The thought of an interview can be nerve-wracking, but the right preparation can make all the difference. Explore this comprehensive guide to Neurotrauma interview questions and gain the confidence you need to showcase your abilities and secure the role.
Questions Asked in Neurotrauma Interview
Q 1. Describe the Glasgow Coma Scale (GCS) and its clinical significance in neurotrauma.
The Glasgow Coma Scale (GCS) is a neurological scale that objectively assesses a patient’s level of consciousness. It’s crucial in neurotrauma because it provides a rapid, standardized assessment of the severity of brain injury. The GCS evaluates three key responses: eye opening, verbal response, and motor response, each scored on a numerical scale. The total score, ranging from 3 (deep coma) to 15 (fully alert), directly correlates with the severity of the brain injury and prognosis. A lower GCS score indicates a more severe injury. For instance, a score of 8 or less generally indicates a severe TBI, requiring immediate intensive care.
Clinically, the GCS is used at the initial assessment and then repeatedly to monitor changes in the patient’s condition. Tracking changes in the GCS over time can be crucial in guiding treatment decisions and predicting patient outcomes. Imagine a patient admitted after a car accident with a GCS of 12. If that score drops to 9 within a few hours, it indicates a worsening condition, prompting closer monitoring and potentially aggressive intervention.
Q 2. Explain the difference between primary and secondary brain injuries.
Primary brain injuries occur at the moment of impact and are the direct result of the traumatic force. Think of it as the initial damage. This could involve contusions (bruises), lacerations (tears), or diffuse axonal injury (damage to the connecting fibers in the brain). Secondary brain injuries, however, develop after the initial insult, often hours or days later. They are a consequence of the body’s response to the primary injury and can be just as devastating.
Examples of secondary injuries include cerebral edema (swelling of the brain), intracranial hemorrhage (bleeding within the skull), increased intracranial pressure (ICP), and infection. Imagine a patient with a primary injury – a contusion – causing swelling (secondary injury) that compresses the brain tissue, causing further neurological damage. Preventing and managing secondary injuries is a critical aspect of neurotrauma care.
Q 3. What are the common causes of traumatic brain injury (TBI)?
Traumatic brain injuries (TBIs) have numerous causes, but some of the most common include:
- Falls: Especially prevalent in elderly populations, falls are a significant contributor to TBIs.
- Motor vehicle accidents: High-impact collisions frequently result in severe TBI.
- Assaults: Blunt force trauma to the head can cause significant brain damage.
- Sports injuries: Contact sports like football and boxing carry a considerable risk of TBI.
- Penetrating injuries: Gunshot wounds or stab wounds directly damage brain tissue.
These causes often lead to a variety of injury patterns, ranging from mild concussions to severe diffuse axonal injury. Understanding the mechanism of injury is essential for guiding diagnosis and treatment.
Q 4. Discuss the management of increased intracranial pressure (ICP) in TBI.
Managing increased intracranial pressure (ICP) in TBI is critical because elevated ICP can compress brain tissue, reducing blood flow and leading to further neurological damage or even death. Treatment strategies are multifaceted and aim to reduce ICP and improve cerebral perfusion (blood flow to the brain).
Management strategies include:
- Hyperventilation: Controlled hyperventilation reduces CO2 levels, causing vasoconstriction and reducing brain volume.
- Osmotherapy: Administering mannitol or hypertonic saline draws fluid out of the brain tissue, reducing swelling.
- Fluid management: Careful control of intravenous fluids to prevent fluid overload.
- Positioning: Elevating the head of the bed to 30 degrees can help reduce ICP.
- Surgical intervention: Craniotomy (surgical removal of part of the skull) may be necessary to relieve pressure in severe cases.
- Sedation and analgesia: Keeping the patient sedated reduces metabolic demand and agitation, thus lowering ICP.
The specific management plan is tailored to the individual patient’s condition and response to treatment. Continuous monitoring of ICP is crucial to guide therapy.
Q 5. What are the imaging modalities used to diagnose neurotrauma?
Several imaging modalities play a vital role in diagnosing neurotrauma. These techniques provide detailed anatomical information and help assess the extent and location of the injury.
- Computed tomography (CT) scan: CT scans are the most commonly used initial imaging technique in neurotrauma due to their speed and ability to detect intracranial hemorrhage, bone fractures, and other structural abnormalities. They are especially useful in acute situations where rapid diagnosis is crucial.
- Magnetic resonance imaging (MRI): MRI offers superior soft tissue contrast and provides detailed images of brain parenchyma, making it useful in evaluating diffuse axonal injury, cerebral edema, and other subtle injuries that might be missed on CT.
