The right preparation can turn an interview into an opportunity to showcase your expertise. This guide to Critical Limb Ischemia Treatment interview questions is your ultimate resource, providing key insights and tips to help you ace your responses and stand out as a top candidate.
Questions Asked in Critical Limb Ischemia Treatment Interview
Q 1. Explain the diagnostic criteria for Critical Limb Ischemia (CLI).
Critical Limb Ischemia (CLI) is diagnosed based on a combination of clinical symptoms and objective findings indicating severe peripheral artery disease (PAD). It’s not just about pain; it’s about the limb’s viability being threatened.
The core diagnostic criteria usually include:
- Ischemic rest pain: Persistent pain in the affected limb, even at rest, typically worse at night. This is a crucial indicator as it points to severely reduced blood flow.
- Tissue loss: This can manifest as ulcers or gangrene (tissue death). The presence of these visibly compromised tissues is a hallmark of CLI.
- Objective evidence of arterial disease: This often involves non-invasive testing, like ankle-brachial index (ABI) measurements, which assess the blood pressure difference between the arms and legs. A severely low ABI, typically below 0.4, is strongly suggestive of CLI.
In essence, CLI represents the most severe stage of PAD, where the limb’s blood supply is critically compromised, threatening its survival.
Q 2. Describe the different stages of CLI.
While there isn’t a universally agreed-upon rigid staging system for CLI, we often consider the severity based on the clinical presentation and the extent of tissue loss:
- Stage I: Ischemic rest pain – Pain even at rest, usually relieved by lowering the limb.
- Stage II: Ischemic rest pain with minor tissue loss (ulcers, superficial wounds).
- Stage III: Ischemic rest pain with major tissue loss (extensive ulceration, gangrene).
- Stage IV: Major tissue loss that necessitates amputation to prevent further complications.
These stages guide treatment decisions. Stage I might benefit from medical management, while stages III and IV often require aggressive intervention like revascularization or amputation.
Q 3. What are the common risk factors associated with CLI?
CLI is a complex condition with multiple interwoven risk factors that increase the likelihood of developing it. Many are modifiable, meaning lifestyle changes can mitigate their impact. These include:
- Smoking: A major contributor, causing vascular damage and reducing blood flow.
- Diabetes: Damages blood vessels and increases the risk of atherosclerosis (hardening of the arteries).
- Hypertension: High blood pressure puts extra strain on arteries, accelerating atherosclerosis.
- Hyperlipidemia: High cholesterol levels contribute to plaque buildup in arteries, narrowing them.
- Obesity: Associated with increased risk of diabetes and hypertension.
- Family history: A strong family history of PAD significantly increases risk.
- Age: The prevalence of CLI significantly increases with age.
It’s crucial to address these risk factors through lifestyle modifications and medical management to prevent or delay the onset of CLI.
Q 4. Outline the non-invasive diagnostic techniques used in CLI.
Several non-invasive techniques are used to diagnose CLI and assess the severity of the disease. These are crucial as they are less invasive than angiography:
- Ankle-Brachial Index (ABI): This is the most common test. It compares the blood pressure in the ankle to the blood pressure in the arm. A low ABI (typically <0.4) indicates reduced blood flow to the leg.
- Toe-Brachial Index (TBI): Similar to ABI, but measures pressure in the toes. It’s often helpful in patients with calcified arteries where ABI may be inaccurate.
- Segmental Doppler Pressure: Measures blood pressure at different points in the leg to identify the location of blockages.
- Transcutaneous Oxygen Pressure (TcPO2): Measures oxygen levels in the skin. Low levels suggest inadequate blood supply.
These tests provide valuable information about the extent of arterial blockage and guide treatment planning.
Q 5. Discuss the role of angiography in CLI diagnosis and management.
Angiography plays a crucial role in both diagnosing and managing CLI. It’s an invasive procedure where a contrast dye is injected into the arteries to visualize them using X-rays.
In diagnosis: Angiography provides detailed images of the arteries, precisely identifying the location, extent, and severity of blockages. This is crucial for determining the best treatment strategy.
