Feeling uncertain about what to expect in your upcoming interview? We’ve got you covered! This blog highlights the most important Collaborative Patient Care with Families interview questions and provides actionable advice to help you stand out as the ideal candidate. Let’s pave the way for your success.
Questions Asked in Collaborative Patient Care with Families Interview
Q 1. Describe your experience facilitating family meetings in healthcare settings.
Facilitating family meetings requires a structured yet flexible approach. I begin by establishing a safe and comfortable environment, ensuring all family members feel heard and respected. I utilize a collaborative, person-centered approach, starting with introductions and clearly stating the meeting’s purpose. The agenda typically includes reviewing the patient’s current medical status, discussing treatment options, addressing concerns, and developing a shared care plan. I actively listen to each family member’s perspective, summarize key points to ensure understanding, and encourage open communication. Following the meeting, I provide written summaries of key decisions and action items.
For example, in a recent meeting with the family of a patient recovering from a stroke, I facilitated a discussion about the patient’s rehabilitation goals, incorporating the family’s input regarding their loved one’s preferences and capabilities. This led to a more realistic and effective rehabilitation plan tailored to the patient’s specific needs and family support system.
Q 2. How do you assess family needs and preferences to incorporate them into the care plan?
Assessing family needs and preferences is crucial for developing a patient-centered care plan. I employ a multifaceted approach, combining direct questioning, observation, and utilizing validated assessment tools. This begins with open-ended questions, allowing families to express their concerns, priorities, and expectations freely. I carefully listen for verbal and nonverbal cues, acknowledging their emotions and validating their experiences. Assessment tools, such as standardized questionnaires assessing family coping mechanisms and caregiver burden, can provide quantitative data to supplement qualitative information gathered through conversation.
For instance, I might use a standardized questionnaire to evaluate the family’s capacity for providing home care. If the assessment reveals a high caregiver burden, I would then explore support services that can help reduce the strain, ensuring the family’s involvement remains sustainable and effective.
Q 3. Explain your approach to resolving conflicts between healthcare professionals and families.
Resolving conflicts between healthcare professionals and families requires skilled mediation and communication. I act as a neutral facilitator, actively listening to all perspectives and reframing statements to foster understanding. I emphasize shared goals—the patient’s well-being—and facilitate open dialogue, ensuring each party feels heard and respected. I utilize conflict resolution techniques, such as brainstorming solutions collaboratively and exploring compromise. When necessary, I involve other members of the healthcare team, such as social workers or chaplains, to provide support and expertise.
In one case, a family disagreed with a physician’s recommendation for aggressive treatment. By carefully listening to both the physician’s rationale and the family’s concerns, I helped them find common ground, ultimately leading to a treatment plan that balanced the patient’s medical needs with the family’s values and preferences.
Q 4. What strategies do you use to communicate complex medical information to families in a clear and understandable way?
Communicating complex medical information clearly necessitates using plain language, avoiding jargon, and tailoring the explanation to the family’s understanding. I use analogies, visual aids, and repetition to reinforce key concepts. I also encourage families to ask questions, addressing their concerns patiently and thoroughly. I assess their understanding continuously throughout the explanation, using teach-back techniques to confirm comprehension.
For example, when explaining a complicated diagnostic test, I might use a simple analogy to illustrate the procedure and its implications. After the explanation, I’d ask the family to explain it back in their own words to confirm their understanding. If there are gaps in understanding, I re-explain the information in a different way.
Q 5. How do you ensure cultural sensitivity and inclusivity when working with diverse families?
Cultural sensitivity and inclusivity are paramount. I begin by actively acknowledging and respecting the family’s cultural background and beliefs. I incorporate culturally appropriate communication styles, such as addressing family members by their preferred titles and being mindful of nonverbal cues. I ensure that interpreters are available when needed and seek to understand the family’s beliefs about health, illness, and treatment. I also strive to incorporate the family’s cultural preferences into the care plan, whenever possible.
For example, if working with a family from a culture where extended family plays a significant role in decision-making, I would actively involve all relevant family members in discussions. I’d also be sensitive to potential language barriers and adapt my communication style to enhance understanding.
