Are you ready to stand out in your next interview? Understanding and preparing for Endometriosis Management interview questions is a game-changer. In this blog, we’ve compiled key questions and expert advice to help you showcase your skills with confidence and precision. Let’s get started on your journey to acing the interview.
Questions Asked in Endometriosis Management Interview
Q 1. Describe the diagnostic criteria for endometriosis.
Unfortunately, there isn’t a single definitive test for endometriosis. Diagnosis relies on a combination of factors, primarily clinical presentation and visualization of endometrial-like tissue outside the uterus. The diagnostic criteria essentially involve a process of elimination and confirmation.
Symptoms: A detailed history focusing on characteristic symptoms like pelvic pain, heavy menstrual bleeding, painful intercourse, and infertility is crucial. The timing and severity of these symptoms are carefully considered.
Pelvic Exam: A physical examination may reveal tenderness in the pelvis or abnormalities in the uterus or ovaries, although these findings alone aren’t diagnostic.
Imaging: Ultrasound, MRI, and CT scans can sometimes identify suspicious lesions but are not conclusive. They might suggest the presence of endometriosis but cannot definitively confirm it.
Laparoscopy: This minimally invasive surgical procedure is considered the gold standard for diagnosis. A small incision allows the surgeon to directly visualize the pelvic organs and obtain a tissue biopsy for definitive histopathological confirmation of endometrial tissue outside the uterus. The presence of characteristic lesions (endometriomas, implants) is key to the diagnosis.
In summary, a diagnosis of endometriosis often requires a thorough evaluation combining clinical presentation with a definitive laparoscopic examination and histopathological confirmation.
Q 2. Explain the different stages of endometriosis.
There isn’t a universally accepted staging system for endometriosis that’s consistently used across all clinics. However, several systems exist, and the most commonly used are based on the location, depth of invasion, and extent of endometrial implants. These systems help guide treatment strategies but don’t perfectly predict the severity of symptoms. Some systems categorize endometriosis by:
Stage I (Minimal): Superficial peritoneal implants, few and small.
Stage II (Mild): More numerous implants, possibly involving ovaries and deeper tissue.
Stage III (Moderate): More extensive involvement of organs with possible ovarian cysts (endometriomas).
Stage IV (Severe): Deep infiltrating endometriosis, significant organ involvement, and potentially adhesions (scar tissue).
The stage doesn’t always correlate directly with symptom severity; a woman with minimal disease can experience debilitating pain, while another with severe disease may have relatively mild symptoms. The classification serves as a guideline, helping to determine treatment plans rather than a precise predictor of individual experience.
Q 3. What are the common symptoms of endometriosis?
Endometriosis symptoms are highly variable, ranging from mild to debilitating. Many women experience a combination of symptoms, and the severity can fluctuate over time. Common symptoms include:
Pelvic Pain: Chronic pelvic pain is the hallmark symptom, often worsening during menstruation (dysmenorrhea).
Heavy Bleeding (Menorrhagia): Prolonged and unusually heavy menstrual bleeding is another common characteristic.
Painful Intercourse (Dyspareunia): Pain during sexual activity is a frequent complaint.
Infertility: Endometriosis can obstruct fallopian tubes and impact fertility.
Painful Urination or Defecation: If the disease involves the bladder or bowel, it can cause pain during these processes.
Fatigue: Many women report chronic fatigue alongside their other symptoms.
Bloating and Digestive Issues: Gastrointestinal symptoms, such as bloating, constipation, and diarrhea, are possible.
It’s important to note that many women with endometriosis experience no symptoms at all, making diagnosis more challenging.
Q 4. Discuss the various treatment options for endometriosis, including medical and surgical approaches.
Treatment for endometriosis is highly individualized and depends on several factors, including the severity of symptoms, the patient’s age, desire for future pregnancy, and overall health. Treatment options range from conservative medical management to surgical intervention.
Medical Management: This focuses on managing pain and reducing the growth of endometrial tissue. Options include:
Hormonal Therapy: Birth control pills, progestins, GnRH agonists/antagonists (suppress ovulation and reduce estrogen levels), and aromatase inhibitors are used to suppress the growth of endometrial tissue.
Pain Medications: Over-the-counter pain relievers (NSAIDs) and stronger prescription medications, including opioids (used cautiously due to potential for addiction), may be necessary for pain management.
Surgical Management: Surgical options aim to remove or destroy endometrial implants. These include:
Laparoscopic Surgery: Minimally invasive procedure to remove visible endometrial implants and cysts.
