outlining the follow-up steps in each case.
Crucially, I involve the patient in the decision-making process, respecting their autonomy and preferences. I answer all their questions honestly and openly, fostering a trusting relationship built on mutual understanding and respect. I ensure they fully understand the benefits and risks before making any decisions.
Q 13. How do you manage patient anxiety related to screening tests?
Managing patient anxiety is a crucial aspect of providing compassionate and effective care. I use a multi-pronged approach. Firstly, I actively listen to the patient’s concerns and validate their feelings. Creating a safe and comfortable environment is vital, so I offer detailed explanations and answer questions patiently.
I normalize the experience by sharing that many women feel anxious before the procedure. I often use analogies to demystify the process, for instance comparing the Pap smear to a routine blood test. I provide clear and concise information about the procedure’s length, discomfort level, and post-procedure care. If necessary, I refer patients to support groups or counseling services for additional emotional support.
In cases of severe anxiety, I might offer relaxation techniques or discuss the possibility of sedation with the patient’s physician. The goal is to ensure the patient feels informed, comfortable, and empowered throughout the process.
Q 14. Describe your experience with quality assurance in cervical cancer screening.
Quality assurance in cervical cancer screening is paramount to ensure accuracy, reliability, and efficiency. My experience encompasses multiple aspects. This involves meticulous adherence to established protocols and guidelines, ensuring proper sample collection, processing, and analysis.
Regular internal audits are conducted to review the entire screening process, from patient registration to result reporting. This includes evaluating staff training, equipment calibration, and adherence to quality control measures. Participation in external quality assurance programs, where anonymized samples are sent to reference laboratories, provides valuable feedback and helps identify areas for improvement.
Data analysis plays a vital role. We routinely analyze screening data to identify trends, assess performance indicators, and track key metrics like participation rates, sensitivity, specificity, and positive predictive value. This data-driven approach allows for continuous monitoring and improvement, ensuring we maintain the highest standards of quality in our cervical cancer screening program.
Q 15. What are the key performance indicators for a cervical cancer screening program?
Key performance indicators (KPIs) for a cervical cancer screening program are crucial for evaluating its effectiveness and identifying areas for improvement. These KPIs should reflect coverage, timeliness, quality, and impact on cancer incidence and mortality.
- Screening Coverage: This measures the percentage of the target population that has undergone screening within a defined period. For example, aiming for 80% coverage among women aged 25-65. Low coverage might indicate barriers to access.
- Timeliness: This assesses how promptly women receive screening after becoming eligible. Delays can lead to missed opportunities for early detection. We might track the average time between eligibility and screening.
- Screening Adequacy/Quality: This refers to the quality of the screening test itself (e.g., Pap smear adequacy, HPV test accuracy). We monitor the percentage of adequate samples and the rate of false-negative results.
- Positive Predictive Value (PPV): This KPI shows the proportion of positive screening tests that truly indicate precancerous or cancerous lesions. A high PPV indicates fewer unnecessary follow-up procedures.
- Cancer Incidence and Mortality Rates: Ultimately, the program’s success is judged by its impact on cervical cancer rates. We track the incidence of cervical cancer and cancer-related deaths in the screened population compared to an unscreened population or national averages.
- Follow-up Rates: For women with abnormal screening results, we monitor the percentage who complete recommended follow-up procedures like colposcopy and treatment.
By consistently monitoring these KPIs, we can identify bottlenecks and implement targeted interventions to improve the program’s overall efficiency and effectiveness.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you ensure equitable access to cervical cancer screening?
Ensuring equitable access to cervical cancer screening is paramount. It requires addressing the social determinants of health that create disparities in access.
- Removing Financial Barriers: Offering affordable or subsidized screening through insurance coverage, government programs, or community-based initiatives is essential. Many women lack insurance or have high deductibles that prevent them from accessing healthcare.
- Geographic Accessibility: Screening services need to be available in convenient locations, including rural and underserved communities. Mobile screening units can be instrumental in reaching remote areas.