Q 6. Describe a time you had to adapt your communication style to effectively engage a family in the care process.
I once worked with a family who was initially very reserved and reluctant to participate in discussions regarding their loved one’s care. I initially tried a more formal, structured approach, which proved ineffective. Observing their nonverbal cues, I realized a more informal and empathetic approach was necessary. I shifted to a more conversational style, sharing personal anecdotes to build rapport and focusing on their emotional needs. This created a safe space for them to express their concerns and ultimately participate actively in care decisions.
This experience highlighted the importance of flexibility and adaptability in my communication style, recognizing that a one-size-fits-all approach is not effective in every situation.
Q 7. How do you involve families in decision-making related to their loved one’s care?
Involving families in decision-making is central to collaborative patient care. I employ a shared decision-making model, providing families with the necessary information to understand their loved one’s condition, treatment options, and potential outcomes. I present information in a balanced and unbiased manner, supporting them in weighing risks and benefits, and clarifying any uncertainties. I encourage them to express their preferences and actively incorporate their input into the care plan. This process ensures that decisions reflect not only the patient’s medical needs but also the family’s values and preferences.
For example, when discussing end-of-life care, I would thoroughly explain different options like hospice care or palliative care, making sure the family understands the benefits and limitations of each choice. I would then collaboratively work with the family to arrive at a decision that aligns with the patient’s wishes and the family’s values.
Q 8. What techniques do you use to build trust and rapport with families during challenging situations?
Building trust and rapport with families, especially during challenging medical situations, is paramount. It’s about establishing a genuine connection based on empathy, respect, and open communication. I begin by actively listening to their concerns and validating their emotions. This isn’t just about hearing words, but truly understanding their perspective, their fears, and their hopes for their loved one. I use reflective listening techniques, mirroring back what they’ve said to ensure understanding and show that I’m engaged. For example, if a family member expresses worry about a potential complication, I might say, “So, it sounds like you’re concerned about the possibility of X happening, and that’s completely understandable.” This validates their feelings and opens the door for further discussion.
I also prioritize clear and honest communication, explaining medical information in a way that’s accessible and avoids jargon. I use simple language, visual aids, and analogies when necessary, ensuring the family feels informed and empowered. I make myself available for questions and address concerns promptly. Transparency and responsiveness are key to building trust. Furthermore, I demonstrate competence and confidence in my approach without being condescending, building their assurance in my expertise and capabilities. Finally, I foster collaboration, ensuring the family feels heard and involved in decision-making processes, creating a shared sense of responsibility and partnership in the patient’s care.
Q 9. How do you handle situations where family members disagree about the best course of treatment?
Disagreements among family members regarding treatment options are common and often emotionally charged. My approach focuses on facilitating constructive dialogue and collaborative decision-making. I start by creating a safe space for each family member to express their views and concerns without interruption. I actively listen to each perspective, acknowledging the validity of their emotions and concerns, even if they differ. Instead of imposing my own opinion, I act as a neutral facilitator, helping them identify their shared goals for the patient’s well-being.
I then help them explore the potential benefits and risks of each treatment option, clarifying any misunderstandings or misconceptions about medical information. I might use a decision-making framework, such as a pros and cons list, to visually organize the information and encourage a more structured discussion. The goal is to guide the family toward a consensus that aligns with the patient’s wishes and values, if known. If consensus remains impossible, I might suggest involving a mediator or ethicist to assist in the process. The focus always remains on respecting the patient’s autonomy and the family’s diverse perspectives while striving for a collaborative path forward. If the patient is capable of participating, it is essential to include their voice and preferences in the decision-making process.
Q 10. Explain your understanding of the principles of family-centered care.
Family-centered care (FCC) is a philosophy that recognizes the family as the constant in a patient’s life and the primary source of support. It emphasizes the importance of respecting the family’s values, beliefs, and cultural practices in all aspects of care. The core principles of FCC include: respect and dignity for the family; information sharing and communication; collaboration and participation in decision-making; partnership with families in care planning and delivery; and coordination of care across settings.
