Every successful interview starts with knowing what to expect. In this blog, we’ll take you through the top Botanical Medicine interview questions, breaking them down with expert tips to help you deliver impactful answers. Step into your next interview fully prepared and ready to succeed.
Questions Asked in Botanical Medicine Interview
Q 1. Define the term ‘phytochemistry’ and its relevance to botanical medicine.
Phytochemistry is the study of phytochemicals, which are chemicals produced by plants. It’s the cornerstone of botanical medicine because it identifies and analyzes the bioactive compounds within plants responsible for their therapeutic effects. Understanding phytochemistry allows us to determine which plant parts contain the most active compounds, the optimal methods for extraction, and the potential benefits and risks associated with using a particular plant. For example, phytochemical analysis of St. John’s Wort reveals the presence of hyperforin and hypericin, compounds believed to be responsible for its antidepressant properties. This knowledge guides the development of standardized extracts and ensures consistent quality and efficacy in medicinal preparations.
Q 2. Explain the difference between a tincture and a decoction.
Both tinctures and decoctions are liquid herbal extracts, but they differ in their preparation methods and resulting characteristics. A tincture is an alcoholic extract, typically made by soaking the plant material (herb, root, bark) in a high-percentage alcohol solution for several weeks. This method effectively extracts a wide range of both water-soluble and alcohol-soluble compounds. Think of it as gently coaxing the plant’s goodness into the alcohol. Tinctures are generally shelf-stable and have a longer shelf life than decoctions due to the alcohol’s preservative properties.
A decoction, on the other hand, involves simmering the plant material in water for an extended period. This method is best suited for extracting compounds from tougher plant parts like roots and bark, where boiling is needed to break down cell walls and release the active constituents. Decoctions are generally less shelf-stable than tinctures and require refrigeration after preparation. For instance, a decoction of ginger root is commonly used to relieve nausea due to the extraction of gingerol compounds, while a tincture of valerian root might be used as a sleep aid, making use of its alcohol-soluble components.
Q 3. Describe the process of preparing a standard herbal infusion.
Preparing a standard herbal infusion is a simple yet crucial process. The method is also known as a tea. It primarily involves steeping dried or fresh herbs in hot (not boiling) water. Here’s a step-by-step process:
- Measure: Start by measuring the desired amount of herb. A typical ratio is 1-2 teaspoons of dried herb per cup (8 ounces) of water. For fresh herbs, you might use a larger quantity.
- Heat the water: Heat the water to just below boiling point (around 190-212°F or 90-100°C). Boiling water can degrade some delicate compounds.
- Steep: Pour the hot water over the herb in a cup or teapot. Cover the container to prevent the volatile compounds from escaping.
- Infuse: Let the mixture steep for the recommended time, usually 5-15 minutes depending on the herb. Longer steeping times generally result in a stronger infusion, but excessive steeping can lead to bitterness.
- Strain: Once steeped, strain the infusion through a fine-mesh strainer or cheesecloth to remove the plant material.
- Serve: Serve the infusion warm or cool, as preferred.
For example, a chamomile infusion is known for its calming properties, while a peppermint infusion can aid digestion. The key is to use appropriate steeping time and quantity of herbs depending upon the desired strength and therapeutic effect.
Q 4. What are the key considerations when selecting herbs for a specific health concern?
Selecting herbs for a specific health concern requires careful consideration of several factors:
- Therapeutic properties: Research the herb’s known actions and indications. For example, echinacea is known for its immune-supporting properties, while milk thistle supports liver health. The selection should be based on scientific evidence and traditional usage.
- Patient’s health history: Assess the patient’s overall health, including any pre-existing conditions, allergies, or medications they are currently taking. Some herbs may interact negatively with certain medications or exacerbate health issues.
- Herb-drug interactions: Consider the potential interactions between the chosen herbs and any conventional pharmaceuticals the patient is using. This is crucial to avoid adverse effects.
- Safety and quality: Ensure the selected herbs are from a reputable source and are of high quality and purity. Avoid herbs that are contaminated with pesticides or heavy metals.
- Dosage and preparation: Determine the appropriate dosage and preparation method based on scientific evidence or established traditional practices.
Always remember that a thorough understanding of the herbs’ properties and the patient’s individual circumstances are vital for safe and effective herbal therapy. It’s often advisable to consult with a qualified herbalist or healthcare professional before incorporating herbs into a treatment plan, especially when dealing with complex health conditions.
Q 5. How do you assess the quality and purity of herbal products?
Assessing the quality and purity of herbal products is paramount for ensuring safety and efficacy. Here are some key considerations:
- Source and reputation: Choose products from reputable suppliers committed to quality control. Look for companies that provide certificates of analysis (COAs) demonstrating the product’s identity, purity, and potency.
