Interviews are opportunities to demonstrate your expertise, and this guide is here to help you shine. Explore the essential Pre and Post-Natal Care interview questions that employers frequently ask, paired with strategies for crafting responses that set you apart from the competition.
Questions Asked in Pre and Post-Natal Care Interview
Q 1. Describe your experience with managing postpartum hemorrhage.
Postpartum hemorrhage (PPH) is a significant complication of childbirth, defined as blood loss exceeding 500ml after vaginal delivery or 1000ml after cesarean delivery. Managing PPH requires a rapid, systematic approach focusing on early identification and prompt intervention. My experience involves utilizing the 4 Ts mnemonic – Tone (uterine atony), Trauma (genital tract lacerations), Tissue (retained placenta), Thrombin (coagulopathy) – to guide assessment and treatment.
For example, if I suspect uterine atony, the primary cause of PPH, I’d initiate uterine massage, administer uterotonics like oxytocin, and consider further interventions such as intrauterine balloon tamponade or surgical procedures like uterine artery embolization or hysterectomy if conservative measures fail. If trauma is suspected, a thorough examination is crucial to identify and repair lacerations. Retained placental tissue would require manual removal. Coagulopathies require immediate blood product support and management of the underlying clotting disorder. Throughout the process, close monitoring of vital signs, blood pressure, and hemoglobin levels is paramount, alongside meticulous documentation of all interventions.
In my practice, I’ve successfully managed numerous cases of PPH, adapting my approach based on the individual patient’s circumstances and the specific cause of the bleeding. Early recognition and prompt, multidisciplinary collaboration are key to positive outcomes.
Q 2. Explain the stages of labor and delivery.
Labor and delivery is a complex process divided into three stages:
- First Stage: This stage begins with the onset of regular uterine contractions and ends with complete cervical dilation (10 cm). It is further divided into latent (early) and active phases, characterized by different rates of cervical change. Think of it as the body preparing for the baby’s journey.
- Second Stage: This stage starts with complete cervical dilation and ends with the birth of the baby. It involves pushing efforts by the mother to expel the fetus. This is the ‘pushing’ phase, where the baby crowns and is delivered.
- Third Stage: This stage begins after the baby’s birth and ends with the expulsion of the placenta. This involves monitoring for signs of placental separation and ensuring complete delivery to prevent complications like postpartum hemorrhage. Think of this as the body’s final act of ‘cleaning up’.
Each stage has its own set of monitoring parameters and potential complications, requiring tailored management. A smooth and safe delivery involves careful monitoring of maternal and fetal well-being throughout all stages.
Q 3. How do you assess fetal well-being during labor?
Assessing fetal well-being during labor is crucial to ensure a safe delivery. This is typically done through continuous electronic fetal monitoring (EFM) which measures the fetal heart rate (FHR) and uterine contractions.
We look for patterns in the FHR tracing that may indicate fetal distress, such as:
- Tachycardia or Bradycardia: An unusually fast or slow FHR.
- Late Decelerations: A drop in FHR that occurs after the onset of a uterine contraction and indicates uteroplacental insufficiency.
- Variable Decelerations: Sudden drops in FHR that are often associated with umbilical cord compression.
- Reduced Variability: Lack of fluctuation in the FHR which can suggest fetal hypoxia.
In addition to EFM, intermittent auscultation using a Doppler device can be used to assess FHR. Other assessments may include checking the amniotic fluid for meconium (fetal stool) and maternal vital signs. The interpretation of these findings necessitates clinical judgment and consideration of the overall clinical picture. If concerning patterns are identified, further interventions may be required, such as changing maternal position, administering oxygen, or even performing a cesarean section.
Q 4. What are the common complications of pregnancy?
Pregnancy can be complicated by a variety of conditions, impacting both the mother and the fetus. Some common complications include:
- Gestational Diabetes: High blood sugar levels that develop during pregnancy.
- Preeclampsia/Eclampsia: A condition characterized by high blood pressure and protein in the urine, potentially leading to seizures and organ damage.
- Preterm Labor: Labor that begins before 37 weeks of gestation.
- Placental Abruption: The premature separation of the placenta from the uterine wall.
- Placenta Previa: The placenta is positioned low in the uterus, covering the cervix.
- Ectopic Pregnancy: Implantation of the fertilized egg outside the uterus.
- Gestational Hypertension: High blood pressure during pregnancy without proteinuria.
The management of these complications varies widely, ranging from lifestyle modifications and medication to surgical interventions. Early identification and proactive management are crucial to minimize risks to both the mother and the baby. Regular prenatal check-ups are essential for early detection and prompt treatment.
Q 5. Describe your approach to providing breastfeeding support.
My approach to breastfeeding support is holistic and individualized, recognizing that each mother-baby dyad is unique. I begin with education during pregnancy, dispelling myths and promoting realistic expectations. This includes discussing the benefits of breastfeeding for both mother and baby, explaining latch techniques, and addressing common concerns like pain, milk supply, or positioning.