- Culturally Competent Care: Providers should be trained to understand and address the cultural beliefs and preferences of diverse populations. Language barriers and mistrust of the healthcare system can significantly impact participation.
- Addressing Transportation Barriers: Providing transportation assistance or incorporating screening into existing community programs can overcome transportation challenges.
- Community Outreach: Active outreach through community leaders, educational campaigns, and targeted messaging is vital to reach underserved populations. This includes addressing health literacy needs and providing accurate information.
- Data Collection and Monitoring: Regular data collection to identify and address disparities is vital. Tracking screening rates by demographic factors (race, ethnicity, socioeconomic status) helps identify gaps in service.
For example, in a community with a large immigrant population, we might collaborate with community leaders to conduct health fairs offering free or low-cost screening, with interpreters available.
Q 17. What are the current guidelines for cervical cancer screening?
Current guidelines for cervical cancer screening vary slightly depending on the organization (e.g., the American Cancer Society, the American College of Obstetricians and Gynecologists) but generally recommend a risk-based approach utilizing either cytology (Pap smear) or HPV testing or a combination thereof.
- Age 21-29: Screening every 3 years with cytology (Pap smear) is typically recommended. HPV testing is generally not recommended in this age group due to the higher rate of transient HPV infections that often resolve spontaneously.
- Age 30-65: Screening with either cytology every 3 years, or co-testing (HPV and cytology) every 5 years, is recommended. Co-testing is generally preferred due to its higher sensitivity and specificity.
- Age 65 and older: Screening can be discontinued if adequate prior negative screenings have been performed and the woman is in good health, with no history of significant cervical disease.
- Special Considerations: Women with a history of cervical precancer or cancer, or those immunocompromised, require individualized screening plans with more frequent testing.
It’s crucial to remember that these are guidelines, and individual risk factors and preferences should always be considered when making screening recommendations. Always refer to the most up-to-date guidelines from your relevant professional organization.
Q 18. How do you stay up-to-date on the latest advancements in cervical cancer screening?
Staying updated on advancements in cervical cancer screening is crucial. I utilize several strategies to ensure my knowledge remains current.
- Professional Organizations: I actively participate in professional organizations like the American College of Obstetricians and Gynecologists (ACOG) and the American Society for Colposcopy and Cervical Pathology (ASCCP). These organizations provide continuing medical education (CME) opportunities, publications, and guidelines updates.
- Peer-Reviewed Journals: I regularly review relevant peer-reviewed journals, such as the Journal of the American Medical Association (JAMA), Obstetrics & Gynecology, and Cancer Prevention Research, to stay abreast of new research findings.
- Conferences and Workshops: Attending conferences and workshops focused on cervical cancer screening and colposcopy provides valuable opportunities for learning about the latest technologies and techniques.
- Online Resources: I utilize reputable online resources from organizations such as the Centers for Disease Control and Prevention (CDC) and the National Cancer Institute (NCI) to access current information and guidelines.
- Collaboration with Colleagues: Regular discussions and case reviews with colleagues in my field facilitate knowledge sharing and allow us to learn from each other’s experiences.
Keeping abreast of emerging technologies and research findings is essential to provide the highest quality and most effective care to my patients.
Q 19. Describe your experience with interpreting colposcopic findings.
Interpreting colposcopic findings requires significant training and experience. Colposcopy involves visualizing the cervix using a magnifying lens and applying acetic acid (vinegar) or Lugol’s iodine to highlight abnormal areas.
I assess various features to determine the severity of abnormalities, including the presence of acetowhite epithelium (changes in color and texture after acetic acid application), abnormal blood vessels, and the location and extent of the lesion.
For example, an acetowhite area with punctation (small, white dots) might suggest a mild dysplasia (abnormal cell growth), whereas extensive acetowhite epithelium with mosaicism (irregular, cobblestone-like pattern) and abnormal vessels could indicate more significant disease requiring biopsy. I am proficient in recognizing the subtle visual cues that distinguish between normal and abnormal findings and correlating these visual clues with the pathological results from biopsies, which are essential for proper diagnosis and management.