- Botanical identification: Verify the botanical identity of the herb to ensure it’s the correct species and that there is no adulteration or substitution with other plants.
- Heavy metal and pesticide testing: Look for products tested for the absence of heavy metals and pesticides, common contaminants.
- Microbial testing: Check for evidence that the product has undergone microbial testing to ensure it’s free from harmful bacteria and fungi.
- Packaging and storage: Ensure proper packaging to protect the product from light, air, and moisture, maintaining its quality and potency. Look for airtight containers and appropriate storage instructions.
A reliable supplier will readily provide information about their sourcing, testing methods, and quality control procedures. If a company is hesitant to share this information, it might be a red flag.
Q 6. Discuss the potential interactions between botanical medicine and conventional pharmaceuticals.
Botanical medicine and conventional pharmaceuticals can interact in several ways, some beneficial and some potentially harmful. Interactions can occur due to shared metabolic pathways, enzyme inhibition or induction, or direct chemical interactions. For instance, St. John’s Wort, used for mild to moderate depression, is a potent inducer of the CYP3A4 enzyme, leading to decreased blood levels of many medications metabolized by this enzyme, potentially reducing their effectiveness. Conversely, grapefruit juice also interacts with many drugs due to inhibiting CYP3A4. Similarly, some herbs such as ginkgo biloba and ginseng can increase the risk of bleeding when combined with blood-thinning medications. It’s crucial to have open communication with healthcare providers about all medications and supplements being taken to minimize the potential risks of adverse interactions. A qualified healthcare professional can help assess potential interactions and adjust treatment plans accordingly.
Q 7. Explain the concept of synergy in herbal combinations.
Synergy in herbal combinations refers to the phenomenon where the combined effect of two or more herbs is greater than the sum of their individual effects. This means that herbs work better together than they do alone. For example, the combination of chamomile and lavender is often used for promoting relaxation and sleep; each herb contributes to this effect but together, they might exhibit a more potent calming effect than either herb alone. This synergistic effect can be due to several mechanisms, including potentiation (one herb enhancing the effect of another), additive effects (herbs with similar actions strengthening each other), or complementary effects (herbs with different actions working together to address multiple aspects of a health concern). Understanding synergy allows herbalists to create effective and tailored formulations that optimize therapeutic outcomes and minimize potential side effects. However, it’s crucial to note that not all herb combinations are synergistic, and some may even be antagonistic (counteracting each other).
Q 8. What are the common contraindications associated with St. John’s Wort?
St. John’s Wort (Hypericum perforatum) is a popular herbal remedy, but it’s crucial to be aware of its potential interactions. The primary contraindication stems from its potent enzyme-inducing properties. Specifically, St. John’s Wort significantly induces the cytochrome P450 3A4 (CYP3A4) enzyme system in the liver. This enzyme is responsible for metabolizing a vast array of medications.
Drug Interactions: Because St. John’s Wort boosts CYP3A4 activity, it can accelerate the breakdown of many drugs, reducing their effectiveness. This is particularly important for medications with a narrow therapeutic index, meaning a small difference between the effective dose and a toxic dose. Examples include some antidepressants (SSRIs, SNRIs), anticoagulants (warfarin), immunosuppressants (cyclosporine), birth control pills, and HIV medications. The decreased efficacy can lead to treatment failure or increased risk of adverse effects.
Photosensitivity: Some individuals taking St. John’s Wort experience increased sensitivity to sunlight. This can manifest as sunburn, even with minimal sun exposure. It’s advisable to use sunscreen and limit sun exposure while using this herb.
Other Interactions: While less common, interactions with other herbal remedies are possible. It’s always best to disclose all herbal and conventional medications to a healthcare provider before starting St. John’s Wort.
In summary, the main contraindication is the significant risk of drug interactions due to its CYP3A4 enzyme induction. This highlights the critical need for careful assessment of a patient’s medication history before recommending St. John’s Wort.
Q 9. Describe the therapeutic uses of chamomile and its potential side effects.
Chamomile (Matricaria chamomilla and Anthemis nobilis) is a widely used herbal remedy known for its calming and anti-inflammatory properties. Its therapeutic uses are numerous:
Anxiety and Insomnia: Chamomile’s calming effects are attributed to its apigenin content, which interacts with GABA receptors in the brain, promoting relaxation and sleep.
Inflammatory Conditions: Its anti-inflammatory action can help soothe irritated skin (e.g., eczema, diaper rash) and digestive issues (e.g., gastritis, irritable bowel syndrome).
Wound Healing: Chamomile has demonstrated some antimicrobial and wound-healing properties.