Laparotomy: A more extensive open surgery for more severe cases requiring removal of larger lesions or extensive adhesions.
Endometrial Ablation: Destruction of the endometrial lining of the uterus, mainly used for heavy bleeding.
Hysterectomy (with or without oophorectomy): Removal of the uterus and possibly the ovaries, a last resort usually considered for women who no longer desire childbearing and have severe symptoms refractory to other treatments.
The best approach involves a collaborative discussion between the patient and her healthcare provider to find the most suitable treatment plan.
Q 5. What are the potential complications of endometriosis?
If left untreated, endometriosis can lead to several potential complications. These complications significantly impact a woman’s quality of life and reproductive health:
Infertility: Endometriosis can cause scarring and inflammation in the reproductive organs, hindering conception. It is a significant cause of infertility.
Chronic Pelvic Pain: Untreated endometriosis often results in persistent, debilitating pelvic pain that can severely impact daily activities.
Ectopic Pregnancy: The presence of endometrial tissue outside the uterus can increase the risk of ectopic pregnancies (pregnancies outside the uterus).
Ovarian Cysts (Endometriomas): Endometrial tissue can form cysts on the ovaries, potentially leading to rupture or torsion (twisting of the ovary), which are surgical emergencies.
Bowel and Bladder Involvement: Deep infiltrating endometriosis can affect the bowel and bladder, causing severe pain, bowel obstruction, or bladder dysfunction.
Adhesions: Scar tissue formation can lead to adhesions, binding organs together and causing pain and obstruction.
Early diagnosis and appropriate management are crucial to minimize the risk of these complications.
Q 6. How do you manage chronic pain associated with endometriosis?
Managing chronic pain associated with endometriosis requires a multi-faceted approach tailored to the individual’s needs. A holistic strategy is often most effective.
Pharmacological Management: This forms the cornerstone of pain management. Options include NSAIDs for mild to moderate pain, stronger analgesics like opioids (used cautiously and sparingly due to the risk of addiction), and other pain-modifying drugs.
Hormonal Therapy: Suppressing hormone production can significantly reduce pain in many women by decreasing the growth and inflammation associated with endometrial implants.
Lifestyle Modifications: Strategies such as regular exercise, stress management techniques (yoga, meditation), and dietary adjustments can have a positive impact on pain levels. It’s important to note that the role of diet in endometriosis management is still an area of ongoing research, with some promising studies examining the impact of eliminating certain foods.
Physical Therapy: Pelvic floor physical therapy can help to improve muscle function, reduce pain, and improve overall pelvic health.
Surgical Intervention: In cases where medical management fails to provide adequate pain relief, surgery may be considered to remove or destroy endometrial lesions.
Interventional Procedures: Nerve blocks or other procedures may be used to provide temporary or longer-lasting pain relief in certain cases.
Psychological Support: Chronic pain can have a profound emotional impact. Cognitive Behavioral Therapy (CBT) and other psychological interventions can be helpful in managing the emotional toll of living with endometriosis.
It’s essential for patients to work closely with their healthcare providers to develop a comprehensive pain management plan that addresses both the physical and emotional aspects of their condition.
Q 7. Explain the role of laparoscopy in the diagnosis and treatment of endometriosis.
Laparoscopy plays a vital role in both the diagnosis and treatment of endometriosis. It is a minimally invasive surgical procedure that provides direct visualization of the pelvic organs.
Diagnosis: Laparoscopy is the gold standard for diagnosing endometriosis. During the procedure, a small incision is made in the abdomen, and a laparoscope (a thin, lighted instrument with a camera) is inserted to visualize the pelvic organs. The surgeon can directly observe characteristic lesions of endometriosis, such as implants and endometriomas. Tissue samples (biopsies) can be collected and sent for histopathological examination to confirm the presence of endometrial tissue outside the uterus. This direct visualization surpasses the limitations of other imaging techniques which can be inconclusive.
Treatment: Laparoscopic surgery is also widely used to treat endometriosis. The surgeon can remove or destroy endometrial implants and cysts, thereby alleviating pain and improving fertility potential. This minimally invasive approach reduces recovery time and minimizes scarring compared to open surgery (laparotomy). Laparoscopic excision of endometriomas and implants is generally preferred over ablation methods as it offers greater precision and reduces the risk of recurrence.
In summary, laparoscopy is an indispensable tool in both the diagnostic journey and the therapeutic management of endometriosis. It combines diagnostic accuracy with effective minimally invasive treatment capabilities.