In management: During the same procedure, revascularization techniques like angioplasty or stenting can often be performed. This means that after visualizing the blockages, the doctor can immediately address them. Angiography also helps assess the success of these interventions.
It’s essential to remember angiography carries risks, so it’s usually reserved for cases where non-invasive methods are inconclusive or when intervention is anticipated.
Q 6. Compare and contrast different revascularization techniques for CLI.
Several revascularization techniques exist for CLI, each with its advantages and disadvantages. The choice depends on factors like the location and extent of the blockage, patient’s overall health, and the presence of comorbidities:
- Percutaneous Transluminal Angioplasty (PTA): A catheter with an inflatable balloon is used to compress plaque against the arterial wall, widening the vessel. It’s less invasive than surgery but may not be suitable for severely diseased arteries.
- Stenting: A metal mesh tube (stent) is placed in the artery to keep it open after angioplasty. Stents prevent restenosis (re-narrowing of the artery).
- Bypass surgery: A healthy blood vessel (from another part of the body) is grafted to bypass the blocked artery. It’s more invasive but is a better option for long, extensive blockages that aren’t suitable for PTA/stenting.
Bypass surgery is a more extensive procedure compared to PTA and stenting, requiring a longer recovery period, while PTA and stenting are minimally invasive options often performed under local anesthesia and have faster recovery times. The decision about which approach is best is a collaborative one between the patient and vascular surgeon.
Q 7. Describe the procedure for angioplasty in CLI.
Angioplasty for CLI involves inserting a catheter (a thin, flexible tube) into an artery, usually in the groin or arm, and guiding it to the affected area of the leg. A balloon at the tip of the catheter is then inflated to compress the plaque against the arterial wall, widening the vessel and restoring blood flow.
Step-by-step procedure:
- Access: A small incision is made in the artery, and the catheter is inserted.
- Catheter Navigation: The catheter is carefully guided through the arteries using fluoroscopy (real-time X-ray imaging) to reach the blockage.
- Balloon Inflation: The balloon is inflated several times, compressing the plaque against the arterial wall.
- Balloon Deflation & Catheter Removal: The balloon is deflated, and the catheter is withdrawn.
- Closure: The access site is closed using pressure or sutures.
Post-procedure, patients are monitored for complications such as bleeding, hematoma formation, or restenosis. Sometimes a stent is placed after angioplasty to maintain the artery’s patency.
Q 8. Explain the use of stents in CLI treatment.
Stents are tiny, expandable mesh tubes used to widen narrowed or blocked arteries in patients with Critical Limb Ischemia (CLI). Think of them as scaffolding for your blood vessels. They’re deployed during a procedure called angioplasty, where a catheter with a balloon is guided to the blockage. The balloon inflates, compressing the plaque against the artery wall, and the stent is then placed to keep the artery open. This improves blood flow to the ischemic limb, relieving pain and potentially preventing amputation.
For example, a patient with severe leg pain due to a blockage in their femoral artery might undergo an angioplasty with stent placement. The stent acts as a permanent support, preventing the artery from closing again. Different types of stents exist, including bare metal stents and drug-eluting stents (DES), which release medication to inhibit further narrowing.
Q 9. Discuss the role of bypass surgery in CLI.
Bypass surgery is a more invasive procedure used to treat CLI when stenting is not feasible or has failed. It involves creating a new pathway for blood to flow around the blocked artery. Imagine building a detour around a traffic jam. A healthy blood vessel, usually from the leg or chest, is grafted onto the artery above and below the blockage, diverting blood flow and restoring perfusion to the limb. This is often necessary for long, extensive blockages.
For instance, a patient with multiple severely narrowed arteries in their leg might benefit from a bypass procedure. The surgeon would carefully select a suitable vessel, prepare it, and then meticulously connect it to create a new bypass. The type of bypass surgery will depend on the location and extent of the disease, with different options including femoropopliteal or femorotibial bypasses.
Q 10. What are the indications for amputation in CLI?