In practice, FCC means actively involving families in every stage of the patient’s journey, from diagnosis and treatment to discharge planning and follow-up care. This involves sharing information clearly and openly, actively listening to their concerns and preferences, and incorporating their input into the treatment plan. It also means adapting care to meet the family’s specific needs and circumstances, while respecting the patient’s autonomy and their right to self-determination. The goal is to empower families to actively participate in care, fostering a sense of partnership and improving the overall quality of care provided.
Q 11. How do you identify and address family support needs beyond direct medical care?
Identifying family support needs extends beyond the immediate medical concerns. I use a holistic approach, considering the family’s emotional, psychological, social, and financial well-being. I start by actively listening to their concerns, observing family dynamics during interactions, and assessing their overall coping mechanisms. Direct questions about their support networks, stress levels, and any challenges they are facing outside the medical realm, such as childcare, work, transportation, or financial strain, are also essential.
For instance, I might ask, “How are you managing childcare arrangements during this time?” or “Are there any financial concerns you’d like to discuss?” Based on this assessment, I can then develop an individualized support plan, connecting them with appropriate resources such as social workers, financial assistance programs, support groups, respite care, or home health services. This proactive identification of needs and referral to supportive services allows us to better address the family’s holistic needs and improve their overall well-being beyond the patient’s direct medical care.
Q 12. What resources do you utilize to support families experiencing emotional distress or financial hardship?
Many resources exist to support families experiencing emotional distress or financial hardship. For emotional support, I often connect families with hospital social workers, chaplains, or mental health professionals who can provide counseling, support groups, or other relevant services. I am also familiar with community-based organizations offering similar support, tailored to the specific needs and cultural backgrounds of families.
Regarding financial hardship, I work closely with hospital financial counselors who can help families understand their billing options, explore payment plans, or apply for financial assistance programs. I also connect them with external resources like charities, non-profit organizations, and government programs dedicated to supporting families facing financial challenges. It is crucial to identify potential barriers to care early on, such as lack of insurance or transportation, and proactively work with the family to navigate these obstacles and ensure they receive the necessary care and support.
Q 13. Describe your experience working with families facing end-of-life care decisions.
Working with families facing end-of-life care decisions requires a profound level of empathy, sensitivity, and understanding. My approach emphasizes open communication, active listening, and validation of the family’s grief and emotional experience. I help families understand the medical prognosis, treatment options (or lack thereof), and the potential trajectory of their loved one’s illness, providing clear information in a compassionate manner. I avoid medical jargon, using relatable language to clarify complex medical concepts.
I create space for open dialogue, addressing their concerns about pain management, comfort measures, and spiritual or emotional needs. I work collaboratively with palliative care specialists, chaplains, and other members of the interdisciplinary team to ensure comprehensive care. I help the family navigate difficult decisions regarding advanced care directives, life-sustaining treatments, and end-of-life care wishes. I emphasize honoring the patient’s preferences, to the best of our ability, and helping families make choices that align with these preferences and values. I also provide support and resources for bereavement counseling after the patient’s passing, recognizing the ongoing emotional needs of the family during this difficult time.
Q 14. How do you ensure effective handoffs between healthcare providers and families during transitions of care?
Effective handoffs during transitions of care are crucial to maintaining continuity and avoiding potential errors or miscommunication. I ensure comprehensive and timely information exchange between healthcare providers and families. This involves clearly documenting the patient’s medical history, treatment plan, and progress notes in the electronic health record (EHR). I also conduct detailed verbal handoffs with the incoming providers, reviewing the patient’s current status, planned interventions, and any outstanding concerns.
Critically, I include the family in this process, ensuring they receive a summary of the patient’s progress and treatment plan from both the outgoing and incoming providers. I answer their questions and address their concerns, confirming their understanding of the transition plan. If the patient is being transferred to another facility, I coordinate with the receiving team to ensure a smooth and seamless transition, addressing logistical issues such as transportation and admission arrangements. This coordinated effort reduces anxiety for the family and prevents lapses in care, ensuring that the patient’s medical needs are consistently addressed throughout their journey.
Q 15. Explain your familiarity with HIPAA regulations and their implications for family communication.