Postpartum, I provide hands-on support with latch assessment and positioning, offering guidance based on the individual needs of each mother and baby. I utilize various techniques to assist with latch problems and address concerns about milk supply. I empower mothers by teaching them how to recognize signs of adequate milk intake and address issues such as mastitis or engorgement. If necessary, I collaborate with lactation consultants or other healthcare professionals to provide more specialized support. I encourage mothers to maintain regular follow-up appointments, offering reassurance and ongoing encouragement throughout their breastfeeding journey. I also emphasize that breastfeeding is a personal choice, and alternative feeding methods are acceptable and should be offered without judgment.
Q 6. How do you counsel patients on newborn care?
Counseling patients on newborn care is a vital aspect of postpartum care. My approach involves a comprehensive education plan covering various aspects of newborn health and well-being. I use a combination of interactive discussions, demonstrations, and printed materials tailored to the parents’ literacy level and cultural background.
Key topics include:
- Feeding: Discussing different feeding methods (breastfeeding, formula feeding), feeding cues, and signs of adequate nutrition.
- Sleeping: Promoting safe sleep practices, including placing the baby on their back, using a firm mattress, and avoiding loose bedding.
- Diapering: Demonstrating proper diapering techniques and addressing issues like diaper rash.
- Bathing: Explaining the importance of hygiene and demonstrating safe bathing practices.
- Cord Care: Educating parents on proper umbilical cord care to prevent infection.
- Recognizing Signs of Illness: Providing parents with clear guidelines on identifying warning signs that require medical attention, such as fever, lethargy, or difficulty breathing.
I also encourage parents to ask questions, providing a safe space for them to express their concerns and receive personalized guidance. My goal is to empower parents with the confidence and knowledge they need to care for their newborn safely and effectively.
Q 7. Explain the importance of postpartum depression screening.
Postpartum depression (PPD) is a significant yet often overlooked complication of childbirth. Screening for PPD is crucial because early detection and intervention can significantly improve maternal and infant outcomes. Untreated PPD can lead to impaired mother-infant bonding, maternal self-neglect, and even severe consequences like neglect or harm to the infant.
I routinely screen for PPD using validated tools such as the Edinburgh Postnatal Depression Scale (EPDS) at various postpartum visits. The EPDS is a simple, self-report questionnaire that helps identify women at risk for PPD. If a screening tool indicates a potential issue, I conduct a thorough clinical assessment, which includes exploring the patient’s mood, sleep patterns, appetite, and overall well-being. I provide education about PPD, discuss treatment options such as therapy, medication, or support groups, and connect them with appropriate resources. Early identification, coupled with appropriate intervention, dramatically enhances maternal mental health and improves family dynamics.
Q 8. What are the signs and symptoms of preeclampsia?
Preeclampsia, also known as toxemia, is a serious condition characterized by high blood pressure and protein in the urine of a pregnant woman. It typically develops after the 20th week of pregnancy. It’s important to note that slightly elevated blood pressure isn’t automatically preeclampsia; the presence of proteinuria (protein in the urine) is a key indicator.
- Symptoms can range from mild to severe. Mild cases might show only elevated blood pressure. More severe cases can include:
- High blood pressure (hypertension): Readings consistently above 140/90 mmHg.
- Protein in the urine (proteinuria): Indicated through a urine test.
- Severe headaches: Often described as persistent and throbbing.
- Vision changes: Blurred vision, light sensitivity, or seeing spots.
- Upper abdominal pain: Often under the ribs, sometimes accompanied by nausea.
- Swelling (edema): Especially in the face, hands, and feet.
- Shortness of breath: Due to fluid retention affecting lung function.
Early detection is crucial. Regular prenatal check-ups with blood pressure monitoring and urine tests are essential for identifying preeclampsia. If any of these symptoms appear, immediate medical attention is necessary.
Q 9. How do you manage gestational diabetes?
Gestational diabetes is a type of diabetes that develops during pregnancy. It usually resolves after delivery, but increases the risk of developing type 2 diabetes later in life. Management focuses on maintaining healthy blood sugar levels through a combination of lifestyle modifications and, if necessary, medication.
- Dietary Management: A balanced diet with controlled carbohydrate intake is crucial. This often involves smaller, more frequent meals throughout the day, and focusing on whole grains, fruits, vegetables, and lean proteins. We work with registered dietitians to create individualized meal plans.
- Exercise: Regular physical activity helps improve insulin sensitivity. We recommend at least 30 minutes of moderate-intensity exercise most days of the week, unless contraindicated by other health conditions.
- Blood Glucose Monitoring: Regular blood glucose testing is essential to track blood sugar levels and adjust the management plan accordingly. This might involve home testing multiple times a day.