Amputation is a last resort in CLI treatment, considered only when all other options have been exhausted and the limb is at significant risk of necrosis (tissue death) or severe infection that cannot be controlled. The decision is complex and involves careful consideration of the patient’s overall health, the severity of the ischemia, the presence of infection, and the patient’s quality of life. Factors such as the extent of gangrene, intractable pain, and lack of response to other interventions guide this difficult decision. We strive to avoid amputation whenever possible, but patient safety and well-being are paramount.
An example would be a patient with extensive gangrene affecting the majority of their foot, despite aggressive medical and interventional management. In such cases, amputation might be the only option to prevent life-threatening sepsis. The goal is always to preserve as much of the limb as possible while ensuring the patient’s survival and comfort.
Q 11. How do you manage pain in patients with CLI?
Pain management in CLI patients is crucial for improving their quality of life and promoting healing. It’s a multifaceted approach, often involving a combination of strategies. We start with analgesics, which can range from over-the-counter medications like acetaminophen to stronger opioid medications if necessary. Nerve blocks might be used to target specific areas of pain, and in some cases, surgical procedures like sympathectomy may be considered to reduce pain caused by nerve damage.
For example, a patient might start with oral pain medications, gradually increasing the dosage as needed. If their pain isn’t adequately controlled, a nerve block might be performed to provide short-term pain relief. In certain circumstances, continuous infusion of analgesics might be required. The goal is to find the optimal balance between pain relief and minimizing side effects.
Q 12. Explain the importance of wound care in CLI.
Wound care is an integral part of CLI management, as these patients often have non-healing ulcers. Proper wound care can prevent infection, promote healing, and reduce the risk of amputation. It involves regular wound cleaning and debridement (removal of dead tissue) to create a healthy wound bed. Appropriate dressings are applied to keep the wound moist and protected, and the patient’s overall hygiene and nutrition are optimized. Advanced techniques such as negative pressure wound therapy might also be employed to improve healing.
For example, a patient with a foot ulcer might receive daily wound cleaning with saline solution, followed by the application of a specialized dressing. Debridement may be necessary to remove necrotic tissue. Regular monitoring of the wound and prompt treatment of any signs of infection are critical. Proper wound care significantly impacts the likelihood of healing and reduces the risk of complications.
Q 13. What are the common complications associated with CLI treatment?
CLI treatment is associated with several potential complications. These can include bleeding at the puncture site, infection at the surgical site or wound, thrombosis (blood clot formation) in the treated artery, restenosis (re-narrowing of the artery), and amputation. Furthermore, patients can experience issues related to anesthesia, such as allergic reactions or respiratory depression. Careful patient selection, meticulous surgical technique, and aggressive post-operative management help minimize these risks.
For instance, a patient might develop a hematoma (blood collection) at the catheter insertion site after angioplasty. Or, a patient undergoing bypass surgery may experience a surgical site infection, requiring antibiotic treatment and potentially additional surgery. Continuous monitoring and prompt intervention are critical in managing these complications.
Q 14. How do you manage post-operative complications after CLI surgery?
Post-operative management after CLI surgery focuses on preventing and managing complications. This involves careful monitoring of vital signs, pain management, wound care, and assessment for signs of infection. Early mobilization is encouraged to prevent complications such as deep vein thrombosis (DVT). Regular assessment of blood flow in the treated limb is essential, and any signs of restenosis or thrombosis are addressed promptly. Patients might require anticoagulation therapy to prevent blood clots, and regular follow-up appointments are crucial for long-term monitoring.
For example, a patient after bypass surgery would receive regular assessments for signs of infection, such as fever, redness, swelling, or increased pain. They may be on anticoagulation therapy to prevent DVT and given rehabilitation to improve mobility. Regular Doppler ultrasound scans might be performed to assess blood flow and detect any issues. Close collaboration between the surgical team, nurses, and rehabilitation specialists is crucial for optimal patient outcomes.
Q 15. What is the role of thrombolytic therapy in CLI?
Thrombolytic therapy, also known as clot-busting therapy, plays a crucial role in treating Critical Limb Ischemia (CLI) by dissolving blood clots that are blocking blood flow to the limbs. It’s primarily used in acute situations where there’s a sudden blockage causing severe pain and tissue damage, often before more definitive procedures can be performed. The most common thrombolytic agents used are tissue plasminogen activator (tPA) and urokinase.