While generally safe, potential side effects are relatively mild but can include:
Allergic Reactions: Individuals with ragweed allergies may experience cross-reactivity, exhibiting symptoms like skin rash or itching. A patch test is recommended before widespread topical application.
Digestive Upset: Although chamomile is often used for digestive issues, excessive consumption can, in some cases, cause nausea or diarrhea.
Drug Interactions: While less frequent than with St. John’s Wort, potential interactions with anticoagulants are possible due to chamomile’s antiplatelet effects. Always consult with a healthcare professional if you are on medication.
In clinical practice, chamomile is often a safe and effective option for mild anxiety, insomnia, and inflammatory skin conditions. However, careful consideration of potential allergic reactions and interactions should be taken before recommending it to patients.
Q 10. How do you approach a patient who wants to use botanical medicine alongside their existing medical treatments?
Approaching a patient who wants to use botanical medicine alongside conventional treatments requires a sensitive and thorough approach. The cornerstone of this approach is open communication and collaboration.
Thorough History: Begin by obtaining a complete medical history, including all current medications, supplements, allergies, and pre-existing conditions. This allows for identification of potential drug interactions or contraindications.
Understanding Patient Goals: Engage in a conversation with the patient to understand their motivations for using botanical medicine. Are they looking for complementary support for their existing condition, or are they aiming for alternative treatments? Clarifying their goals is vital.
Risk Assessment: Evaluate the potential risks and benefits of incorporating botanical medicine into their treatment plan. Consider the evidence-based efficacy of the chosen herb and the potential for drug interactions.
Shared Decision-Making: Involve the patient in the decision-making process. Explain the evidence, risks, and potential benefits clearly, allowing the patient to make an informed choice. This empowers the patient and establishes trust.
Monitoring: Closely monitor the patient’s response to the combined treatments. Regular check-ups, including symptom assessment and lab tests where appropriate, are essential.
Communication with Other Healthcare Providers: If the patient is under the care of other healthcare professionals, such as a physician or specialist, clear communication about the botanical medicine use is crucial to ensure coordinated and safe care.
For example, a patient with mild anxiety might wish to use chamomile alongside their prescribed antidepressant. A careful assessment would involve checking for potential interactions and ensuring the chamomile doesn’t interfere with the antidepressant’s efficacy. This requires a collaborative approach involving both the patient and their conventional healthcare provider.
Q 11. Discuss the importance of accurate botanical identification in herbal medicine.
Accurate botanical identification is paramount in herbal medicine; it’s the very foundation of safe and effective practice. Mistakes in identification can have serious consequences, ranging from ineffectiveness to toxicity.
Species Variation: Different plant species, even within the same genus, can have vastly different chemical compositions and therapeutic properties. Misidentifying a plant could lead to using an ineffective or even harmful species.
Toxicity: Many plants contain toxic compounds. Misidentification can result in accidental ingestion of poisonous plants, leading to serious health problems or death. For instance, mistaking poison hemlock for wild carrot or other edible plants can be fatal.
Efficacy: The active compounds responsible for the therapeutic effects are often present in specific parts of the plant (roots, leaves, flowers, etc.) and vary in concentration. Proper identification ensures that the correct plant part is used at the right time of year for optimal efficacy.
To ensure accuracy, herbalists should utilize several identification methods. These include:
Visual Identification: Careful examination of morphological characteristics such as leaf shape, flower structure, stem characteristics, and overall plant habit is crucial.
Microscopic Examination: Microscopic analysis of plant tissues can reveal specific cellular structures that help confirm identification.
DNA Barcoding: Advanced techniques like DNA barcoding provide highly accurate species identification.
Expert Consultation: Consulting with experienced botanists or herbalists can help verify identification and ensure accuracy.
In essence, accurate botanical identification is a non-negotiable aspect of responsible herbal medicine practice, safeguarding both patient safety and treatment efficacy.
Q 12. Explain the concept of ‘Doctrine of Signatures’ and its relevance (or lack thereof) in modern herbalism.
The Doctrine of Signatures is an ancient belief that the appearance of a plant suggests its medicinal use. For example, a plant with a heart-shaped leaf might be believed to be good for the heart. While a fascinating historical concept, it holds little relevance in modern herbalism.
Lack of Scientific Basis: The Doctrine of Signatures lacks any scientific basis. The perceived resemblance between a plant’s appearance and a bodily organ or ailment is purely coincidental and doesn’t reflect actual medicinal properties.
Potential for Harm: Relying on the Doctrine of Signatures can be dangerous. A plant may appear similar to another, but it can be ineffective or even toxic if used for the intended purpose based solely on appearance.
Emphasis on Evidence-Based Practices: Modern herbalism emphasizes scientifically validated evidence. Therapeutic uses are determined through rigorous research, including phytochemical analysis, pre-clinical studies, and clinical trials, not based on visual similarities.