Q 8. What are the current advancements in endometriosis research?
Endometriosis research is rapidly evolving, focusing on improved diagnostics, targeted therapies, and a deeper understanding of the disease’s pathogenesis. Several key advancements are underway:
Improved Imaging Techniques: Researchers are exploring advanced imaging modalities like MRI and ultrasound with contrast agents to enhance the detection of endometriosis lesions, particularly those that are deeply infiltrating.
Biomarkers: Studies are actively searching for reliable biomarkers in blood or other bodily fluids that can definitively diagnose endometriosis, eliminating the need for invasive procedures in many cases. This is a crucial area because currently, diagnosis relies heavily on laparoscopy.
Targeted Therapies: The development of drugs that specifically target the underlying mechanisms of endometriosis, such as inflammation and immune dysregulation, is a major focus. This includes exploring novel hormonal therapies and immunotherapies that offer more precise treatment with fewer side effects.
Genetic Research: Scientists are investigating the genetic factors that contribute to the development and progression of endometriosis to identify individuals at higher risk and develop personalized treatment strategies.
Minimally Invasive Surgery Techniques: Advances in robotic and laparoscopic surgery are leading to less invasive procedures with quicker recovery times for patients undergoing surgical management of endometriosis.
These advancements hold great promise for improving the lives of women affected by this challenging condition.
Q 9. How do you counsel patients about fertility concerns related to endometriosis?
Counseling patients about fertility concerns is a crucial aspect of endometriosis management. It’s essential to approach this conversation with empathy and provide accurate, evidence-based information. My approach typically includes:
Explaining the impact of endometriosis on fertility: I clearly explain how endometriosis can affect fertility by causing inflammation, scarring, and distortion of the pelvic organs, potentially hindering egg release, fertilization, and implantation.
Individualized assessment: I carefully assess each patient’s reproductive goals and desires, understanding that some may prioritize preserving fertility while others may be ready to move forward with family planning or have already completed their family.
Discussing treatment options and their impact on fertility: We discuss the various treatment approaches—hormonal therapies, surgery, and assisted reproductive technologies (ART)—and their potential effects on fertility. For example, some hormonal therapies can temporarily suppress ovulation, while surgery may improve fertility outcomes in some cases.
Referral to specialists: If necessary, I refer patients to reproductive endocrinologists or fertility specialists for further evaluation and guidance regarding ART options like in-vitro fertilization (IVF).
Providing emotional support: Infertility can be emotionally challenging, and I offer emotional support and resources to help patients cope with the stress and uncertainty.
It is important to remember that not all women with endometriosis will experience infertility, and many women with endometriosis successfully conceive naturally or with the assistance of fertility treatments.
Q 10. Describe the different types of surgical procedures used to treat endometriosis.
Surgical procedures for endometriosis range from minimally invasive to more extensive approaches, tailored to the patient’s specific condition and needs. Common procedures include:
Laparoscopy: This minimally invasive technique involves small incisions and a camera to visualize and remove endometrial implants. It is frequently used for diagnosis and treatment of early-stage endometriosis.
Laparotomy: A more extensive open surgical procedure required for severe or deeply infiltrating endometriosis. This allows for the removal of larger lesions and extensive adhesions.
Ovarian Cystectomy: Surgical removal of endometriomas (chocolate cysts) on the ovaries.
Endometrioma excision: Precise removal of endometriomas with intention of preserving ovarian tissue.
Uterine Nerve Ablation (UNA): Performed to reduce chronic pelvic pain by disrupting pain signals to the uterus.
Sacrocolpopexy: Surgical procedure to repair pelvic organ prolapse.
Bowel Resection: Removal of bowel sections involved with endometriosis, if necessary.
The choice of procedure depends on several factors, including the extent and location of endometriosis, the patient’s symptoms, and her reproductive goals. Post-operative management is crucial for optimal outcomes.
Q 11. What are the long-term effects of endometriosis on a patient’s health?
The long-term effects of endometriosis can significantly impact a woman’s overall health and well-being. These can include:
Chronic Pelvic Pain: This is a hallmark symptom, often persisting even after treatment.
Infertility: Endometriosis can significantly impair fertility, leading to difficulty conceiving.
Reduced Quality of Life: The chronic pain and other associated symptoms can negatively affect work, relationships, and overall daily functioning.
Increased Risk of Ovarian Cancer: Though the risk is elevated, it remains relatively low.