However, thrombolytic therapy is not without risks. It can cause bleeding complications, and it’s not always effective in dissolving all the clots. We carefully consider the patient’s overall health, the location and extent of the blockage, and the potential risks and benefits before recommending this treatment. For instance, we might prioritize thrombolytics for a patient experiencing acute limb ischemia with rapidly worsening symptoms, but we might opt for a different approach for someone with more chronic, stable CLI.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Describe your approach to patient selection for different CLI treatment modalities.
Patient selection for CLI treatment is a complex process that involves a careful assessment of several factors. We consider the patient’s overall health, the severity of their CLI (using the Rutherford classification, which I’ll explain later), the location and extent of the blockage, the presence of comorbidities like diabetes or kidney disease, and the patient’s preferences.
- Superficial Femoral Artery (SFA) Disease: For patients with SFA disease and good overall health, we might consider minimally invasive techniques like angioplasty or stenting.
- Below-the-knee (BTK) Disease: BTK disease often presents a greater challenge. If the vessels are unsuitable for angioplasty, we might explore bypass surgery using autologous veins or synthetic grafts.
- Severe CLI with Tissue Loss: Patients with critical limb ischemia and extensive tissue loss might require amputation as a last resort to prevent life-threatening infection. We aim to explore all other options first, though.
- Multi-vessel disease: Patients with extensive disease requiring multiple interventions might benefit from staged procedures to minimize risk.
Each case is unique and requires a personalized treatment strategy, developed in close collaboration with the patient.
Q 17. How do you assess the effectiveness of CLI treatment?
Assessing the effectiveness of CLI treatment involves a multi-faceted approach. We monitor several key indicators:
- Clinical Improvement: We look for a reduction in pain, improved wound healing, and an increase in walking distance.
- Ankle-Brachial Index (ABI): ABI measures the blood pressure in the ankle compared to the arm. A higher ABI after treatment shows improved blood flow.
- Angiography: Follow-up angiography allows us to visually assess the patency (openness) of the treated vessels.
- Wound Healing: We meticulously monitor wound healing progress, noting any signs of infection or delayed healing.
- Patient-reported Outcomes: We also consider the patient’s self-reported improvement in quality of life, including pain levels and functional capacity.
Combining these assessments provides a comprehensive picture of treatment success.
Q 18. What are the long-term management strategies for CLI patients?
Long-term management of CLI is crucial to prevent recurrence and maintain quality of life. This includes:
- Medication Management: Continued use of antiplatelet agents (like aspirin or clopidogrel) to prevent blood clot formation is vital. We also manage any underlying conditions like diabetes and hypertension.
- Lifestyle Modifications: Smoking cessation, regular exercise, and a healthy diet are essential.
- Regular Follow-up: Routine check-ups allow us to monitor for any signs of disease progression or complications.
- Wound Care: Patients often require ongoing wound care to promote healing.
- Revascularization Surveillance: Periodic assessments may be required to detect any recurrence of arterial occlusion and guide further reintervention.
A proactive, multidisciplinary approach ensures the best possible long-term outcomes.
Q 19. Discuss the role of lifestyle modifications in CLI prevention and management.
Lifestyle modifications are paramount in both the prevention and management of CLI. These changes address the underlying risk factors that contribute to peripheral artery disease (PAD), the precursor to CLI.
- Smoking Cessation: Smoking significantly damages blood vessels, accelerating the progression of PAD. Quitting smoking is the single most important step.
- Regular Exercise: Regular, moderate-intensity exercise helps improve circulation and strengthens leg muscles.
- Healthy Diet: A balanced diet low in saturated fats, cholesterol, and sodium helps maintain healthy blood pressure and cholesterol levels.
- Weight Management: Maintaining a healthy weight reduces strain on the cardiovascular system.
- Blood Sugar Control: For patients with diabetes, strict blood sugar control is essential to prevent further vascular damage.
We work closely with patients to develop personalized lifestyle plans tailored to their individual needs and circumstances.
Q 20. Explain your understanding of the Rutherford classification system for CLI.