The Doctrine of Signatures represents a fascinating chapter in the history of herbal medicine. However, in today’s evidence-based approach, it serves more as a historical curiosity than a practical guide for identifying and utilizing medicinal plants.
Q 13. What is the role of clinical trials in validating the efficacy of herbal remedies?
Clinical trials play a crucial role in validating the efficacy and safety of herbal remedies. While anecdotal evidence and traditional use are valuable starting points, they don’t provide the level of scientific rigor needed to establish therapeutic value definitively.
Establishing Efficacy: Well-designed clinical trials provide evidence on whether an herbal remedy works for a specific condition. They involve rigorous study designs, including randomized controlled trials (RCTs), to determine the treatment’s effectiveness compared to a placebo or standard treatment.
Determining Safety: Clinical trials also assess the safety profile of herbal remedies, identifying potential side effects, adverse reactions, and drug interactions. This is crucial for determining the appropriate dosage and identifying contraindications.
Standardization: Herbal remedies can have variable chemical compositions depending on factors like growing conditions and harvesting methods. Clinical trials help establish standardization, ensuring that the product being tested maintains a consistent level of active compounds.
Regulatory Approval: Data from well-conducted clinical trials are often required for regulatory approval of herbal medicinal products, ensuring that they meet certain quality, safety, and efficacy standards.
However, it’s important to note that conducting rigorous clinical trials with herbal remedies can be complex. The complexity of herbal formulations, the variability of plant materials, and the challenges in blinding studies are some factors that make herbal research challenging, but not impossible. High-quality clinical trial data is fundamental to supporting the responsible and effective use of herbal medicines.
Q 14. Describe different methods for extracting active compounds from plants.
Several methods are used to extract active compounds from plants, each with its advantages and disadvantages. The choice of method depends on the desired compounds, the plant material, and the intended application.
Maceration: This is a simple method involving soaking the plant material in a solvent (often water, alcohol, or a mixture) for an extended period. It’s a gentle method suitable for heat-sensitive compounds but can be time-consuming.
Percolation: Similar to maceration, but the solvent continuously flows through the plant material, leading to higher extraction efficiency.
Decoction: The plant material is boiled in water for a prolonged period. This method is effective for extracting water-soluble compounds from tough plant parts like roots and barks.
Infusion: The plant material is steeped in hot water for a shorter time than decoction. This gentler method is suitable for delicate plant parts like leaves and flowers.
Solvent Extraction (e.g., Soxhlet extraction): This method utilizes organic solvents to extract compounds based on their solubility. It’s more efficient than aqueous methods but requires specialized equipment and consideration of solvent toxicity.
Supercritical Fluid Extraction (SFE): This advanced technique utilizes supercritical CO2 as a solvent. It’s environmentally friendly, efficient, and allows for the selective extraction of specific compounds.
Ultrasound-Assisted Extraction (UAE): This method uses ultrasonic waves to enhance the extraction process by disrupting cell walls and increasing the solvent’s penetration into plant tissues.
The selection of extraction method is crucial for achieving the desired quality and yield of active compounds. Understanding the properties of the plant and the target compounds is critical for choosing the most suitable extraction technique.
Q 15. How do you determine the appropriate dosage of an herbal preparation?
Determining the appropriate dosage of an herbal preparation is a nuanced process that requires careful consideration of several factors. It’s not a one-size-fits-all approach, and a standardized dosage rarely exists. Instead, we must consider the patient’s individual characteristics, the specific herb being used, and the desired outcome.
- Patient Factors: Age, weight, overall health, existing medical conditions, and concurrent medications significantly influence dosage. For example, a child will require a much smaller dose than an adult, and someone with liver or kidney impairment may need a reduced dose to avoid potential toxicity.
- Herb-Specific Factors: Different herbs have different potencies and active constituents. The concentration of active compounds in the preparation (tincture, extract, tea, etc.) also plays a crucial role. For instance, a standardized extract of Echinacea will have a consistent concentration of active compounds, making dosage calculation more predictable than with a simple tea made from the herb.
- Desired Outcome: The intended therapeutic effect determines the appropriate dosage. A lower dose may be sufficient for mild symptoms, while a higher dose (always within safe limits) may be necessary for more severe conditions. This requires careful monitoring and adjustment based on the patient’s response.
In practice, I often start with a low dose and gradually increase it until the desired effect is achieved, while carefully monitoring for adverse reactions. This approach, coupled with thorough patient history and ongoing assessment, ensures safety and effectiveness.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Discuss the ethical considerations related to harvesting and sourcing herbal materials.
Ethical harvesting and sourcing of herbal materials are paramount in botanical medicine. It’s not only about ensuring the quality and safety of the product but also about protecting biodiversity and supporting sustainable practices.