- Medication: If lifestyle modifications aren’t enough to control blood sugar levels, insulin therapy or oral medications might be prescribed. The choice depends on the individual’s health and response to treatment.
Regular monitoring is key. Frequent check-ups with an obstetrician and endocrinologist are needed to monitor the mother’s and baby’s health and adjust the treatment plan as needed. We carefully monitor fetal growth to detect potential complications.
Q 10. What are your strategies for pain management during labor?
Pain management during labor is a critical aspect of providing holistic care. Our approach is individualized and focuses on empowering the birthing person to choose the methods that best suit their needs and preferences.
- Non-pharmacological methods: These include relaxation techniques (breathing exercises, meditation, visualization), hydrotherapy (water immersion), massage, aromatherapy, and positioning changes. These are excellent first-line options, and often highly effective in early labor.
- Pharmacological methods: When non-pharmacological methods are insufficient, we offer a range of options, including analgesics (like opioids) and regional anesthesia (epidural, spinal). We carefully consider the stage of labor, maternal health, and fetal well-being before recommending any medication. We educate the birthing person about the benefits, risks, and side effects of each option.
- Continuous support: Emotional and physical support during labor significantly impacts pain perception. We encourage the presence of a doula, partner, or family member to provide comfort and assistance.
Our goal is to minimize pain and maximize comfort to ensure a positive birthing experience. We involve the patient in every step of the decision-making process.
Q 11. Describe your experience with assisting with vaginal delivery.
Assisting with vaginal delivery involves a collaborative approach between the obstetrician, nurses, and other healthcare professionals. My role includes providing continuous support and monitoring, preparing the delivery room, assisting with the delivery, and providing postpartum care.
- Monitoring the mother and baby: Continuous monitoring of vital signs, fetal heart rate, and maternal progress is crucial. This ensures early detection and management of any complications.
- Assisting with pushing: I guide the birthing person through the pushing stage, providing encouragement and feedback.
- Managing the perineum: I assist in protecting the perineum (the area between the vagina and anus) to reduce the risk of tearing during delivery.
- Suctioning the baby: If needed, I assist in clearing the baby’s airway.
- Providing immediate newborn care: This includes APGAR scoring, weighing, and assessing the baby’s overall health.
I’ve assisted in hundreds of vaginal deliveries, each unique and rewarding. The experience teaches you the importance of patience, adaptability, and quick decision-making. It’s incredibly fulfilling to witness the miracle of birth.
Q 12. How do you handle a breech presentation during delivery?
A breech presentation, where the baby’s buttocks or feet are positioned to come out first instead of the head, requires careful management. The decision on how to proceed depends on several factors including gestational age, fetal well-being, maternal health, and the experience of the healthcare provider.
- External Cephalic Version (ECV): This is an attempt to manually turn the baby to a head-down position before labor begins. It’s usually attempted after 37 weeks of gestation and requires careful monitoring of both the mother and the baby.
- Vaginal Delivery: In some cases, vaginal delivery is possible with a breech presentation, but it requires expertise and often involves specific techniques such as assisted breech delivery. This is typically only attempted by experienced clinicians.
- Cesarean Section: A cesarean section is often the safest option for breech presentations, particularly for first-time mothers and babies with certain risk factors. This is often the preferred method due to reduced risk of complications for both mother and baby.
The choice of management strategy is crucial and requires a shared decision-making process between the obstetrician and the birthing person. The risks and benefits of each option are carefully weighed.
Q 13. Explain your approach to cesarean section care.
Cesarean section care encompasses the entire process, from pre-operative preparation to post-operative recovery. My approach involves comprehensive patient education, meticulous surgical technique, and thorough post-operative monitoring.
- Pre-operative care: This includes detailed explanations of the procedure, addressing the patient’s anxieties and concerns, reviewing medications and allergies, and ensuring informed consent.
- Intra-operative care: Maintaining sterility, performing the surgery with precision, minimizing blood loss, and ensuring the safety of both the mother and the baby are my top priorities.
- Post-operative care: This focuses on pain management, monitoring vital signs, wound care, early mobilization, bowel and bladder function assessment, and providing emotional support. We also discuss the recovery process and provide guidance on appropriate exercises.
Post-operative care is just as vital as the surgery itself. We strive to minimize complications and promote optimal healing and recovery. We monitor for signs of infection, bleeding, and other potential problems. Open communication and patient education are essential throughout the entire process.
Q 14. Describe the importance of newborn screening tests.
Newborn screening tests are crucial for early detection of potentially serious, but treatable, conditions. Early identification allows for timely interventions, significantly improving the child’s long-term health outcomes. These tests are typically performed shortly after birth, usually within 24-48 hours.
- Metabolic disorders: These tests screen for conditions like phenylketonuria (PKU) and hypothyroidism, which, if left untreated, can lead to severe intellectual disability.
- Hearing loss: Early detection of hearing loss allows for early intervention and therapies, improving language development.