- Magnetic resonance angiography (MRA): MRA is used to visualize blood vessels in the brain and neck, assessing for vascular injury such as aneurysms or dissections.
- Cerebral angiography: A more invasive procedure used to visualize cerebral vasculature with greater detail, helpful in certain vascular emergencies.
The choice of imaging modality depends on clinical suspicion, urgency, and the specific information required.
Q 6. Describe the clinical presentation of a patient with a cervical spine injury.
The clinical presentation of a patient with a cervical spine injury varies greatly depending on the severity and level of the injury. However, some common features include:
- Neck pain: This is often the most prominent symptom.
- Neurological deficits: Depending on the level of injury, patients may experience weakness, paralysis, numbness, or tingling in the arms, legs, or trunk. This could include loss of sensation or movement below the level of injury.
- Respiratory compromise: High cervical injuries (C1-C4) can affect the phrenic nerve, causing respiratory distress and the need for mechanical ventilation.
- Spinal shock: This is a temporary period of decreased reflexes, flaccid paralysis, and loss of sensation below the level of injury.
- Bowel and bladder dysfunction: Loss of bowel and bladder control may occur.
Immediate immobilization of the neck is crucial to prevent further injury. Any suspicion of cervical spine injury warrants careful neurological examination and appropriate imaging studies (X-ray, CT scan).
Q 7. Explain the management of spinal shock.
Spinal shock is a temporary neurogenic condition that occurs after a spinal cord injury. It’s characterized by a loss of all reflexes below the level of the injury, resulting in flaccid paralysis, loss of sensation, and loss of bowel and bladder control. It’s essential to understand that spinal shock is not permanent; it typically resolves within days to weeks.
Management of spinal shock focuses on supporting the patient’s vital functions and preventing further complications. This includes:
- Maintaining airway patency and ventilation: If respiratory function is compromised, mechanical ventilation may be necessary.
- Maintaining blood pressure: Fluid resuscitation or vasopressors may be used to maintain adequate blood pressure and perfusion to the spinal cord.
- Preventing secondary injuries: Careful monitoring and management of potential complications such as pressure sores, deep vein thrombosis (DVT), and urinary tract infections are crucial.
- Bowel and bladder management: Regular bowel and bladder programs to prevent complications.
- Rehabilitation: Once spinal shock resolves, rehabilitation therapies help restore function and improve quality of life.
Careful monitoring and supportive care are key to helping patients recover from spinal shock and maximizing their long-term outcome.
Q 8. What are the different types of skull fractures?
Skull fractures are breaks in the cranial bones, often resulting from trauma. They are classified based on several factors, including the type of fracture line and whether the bone is displaced or depressed.
- Linear fractures: These are simple, clean breaks in the bone without significant displacement or depression. Think of it like a hairline crack in a windowpane. They are often the least severe type.
- Comminuted fractures: These involve multiple fracture lines resulting in fragmentation of the bone into several pieces. Imagine a shattered window.
- Depressed fractures: In these, a fragment of the bone is pushed inwards towards the brain. This is a more serious type, as it can directly injure the brain tissue.
- Basilar skull fractures: These fractures occur at the base of the skull, often involving the temporal or occipital bones. They are difficult to diagnose by imaging alone and are often suggested by the presence of specific signs like ‘raccoon eyes’ (periorbital ecchymosis) or Battle’s sign (mastoid ecchymosis). They can involve tears in the dura and lead to cerebrospinal fluid leaks.
- Diastatic fractures: These occur at the sutures (joints) of the skull and cause widening of the suture lines.
The severity of a skull fracture depends on its type, location, and associated injuries. Even linear fractures can be associated with underlying brain injury.
Q 9. Discuss the role of neuroprotective agents in TBI management.
Neuroprotective agents are medications designed to protect the brain from secondary injury after a traumatic brain injury (TBI). Secondary injury refers to the damage that occurs after the initial impact, often due to inflammation, swelling, and excitotoxicity. While there isn’t a universally effective neuroprotective agent yet, research focuses on several strategies.
These agents aim to reduce cell death and improve functional outcomes. Examples of therapeutic strategies under investigation include:
- NMDA receptor antagonists: These drugs block the action of glutamate, a neurotransmitter that can be excessively released after TBI, leading to neuronal damage.
- Anti-oxidants: These help combat the harmful effects of free radicals, which contribute to cellular damage.
- Anti-inflammatory agents: These drugs aim to reduce inflammation in the brain, which can exacerbate damage.