My experience includes thousands of colposcopic examinations, ranging from routine surveillance to cases with high-grade abnormalities. I am experienced in performing targeted biopsies and directing further management plans based on the colposcopic findings and biopsy results.
Q 20. What are the common complications of colposcopic procedures?
Colposcopic procedures are generally safe, but complications can occur, albeit rarely.
- Bleeding: Minor bleeding is common, but significant hemorrhage is uncommon. It usually responds to direct pressure.
- Infection: Infection at the biopsy site is a potential risk, but proper sterilization techniques and post-procedure care significantly reduce this risk.
- Pain: While discomfort is possible, it’s usually mild and can be managed with analgesics. Appropriate patient preparation and explanation can minimize pain.
- Cervical Stenosis: In rare cases, repeated biopsies may lead to narrowing of the cervical canal (stenosis), which can impact future pregnancies. This is a rare complication and is largely avoidable with proper technique.
- Reaction to Solutions: Some patients may have a mild allergic reaction to the acetic acid or Lugol’s iodine solution applied during colposcopy, this is usually mild and transient.
Proper patient selection, meticulous technique, and appropriate post-procedure care are essential in minimizing the risk of these complications.
Q 21. How do you manage a patient who refuses cervical cancer screening?
When a patient refuses cervical cancer screening, it’s vital to approach the situation with empathy and understanding. The refusal might stem from various reasons, including fear, lack of knowledge, cultural beliefs, or previous negative experiences.
- Non-judgmental Conversation: Begin by creating a safe space for open communication. Listen to the patient’s concerns without judgment and explore the reasons behind their refusal.
- Education and Counseling: Provide accurate and accessible information about cervical cancer, screening methods, and the benefits of early detection. Address any misconceptions or fears the patient might have.
- Shared Decision-Making: Emphasize that the decision about screening is theirs. Explain the risks and benefits of screening and help them weigh the options to empower their choice.
- Addressing Barriers: Identify and attempt to resolve any barriers to screening, such as lack of insurance, transportation difficulties, or cultural barriers. Connecting the patient with resources to address these barriers can facilitate access to care.
- Documentation: Thoroughly document the patient’s refusal, including the reasons provided, the information shared, and any resources offered. This is important for legal and medical record-keeping purposes.
- Follow-up: Schedule a follow-up appointment to revisit the topic and provide further support, if appropriate. Avoid pressuring the patient; instead, offer ongoing support and reiterate that the decision rests with them.
Respecting patient autonomy is critical. Even if we believe screening is beneficial, the patient’s right to refuse must be upheld. However, continued education and support are key to potentially changing their mind in the future.
Q 22. How do you address patient concerns about false positive results?
Addressing patient concerns about false positives in cervical cancer screening is crucial for maintaining trust and ensuring continued participation in preventative care. A false positive means the test suggests cancer when, in fact, it’s not present. This can cause significant anxiety and distress. My approach involves a multi-pronged strategy:
Empathy and Validation: I begin by acknowledging the patient’s feelings. Saying something like, “I understand this news is upsetting, and it’s completely normal to feel anxious after receiving a positive screening result.” helps establish a supportive environment.
Clear Explanation: I clearly explain the limitations of the test. I emphasize that a positive Pap smear or HPV test doesn’t automatically mean cancer. Many factors can cause abnormal results, including inflammation or infection. I use analogies, like comparing it to a smoke detector that sometimes goes off due to burnt toast, not a fire.
Detailed Explanation of Next Steps: I outline the precise next steps, emphasizing that further investigation, such as a colposcopy, is necessary to determine the cause of the abnormality. I explain the procedure in detail, answering all questions patiently. I reassure them that this is a standard procedure and that most women with abnormal screenings do not have cancer.
Realistic Expectations: I manage expectations about the time it might take to get conclusive results. I explain that the process may involve several appointments, and I set realistic timelines for each step.
Ongoing Support: I offer ongoing support throughout the process, ensuring the patient feels heard and understood. This includes providing contact information for follow-up and making myself available to answer questions.