- Congenital heart defects: These tests can detect subtle heart murmurs that might indicate a heart problem requiring further investigation.
- Hemoglobin disorders: Screening for sickle cell anemia and other hemoglobinopathies is critical for planning appropriate management and preventing complications.
Newborn screening saves lives and reduces the long-term impact of many preventable conditions. Parents should receive clear explanations of the tests, their significance, and the implications of the results. Early diagnosis and treatment can dramatically change a child’s life.
Q 15. What are the common concerns of new parents regarding infant feeding?
Infant feeding is a primary concern for new parents, often leading to anxiety and uncertainty. The most common concerns revolve around:
- Adequacy of milk supply: Many mothers worry about whether their baby is getting enough milk, especially in the early days. This is often fueled by anxieties around infrequent latching or a baby’s seemingly insatiable appetite.
- Latching difficulties: Successfully breastfeeding requires proper latch technique. Difficulties with latching can lead to pain for the mother and ineffective milk transfer for the baby.
- Choosing between breastfeeding and formula feeding: The decision between breastfeeding and formula feeding can be emotionally charged, with societal pressures and personal beliefs often influencing the choice. Parents need support in making informed decisions based on their circumstances.
- Baby’s weight gain: Parents closely monitor their baby’s weight gain as an indicator of adequate nutrition. Slow weight gain can trigger worries about insufficient milk intake, leading to unnecessary stress.
- Managing feeding schedules: Establishing a feeding routine can be challenging. Parents often seek guidance on how frequently to feed their baby, whether to follow a schedule, and how to recognize hunger cues.
I address these concerns by providing personalized education and support. This includes demonstrating proper latch techniques, discussing milk supply indicators (e.g., wet diapers, baby’s behavior), and helping parents understand normal feeding patterns. I offer reassurance and normalize the challenges of breastfeeding, emphasizing the importance of patience and persistence.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you counsel patients on infant sleep safety?
Infant sleep safety is paramount. My counseling emphasizes the ‘ABCs of Safe Sleep’: Alone, on their Back, in a Crib.
- Alone: Babies should sleep alone in their crib, without any blankets, pillows, toys, or bumpers. These items pose a suffocation risk.
- Back: Placing a baby on their back to sleep significantly reduces the risk of Sudden Infant Death Syndrome (SIDS).
- Crib: A firm, flat sleep surface is essential. Avoid using soft surfaces like sofas or adult beds.
Furthermore, I counsel parents on creating a safe sleep environment by:
- Maintaining a comfortable room temperature.
- Dressing the baby in appropriate clothing for the temperature.
- Avoiding overheating.
- Pacifier use: Offering a pacifier at bedtime and during naps can reduce the risk of SIDS in breastfed babies.
- Room sharing (not bed sharing): Room sharing for the first six months is recommended, but always in a separate crib.
I often share real-life examples of SIDS cases to emphasize the importance of these safety measures and address common myths and misconceptions surrounding infant sleep.
Q 17. How do you address concerns about postpartum weight loss?
Postpartum weight loss is a common concern, but it’s crucial to address it sensitively and realistically. I emphasize a gradual, healthy approach rather than focusing on rapid weight loss. The focus should be on overall well-being, not just weight.
My approach involves:
- Promoting healthy eating habits: I encourage balanced nutrition, focusing on whole foods and avoiding restrictive diets. I address any nutritional deficiencies postpartum.
- Encouraging gradual physical activity: Gentle exercise, like walking or postnatal yoga, is gradually introduced, always considering the mother’s physical recovery.
- Addressing emotional factors: Postpartum mood changes can significantly affect eating habits and exercise motivation. I assess for postpartum depression and provide appropriate referrals if necessary.
- Realistic expectations: I emphasize that weight loss takes time and that the body needs time to recover after childbirth. Rapid weight loss is generally discouraged, and I counsel patients on setting realistic goals.
- Long-term lifestyle changes: Instead of promoting short-term weight loss strategies, I focus on building sustainable healthy habits that support long-term well-being.
I use motivational interviewing techniques to empower patients to make informed decisions about their health and wellbeing. I celebrate small victories and create a supportive environment to foster success.
Q 18. What is your experience with providing family-centered care?
Family-centered care is the cornerstone of my practice. I believe that families are the experts in their own lives and should be actively involved in every decision regarding their health and well-being. I strive to create a collaborative partnership where the family’s values, beliefs, and preferences are respected and incorporated into the care plan.
My experience includes:
- Shared decision-making: I actively involve parents in developing and implementing their baby’s care plan, ensuring they understand all options and potential outcomes.
- Open communication: I maintain open and honest communication with the family, answering their questions patiently and addressing their concerns with empathy.
- Empowering families: I empower families by providing them with the knowledge and resources they need to care for their newborn. I encourage them to ask questions and advocate for their needs.