- Sustainable Harvesting: Over-harvesting can lead to depletion of plant populations, endangering the species. Ethical harvesting involves taking only what is needed, leaving sufficient plants to reproduce and ensuring the long-term survival of the species. This might involve selective harvesting or using only specific parts of the plant.
- Wildcrafting vs. Cultivation: Wildcrafting, while sometimes necessary, should be done responsibly, with knowledge of the plant’s growth cycle and avoiding endangered species. Cultivation, whenever feasible, is preferable as it allows for controlled harvesting and reduces the environmental impact.
- Fair Trade and Ethical Sourcing: Supporting fair trade practices ensures that those involved in the harvesting and processing of herbal materials receive fair compensation and work in safe conditions. This is especially important for those in developing countries where many herbal remedies originate.
- Transparency and Traceability: Knowing the origin of herbal materials is critical. This includes information on the growing conditions, harvesting methods, and processing techniques. Transparent supply chains build trust and ensure the quality and safety of the product.
For example, I prioritize suppliers who demonstrate commitment to sustainable and ethical practices, providing documentation that supports their claims. This commitment extends to informing patients about the origin and harvesting methods of the herbs they are using.
Q 17. Explain the importance of patient education in botanical medicine.
Patient education is the cornerstone of safe and effective botanical medicine. It empowers patients to actively participate in their healthcare and makes them responsible partners in the therapeutic process.
- Understanding the Herb: Patients need to understand the herb’s intended use, its potential benefits, and its potential risks. This includes information about active constituents, possible interactions with other medications, and expected side effects.
- Proper Dosage and Administration: Clear instructions on dosage, frequency of administration, and methods of preparation are crucial to avoid errors and ensure efficacy. I always provide written instructions and answer any questions the patient may have.
- Monitoring and Reporting: Patients should be educated on how to monitor their response to the treatment and report any adverse reactions or unexpected effects. Open communication is critical for adjusting the treatment plan as needed.
- Lifestyle Modifications: In many cases, lifestyle changes complement herbal remedies. This might include dietary adjustments, exercise recommendations, stress management techniques, or other lifestyle choices that promote overall well-being.
For instance, I would explain to a patient using St. John’s Wort for mild depression that it may take several weeks to see an effect and that they should avoid exposure to direct sunlight to reduce the risk of photosensitivity.
Q 18. How do you manage adverse reactions to herbal remedies?
Managing adverse reactions to herbal remedies requires a systematic approach that prioritizes patient safety and effective communication.
- Assessment: The first step is to carefully assess the nature and severity of the adverse reaction. This involves gathering information from the patient about their symptoms, the timing of onset, and the dosage of the herb.
- Discontinuation: If the reaction is significant, the herb should be discontinued immediately. This is especially important for serious reactions like allergic responses or significant organ dysfunction.
- Supportive Care: Supportive care might involve managing symptoms with appropriate medications or other interventions. For instance, an allergic reaction might require antihistamines or corticosteroids.
- Referral: Depending on the severity of the reaction, referral to a physician or other healthcare professional may be necessary. This is especially crucial if the reaction is severe, life-threatening, or if the cause is unclear.
- Documentation: Thorough documentation of the adverse reaction, including the herb involved, the dosage, the symptoms experienced, and the management provided, is essential for future reference and potential reporting to relevant regulatory bodies.
For example, if a patient experiences a mild gastrointestinal upset after taking chamomile tea, we might recommend reducing the dose or switching to a different preparation. However, a severe allergic reaction, such as anaphylaxis, would require immediate discontinuation of the herb and emergency medical attention.
Q 19. What are some common safety precautions to advise patients about when using herbal remedies?
Safety precautions are essential when using herbal remedies, especially when considering potential drug interactions or contraindications.
- Consult a Healthcare Professional: Always advise patients to consult with a healthcare provider before starting any herbal remedy, particularly if they have pre-existing conditions, are pregnant or breastfeeding, or are taking other medications. Many herbs can interact with prescription drugs, leading to unpredictable or potentially harmful effects.
- Start with Low Doses: Recommend starting with low doses and gradually increasing them under supervision to minimize the risk of adverse reactions. This is especially important for potent herbs.
- Read Labels Carefully: Advise patients to read the labels carefully and follow the instructions provided. This includes information about dosage, warnings, and potential side effects.
- Avoid Herbs During Pregnancy and Breastfeeding: Many herbs are not well-studied in pregnant or breastfeeding women and may pose risks to the mother or child. It’s generally recommended to avoid them unless specifically advised by a healthcare professional.
- Store Properly: Herbal remedies should be stored properly to maintain their quality and prevent degradation. This may involve keeping them in a cool, dark, and dry place.