HIPAA, the Health Insurance Portability and Accountability Act, is crucial for protecting patient privacy. In the context of family communication, it dictates what information can be shared with family members and how. Essentially, we need explicit consent from the patient to discuss their health information with anyone, including family. If the patient is incapacitated, we explore options such as designated surrogates or durable power of attorney for healthcare decisions.
For example, I can’t share a patient’s diagnosis with their sibling without the patient’s consent, even if the sibling appears distressed. However, I can offer support to the family and assure them I’ll do everything possible to ensure timely and appropriate information sharing within HIPAA guidelines. This often involves explaining the patient’s rights and obtaining the necessary permissions. If a patient is incapacitated and there is no designated surrogate, we work within the hospital’s established policies to address the information-sharing needs on a case-by-case basis.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What is your approach to dealing with difficult family members who express hostility or aggression?
Dealing with hostile or aggressive family members requires a calm and empathetic approach. My first priority is ensuring the safety and well-being of everyone involved, including the patient and the healthcare team. I begin by actively listening to their concerns, validating their emotions even if I don’t agree with their expressions. Understanding the root of their aggression – fear, grief, or feeling unheard – is crucial. I might use de-escalation techniques, speaking in a quiet, calm tone, and offering them options for expressing their concerns. I would also involve other members of the healthcare team, like social workers or chaplains, as needed.
For instance, if a family member is loudly accusing the medical team of negligence, I might respond by saying something like, “I understand you’re feeling angry and frustrated right now. Let’s find a quiet place where we can talk about your concerns more calmly.” If the behavior becomes physically threatening, I’ll immediately call security for assistance.
Q 17. Describe a time you successfully advocated for a family’s needs within a healthcare system.
I once worked with a family whose child was diagnosed with a serious illness requiring extensive, costly treatment. The family was uninsured and overwhelmed by the financial burden. I advocated for them by connecting them with social workers who explored various financial assistance programs and charities. I also helped them navigate the complex insurance application process, explaining the options clearly and supporting them through each step. Additionally, I liaised with the hospital’s financial assistance department to negotiate a payment plan and explored options to reduce the overall cost of treatment. Ultimately, we secured sufficient financial assistance to ensure the child received the necessary care. The gratefulness and relief on their faces were immensely rewarding.
Q 18. How do you utilize technology to support collaboration and communication with families?
Technology plays a significant role in enhancing collaboration and communication with families. We utilize patient portals for secure messaging, allowing families to access lab results, medical records, and schedule appointments. Video conferencing platforms enable virtual family meetings, especially beneficial for families living far away or with mobility challenges. I also use secure email and phone calls, but always ensuring compliance with HIPAA regulations.
For example, I might use a video conferencing tool to walk a family through a complex treatment plan, allowing them to ask questions in real-time and fostering a more interactive and personal experience compared to a phone call.
Q 19. How do you measure the effectiveness of your collaborative efforts with families?
Measuring the effectiveness of collaborative efforts involves qualitative and quantitative approaches. Quantitative measures might include tracking patient satisfaction scores via surveys, assessing family involvement in care decisions, or analyzing the reduction in hospital readmission rates. Qualitative data comes from direct feedback from families, observations of family participation in care conferences, and evaluations from the interdisciplinary care team. We look for improved patient outcomes, increased family satisfaction, and better understanding and adherence to treatment plans as key indicators of success.
Q 20. What are some common barriers to effective family-centered care, and how do you address them?
Barriers to effective family-centered care are multifaceted. Language barriers, cultural differences, differing family dynamics (conflicts, lack of decision-making consensus), and fear or mistrust of the healthcare system are common challenges. Financial constraints, lack of access to transportation or childcare, and limited health literacy can also significantly impact participation.
To address these barriers, we utilize interpreters when necessary, provide culturally sensitive care, and ensure our communication is clear and easy to understand. We engage social workers to assist with resource coordination and support families facing financial or logistical challenges. Educational materials and support groups can help improve health literacy and empowerment. Building trust and open communication is essential to overcome these hurdles.
Q 21. Describe your experience working within an interdisciplinary team to support families.
Working within an interdisciplinary team is fundamental to effective family-centered care. Our team typically includes physicians, nurses, social workers, therapists, and case managers. We conduct regular care conferences, involving the family as active participants in the decision-making process. Each member contributes their expertise to offer holistic care that considers physical, emotional, and social aspects. Open communication, shared goals, and a collaborative approach ensure everyone is on the same page, working in the best interest of the patient and their family.