- Growth factors: These promote neuronal survival and repair.
The effectiveness of neuroprotective agents in clinical practice remains a significant area of ongoing research. The challenge is often delivering these agents to the affected brain regions quickly and effectively enough to make a difference, and many trials have unfortunately failed to show substantial clinical benefit.
Q 10. Describe the assessment of cranial nerve function.
Assessment of cranial nerve function is crucial in evaluating patients with TBI to identify the location and extent of neurological damage. Cranial nerves are 12 pairs of nerves that originate directly from the brain and control various functions like eye movement, facial expression, hearing, and swallowing. A systematic assessment involves testing each nerve individually.
The assessment typically involves:
- CN I (Olfactory): Testing sense of smell.
- CN II (Optic): Assessing visual acuity and visual fields.
- CN III (Oculomotor), IV (Trochlear), VI (Abducens): Evaluating eye movements, pupil size and reactivity.
- CN V (Trigeminal): Testing facial sensation and muscle strength (jaw movements).
- CN VII (Facial): Assessing facial symmetry and muscle strength.
- CN VIII (Vestibulocochlear): Evaluating hearing and balance.
- CN IX (Glossopharyngeal), X (Vagus): Assessing swallowing, gag reflex, and voice quality.
- CN XI (Accessory): Evaluating shoulder and neck muscle strength.
- CN XII (Hypoglossal): Assessing tongue movement.
Findings are carefully documented, and any abnormalities can help pinpoint the site of neurological injury within the brainstem or other areas.
Q 11. Explain the process of managing a patient with a traumatic subdural hematoma.
Management of a traumatic subdural hematoma (SDH) depends on the size, rate of growth, and the patient’s clinical status. An SDH is a collection of blood between the dura mater (the outer layer of the brain coverings) and the arachnoid mater (the middle layer).
The process typically involves:
- Immediate stabilization: Maintaining airway, breathing, and circulation (ABCs).
- Neurological examination: Assessing level of consciousness, pupillary response, motor strength, and sensory function.
- Neuroimaging (CT scan): Identifying the location, size, and characteristics of the SDH.
- Surgical intervention (often craniotomy): If the SDH is large, rapidly expanding, causing significant neurological compromise, or showing signs of midline shift, surgical evacuation is usually necessary. This involves removing the clot and controlling the bleeding.
- Medical management: This might involve monitoring intracranial pressure (ICP), managing cerebral edema, and administering medications to reduce swelling and prevent seizures.
- Post-operative care: This includes intensive care monitoring, rehabilitation, and careful assessment for complications such as infection.
The specific treatment approach is tailored to the individual patient’s condition. Some smaller, stable SDHs may be managed conservatively with close monitoring, while others require immediate surgical intervention to prevent irreversible brain damage. Early diagnosis and prompt treatment are critical for optimal outcomes.
Q 12. What are the different types of traumatic axonal injury (TAI)?
Traumatic axonal injury (TAI) is a type of diffuse brain injury involving damage to the axons (nerve fibers) of the brain. It’s a common, and often severe, consequence of rotational or acceleration-deceleration forces to the head.
TAI is classified based on the severity and extent of axonal damage:
- Mild TAI: Characterized by subtle axonal damage with minimal clinical manifestations. Patients may experience mild cognitive impairment or headache.
- Moderate TAI: Shows more significant axonal damage, leading to more pronounced neurological deficits such as prolonged coma, and significant cognitive and motor impairments.
- Severe TAI: Involves widespread axonal damage with severe neurological deficits, including prolonged coma, significant cognitive and motor impairments, and often results in persistent vegetative state or death.
It’s important to understand that TAI is not always easily detectable by conventional neuroimaging techniques like CT scans. Advanced imaging such as diffusion tensor imaging (DTI) MRI can be helpful in detecting and characterizing axonal damage.
Q 13. Describe the rehabilitation strategies for patients with TBI.
Rehabilitation after TBI is a crucial and multifaceted process aimed at restoring lost function and maximizing independence. It’s a long-term process tailored to the individual needs of the patient. It typically involves a multidisciplinary team including neurologists, physiatrists, therapists (physical, occupational, speech), psychologists, and social workers.
Key strategies include:
- Physical therapy: Improves motor skills, strength, balance, and coordination. This might include range of motion exercises, gait training, and strengthening programs.
- Occupational therapy: Focuses on improving daily living skills, such as dressing, bathing, and eating. It also addresses cognitive impairments and adaptive strategies.