The Rutherford classification system is a widely used staging system for CLI that categorizes the severity of the disease based on clinical presentation and the presence of tissue loss. It ranges from category 0 (asymptomatic) to category 6 (major amputation or death). The higher the category, the more severe the CLI. For instance, category 4 indicates rest pain and minor tissue loss, while category 6 represents the most serious outcomes. This system helps clinicians standardize the assessment of CLI and guide treatment decisions. It helps us communicate effectively and plan for appropriate care.
Q 21. Describe the use of pharmacological agents in CLI treatment.
Pharmacological agents play a significant role in CLI management, both for symptom relief and disease modification.
- Antiplatelet Agents: Aspirin and clopidogrel are crucial to prevent blood clot formation and reduce the risk of re-occlusion after revascularization procedures.
- Statins: Statins lower cholesterol levels, improving overall cardiovascular health and potentially slowing the progression of PAD.
- Cilostazol: Cilostazol is a phosphodiesterase inhibitor that improves blood flow and reduces claudication symptoms.
- Pentoxifylline: Pentoxifylline improves blood rheology (the flow properties of blood) and reduces symptoms.
- Pain Management: Analgesics, such as opioids (used cautiously), NSAIDs, and other pain-relieving medications are essential for managing rest pain.
The choice of pharmacological agents depends on the individual patient’s condition, comorbidities, and response to treatment. We carefully monitor patients for side effects and adjust medication as needed.
Q 22. What are the current guidelines for CLI management?
Current guidelines for Critical Limb Ischemia (CLI) management are complex and evolve with ongoing research. They emphasize a multidisciplinary approach, focusing on risk factor modification, revascularization (restoring blood flow), and wound care. The cornerstone is accurate diagnosis using ankle-brachial index (ABI), toe-brachial index (TBI), and imaging studies like angiography. Treatment decisions are stratified based on the severity of ischemia, location of disease, and patient-specific factors such as comorbidities.
Conservative Management: For mild CLI, this initially involves aggressive risk factor modification (smoking cessation, diabetes control, blood pressure management), pain management, and wound care.
Revascularization: For more advanced CLI, the aim is to restore blood flow. Options include:
- Percutaneous transluminal angioplasty (PTA): A minimally invasive procedure using a balloon catheter to open blocked arteries.
- Stenting: Placing a small mesh tube in the artery to keep it open.
- Surgical revascularization: Includes bypass surgery (creating a new pathway for blood flow) or amputation (in severe cases when revascularization is not feasible).
Wound Care: Proper wound care is crucial to prevent infection and promote healing. This includes debridement (removal of dead tissue), appropriate dressings, and infection control.
These guidelines are constantly updated by organizations like the Society for Vascular Surgery (SVS) and the American Heart Association (AHA), emphasizing a tailored approach for each patient’s specific clinical picture.
Q 23. How do you counsel patients about the risks and benefits of CLI treatment options?
Counseling patients about CLI treatment is crucial. I begin by explaining the disease in clear, simple terms, emphasizing the severity of the condition and the potential consequences of inaction, such as amputation. I thoroughly discuss each treatment option, outlining the risks and benefits of each procedure in detail, using analogies to make complex information more accessible.
For instance, when explaining angioplasty, I liken the balloon catheter to a plumber’s snake clearing a clogged pipe. For bypass surgery, I might explain it as creating a new road around a blocked highway to restore blood flow. I make sure patients understand the potential complications, including bleeding, infection, and the need for post-procedure rehabilitation.
It’s a collaborative process; I encourage patients to ask questions, address concerns, and actively participate in making informed decisions that align with their values and preferences. Shared decision-making is paramount. I provide them with written materials to reinforce what we’ve discussed and always emphasize the importance of following the post-treatment care plan.
Q 24. Describe a challenging CLI case you have managed and how you approached it.
One particularly challenging case involved a 78-year-old patient with severe CLI in both legs, multiple comorbidities (diabetes, heart failure, chronic kidney disease), and extensive foot ulcers. Revascularization posed significant risks given his overall health status. A purely surgical approach was high-risk due to his comorbidities. A conservative approach alone was unlikely to save his limbs.