Increased Risk of Ectopic Pregnancy: Pregnancy outside the uterus is more likely.
Fatigue: Persistent tiredness is very common among women with endometriosis.
Depression and Anxiety: The chronic nature of the disease and its impact on daily life can contribute to mental health issues.
Bowel and Bladder Dysfunction: In advanced cases, endometriosis can affect bowel and bladder function, causing pain, urgency, or incontinence.
Regular follow-up care is essential to monitor for any complications and manage symptoms effectively over the long term.
Q 12. How do you differentiate endometriosis from other conditions with similar symptoms?
Differentiating endometriosis from other conditions with similar symptoms can be challenging, as many conditions share overlapping symptoms like pelvic pain and irregular bleeding. Careful history taking, physical examination, and appropriate diagnostic tests are crucial. Conditions to consider include:
Adenomyosis: This condition involves the growth of endometrial tissue into the uterine muscle. It is often differentiated through imaging and sometimes requires a biopsy.
Pelvic Inflammatory Disease (PID): An infection of the female reproductive organs, often associated with sexually transmitted infections. Symptoms are usually more acute and accompanied by fever and vaginal discharge.
Irritable Bowel Syndrome (IBS): A chronic gastrointestinal disorder characterized by abdominal pain, bloating, and altered bowel habits. Careful history and bowel symptom assessment can be helpful in differentiation.
Ovarian Cysts: Fluid-filled sacs on the ovaries. Imaging techniques can typically help differentiate between ovarian cysts and endometriomas.
Fibroids: Benign tumors that grow in the uterus. Often diagnosed through imaging studies like ultrasound or MRI.
A thorough evaluation, often involving imaging and sometimes laparoscopy, is necessary for an accurate diagnosis.
Q 13. What are the limitations of current diagnostic tools for endometriosis?
Current diagnostic tools for endometriosis have limitations, leading to delays in diagnosis and impacting treatment initiation. The major limitations include:
Lack of a definitive diagnostic test: There is no single blood test or imaging technique that can reliably diagnose endometriosis. Laparoscopy, a surgical procedure, remains the gold standard for diagnosis, which is invasive.
Subjectivity in imaging: Imaging studies like ultrasound and MRI can miss small or deeply infiltrating lesions, leading to underdiagnosis.
Variability in symptom presentation: Symptoms of endometriosis can vary greatly between individuals, making it challenging to rely solely on clinical presentation for diagnosis. Some women have minimal or no symptoms.
High cost and invasiveness of laparoscopy: Laparoscopy, while the gold standard, is an invasive procedure with associated risks and costs.
The need for more accurate, non-invasive diagnostic tools is a major area of focus in endometriosis research.
Q 14. Explain the role of hormonal therapy in managing endometriosis.
Hormonal therapy plays a significant role in managing endometriosis symptoms, particularly pain and heavy bleeding. It works by suppressing or modifying the hormonal environment that fuels the growth and activity of endometrial implants. Commonly used hormonal therapies include:
Combined Oral Contraceptives (COCs): These pills contain estrogen and progestin, helping to regulate the menstrual cycle and reduce the stimulation of endometrial tissue.
Progestins: These medications reduce the production of estrogen, inhibiting the growth of endometrial implants. They can be administered orally, injectably, or through an intrauterine device (IUD).
GnRH agonists and antagonists: These medications suppress the production of estrogen and progesterone, effectively creating a state of artificial menopause. They are highly effective in reducing pain but can cause significant side effects like hot flashes and bone loss, requiring careful monitoring.
Danazol: A synthetic steroid that reduces the production of certain hormones, resulting in decreased endometrial growth. It has many side effects and is less commonly used now.
The choice of hormonal therapy depends on various factors, including the patient’s age, reproductive goals, symptom severity, and personal preferences. It is crucial to monitor for side effects and adjust the treatment as needed.
Q 15. Discuss the use of pain medication in endometriosis management.
Pain management is a cornerstone of endometriosis care, as chronic pelvic pain is a hallmark symptom. We utilize a multi-modal approach, tailoring treatment to the individual’s pain level and response. This often involves a combination of strategies.
- Over-the-counter analgesics: Such as ibuprofen or naproxen, are often the first line of defense for mild to moderate pain. These are NSAIDs (Non-Steroidal Anti-Inflammatory Drugs) and work by reducing inflammation.