- Speech therapy: Addresses communication difficulties, including language impairments, swallowing problems, and cognitive communication disorders.
- Cognitive rehabilitation: Targets cognitive impairments like memory, attention, and executive functions. Techniques include memory strategies, problem-solving training, and attention retraining.
- Pharmacological management: Medications may be used to manage symptoms such as depression, anxiety, seizures, or spasticity.
- Psychosocial support: Addressing emotional and psychological issues associated with TBI is crucial for successful rehabilitation. Support for families and caregivers is also essential.
The rehabilitation process is individualized and iterative, regularly assessing progress and adapting interventions as needed. Recovery can vary considerably among individuals.
Q 14. What are the common complications of TBI?
Traumatic brain injury can lead to a range of short-term and long-term complications. These complications can significantly impact a patient’s quality of life and require ongoing management.
Common complications include:
- Infection: Meningitis, encephalitis, or wound infections can occur.
- Seizures: Epilepsy is a common long-term consequence.
- Hydrocephalus: Accumulation of cerebrospinal fluid within the brain can cause increased intracranial pressure.
- Post-traumatic amnesia: Loss of memory surrounding the injury.
- Cognitive deficits: Impairments in memory, attention, executive functions, and processing speed.
- Motor deficits: Weakness, paralysis, spasticity, or ataxia.
- Sensory deficits: Changes in sensation, such as numbness, tingling, or pain.
- Speech and language disorders: Aphasia (difficulty speaking) or dysarthria (difficulty articulating speech).
- Swallowing difficulties (dysphagia): Increased risk of aspiration pneumonia.
- Post-traumatic headache: Persistent and debilitating headaches.
- Depression and anxiety: Common mental health challenges after TBI.
- Sleep disturbances: Difficulty sleeping or staying asleep.
The specific complications experienced depend on the severity and location of the injury. Careful monitoring and management of these complications are essential to improve patient outcomes and quality of life.
Q 15. Explain the role of therapeutic hypothermia in TBI.
Therapeutic hypothermia, or induced hypothermia, is a neuroprotective technique used in the management of severe traumatic brain injury (TBI). It involves lowering the patient’s core body temperature to 32-34°C (89.6-93.2°F) for a specific period, typically 24-72 hours. This controlled cooling slows down the metabolic rate of brain cells, reducing their oxygen demand and limiting the extent of secondary brain injury.
The rationale behind this is that after a TBI, a cascade of damaging events occurs, including inflammation, swelling (cerebral edema), and excitotoxicity (over-stimulation of nerve cells). Hypothermia helps to mitigate these processes. It’s like putting a fire on ice – slowing down the spread and intensity of the damage.
Practical Application: Hypothermia is typically initiated within 6 hours of the injury, after initial stabilization. Continuous monitoring of core temperature, heart rate, blood pressure, and neurological status is crucial. The patient’s temperature is carefully lowered and maintained using cooling blankets, ice packs, or specialized cooling devices. Rewarming is done gradually to prevent complications. However, it’s important to note that therapeutic hypothermia is not suitable for all TBI patients and carries potential risks such as cardiac arrhythmias and infection.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Discuss the challenges in diagnosing and managing mild TBI.
Mild traumatic brain injury (mTBI), often referred to as a concussion, presents significant diagnostic and management challenges. The primary difficulty lies in the subjective nature of symptoms. Unlike severe TBI, where there’s often clear evidence of injury, mTBI symptoms can vary greatly and are often subtle. Patients may experience headaches, dizziness, memory problems, fatigue, or difficulty concentrating – symptoms that are also common in many other conditions.
Challenges in Diagnosis: There are no definitive objective markers for mTBI. Neuroimaging techniques like CT scans or MRIs may be normal, leading to missed or delayed diagnoses. This reliance on subjective reporting makes diagnosis heavily dependent on the patient’s reliability and the clinician’s ability to interpret the symptoms accurately. Different patients experience different symptoms, and there’s no ‘one size fits all’ approach.
Challenges in Management: Treatment for mTBI is primarily supportive and focuses on symptom management. This includes rest, avoiding strenuous activities, gradual return to normal activities, and management of pain and other symptoms. However, patients may experience symptom prolongation and functional impairments, leading to significant difficulties in education, work, and social life. Effective management requires a holistic approach involving medical professionals, therapists (physical, occupational, speech), and support networks.
Q 17. What are the long-term effects of spinal cord injury?
Spinal cord injury (SCI) can lead to devastating long-term effects, profoundly impacting a person’s physical, cognitive, and psychosocial well-being. The extent and type of long-term effects depend on the severity and location of the injury.