- Culturally sensitive care: I take into consideration the family’s cultural background, beliefs, and practices when developing the care plan.
- Sibling inclusion: I actively involve siblings in the process, as appropriate, to minimize disruption and ensure a smooth transition for the whole family.
For example, I recently worked with a family who preferred a natural childbirth approach. I collaborated with them to develop a birth plan that met their needs while ensuring the safety of both the mother and baby. This involved discussing pain management options and providing them with resources to help them make informed choices.
Q 19. How do you handle patient concerns or complaints?
Handling patient concerns and complaints is an essential part of providing quality care. My approach is guided by empathy, active listening, and a commitment to resolving issues fairly and efficiently.
My steps include:
- Active listening: I begin by actively listening to the patient’s concerns without interruption, showing empathy and understanding.
- Clarifying the issue: I ask clarifying questions to fully understand the nature of the complaint and the patient’s expectations.
- Acknowledging the patient’s feelings: I acknowledge the patient’s feelings and validate their concerns, even if I don’t agree with their perspective.
- Investigating the situation: I thoroughly investigate the situation to determine the facts and identify any potential areas for improvement.
- Developing a solution: I collaborate with the patient to develop a solution that addresses their concerns. This may involve apologizing for any shortcomings, implementing changes in practice, or referring the patient to appropriate resources.
- Following up: I follow up with the patient to ensure they are satisfied with the resolution and to monitor their ongoing care needs.
Documentation is crucial. I meticulously document the complaint, the steps taken to address it, and the outcome. This ensures accountability and helps to improve future care delivery.
Q 20. What are the risk factors for preterm labor?
Preterm labor, labor that begins before 37 weeks of pregnancy, has numerous risk factors. These factors can be categorized into maternal, fetal, and placental factors.
- Maternal factors: These include previous preterm birth, current infection (e.g., urinary tract infection, chorioamnionitis), multiple gestation (twins or more), pre-existing medical conditions (diabetes, hypertension, autoimmune diseases), smoking, substance abuse, inadequate prenatal care, and extreme stress.
- Fetal factors: Fetal anomalies or abnormalities can contribute to preterm labor.
- Placental factors: Placental abruption (premature separation of the placenta from the uterine wall), placenta previa (placenta covering the cervix), and placental insufficiency (inadequate blood flow to the placenta) can all trigger preterm labor.
It’s important to note that many women with these risk factors will not go into preterm labor. However, identifying these risk factors allows for proactive monitoring and interventions to reduce the risk. Regular prenatal checkups are vital for early detection and management of these potential complications.
Q 21. How do you assess fetal growth and development?
Assessing fetal growth and development is crucial for ensuring a healthy pregnancy. Several methods are used throughout pregnancy to monitor this.
- Ultrasound: Ultrasound scans, both transabdominal and transvaginal, are used to measure fetal biometric parameters such as biparietal diameter (head size), head circumference, abdominal circumference, and femur length. These measurements are compared to gestational age-specific norms to assess fetal growth.
- Fundal height measurement: This simple measurement, taken from the top of the pubic bone to the top of the uterus, provides a rough estimate of uterine size and thus fetal growth. However, it is less accurate than ultrasound.
- Fetal movement counting: Mothers are encouraged to monitor fetal movements regularly. A decrease in fetal movements can signal a potential problem and warrant further investigation.
- Biophysical profile (BPP): A BPP combines ultrasound assessment of fetal breathing movements, fetal movements, fetal tone, amniotic fluid volume, and non-stress test (NST) results to comprehensively assess fetal well-being.
- Non-stress test (NST): This test monitors fetal heart rate in response to fetal movements. A reactive NST indicates a healthy fetus.
By combining these methods, we can build a comprehensive picture of fetal growth and development. Any deviations from expected norms trigger further investigations to identify potential problems and provide timely interventions.
Q 22. Describe your experience with electronic fetal monitoring.
Electronic Fetal Monitoring (EFM) is a crucial tool in obstetrics, used to assess fetal well-being during labor and delivery. My experience encompasses both external and internal monitoring techniques. External monitoring utilizes a tocotransducer to measure uterine contractions and a Doppler ultrasound to detect the fetal heart rate (FHR). This method is non-invasive but can be less accurate. Internal monitoring, on the other hand, involves placing a fetal scalp electrode (FSE) to directly monitor the FHR and an intrauterine pressure catheter (IUPC) to accurately measure uterine contractions. This provides more precise data but carries a slightly increased risk of infection.
I’m proficient in interpreting EFM tracings, identifying patterns indicative of fetal distress, such as late decelerations, variable decelerations, and bradycardia. For example, recurrent late decelerations, where the FHR slows after the peak of a contraction, often signal uteroplacental insufficiency and require prompt intervention. I’m experienced in making clinical decisions based on EFM findings, including the need for interventions such as changing maternal position, administering oxygen, or performing a Cesarean section.