- Prescription pain medications: For more severe pain, we might prescribe stronger analgesics like opioids (e.g., codeine, oxycodone) or other pain relievers. Opioid use is carefully managed due to the risk of dependence and side effects. We often explore alternative options first.
- Other pain management strategies: This includes therapies such as physical therapy to address pelvic floor muscle tension, nerve blocks to target specific nerve pathways, and even psychological support such as Cognitive Behavioral Therapy (CBT) to help manage pain perception and coping mechanisms.
For example, a patient with mild pain during their period might successfully manage their symptoms with ibuprofen. Conversely, a patient with debilitating chronic pain may require a combination of opioids, physical therapy, and CBT.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you assess the effectiveness of endometriosis treatment?
Assessing treatment effectiveness in endometriosis requires a holistic approach, looking beyond just pain reduction. We use several key measures:
- Pain scores: Patients regularly complete pain diaries or questionnaires (e.g., visual analogue scale) to track pain levels and intensity.
- Symptom improvement: We assess changes in other symptoms associated with endometriosis, such as heavy bleeding (menorrhagia), painful intercourse (dyspareunia), and bowel or bladder problems.
- Quality of life measures: We use standardized questionnaires to gauge how endometriosis impacts patients’ daily lives, their work, and relationships. Improved quality of life is a significant indicator of successful treatment.
- Imaging studies: Repeat imaging (ultrasound, MRI) may be used to evaluate the size and extent of endometriosis lesions and assess changes after treatment, particularly after surgery.
- Biomarkers: Research is ongoing in the use of blood tests to measure levels of specific markers associated with endometriosis, potentially assisting in monitoring treatment response.
For instance, a patient might report a significant reduction in pain scores, improved bowel function, and a better overall quality of life after undergoing surgery, demonstrating successful treatment.
Q 17. What are the potential risks and benefits of each treatment option?
Treatment options for endometriosis vary widely, each carrying potential benefits and risks. It’s crucial to discuss these carefully with patients to facilitate informed decision-making.
- Medical Management (Hormone Therapy): Benefits include pain reduction and suppression of endometriosis growth. Risks may include weight gain, mood changes, and increased blood clot risk. Examples include hormonal contraceptives (pills, IUDs), GnRH agonists/antagonists.
- Surgical Management: Benefits include removal of endometriosis lesions, improving fertility potential (in some cases), and providing long-term pain relief. Risks involve potential complications like infection, bleeding, and bowel/bladder injury. Types include laparoscopy (minimally invasive) and laparotomy (open surgery).
- Supportive Care: This encompasses therapies like physical therapy (helps with pelvic pain and mobility), dietary changes (reducing inflammatory foods), stress management techniques (yoga, mindfulness), and psychological counseling. Risks are minimal, but effectiveness may vary between individuals.
For example, a young woman desiring pregnancy might choose hormone therapy initially, but if this fails, surgery might be considered. A patient prioritizing pain relief and not wanting children might opt for more aggressive hormone therapy or surgery.
Q 18. How do you manage patient expectations regarding endometriosis treatment?
Managing patient expectations is vital in endometriosis care, as treatment outcomes vary widely. It’s crucial to be transparent and realistic. I start by clearly explaining the disease process, treatment options, and the potential benefits and limitations of each approach.
- Realistic Goal Setting: We work collaboratively to set realistic, achievable goals. Complete cure isn’t always possible, but significant symptom improvement and improved quality of life are realistic aims.
- Open Communication: Regular communication is key. I encourage patients to ask questions and share concerns at any point. This builds trust and helps manage expectations.
- Shared Decision-Making: I empower patients to actively participate in their care by discussing options, weighing pros and cons, and making informed choices that align with their values and goals.
- Managing Setbacks: It’s important to prepare patients for the possibility of setbacks. Treatment might not work immediately, or symptoms may return. Having a plan to address these situations reduces disappointment and maintains hope.
For instance, I might tell a patient that while surgery can significantly reduce pain, it may not completely eliminate it and that long-term management with medication or other therapies may still be needed.
Q 19. How do you address psychological issues related to endometriosis?
Endometriosis significantly impacts psychological well-being. The chronic pain, fatigue, and impact on fertility can lead to anxiety, depression, and feelings of isolation. Addressing these psychological issues is as important as managing the physical symptoms.
- Screening and Assessment: I routinely screen patients for anxiety and depression using validated questionnaires.
- Referral to Mental Health Professionals: If significant psychological issues are identified, I refer patients to therapists or psychiatrists specializing in chronic pain management.