Physical Effects: These can include paralysis (paraplegia – lower body; quadriplegia – all four limbs), loss of sensation (numbness, tingling), muscle weakness or spasticity, bowel and bladder dysfunction, chronic pain (neuropathic pain), and increased risk of pressure sores. Mobility and independence are significantly affected, requiring assistive devices and ongoing physical therapy.
Cognitive Effects: Some individuals experience cognitive impairments, such as memory problems, attention deficits, and difficulty with executive functions (planning, organization). These cognitive changes can affect their ability to learn, work, and manage their daily lives.
Psychosocial Effects: SCI can significantly impact mental health, increasing the risk of depression, anxiety, and post-traumatic stress disorder (PTSD). The loss of physical function and independence, alongside social isolation and financial strain, can significantly affect emotional well-being. Specialized psychological support and social services are crucial to address these challenges.
Q 18. Describe the different types of spinal cord injuries.
Spinal cord injuries are classified in several ways, focusing on the mechanism of injury, the level of injury, and the completeness of the injury.
By Mechanism: SCI can result from various mechanisms, including blunt trauma (e.g., car accidents), penetrating trauma (e.g., gunshot wounds), or fractures. The forces involved determine the severity and type of damage.
By Level: Injuries are classified based on the level of the spinal column affected (e.g., cervical, thoracic, lumbar, sacral). The higher the injury, the greater the extent of functional impairment.
By Completeness: Injuries are classified as complete or incomplete based on the degree of neurological function preserved below the level of injury. A complete injury results in total loss of motor and sensory function below the level of injury, while an incomplete injury means some function is preserved.
Examples of Incomplete Injuries: Central cord syndrome, anterior cord syndrome, Brown-Séquard syndrome, and Cauda equina syndrome are all examples of incomplete SCI, each with a unique pattern of preserved and lost function.
Q 19. Explain the use of medications in managing neurotrauma patients.
Medications play a crucial role in managing neurotrauma patients, targeting various aspects of the injury and its consequences.
Pain Management: Analgesics, including opioids and non-opioid medications, are essential for managing pain, a common and debilitating symptom. Careful monitoring and management of opioid use are crucial to avoid complications.
Cerebral Edema Reduction: Mannitol, a hyperosmolar agent, can help reduce cerebral edema (swelling in the brain) by drawing fluid out of the brain tissue. Corticosteroids, such as methylprednisolone, were previously used, but their effectiveness is now debated.
Seizure Prevention: Anticonvulsants, such as phenytoin or levetiracetam, may be administered prophylactically to prevent seizures, which are a significant risk following TBI.
Spasticity Management: In SCI, medications like baclofen or tizanidine can help manage muscle spasticity (increased muscle tone and stiffness).
Other Medications: Other medications may be used to address specific complications, such as infections, autonomic dysreflexia (in SCI), or deep vein thrombosis (blood clots).
Important Note: Medication management is individualized, tailored to the specific patient’s needs and monitored closely for efficacy and side effects.
Q 20. What are the ethical considerations in neurotrauma care?
Neurotrauma care presents several complex ethical considerations, often requiring difficult decisions with significant consequences for the patient and their family.
Decision-Making Capacity: Determining the patient’s capacity to make informed decisions, particularly in cases of severe TBI, can be challenging. Surrogate decision-makers, often family members, may need to be involved, raising questions about their authority and the best interests of the patient.
Resource Allocation: Neurotrauma care is resource-intensive, leading to ethical dilemmas regarding the allocation of scarce resources, especially in cases of multiple patients with varying prognoses. Decisions about prioritizing treatment and resource utilization must be made thoughtfully and equitably.
End-of-Life Care: In situations where recovery is unlikely, ethical discussions regarding end-of-life care, including withdrawing or withholding life-sustaining treatment, become crucial. These decisions must be made in accordance with the patient’s wishes (or surrogate decisions) and involve careful consideration of the patient’s quality of life.
Informed Consent: Obtaining informed consent for all treatments and procedures is essential, but can be challenging in acute settings or when dealing with impaired cognitive capacity. Transparency and clear communication are vital.
Confidentiality: Maintaining patient confidentiality while ensuring effective communication among healthcare providers and family members requires a balance between ethical obligations and practical necessities.
Q 21. Discuss the importance of interdisciplinary collaboration in neurotrauma management.
Interdisciplinary collaboration is paramount in neurotrauma management, given the multifaceted nature of these injuries. Effective care requires the expertise of various healthcare professionals working together seamlessly.