Throughout my career, I’ve actively participated in quality improvement initiatives related to EFM, ensuring accurate interpretation and timely responses to critical findings. I regularly participate in continuing medical education focused on advancements in fetal monitoring technology and interpretation techniques.
Q 23. How do you interpret a non-stress test?
A Non-Stress Test (NST) is a simple, non-invasive test used to assess fetal well-being. It involves monitoring the fetal heart rate (FHR) and its reactivity to fetal movement. A reactive NST, considered reassuring, shows at least two accelerations of the FHR (increases of at least 15 bpm above the baseline lasting at least 15 seconds) within a 20-minute period. This indicates good fetal oxygenation and a healthy nervous system.
A non-reactive NST, however, doesn’t show the required accelerations, raising concerns about potential fetal distress. In such cases, further evaluation is necessary, often using biophysical profiles (BPP) or contraction stress tests (CST). It’s crucial to remember that a non-reactive NST is not a definitive diagnosis of fetal compromise, but a signal to investigate further.
For example, a mother with gestational diabetes might have a non-reactive NST due to fetal hypoglycemia. In contrast, a mother with placental insufficiency might have a non-reactive NST due to reduced fetal oxygenation. The specific cause needs to be determined through further investigation and management.
Q 24. What is your experience with administering medications during labor?
Administering medications during labor requires careful consideration of both maternal and fetal well-being. My experience encompasses the use of various analgesics and anesthetic agents, including opioids (e.g., fentanyl, meperidine), regional anesthesia (epidural, spinal), and general anesthesia. I am skilled in assessing the appropriate medication, dosage, and timing based on the stage of labor, the mother’s medical history, and the fetal status. For instance, I’d carefully assess the risk of respiratory depression in the newborn if administering an opioid near delivery.
I’m particularly skilled in managing epidural anesthesia, a common method for pain relief during labor. This involves carefully selecting the insertion site, administering the anesthetic agent, and monitoring the mother for complications such as hypotension or unintended nerve blockade. I also have experience in managing potential complications related to medication administration, such as allergic reactions or adverse effects on the mother or fetus.
I always prioritize informed consent, ensuring that the mother understands the benefits, risks, and alternatives associated with each medication before administration. Documentation is meticulous, recording the type and dose of medication, time of administration, and maternal and fetal responses.
Q 25. What are your strategies for preventing postpartum infections?
Preventing postpartum infections is a top priority. My strategies focus on several key areas: meticulous hand hygiene for all healthcare providers, proper wound care for episiotomies or lacerations, and prompt identification and treatment of any signs of infection. Postpartum hemorrhage, a major risk factor for infection, is carefully managed through timely assessment and intervention.
Patient education plays a crucial role. I provide detailed instructions on perineal hygiene, proper wound care, and recognizing signs of infection, such as fever, increased vaginal discharge, or localized pain. I emphasize the importance of rest and adequate nutrition to support the body’s natural immune response.
Prophylactic antibiotics are sometimes indicated, for instance, in cases of prolonged rupture of membranes or Cesarean section. Early recognition and treatment of any infection are vital to prevent serious complications such as sepsis. For example, a patient presenting with a fever and foul-smelling lochia (postpartum vaginal discharge) would receive immediate assessment and treatment with antibiotics. Early identification and intervention are key.
Q 26. How do you manage a patient with a prolonged labor?
Prolonged labor, defined as labor lasting beyond a reasonable timeframe, requires careful assessment and management. The first step is to accurately determine the cause of the prolonged labor: Is it due to inadequate contractions (hypotonic uterine dysfunction), cephalopelvic disproportion (baby’s head too large for the pelvis), or fetal malposition? A thorough assessment includes a vaginal examination to assess cervical dilation and effacement, as well as fetal monitoring to assess fetal well-being.
Management strategies depend on the underlying cause. For hypotonic uterine dysfunction, augmentation of labor with oxytocin may be considered, while other interventions include amniotomy (artificial rupture of membranes). If cephalopelvic disproportion is suspected, a Cesarean section may be necessary. If the fetus is in a malposition, maneuvers such as external cephalic version may be attempted, although this depends on several factors, including fetal maturity and position.
Throughout the process, continuous monitoring of both maternal and fetal well-being is crucial. I will closely monitor for signs of maternal exhaustion, dehydration, and infection, and assess the fetal heart rate for signs of distress. Regular communication with the patient and her family is essential to ensure they are informed and involved in decision-making.
Q 27. How do you assess for potential birth trauma in the newborn?
Assessing for potential birth trauma in the newborn involves a systematic approach beginning immediately after delivery. The Apgar score, evaluated at 1 and 5 minutes after birth, provides an initial assessment of the newborn’s overall condition, focusing on heart rate, respiratory effort, muscle tone, reflex irritability, and color. A low Apgar score indicates a need for immediate resuscitation and further investigation.