For example, I would caution a patient taking blood thinners against using Ginkgo biloba without consulting their doctor, as Ginkgo can increase bleeding risk.
Q 20. Discuss the regulatory landscape surrounding herbal products in your region.
(Note: The regulatory landscape surrounding herbal products varies significantly depending on the region. This answer provides a general overview, and specific regulations should be consulted for your region.)
The regulatory landscape for herbal products is complex and often less stringent than that for pharmaceutical drugs. In many regions, herbal products are categorized as dietary supplements or food products, resulting in less rigorous testing and approval processes. This can raise concerns about quality control, standardization, and safety.
Regulations often focus on labeling requirements, such as accurate ingredient lists, claims substantiation, and warnings about potential interactions or side effects. There may also be Good Manufacturing Practices (GMP) guidelines that manufacturers must follow to ensure the quality and safety of their products. However, the level of enforcement and the stringency of these regulations can vary considerably.
It’s essential to stay updated on the specific regulations in your area and to ensure that any herbal products used meet the minimum quality standards. This includes consulting with relevant regulatory agencies and seeking out reputable suppliers committed to quality control and ethical sourcing.
Q 21. Describe your experience with different herbal extraction methods (e.g., maceration, percolation).
I have extensive experience with various herbal extraction methods, each offering distinct advantages and disadvantages depending on the herb and desired outcome.
- Maceration: This is a simple method involving soaking the plant material in a solvent (usually alcohol or water) for an extended period (often several weeks). It’s relatively easy to perform but can be less efficient than other methods. I use maceration for herbs that are delicate and might be damaged by more aggressive techniques.
- Percolation: This method involves slowly passing a solvent through a bed of plant material. It’s more efficient than maceration, yielding a higher concentration of active compounds. I use percolation for herbs that are more robust and where a higher concentration of extract is desired.
- Decoction: This involves boiling the plant material in water. It’s suitable for extracting water-soluble compounds from tough plant parts, such as roots or bark. I utilize decoctions for herbs where water-soluble compounds are of primary interest.
- Tinctures: These are liquid extracts typically made using alcohol as a solvent. Alcohol helps to extract a wider range of compounds, including both water-soluble and fat-soluble components, creating a concentrated extract. Many of my herbal formulations incorporate tinctures due to their stability and concentration.
- Hydroalcoholic Extracts: These extracts use a mixture of water and alcohol, often combining the benefits of both solvents. They are suitable for a broad range of herbs and provide a good balance between extraction efficiency and preservation of active compounds.
The choice of extraction method depends on several factors, including the nature of the plant material, the desired constituents, and the intended application. Each method has its unique characteristics, and a thorough understanding of these is crucial for producing safe and effective herbal preparations.
Q 22. Explain the difference between single herbs and herbal formulas.
The core difference between single herbs and herbal formulas lies in their complexity and synergistic effects. A single herb, like chamomile (Matricaria chamomilla), utilizes the plant’s inherent properties for therapeutic purposes. Its effects are largely determined by the active compounds present in that specific plant. For instance, chamomile is known for its calming and anti-inflammatory properties due to compounds like apigenin.
An herbal formula, conversely, is a carefully crafted blend of several herbs, each selected for its specific action and contribution to the overall therapeutic goal. The formula’s efficacy relies not only on the individual herbs’ properties but also on the synergistic interactions between them. Think of it like an orchestra – each instrument (herb) plays a unique part, but together they create a harmonious and more powerful effect than any single instrument could achieve alone. For example, a formula for digestive upset might combine ginger (for anti-nausea), peppermint (for spasmolytic effects), and chamomile (for anti-inflammatory and soothing effects). The combination targets multiple facets of the problem for a more comprehensive approach.
Q 23. How do you approach diagnosing a patient using a combination of conventional and botanical approaches?
My approach to diagnosis integrates conventional and botanical medicine seamlessly. It starts with a thorough patient history, including their current symptoms, medical history, lifestyle, and dietary habits. I then use conventional diagnostic tools, such as blood tests, imaging (if necessary), and physical examination to identify any underlying pathology. This provides a foundation for understanding the patient’s physiological state.
Next, I incorporate botanical medicine principles by considering the patient’s individual constitution and the energetic patterns reflected in their symptoms. This involves exploring possible imbalances in their energy flow, as understood in Traditional Chinese Medicine (TCM) or Ayurveda, for example. I also assess the patient’s emotional and psychological well-being, as these factors often impact health. The integration of both perspectives allows me to develop a comprehensive treatment plan that addresses both the physiological and energetic dimensions of illness. For instance, if a patient presents with anxiety and digestive issues, conventional tests might reveal nothing, but a botanical approach might uncover patterns suggestive of liver Qi stagnation, informing the selection of herbs like Scutellaria baicalensis and Chrysanthemum morifolium.