- Support Groups: Connecting patients with support groups provides a safe space to share experiences and learn coping mechanisms from others facing similar challenges.
- Psychoeducational Interventions: Education about endometriosis, pain management strategies, and available support resources can empower patients and improve their sense of control.
- Mindfulness and Relaxation Techniques: These can help patients manage stress, improve sleep, and reduce pain perception.
For example, I might recommend CBT to help a patient manage their pain and negative thoughts, or refer them to a support group to connect with other women living with endometriosis.
Q 20. Describe your experience with minimally invasive surgical techniques for endometriosis.
My experience with minimally invasive surgical techniques for endometriosis, primarily laparoscopy, has been extensive. Laparoscopy offers several advantages over open surgery, including smaller incisions, less pain, shorter hospital stays, and faster recovery times.
- Diagnostic Laparoscopy: Used to confirm the diagnosis, assess the extent of disease, and obtain tissue samples for histopathological examination.
- Therapeutic Laparoscopy: Involves removing or destroying endometrial implants through various techniques like excision, ablation, or coagulation. This often provides better long-term results compared to less invasive methods.
- Advanced Techniques: I utilize advanced techniques such as dye studies to detect subtle lesions and specialized instruments for precise excision of implants to minimize damage to surrounding tissues.
For example, in a patient with suspected deep infiltrating endometriosis (DIE), laparoscopy allows for precise visualization and removal of implants affecting the bowel or bladder, preventing extensive damage associated with open surgery. The reduced invasiveness also means faster recovery and a quicker return to daily life.
Q 21. What is your approach to managing severe cases of endometriosis?
Managing severe endometriosis cases often requires a multidisciplinary approach and a tailored strategy depending on the patient’s specific needs and goals. These patients often present with extensive disease, debilitating pain, and significant impact on their quality of life.
- Comprehensive Assessment: Thorough evaluation of the patient’s medical history, symptoms, and imaging studies is crucial to identify the extent of the disease and the impact on various organs.
- Surgical Intervention: Often, comprehensive surgery (e.g., excision of deep infiltrating endometriosis) is necessary, sometimes requiring collaboration with specialists such as colorectal surgeons or urologists.
- Medical Management: Hormonal therapies (such as GnRH agonists/antagonists, or aromatase inhibitors) are often utilized pre and post-surgery to suppress endometriosis growth and manage pain.
- Long-Term Pain Management: A multi-modal pain management approach, including medication, physical therapy, nerve blocks, and psychological support, is crucial.
- Fertility Preservation: For patients desiring pregnancy, fertility preservation strategies, such as ovarian tissue cryopreservation, might be considered prior to aggressive treatment.
For example, a patient with severe DIE affecting the bowel and bladder may require a staged surgical approach, combining laparoscopy with open surgery. Post-surgery, they might need hormone therapy, long-term pain management, and potentially psychological support to cope with the challenges of living with the condition. Our goal is always to improve their quality of life, even if complete cure is not possible.
Q 22. How do you incorporate patient preferences into treatment plans?
Shared decision-making is central to endometriosis management. I believe that treatment should always be tailored to the individual patient’s needs, values, and preferences. This means actively listening to understand their concerns about pain, fertility, and overall well-being. For instance, one patient might prioritize pain relief above all else, while another might be focused on preserving fertility. We discuss all available options – from medication and surgery to lifestyle changes and complementary therapies – explaining the benefits, risks, and limitations of each. Together, we weigh the pros and cons to arrive at a personalized treatment plan that aligns with their goals and preferences. I use validated questionnaires to assess pain levels, quality of life, and fertility desires to guide this conversation and ensure a truly patient-centered approach. This collaborative approach fosters trust and improves adherence to the chosen treatment plan.
Q 23. How do you stay up-to-date on the latest research and advancements in endometriosis management?
Staying current in the rapidly evolving field of endometriosis management is crucial. I regularly review peer-reviewed journals such as Human Reproduction Update, Fertility and Sterility, and Obstetrics & Gynecology. I actively participate in professional organizations like the American Society for Reproductive Medicine (ASRM) and the Endometriosis Foundation of America (EFA), attending conferences and webinars to learn about the latest research findings and treatment strategies. Moreover, I engage in continuing medical education (CME) courses specifically focused on endometriosis, and I frequently consult reputable online resources and clinical practice guidelines to ensure my knowledge remains up-to-date and aligned with best practices. This commitment to continuous learning is essential for providing my patients with the most effective and evidence-based care.