Team Members: A typical neurotrauma team includes neurosurgeons, neurologists, trauma surgeons, intensive care physicians, nurses, physical therapists, occupational therapists, speech-language pathologists, respiratory therapists, dieticians, social workers, and psychologists. Each brings unique skills and knowledge.
Benefits of Collaboration: Working together, the team can develop a comprehensive care plan addressing the patient’s physical, cognitive, and psychosocial needs. This includes optimizing medical management, facilitating rehabilitation, and providing emotional and psychosocial support. Improved communication and shared decision-making within the team leads to better patient outcomes.
Communication and Coordination: Effective communication is the cornerstone of interdisciplinary collaboration. Regular team meetings, shared electronic health records, and clear communication channels ensure that everyone is up-to-date on the patient’s progress and needs. A well-defined leadership structure facilitates efficient coordination and decision-making within the team.
Example: A patient with severe TBI might require the coordinated efforts of a neurosurgeon (to address surgical needs), an intensivist (for critical care), a neurologist (for neurological monitoring), and a physical therapist (for rehabilitation). Effective communication among these professionals is crucial for optimizing patient outcomes.
Q 22. How do you assess the cognitive and emotional impact of neurotrauma?
Assessing the cognitive and emotional impact of neurotrauma requires a multi-faceted approach. We utilize a combination of standardized neuropsychological tests and clinical interviews to comprehensively evaluate the patient.
Cognitive assessment involves tests measuring attention, memory (both short-term and long-term), executive function (planning, problem-solving), language, and visuospatial skills. Examples include the Montreal Cognitive Assessment (MoCA) and the Wechsler Adult Intelligence Scale (WAIS). These tests help quantify the degree of cognitive impairment.
Emotional assessment is equally crucial. We assess for symptoms of depression, anxiety, post-traumatic stress disorder (PTSD), irritability, and emotional lability through clinical interviews, standardized questionnaires like the Patient Health Questionnaire-9 (PHQ-9) for depression and the Generalized Anxiety Disorder 7-item scale (GAD-7) for anxiety, and observation of the patient’s behavior. We also consider the patient’s pre-morbid personality and psychosocial factors to understand the impact of the injury within their individual context.
The results from these assessments inform treatment planning, including therapies like cognitive rehabilitation, psychotherapy, and medication management, tailored to the specific cognitive and emotional deficits.
Q 23. Describe your experience with managing patients with diffuse axonal injury.
Diffuse axonal injury (DAI) is a severe form of traumatic brain injury characterized by widespread damage to axons throughout the brain. Managing DAI patients is incredibly complex and challenging due to the diffuse nature of the injury, making it difficult to pinpoint specific areas for targeted intervention.
My experience involves managing the entire spectrum of care, from initial stabilization in the intensive care unit (ICU), focusing on maintaining cerebral perfusion pressure (CPP) and reducing intracranial pressure (ICP), to long-term rehabilitation. This includes close monitoring for complications like cerebral edema, seizures, and hydrocephalus.
Treatment often involves supportive care, managing secondary injury mechanisms, and facilitating neurorehabilitation. This may include medication for managing symptoms like spasticity and pain, physical therapy to improve motor function, occupational therapy to improve daily living skills, and speech therapy to address communication difficulties. Prognosis is highly variable and depends on the severity of the injury.
A key aspect of management is close collaboration with a multidisciplinary team including neurologists, neurosurgeons, neuropsychologists, physical therapists, occupational therapists, speech therapists, and social workers.
Q 24. What is your experience with advanced life support (ALS) protocols in neurotrauma?
Advanced life support (ALS) protocols in neurotrauma are critical for immediate stabilization and management of life-threatening conditions. My experience includes proficiency in managing the airway, breathing, and circulation (ABCs) in acutely injured patients. This involves securing the airway, often through endotracheal intubation, providing ventilation with mechanical support, and managing hemodynamic instability.
I’m experienced in using advanced monitoring techniques such as intracranial pressure (ICP) monitoring, cerebral perfusion pressure (CPP) monitoring, and brain tissue oxygenation (PbtO2) monitoring to guide treatment and optimize cerebral blood flow. Understanding and applying the principles of hypothermia management in cases of severe traumatic brain injury is also critical.
Furthermore, rapid assessment for signs of herniation and prompt neurosurgical intervention when necessary are critical components of ALS in neurotrauma. The ability to quickly interpret clinical findings, order relevant investigations, and initiate prompt treatment are essential skills in this high-pressure environment. Regular training and participation in simulated scenarios are crucial to maintain proficiency in these life-saving procedures.