Q 24. What is your understanding of the placebo effect in relation to herbal treatments?
The placebo effect is a powerful phenomenon that can influence the outcome of any treatment, including herbal medicine. It refers to a patient’s experience of improvement simply because they *believe* they are receiving an effective treatment, regardless of the treatment’s actual pharmacological properties. It’s a complex interplay of psychological and physiological factors.
In botanical medicine, the placebo effect shouldn’t be dismissed. A practitioner’s confidence, the ritual of taking the herbs, and the patient’s belief in the treatment can positively influence the healing process. However, it’s crucial to distinguish between the placebo effect and true therapeutic efficacy. Rigorous clinical trials are necessary to demonstrate that a herb or formula provides a benefit beyond the placebo response. Ethically, it is essential to be transparent with patients about the potential role of the placebo effect and to focus on providing the best possible, evidence-based care.
Q 25. Describe a situation where you had to address a patient’s concerns or misunderstandings about herbal medicine.
One patient, a middle-aged woman, expressed skepticism about herbal medicine, believing it to be less effective or even dangerous compared to conventional pharmaceuticals. She had experienced chronic fatigue and was hesitant to use herbs due to past experiences with supplements that had little effect. I listened empathetically and explained the evidence-based scientific research behind the specific herbs I proposed. I discussed the different mechanisms of action, highlighting that herbs work differently and often more gently than pharmaceuticals. I focused on the synergistic effects of the formula I designed, emphasizing the combined benefits beyond the effects of individual herbs. I provided her with peer-reviewed studies and information about the quality control of the herbal products I used. Finally, I offered a trial period where we could monitor her progress carefully and adjust the treatment as needed, allowing her to see the efficacy firsthand. Her trust grew significantly as we progressed, and she ultimately experienced considerable relief from her symptoms.
Q 26. How do you stay current with the latest research and developments in botanical medicine?
Staying current in botanical medicine requires a multi-faceted approach. I regularly review peer-reviewed journals such as the Journal of Ethnopharmacology and Phytomedicine to access the latest scientific findings on herbal remedies. I attend professional conferences and workshops, often presented by leading experts in the field. This provides a forum for networking with colleagues and learning about cutting-edge research and clinical practice. Additionally, I leverage online databases like PubMed and Google Scholar to search for relevant studies and stay abreast of new developments in herbal research.
Participation in continuing education courses is essential. I focus on courses that cover topics like clinical herbalism, phytochemistry, and the latest advances in herbal medicine research. This ongoing learning enables me to ensure that my knowledge and practices align with current evidence and best practices.
Q 27. What resources do you use to verify the safety and efficacy of herbal remedies?
Verifying the safety and efficacy of herbal remedies is paramount. I rely on several crucial resources: reputable scientific literature (peer-reviewed journals and books); comprehensive herbals and pharmacopeias (such as the British Herbal Pharmacopoeia); and professional organizations such as the American Herbalists Guild (AHG). These sources provide detailed information on a herb’s chemical constituents, known pharmacological effects, potential interactions with conventional medications, and reported adverse effects.
I also examine the quality control measures of the herbal products I use. I prefer products from reputable suppliers who conduct rigorous testing for purity, potency, and the absence of contaminants. It’s important to verify that the products have undergone appropriate quality assurance processes. This multifaceted approach helps minimize the risks associated with herbal treatments and ensure the safety and efficacy of the remedies I recommend.
Q 28. Describe your approach to maintaining accurate patient records related to herbal treatments.
Maintaining accurate patient records is crucial for ethical and legal reasons. My approach involves using a secure electronic health record (EHR) system designed to manage patient information in compliance with all relevant regulations. The EHR meticulously documents all aspects of patient care, including a detailed patient history, diagnosis, treatment plan, progress notes, herbal formulas prescribed (including specific herbs, dosages, and preparations), and any adverse effects observed.
The documentation is written in a clear and concise manner, utilizing standardized terminology to avoid ambiguity. I also include patient consent forms reflecting their understanding of the treatment plan. Regularly reviewing patient charts helps to track progress, assess the efficacy of the interventions, and identify any potential problems or adverse reactions early on. This thorough record-keeping ensures consistent, safe, and effective care, and it also provides crucial information if a consultation with other healthcare professionals is needed.
Key Topics to Learn for Botanical Medicine Interview
- Plant Identification and Taxonomy: Understanding plant families, species, and their distinguishing characteristics is fundamental. Practical application includes accurate herb identification for safe and effective use.
- Phytochemistry: Knowledge of the active constituents in plants (alkaloids, glycosides, etc.) and their therapeutic properties is crucial. This includes understanding how these compounds interact with the body.