Q 24. Describe a challenging case of endometriosis you have managed and how you approached it.
I once managed a case of a 38-year-old patient with severe, deeply infiltrating endometriosis, affecting her bowel and bladder. She had experienced debilitating pain for over 15 years, with multiple unsuccessful surgeries. This presented a significant challenge because extensive bowel and bladder involvement increased the surgical risk. My approach involved a multidisciplinary team, including a colorectal surgeon, a urologist, and a pain management specialist. We meticulously planned the surgery using advanced imaging techniques (MRI) to map the extent of the disease. The surgery was staged to minimize complications, focusing on addressing the most critical areas first. Post-surgery, we implemented a comprehensive pain management plan, combining medication, physical therapy, and psychological support. Regular follow-ups were crucial to monitor her response and make necessary adjustments. Her case highlighted the importance of a holistic, collaborative approach in managing complex endometriosis.
Q 25. What are your views on the use of complementary and alternative medicine in endometriosis management?
Complementary and alternative medicine (CAM) therapies, such as acupuncture, yoga, and dietary changes, can be beneficial for managing some endometriosis symptoms, particularly pain and stress. However, it’s crucial to emphasize that these should be considered *supplementary* therapies, not replacements for evidence-based medical interventions. I encourage open discussions with my patients about their interest in CAM therapies, but I carefully assess their safety and efficacy. For example, while acupuncture might help manage pain, it won’t address the underlying disease process. I always ensure patients understand the limitations of CAM and that they should not delay or discontinue proven medical treatments in favor of unproven or potentially harmful therapies. A balanced approach, combining evidence-based medicine with appropriate CAM interventions tailored to the individual, can offer comprehensive symptom management.
Q 26. How would you approach a patient with suspected endometriosis who presents with infertility?
Infertility is a significant concern for many women with endometriosis. My approach to a patient with suspected endometriosis and infertility involves a thorough evaluation, including a detailed history, physical examination, and imaging studies (transvaginal ultrasound, MRI). Laparoscopic surgery is often necessary to confirm the diagnosis and assess the extent of endometriosis. Based on the findings, we discuss treatment options. This might include medical management to suppress endometriosis (hormone therapy) or surgery to remove endometrial implants. If surgery is performed, we will try to preserve fertility where possible. Assisted reproductive technologies (ART), such as in-vitro fertilization (IVF), are often considered if other treatments are unsuccessful. Throughout this process, I provide emotional support and realistic expectations, recognizing the emotional toll infertility can have on patients.
Q 27. Explain the impact of endometriosis on quality of life.
Endometriosis significantly impacts quality of life. The chronic pelvic pain can be debilitating, interfering with daily activities, work, relationships, and overall well-being. Many women experience fatigue, digestive issues, painful bowel movements, and painful urination. The emotional burden is substantial, with many patients experiencing anxiety, depression, and a decreased sense of self-worth. The impact extends beyond the individual, affecting family members and partners. The diagnosis itself can be a long and frustrating journey, adding to the emotional stress. The severity of the impact varies greatly depending on the stage and location of the disease, highlighting the need for a comprehensive assessment of the patient’s experience and a tailored management plan that addresses both the physical and psychological aspects.
Q 28. Discuss the ethical considerations related to endometriosis treatment and research.
Ethical considerations in endometriosis treatment and research are multifaceted. Informed consent is paramount, ensuring patients fully understand the benefits, risks, and alternatives to all treatment options. Equity of access to diagnosis and treatment is a major concern; disparities exist in access to specialized care based on socioeconomic status, geographic location, and insurance coverage. Research ethics must prioritize patient safety and well-being, ensuring that research protocols are carefully designed and monitored. Data privacy and confidentiality are also crucial. Finally, the potential for bias in research is an important consideration, ensuring diverse representation in studies and avoiding perpetuation of stereotypes surrounding endometriosis and its impact on women’s health. Addressing these ethical considerations is essential for ensuring that patients receive appropriate and equitable care and that research advances the field responsibly.
Key Topics to Learn for Endometriosis Management Interview
- Diagnosis and Assessment: Understanding various diagnostic methods, interpreting imaging results (ultrasound, MRI), and recognizing clinical presentations of endometriosis.
- Medical Management: Knowledge of pharmacological interventions including hormonal therapies (e.g., GnRH agonists/antagonists, combined oral contraceptives), pain management strategies, and the rationale behind treatment choices.