My approach involved a multidisciplinary team consisting of vascular surgeons, wound care specialists, endocrinologists, and nephrologists. We implemented a phased approach: initial aggressive wound care and diabetic control to optimize his overall health, followed by a less invasive approach to revascularization. We opted for a staged PTA and stenting procedure on one leg, followed by a close observation and assessment of response. This approach minimized surgical risk while aiming for limb salvage. While complete limb salvage wasn’t achieved in both legs, the staged approach significantly improved his wound healing and pain control, delaying the need for amputation until the end stage.
Q 25. How do you stay updated on the latest advancements in CLI treatment?
Staying updated in the rapidly evolving field of CLI treatment involves a multi-pronged approach. I regularly attend national and international vascular surgery conferences, where I engage in discussions with leading experts and learn about new techniques and technologies.
Professional Journals: I subscribe to and actively read peer-reviewed journals such as J Vasc Surg, Circulation, and others, focusing on articles about CLI diagnosis, management, and new devices.
Online Resources: I utilize reputable online platforms like the websites of the SVS and AHA for guidelines and updates.
Continuing Medical Education (CME): I participate regularly in CME courses and webinars, specifically tailored to the treatment of CLI and related vascular diseases.
Collaboration: Regular discussions with colleagues and participation in case conferences are crucial for sharing knowledge and learning from others’ experiences.
Q 26. What is your experience with specific CLI treatment devices?
My experience encompasses a wide range of CLI treatment devices. I am proficient with various angioplasty balloons (e.g., scoring balloons, drug-eluting balloons), stents (bare-metal stents, drug-eluting stents), and imaging modalities (intravascular ultrasound, optical coherence tomography) used to guide and assess the success of these procedures.
I have hands-on experience with various surgical devices used in bypass procedures, including different types of grafts (synthetic, autologous vein) and surgical instruments. My familiarity extends to wound care technologies, including advanced dressings and negative pressure wound therapy (NPWT) systems. The choice of device is always tailored to the patient’s individual needs and the specific characteristics of the CLI presentation.
Q 27. How do you collaborate with other healthcare professionals in managing CLI patients?
Collaboration is pivotal in CLI management. I work closely with a multidisciplinary team including:
Vascular Surgeons: For surgical interventions and complex cases requiring open surgical procedures.
Interventional Radiologists: For minimally invasive techniques like angioplasty and stenting.
Wound Care Specialists: To manage and treat ulcers and prevent infections.
Endocrinologists & Diabetologists: For optimal management of underlying conditions like diabetes.
Nephrologists: For patients with kidney disease.
Podiatrists: To assess foot health and manage foot ulcers.
Physical Therapists: To help patients regain mobility and improve their functional capacity following treatment.
Regular case conferences, shared patient charts, and clear communication are essential for successful outcomes.
Q 28. What are your salary expectations for this position?
My salary expectations are commensurate with my experience, qualifications, and the responsibilities of this position. I am confident that my expertise and contributions will significantly benefit your organization. I am open to discussing specific compensation details further.
Key Topics to Learn for Critical Limb Ischemia Treatment Interview
- Pathophysiology of Critical Limb Ischemia (CLI): Understand the underlying mechanisms of CLI, including the role of atherosclerosis, thrombosis, and ischemia-reperfusion injury.
- Clinical Presentation and Diagnosis: Master the ability to recognize the clinical signs and symptoms of CLI, and be familiar with diagnostic tools such as ankle-brachial index (ABI), Doppler ultrasound, and angiography.
- Medical Management of CLI: Discuss the role of medication in CLI treatment, including antiplatelet agents, statins, and pain management strategies.
- Revascularization Techniques: Detail various revascularization procedures, including percutaneous transluminal angioplasty (PTA), stenting, and surgical bypass, outlining their indications and limitations.
- Wound Care and Management: Explain the importance of proper wound care in CLI patients, encompassing debridement, infection control, and the use of advanced wound therapies.
- Risk Factor Modification: Discuss strategies for managing and mitigating risk factors such as smoking, diabetes, hypertension, and hyperlipidemia to prevent CLI progression.
- Patient Selection and Treatment Planning: Demonstrate an understanding of the factors that influence treatment decisions and the ability to create individualized treatment plans.