For instance, if a patient is struggling with depression following a major surgery, the nurse might report this to the social worker who can then assess for depression and facilitate appropriate support. The physician would be kept informed so that the medication could be adjusted if necessary, all while keeping the family informed and involved in the process
Q 22. How do you maintain appropriate professional boundaries while building strong relationships with families?
Maintaining professional boundaries while building strong relationships with families is a delicate balance. It’s about creating a warm and supportive environment while upholding the ethical standards of my profession. I achieve this through clear communication and consistent application of professional boundaries.
- Clear Communication: From the outset, I clearly define my role and the limits of my professional involvement. I explain that while I’m dedicated to supporting them, I have personal boundaries and professional responsibilities to uphold. This may involve setting appropriate time limits for meetings or clarifying that I won’t be involved in non-medical decisions unless directly relevant to the patient’s care.
- Respectful Listening: I actively listen to the family’s concerns, perspectives, and emotions without letting the emotional intensity of a situation blur professional boundaries. I demonstrate empathy without becoming emotionally entangled.
- Documentation: Meticulous documentation of all interactions protects both the family and myself, creating a clear record of what was discussed and agreed upon. This avoids misunderstandings and ensures professional accountability.
- Self-Reflection: I regularly reflect on my interactions with families, identifying any instances where boundaries might have been crossed, unintentionally or otherwise. This self-awareness is vital for continual professional growth.
For example, if a family member seeks my personal advice outside of medical concerns, I would politely explain that I’m not qualified to provide such advice and direct them to appropriate resources, such as a social worker or counselor.
Q 23. Explain your understanding of the ethical considerations involved in collaborative patient care with families.
Ethical considerations in collaborative patient care with families are paramount. My practice is guided by principles of autonomy, beneficence, non-maleficence, and justice.
- Autonomy: I respect the family’s right to make decisions about their loved one’s care, within legal and ethical limits. This includes providing them with all necessary information to make informed choices, even if I disagree with their decisions. I facilitate shared decision-making, not dictate treatment.
- Beneficence: I strive to act in the best interests of the patient. This involves considering the family’s values and preferences while prioritizing the patient’s well-being.
- Non-maleficence: I am committed to avoiding harm to the patient and the family. This includes careful consideration of the potential emotional and psychological impact of my actions and communication styles.
- Justice: I ensure fair and equitable treatment for all families, regardless of their background, social status, or beliefs.
- Confidentiality: I always uphold patient confidentiality, ensuring that information is only shared with individuals who have a legitimate need to know.
For instance, if a family requests a treatment that I deem medically inappropriate, I would explain the potential risks and benefits clearly and explore alternative options, involving them in the decision-making process. I would never withhold information to influence their choice.
Q 24. How do you document your interactions with families, ensuring accuracy and confidentiality?
Accurate and confidential documentation of my interactions with families is essential. I use the electronic health record (EHR) system according to my institution’s policies. My documentation includes:
- Date and time of interaction: Ensuring chronological order and easy tracking.
- Individuals present: Precisely who was involved in the discussion.
- Reason for interaction: Clearly stating the purpose of the meeting or communication.
- Discussion points: Detailed notes summarizing the conversation, including the family’s concerns, questions, and any decisions made.
- Action items: outlining next steps and any assigned responsibilities.
- Family’s expressed wishes: Documenting their preferences and decisions, even if I disagree.
All entries are factual, objective, and avoid subjective opinions or interpretations. I use professional medical terminology where appropriate but ensure that complex details are also summarized in plain language. I use strict adherence to HIPAA guidelines to maintain patient confidentiality and only access and share information on a need-to-know basis.
Q 25. Describe your experience with patient advocacy.
Patient advocacy is a cornerstone of my practice. It involves actively supporting patients and their families in navigating the healthcare system and advocating for their rights and best interests.
- Information access: Ensuring families understand medical information and have access to resources.
- Navigating systems: Assisting with paperwork, appointments, referrals, etc.