Q 23. What is your experience with managing patients with a history of cervical cancer?
Managing patients with a history of cervical cancer requires a holistic and long-term approach. My experience involves close monitoring for recurrence, managing treatment-related side effects, and providing ongoing psychosocial support. This includes:
Regular Follow-up Appointments: I schedule regular follow-up appointments, including pelvic exams and imaging studies (such as CT scans or MRIs), to monitor for signs of recurrence. The frequency of these appointments depends on several factors, including the stage of the original cancer and the type of treatment received.
Symptom Management: I actively manage symptoms related to treatment, such as pain, fatigue, or urinary/bowel issues, using medication, physical therapy, or other appropriate interventions. This includes open communication with the patient and tailoring the treatment plan to their specific needs.
Psychosocial Support: I recognize the significant emotional impact of a cancer diagnosis and its treatment. I provide or refer patients to counseling or support groups to help them cope with the physical and emotional challenges they face. This is crucial for their overall well-being and ability to manage their long-term health.
Collaboration with Other Specialists: I collaborate closely with oncologists, radiologists, and other specialists to ensure comprehensive and coordinated care for the patient. This multidisciplinary approach is essential for successful long-term management.
Q 24. Describe your experience working in a multidisciplinary team setting.
My experience in multidisciplinary team settings, particularly in cervical cancer care, has been extensive and highly rewarding. I routinely work alongside gynecologists, oncologists, pathologists, radiologists, nurses, and social workers. Effective teamwork is vital for optimal patient outcomes. My contributions include:
Collaborative Diagnosis and Treatment Planning: I actively participate in tumor boards and case conferences, contributing my expertise in cervical cancer screening and pathology interpretation to help create comprehensive treatment plans.
Effective Communication: I ensure clear and consistent communication among all team members, sharing relevant patient information and facilitating seamless transitions between different stages of care.
Shared Decision-Making: I participate in shared decision-making processes, ensuring the patient’s preferences and values are integrated into treatment plans.
Education and Training: I frequently participate in educational initiatives within the team, sharing knowledge and best practices related to cervical cancer screening and management.
For example, in one case, a patient presented with an abnormal Pap smear. Through collaborative discussion with the gynecologist and pathologist, we were able to promptly initiate a colposcopy, leading to early detection and intervention before the cancer progressed.
Q 25. How do you handle difficult or emotionally challenging patient interactions?
Handling difficult or emotionally challenging patient interactions is a critical aspect of my role. My approach emphasizes empathy, active listening, and a focus on building trust. I utilize the following strategies:
Active Listening: I carefully listen to the patient’s concerns without interrupting, validating their feelings, and acknowledging the emotional weight of their situation. I use reflective listening techniques to ensure I understand their perspective.
Empathy and Validation: I demonstrate empathy by acknowledging the patient’s feelings and experiences. This helps establish rapport and creates a safe space for open communication.
Clear and Honest Communication: I communicate clearly and honestly, using language the patient understands. I avoid medical jargon and tailor my explanations to the individual’s level of understanding.
Setting Boundaries: In challenging situations, I set clear and respectful boundaries while maintaining a professional and compassionate approach. I ensure my own emotional well-being is protected.
Seeking Support When Needed: I recognize that not every interaction can be managed alone. I seek support from colleagues, supervisors, or mental health professionals when needed.
For instance, I’ve had patients struggling with the emotional impact of a diagnosis, who needed additional time and support to process information. This required patience, a collaborative approach with social work services, and ongoing support to help the patient through their journey.
Q 26. How do you maintain patient confidentiality in a healthcare setting?
Maintaining patient confidentiality is paramount in healthcare. I adhere strictly to HIPAA regulations and institutional policies regarding patient privacy. My practices include:
Strict Adherence to HIPAA: I am thoroughly familiar with HIPAA regulations and ensure all my actions comply with these guidelines.
Secure Data Handling: I only access patient information when necessary for clinical care and maintain secure data handling practices, including password protection and secure disposal of paper records.