- Herbal Preparations and Dosage Forms: Familiarity with various methods of herbal preparation (tinctures, decoctions, etc.) and appropriate dosage forms for different conditions is essential for safe and effective practice.
- Pharmacology and Therapeutics of Botanicals: Understanding the mechanisms of action of botanical medicines and their therapeutic applications in treating various health conditions is critical. This includes knowledge of contraindications and potential drug interactions.
- Clinical Applications and Case Studies: Reviewing successful case studies and understanding the clinical application of botanical medicine in different therapeutic areas will demonstrate your practical experience and problem-solving skills.
- Safety and Quality Control: Knowledge of quality control measures, ethical sourcing of botanicals, and potential adverse effects is crucial for responsible practice. This includes understanding proper storage and handling procedures.
- Traditional Medicine Systems: Familiarity with traditional systems (Ayurveda, Traditional Chinese Medicine, etc.) that utilize botanical medicine will broaden your understanding and perspective.
- Research and Evidence-Based Practice: Demonstrating an understanding of current research and evidence-based practices in botanical medicine is important for showcasing your commitment to professional development.
Next Steps
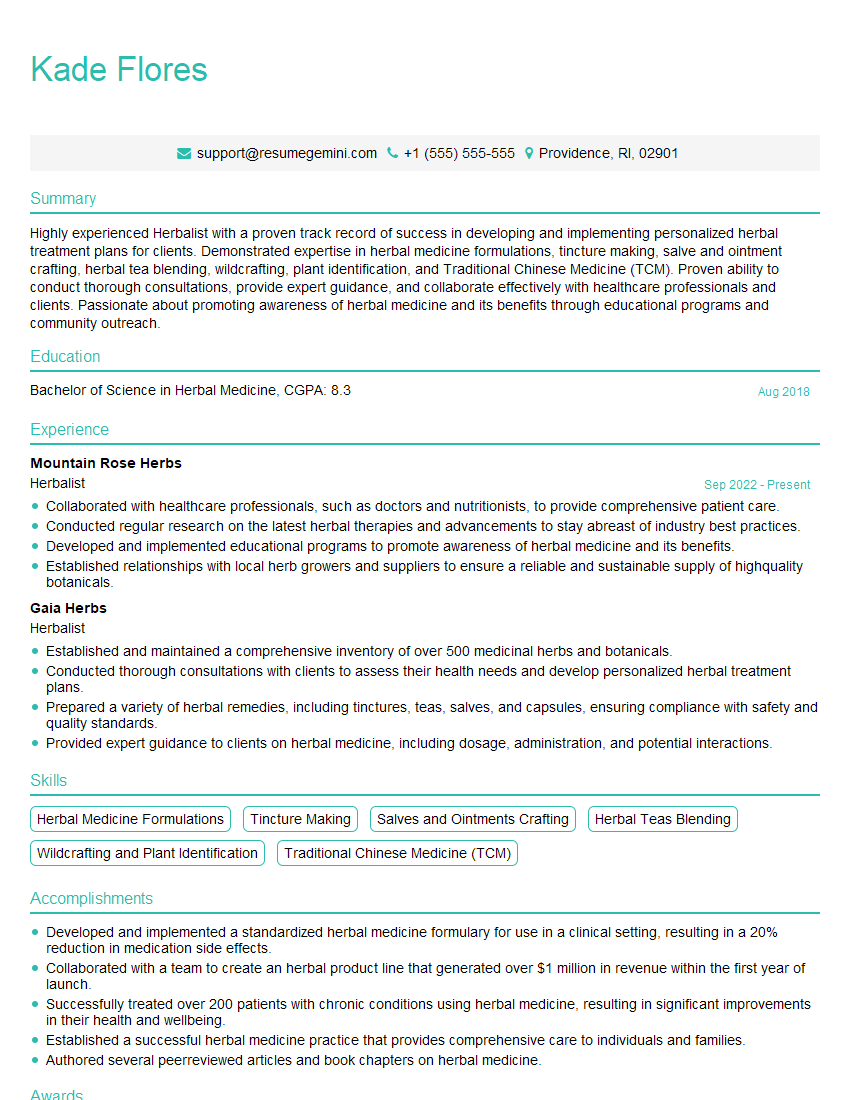
Mastering Botanical Medicine opens doors to a rewarding career with diverse opportunities in research, clinical practice, and education. To maximize your job prospects, a well-crafted, ATS-friendly resume is essential. ResumeGemini is a trusted resource to help you build a professional resume that highlights your skills and experience effectively. Examples of resumes tailored specifically to Botanical Medicine careers are provided to guide you in creating a compelling application.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.