- Conflict resolution: Mediating between the family and healthcare team when disagreements arise.
- Empowering families: Equipping them with knowledge and resources to participate fully in care decisions.
For example, I recently helped a family obtain financial assistance for their child’s medication by connecting them with relevant social workers and navigating the application process. I also advocated for a patient who required specialized equipment by liaising with insurance companies and the hospital administration to expedite the process.
Q 26. How do you handle situations where family requests conflict with medically recommended treatment?
When family requests conflict with medically recommended treatment, a collaborative and ethical approach is crucial. I follow a structured process:
- Open Communication: I listen carefully to understand the family’s concerns and perspectives. This involves active listening, empathy, and validation of their feelings.
- Education and Explanation: I provide clear, comprehensive information about the medical condition, treatment options, benefits, and risks. I ensure they understand the medical rationale behind recommendations.
- Shared Decision-Making: I involve the family in a collaborative discussion to explore alternatives, address concerns, and find a mutually acceptable plan. This may involve consulting other healthcare professionals, such as ethicists or chaplains.
- Ethical Consultation: If a resolution cannot be reached, I may involve an ethics committee to assist in navigating complex ethical dilemmas and ensure appropriate decision-making.
- Documentation: All discussions and decisions are meticulously documented in the patient’s chart.
It’s essential to remember that while I provide medical expertise, the final decision rests with the family. Respecting their autonomy is key, even if it means accepting decisions that are not medically optimal. This process ensures that everyone feels heard and that decisions are made in the best interests of the patient, considering both the medical and family perspectives.
Q 27. What is your approach to providing emotional support to families facing difficult medical situations?
Providing emotional support to families facing difficult medical situations requires sensitivity, empathy, and a holistic approach.
- Active Listening: Creating a safe space for families to express their emotions without judgment.
- Empathy and Validation: Acknowledging and validating the family’s feelings of grief, fear, anxiety, or anger.
- Information and Resources: Providing accurate and accessible information about the patient’s condition and connecting them with support resources such as grief counseling, support groups, or social workers.
- Realistic Hope: Offering realistic hope and optimism while acknowledging the challenges ahead.
- Professional Boundaries: While offering emotional support, it’s vital to maintain professional boundaries, ensuring that I don’t overstep or create dependency.
For instance, if a family is grieving the loss of a loved one, I might offer my condolences, provide information about bereavement support services, and let them know that they can contact me at any time if they need to talk. I would also create a supportive space for them to process their grief and share memories of their loved one.
Q 28. How do you prioritize patient and family needs while working in a high-pressure environment?
Prioritizing patient and family needs in a high-pressure environment requires efficient time management, effective delegation, and strong organizational skills. I utilize several strategies:
- Effective Time Management: I prioritize tasks based on urgency and impact, ensuring that critical patient and family needs are addressed promptly. This includes effective scheduling and delegation of tasks.
- Clear Communication: Keeping the family informed throughout the process prevents misunderstandings and reduces anxiety. This also allows for proactive problem-solving.
- Teamwork: I collaborate effectively with other healthcare professionals to share the workload and ensure comprehensive care. This minimizes stress and improves efficiency.
- Self-Care: Prioritizing my own well-being, through activities like regular breaks, exercise, and maintaining healthy work-life balance, helps me stay focused and provide the best possible care. Burnout prevention is crucial to sustain effective patient care.
- Advocacy for Resources: When facing resource constraints, I advocate for my patients and families, securing additional support when needed. This could involve seeking additional staffing, requesting specialized services or securing financial assistance.
For example, during a busy shift, I might prioritize addressing a critically ill patient’s immediate needs first, while delegating less urgent tasks to other members of the team. Simultaneously, I ensure that I make time for short check-ins with concerned family members to provide updates and answer any questions. This approach ensures both patient and family needs are effectively addressed in a timely manner.
Key Topics to Learn for Collaborative Patient Care with Families Interview
- Family-Centered Care Principles: Understanding the core values and philosophies underpinning collaborative care, including respect for family autonomy, shared decision-making, and cultural sensitivity.
- Communication & Collaboration Strategies: Developing effective communication techniques for interacting with diverse family members, building rapport, navigating conflicts, and fostering teamwork among healthcare professionals and family members. Practical application: Role-playing scenarios to practice active listening and conflict resolution.