Q 25. What are the latest advancements in the treatment of neurotrauma?
The field of neurotrauma treatment is constantly evolving. Recent advancements include:
- Improved neuroimaging techniques: Advanced MRI and CT scans offer better visualization of brain injuries, allowing for more precise diagnosis and treatment planning.
- Therapeutic hypothermia: Controlled cooling of the brain after severe injury can reduce secondary injury and improve outcomes.
- Neuroprotective agents: Ongoing research explores drugs that can protect brain cells from further damage after injury.
- Stem cell therapy: Experimental therapies using stem cells show promise for repairing damaged brain tissue.
- Advanced neurorehabilitation techniques: Virtual reality, robotic-assisted therapy, and other innovative approaches are enhancing rehabilitation outcomes.
- Personalized medicine: Genetic testing and other techniques help tailor treatments to individual patients.
These advancements, while still under development or limited in their widespread application, offer hope for improved outcomes for patients with neurotrauma in the future.
Q 26. Describe a challenging neurotrauma case you managed and the outcome.
One particularly challenging case involved a young motorcyclist who sustained a severe traumatic brain injury with a large epidural hematoma and diffuse axonal injury after a high-speed collision. The patient arrived in the emergency department with decreased level of consciousness and unstable vital signs.
Immediate neurosurgical intervention was required to evacuate the epidural hematoma. Post-surgery, the patient required intensive care management, including ICP monitoring, and aggressive management of cerebral edema. He experienced prolonged periods of unconsciousness, and his recovery was slow and arduous.
The multidisciplinary team worked tirelessly to support his recovery, with intensive physical, occupational, and speech therapies. The patient demonstrated remarkable resilience. Although he sustained significant residual cognitive and physical deficits, he eventually transitioned to a rehabilitation facility and later, to a long-term care facility. He was able to achieve a degree of independence and quality of life that exceeded initial expectations. This case highlighted the importance of aggressive initial management, close monitoring, and comprehensive rehabilitation in optimizing outcomes even in severely injured patients.
Q 27. How do you communicate complex medical information to patients and their families?
Communicating complex medical information to patients and their families requires empathy, patience, and clear, concise language. I avoid medical jargon whenever possible, using simple, relatable terms. I explain diagnoses and treatment plans in a way that is easy to understand, checking for understanding regularly. I use visual aids, such as diagrams and pictures, whenever appropriate.
I also tailor my communication to the individual’s level of understanding and emotional state. I actively listen to their concerns and answer their questions honestly and openly. If information is particularly complex or emotionally challenging, I may break it down into smaller, more manageable pieces across multiple conversations. I always encourage patients and families to ask questions and provide them with written materials to review later. Involving other members of the healthcare team, such as social workers or chaplains, can also be helpful in supporting the patient and family emotionally.
Q 28. How do you manage your workload and stress in a high-pressure environment?
Managing workload and stress in a high-pressure environment like neurotrauma requires a multi-pronged approach. Effective time management is essential. I prioritize tasks, delegate when appropriate, and utilize electronic health records and other technology to improve efficiency. Maintaining a healthy work-life balance is crucial. I ensure I get adequate sleep, exercise regularly, and engage in activities that help me relax and de-stress.
Building strong relationships with my colleagues is also vital. Open communication and teamwork help distribute the workload and provide mutual support. Finally, seeking supervision and utilizing professional resources, such as peer support groups or employee assistance programs, helps in addressing burnout and maintaining mental wellbeing. Regular self-reflection and mindful practices are essential to manage the emotional toll of working in this demanding field.
Key Topics to Learn for Neurotrauma Interview
- Primary and Secondary Injuries: Understanding the immediate and cascading effects of traumatic brain injury (TBI), including mechanisms of injury and the evolving pathophysiology.
- Neuroimaging Techniques: Interpreting CT scans, MRI, and other neuroimaging modalities to assess the extent and location of brain damage. Practical application: Differentiating between various types of hemorrhages and identifying edema.
- Clinical Assessment and Neurological Examination: Mastering the Glasgow Coma Scale (GCS), assessing cranial nerves, and interpreting changes in neurological status. Practical application: Determining prognosis and guiding treatment decisions based on a patient’s clinical presentation.
- Intracranial Pressure (ICP) Management: Understanding the pathophysiology of elevated ICP, and the various medical and surgical interventions employed for its control. Practical application: Analyzing ICP waveforms and interpreting their clinical significance.