A thorough physical examination is essential, focusing on signs of head injuries (cephalhematoma, caput succedaneum), clavicular fractures, nerve injuries (e.g., brachial plexus palsy), and facial nerve palsy. Detailed observation of the infant’s behavior, including alertness, tone, and feeding ability, is also critical.
Further investigations may include blood tests to assess for metabolic acidosis, and imaging studies (e.g., ultrasound, X-ray) if there’s a suspicion of fractures or intracranial injury. Early identification and treatment of any birth trauma are crucial to minimize long-term consequences. I am skilled in recognizing and managing various types of birth trauma, ensuring prompt intervention and referral to specialists if needed.
Q 28. Describe your experience with providing education on contraception.
Providing education on contraception is an integral part of comprehensive reproductive health care. My approach involves a patient-centered discussion, tailoring the information to the individual’s needs, preferences, and health status. I begin by discussing the various methods available, including hormonal methods (pills, patches, injections, implants), barrier methods (condoms, diaphragms), and intrauterine devices (IUDs).
I explain the advantages and disadvantages of each method, considering factors such as efficacy, side effects, cost, and ease of use. For example, I would discuss the increased risk of blood clots associated with some hormonal methods with patients with a history of thrombosis. For young women, long-acting reversible contraception (LARC) such as IUDs or implants may be discussed. I carefully address potential contraindications and risks for each method, ensuring patients are well-informed before making a choice.
I also provide education on proper use and follow-up care for each contraceptive method. For example, I would explain the importance of consistent use for the pill and the need for regular check-ups for IUD users. Ultimately, my goal is to empower patients to make informed decisions about their reproductive health.
Key Topics to Learn for Pre and Post-Natal Care Interview