- Assessment & Planning with Families: Methods for assessing family needs, strengths, and resources; developing individualized care plans that incorporate family goals and preferences; and utilizing family-centered assessment tools.
- Ethical Considerations: Navigating ethical dilemmas related to patient autonomy, family disagreements, confidentiality, and cultural differences in decision-making processes.
- Legal Aspects of Family Involvement: Understanding relevant laws and regulations concerning informed consent, patient advocacy, and family rights.
- Advocacy & Support for Families: Identifying and addressing barriers to care, connecting families with necessary resources, and providing emotional and practical support throughout the care journey. Problem-solving approach: Developing strategies for navigating systemic barriers to accessing care.
- Cultural Competence & Sensitivity: Demonstrating awareness and sensitivity to diverse cultural beliefs, values, and practices impacting family involvement in healthcare.
- Measuring Outcomes & Evaluation: Methods for evaluating the effectiveness of family-centered care interventions and making necessary adjustments to improve patient and family experiences.
Next Steps
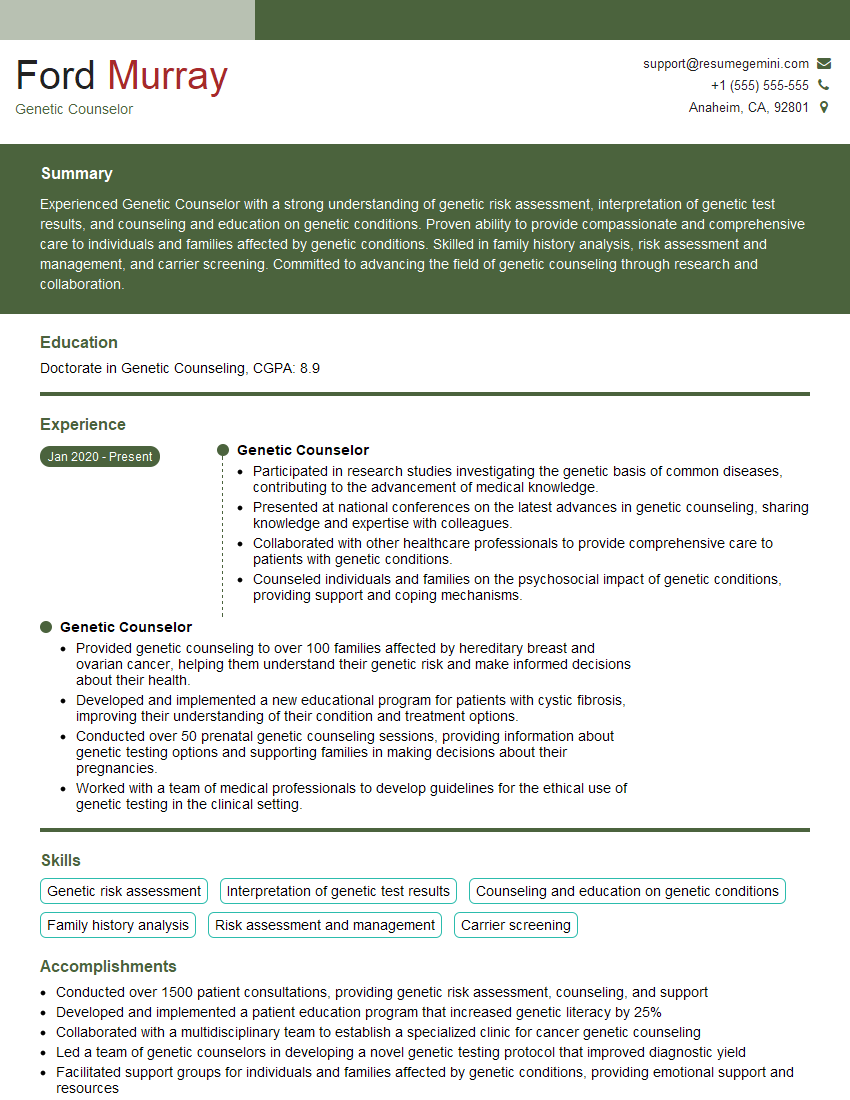
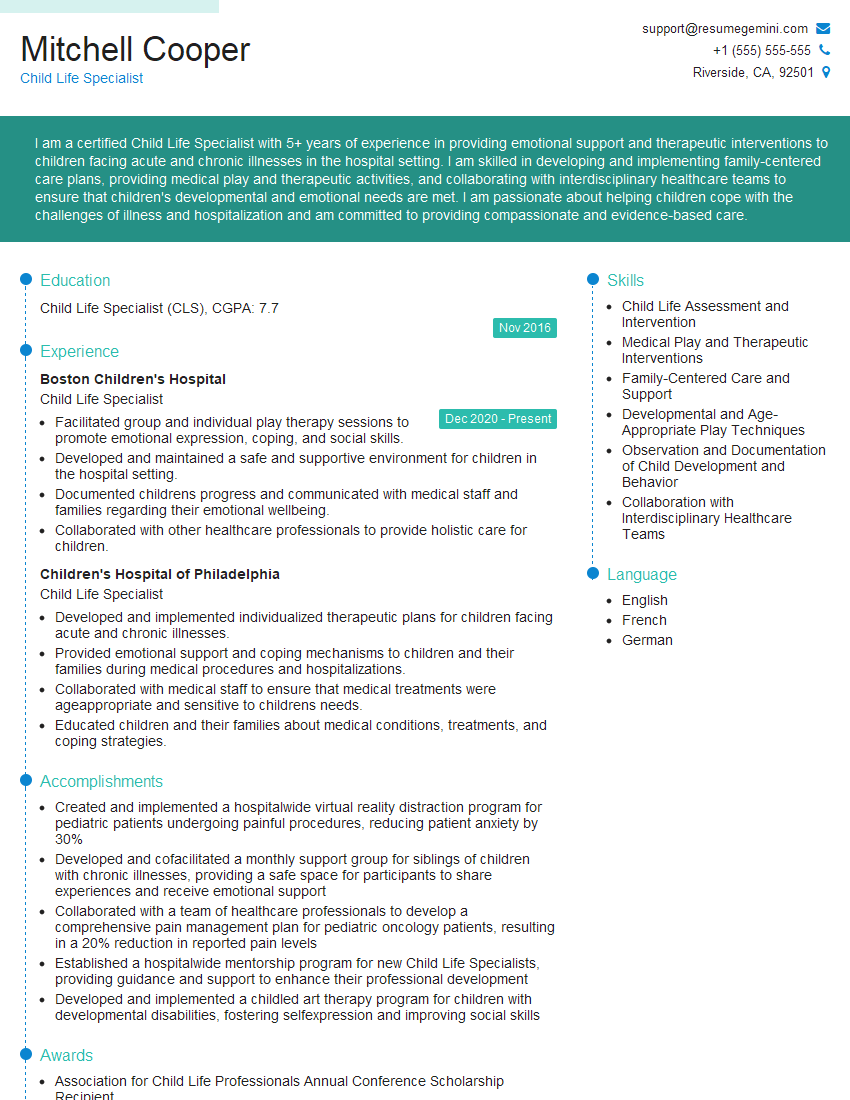
Mastering Collaborative Patient Care with Families significantly enhances your career prospects in healthcare, showcasing your ability to provide holistic, patient-centered care and work effectively within interdisciplinary teams. This skill is highly valued by employers seeking compassionate and effective healthcare professionals. To maximize your chances of securing your dream role, creating an ATS-friendly resume is crucial. This ensures your qualifications are easily identified by Applicant Tracking Systems used by many organizations. We strongly recommend using ResumeGemini to build a professional and effective resume tailored to the specifics of your experience in Collaborative Patient Care with Families. ResumeGemini provides excellent tools and resources, and offers examples of resumes specifically designed for this field to guide you.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hi, I have something for you and recorded a quick Loom video to show the kind of value I can bring to you.
Even if we don’t work together, I’m confident you’ll take away something valuable and learn a few new ideas.
Here’s the link: https://bit.ly/loom-video-daniel
Would love your thoughts after watching!
– Daniel
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.