Limited Access to Information: I limit access to patient information to authorized personnel only.
Confidential Communication: I conduct all communication regarding patient information in private settings and ensure that conversations cannot be overheard.
Reporting Breaches: I promptly report any breaches in confidentiality according to established protocols.
This includes careful handling of electronic health records, ensuring only authorized individuals have access, and using appropriate methods for communicating with patients and other healthcare providers.
Q 27. Explain the process for reporting suspected cervical cancer cases.
Reporting suspected cervical cancer cases follows a well-defined process designed to ensure prompt diagnosis and treatment. The steps typically involve:
Initial Assessment: When a concerning finding arises during a Pap smear or HPV test, further evaluation, such as a colposcopy, is conducted.
Biopsy: If the colposcopy reveals suspicious areas, a biopsy is performed to obtain tissue samples for microscopic examination.
Pathology Report: The pathologist examines the biopsy sample to determine whether cancer cells are present. The report will provide a detailed description of the findings, including the type and stage of cancer if present.
Notification and Referral: If the pathology report confirms the presence of cervical cancer, the patient’s physician will inform the patient and refer them to an oncologist or other specialist for further evaluation and treatment.
Staging and Treatment: The oncologist performs a thorough evaluation to determine the stage of the cancer. This information guides the development of a personalized treatment plan.
Reporting to Registries (if applicable): Depending on local regulations, the case may also be reported to cancer registries for tracking and research purposes.
The process emphasizes swift communication and collaboration between different healthcare professionals to ensure timely and appropriate management of the case.
Q 28. What are the latest advancements in cervical cancer screening technologies?
Cervical cancer screening technologies are constantly evolving, aiming for improved accuracy, reduced invasiveness, and cost-effectiveness. Some key advancements include:
HPV DNA Testing: HPV DNA testing has become increasingly important, offering superior sensitivity in detecting high-risk HPV types that are the primary cause of cervical cancer. This can sometimes replace or supplement traditional Pap tests.
Liquid-based Cytology: Liquid-based cytology, a technique used in Pap tests, allows for better cell preservation and visualization, improving diagnostic accuracy.
Automated Cervical Cancer Screening: Automated systems employing image analysis are being developed to improve the efficiency and consistency of Pap smear interpretation, reducing inter-observer variability.
Artificial Intelligence (AI): AI-powered algorithms are being integrated into cervical cancer screening, promising more precise and early detection of precancerous lesions.
Primary HPV Screening: Some guidelines now recommend HPV testing as the primary screening method, particularly for women over 30. This can potentially reduce the number of unnecessary follow-up procedures.
These advancements are leading to more accurate and efficient screening, reducing the number of false positives and improving early detection rates, contributing to better patient outcomes.
Key Topics to Learn for Cervical Cancer Screening Interview
- Cervical Cancer Screening Methods: Understanding the nuances of Pap smears, HPV testing, and colposcopy; including their indications, limitations, and interpretation of results.
- Risk Factors and Prevention: Identifying key risk factors for cervical cancer (e.g., HPV infection, smoking, immunosuppression) and discussing preventative measures such as vaccination and regular screening.
- Screening Guidelines and Recommendations: Familiarity with current guidelines from organizations like the American Cancer Society and the USPSTF regarding screening frequency, target populations, and appropriate age ranges.
- Interpreting Cytology and Histopathology Reports: Demonstrating the ability to understand and interpret common terminology and results from cervical cytology and biopsy reports.
- Patient Counseling and Education: Describing effective strategies for communicating complex medical information to patients about cervical cancer screening, risks, and benefits, including addressing patient concerns and anxieties.
- Ethical Considerations and Informed Consent: Understanding the ethical implications of cervical cancer screening, including informed consent procedures and addressing issues related to patient autonomy and confidentiality.
- Quality Assurance and Program Evaluation: Knowledge of quality assurance measures in cervical cancer screening programs and the ability to evaluate program effectiveness and identify areas for improvement.