- Post-Treatment Monitoring and Follow-up: Explain the importance of post-procedure monitoring, including surveillance for complications such as restenosis and infection.
- Emerging Therapies and Research: Stay updated on the latest advancements in CLI treatment, including novel pharmacological and interventional strategies.
- Ethical Considerations and Shared Decision-Making: Discuss the importance of patient autonomy and shared decision-making in the context of CLI treatment, considering the potential risks and benefits of various options.
Next Steps
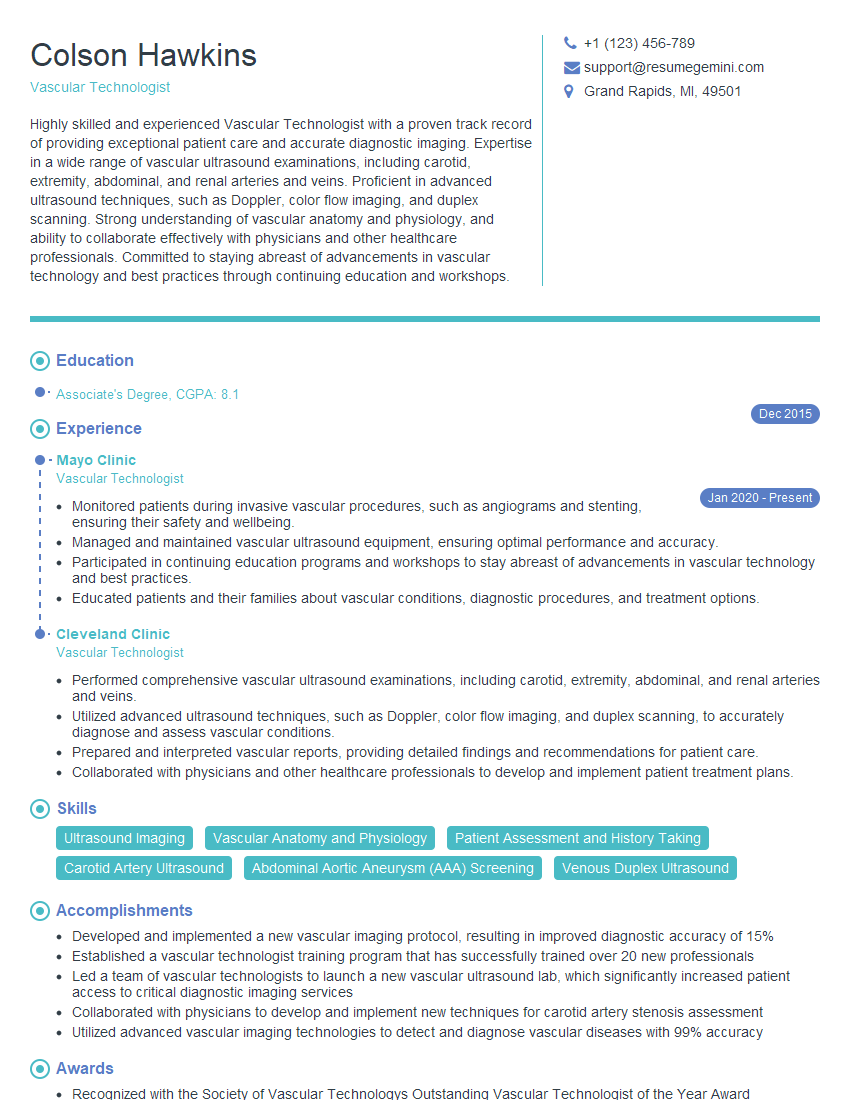
Mastering Critical Limb Ischemia Treatment significantly enhances your career prospects in vascular surgery, interventional radiology, or related fields. A strong understanding of this complex area demonstrates expertise and commitment to patient care. To maximize your job search success, create an ATS-friendly resume that effectively showcases your skills and experience. ResumeGemini is a trusted resource that can help you build a professional and impactful resume. We provide examples of resumes tailored to Critical Limb Ischemia Treatment to guide you in crafting a compelling application that stands out from the competition.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.