- Prenatal Care: Understanding the stages of pregnancy, routine prenatal visits, risk assessment and management (e.g., gestational diabetes, pre-eclampsia), nutritional counseling, and education on fetal development.
- Postnatal Care: Postpartum physical and emotional changes, breastfeeding support and challenges, newborn care education (e.g., bathing, feeding, swaddling), identifying postpartum depression and anxiety, family planning counseling.
- Patient Communication and Education: Effective communication techniques for delivering sensitive information, tailoring education to diverse patient populations, addressing patient concerns and anxieties, building rapport and trust.
- Practical Application: Developing care plans based on individual patient needs, collaborating with interdisciplinary teams (physicians, midwives, nurses), documenting patient encounters accurately and comprehensively, managing emergencies effectively.
- Legal and Ethical Considerations: Understanding patient confidentiality (HIPAA), informed consent, ethical decision-making in challenging situations, recognizing and responding to potential abuse or neglect.
- Technological Proficiency: Familiarity with Electronic Health Records (EHRs), patient portals, telehealth platforms, and other relevant technologies used in prenatal and postnatal care.
- Problem-Solving: Developing critical thinking skills to analyze patient data, identify potential complications, and develop appropriate interventions. Experience with troubleshooting common issues during pregnancy and postpartum.
Next Steps
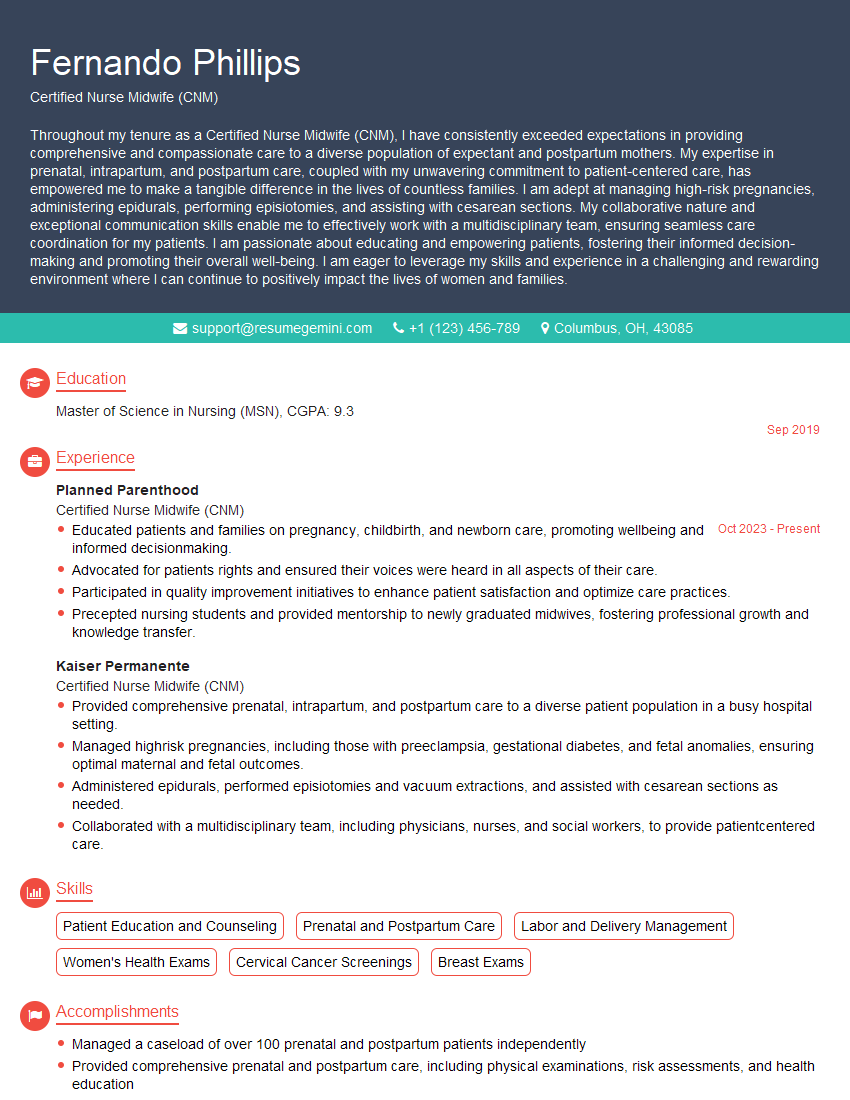
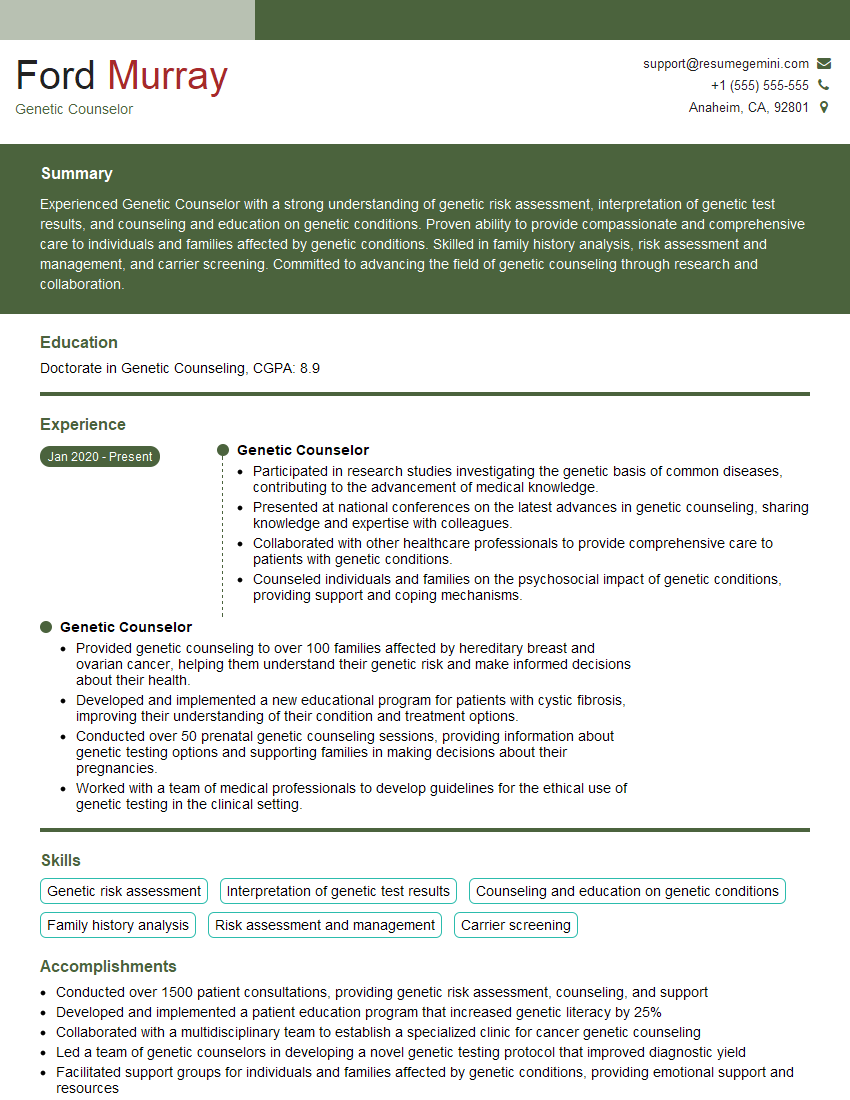
Mastering pre and postnatal care positions you for a rewarding career with significant growth potential in a field dedicated to supporting families during a crucial life stage. A strong resume is your key to unlocking these opportunities. Creating an ATS-friendly resume increases your chances of getting noticed by recruiters and securing interviews. ResumeGemini is a trusted resource to help you craft a professional and impactful resume that highlights your skills and experience effectively. Examples of resumes tailored to Pre and Post-Natal Care professionals are available within ResumeGemini to help guide you.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.