- Surgical Management: Familiarity with laparoscopic and open surgical techniques for endometriosis excision, including the principles of minimally invasive surgery and potential complications.
- Patient Care and Counseling: Developing effective communication strategies for patient education, addressing emotional and psychological aspects of endometriosis, and creating individualized treatment plans.
- Advanced Techniques: Understanding of emerging technologies and research in endometriosis management, such as novel imaging modalities, targeted therapies, and regenerative medicine approaches.
- Ethical Considerations: Awareness of ethical dilemmas related to informed consent, shared decision-making, and access to care, particularly in resource-constrained settings.
- Research and Evidence-Based Practice: Ability to critically appraise medical literature, apply evidence-based principles to clinical decision-making, and identify areas for future research in endometriosis management.
- Case Studies and Problem-Solving: Analyzing complex case scenarios to diagnose and develop appropriate management plans, demonstrating clinical reasoning and problem-solving skills.
Next Steps
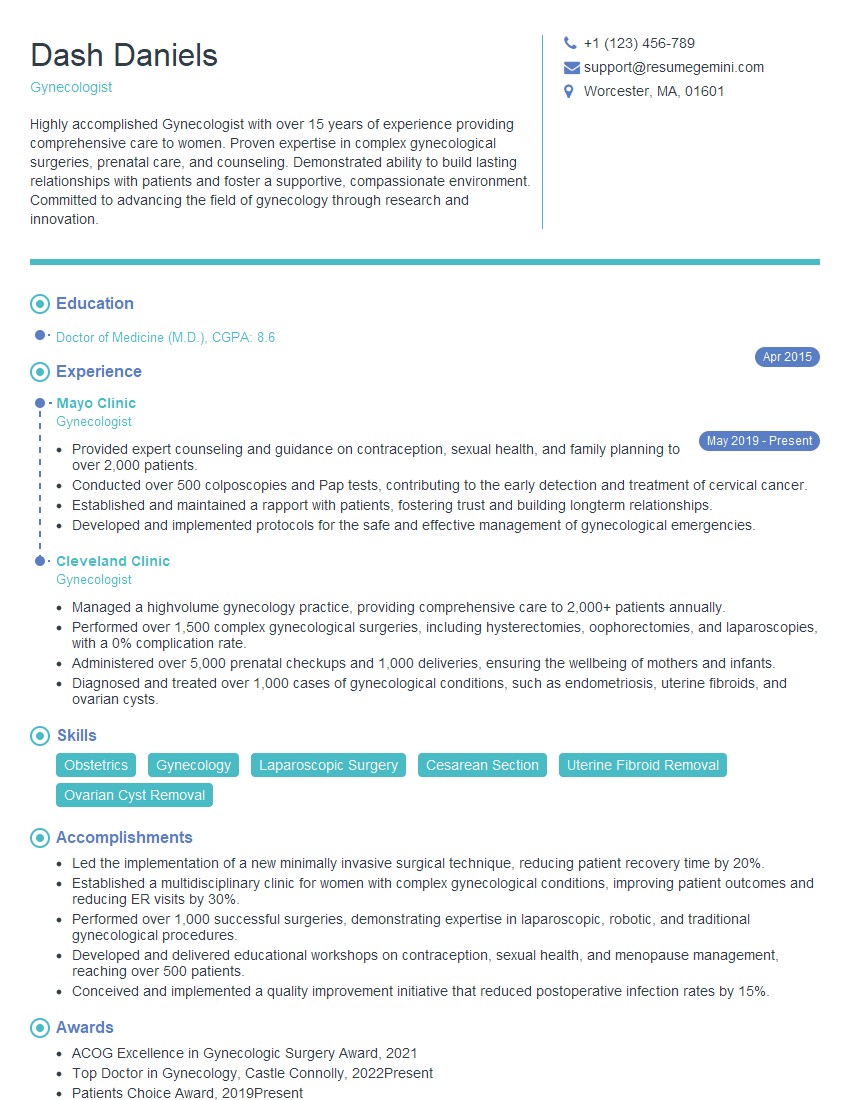
Mastering Endometriosis Management significantly enhances your career prospects in women’s health, opening doors to specialized roles and advanced opportunities. A strong resume is crucial for showcasing your skills and experience effectively to potential employers. Building an ATS-friendly resume maximizes your chances of getting your application noticed. To help you craft a compelling and effective resume, we recommend using ResumeGemini, a trusted resource for building professional resumes. Examples of resumes tailored to Endometriosis Management are available to guide you through the process.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.