- Surgical Interventions: Familiarity with craniotomies, burr holes, and other neurosurgical procedures used in the management of acute neurotrauma. Practical application: Understanding the indications and contraindications for each procedure.
- Medical Management: Understanding the role of medications, including osmotic diuretics and corticosteroids, in the treatment of neurotrauma. Practical application: Knowing the potential benefits and side effects of these medications.
- Rehabilitation and Recovery: Understanding the long-term implications of TBI and the various rehabilitative approaches used to improve functional outcomes. Practical application: Designing a comprehensive rehabilitation plan based on a patient’s specific needs.
- Ethical Considerations: Addressing ethical dilemmas related to end-of-life care and decision-making in patients with severe neurotrauma.
Next Steps
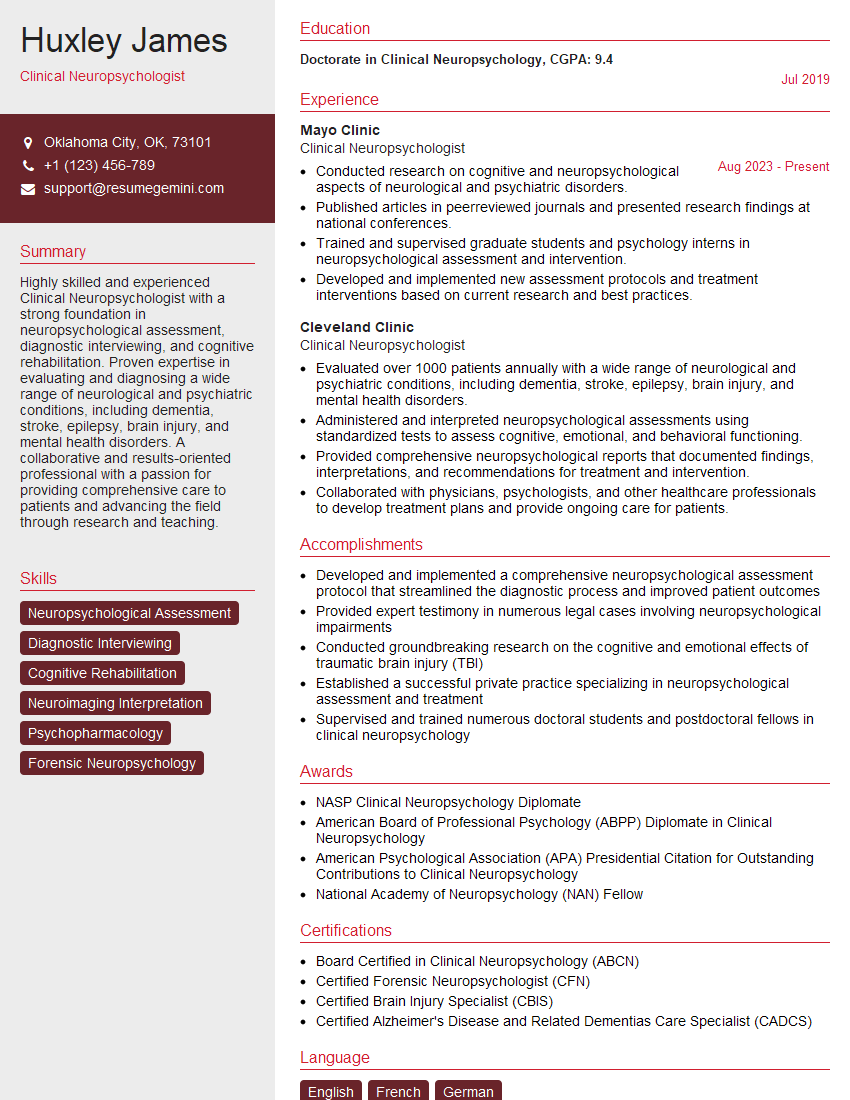
Mastering the complexities of neurotrauma is crucial for a successful and rewarding career in this challenging yet incredibly fulfilling field. It opens doors to specialized roles and positions of leadership within healthcare. To maximize your job prospects, creating a strong, ATS-friendly resume is essential. ResumeGemini offers a powerful tool to help you build a professional resume that showcases your skills and experience effectively. We provide examples of resumes tailored specifically to Neurotrauma professionals to help guide you through the process.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hi, I have something for you and recorded a quick Loom video to show the kind of value I can bring to you.
Even if we don’t work together, I’m confident you’ll take away something valuable and learn a few new ideas.
Here’s the link: https://bit.ly/loom-video-daniel
Would love your thoughts after watching!
– Daniel
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.