- Data Analysis and Reporting: Demonstrating the ability to analyze screening data, identify trends, and report findings to relevant stakeholders.
- Emerging Technologies and Future Directions: Staying current on advancements in cervical cancer screening technologies and research, such as liquid-based cytology and HPV self-sampling.
- Case Studies and Problem Solving: Preparing to discuss real-world scenarios involving atypical results, patient management challenges, and ethical dilemmas related to cervical cancer screening.
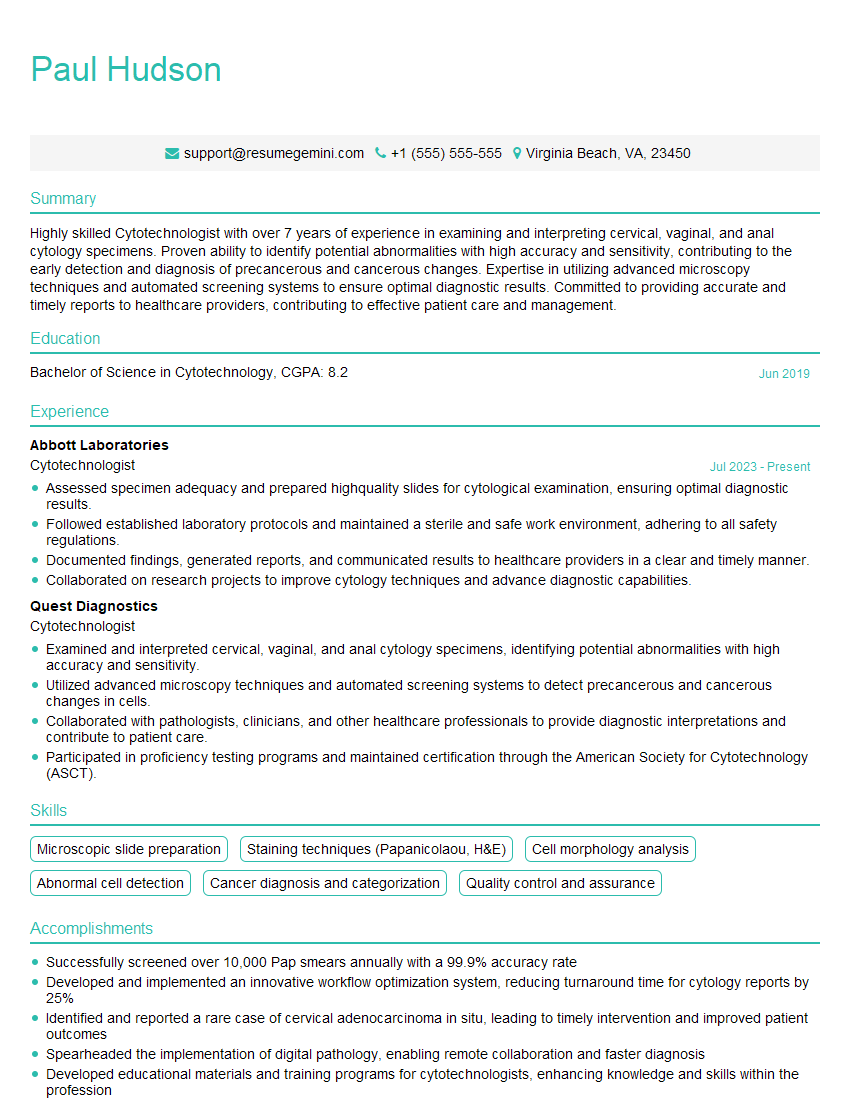
Next Steps
Mastering Cervical Cancer Screening is crucial for advancing your career in public health, healthcare administration, or clinical practice. A strong understanding of these topics will significantly enhance your interview performance and demonstrate your expertise. To maximize your job prospects, focus on creating an ATS-friendly resume that highlights your relevant skills and experience. ResumeGemini is a trusted resource that can help you build a professional and impactful resume tailored to the specific demands of the Cervical Cancer Screening field. Examples of resumes tailored to this area are provided to guide you.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.