Are you ready to stand out in your next interview? Understanding and preparing for Exposure and Response Prevention (ERP) interview questions is a game-changer. In this blog, we’ve compiled key questions and expert advice to help you showcase your skills with confidence and precision. Let’s get started on your journey to acing the interview.
Questions Asked in Exposure and Response Prevention (ERP) Interview
Q 1. Describe the core principles of Exposure and Response Prevention (ERP).
Exposure and Response Prevention (ERP) is the gold standard treatment for obsessive-compulsive disorder (OCD) and related anxiety disorders. Its core principle lies in breaking the cycle of obsessive thoughts and compulsive behaviors. It works by systematically exposing individuals to feared stimuli (the ‘exposure’ part) and then preventing them from engaging in their usual compulsive responses or avoidance behaviors (the ‘response prevention’ part).
Imagine someone with a fear of contamination. Their obsession might be the thought of being covered in germs. Their compulsion might be excessive handwashing. ERP would involve gradually exposing them to situations that trigger these fears (e.g., touching a doorknob, handling dirty laundry) and then resisting the urge to wash their hands excessively. Over time, the anxiety diminishes as they learn that the feared outcome doesn’t materialize.
This process gradually reduces the power of obsessions and the need for compulsions, leading to improved functioning and quality of life. The key is gradual exposure and consistent response prevention, working collaboratively with the client to build confidence and resilience.
Q 2. Explain the difference between in-vivo and imaginal exposure.
Both in-vivo and imaginal exposure are crucial techniques within ERP, but they differ in their mode of delivery. In-vivo exposure involves direct, real-life exposure to feared situations or objects. For example, if someone has a social anxiety disorder, in-vivo exposure might involve attending a social gathering. Imaginal exposure, conversely, involves imagining the feared situation vividly. If the same person fears public speaking, imaginal exposure might involve repeatedly visualizing themselves giving a speech, experiencing and processing the associated anxiety within a safe therapeutic setting.
The choice between the two depends on several factors including the client’s comfort level, the feasibility of in-vivo exposure, and the specific nature of the anxiety. Often, a combination of both approaches yields the best results. In-vivo exposure is generally considered more powerful due to its real-world relevance, but imaginal exposure can be extremely helpful in situations where in-vivo exposure is difficult, impractical, or too anxiety-provoking to begin with.
Q 3. How do you assess a client’s readiness for ERP?
Assessing a client’s readiness for ERP is crucial for successful therapy. It’s not a one-size-fits-all approach. I utilize a multi-faceted assessment that encompasses:
- Motivation and commitment: The client needs to be actively motivated to change and willing to engage fully in the process.
- Understanding of the treatment: The client should have a clear understanding of ERP’s principles and how it works. This involves thorough psychoeducation.
- Anxiety management skills: Clients benefit from having some basic coping mechanisms to manage anxiety during exposure exercises. These might include relaxation techniques or mindfulness practices.
- Therapeutic alliance: A strong therapeutic relationship built on trust and collaboration is essential. The client needs to feel safe and supported by the therapist.
- Baseline anxiety levels: An initial assessment of the client’s anxiety levels helps establish a starting point and monitor progress.
If a client lacks readiness, I would focus on building the necessary foundation before initiating formal ERP. This might involve psychoeducation, relaxation training, or addressing any co-occurring conditions.
Q 4. What are some common challenges encountered during ERP therapy, and how do you address them?
Several challenges can arise during ERP. Avoidance remains a significant hurdle, as clients might try to escape exposure exercises. I address this by collaboratively developing a hierarchy of feared situations and gradually working through them, starting with less anxiety-provoking stimuli. Safety behaviors, like checking or reassurance-seeking, interfere with the therapeutic process. I help clients identify and gradually reduce these behaviors. Emotional dysregulation can be challenging, requiring the implementation of emotion regulation techniques.
Reluctance to participate is another common challenge, often stemming from fear of the anxiety itself. I validate these feelings while encouraging engagement by emphasizing the benefits of ERP and collaboratively crafting a personalized treatment plan. I continually reassess and adjust the exposure hierarchy to ensure the process remains manageable and motivating. Building a strong therapeutic alliance is key in navigating these challenges, fostering open communication, and tailoring the approach to meet individual needs.
Q 5. Describe your approach to tailoring ERP to different anxiety disorders (e.g., OCD, PTSD, phobias).
While the core principles of ERP remain consistent across different anxiety disorders, the specific targets and techniques vary. For OCD, ERP focuses on exposing clients to obsession-related triggers and preventing compulsive responses. For PTSD, exposure might involve recounting traumatic memories or revisiting trauma-related places. For phobias, ERP targets the specific feared object or situation.
With OCD, the hierarchy might involve gradually touching contaminated objects. With PTSD, it might involve writing about the trauma or gradually approaching related sensory cues. For a phobia of spiders, exposure might involve looking at pictures of spiders, then observing real spiders in a controlled setting, and ultimately interacting with them. The tailoring lies in the specific content of the exposure and the pace at which the exposure is introduced. Collaboration with the client is crucial to ensure the process remains relevant and manageable.
Q 6. How do you incorporate relapse prevention strategies into ERP treatment?
Relapse prevention is a critical component of ERP. It involves equipping clients with skills and strategies to manage anxiety and prevent a return to compulsive behaviors. This includes:
- Identifying high-risk situations: Clients learn to recognize situations or thoughts that might trigger relapse.
- Developing coping strategies: Clients develop alternative ways of dealing with anxiety, such as relaxation techniques, mindfulness, and problem-solving skills.
- Planning for setbacks: Clients are prepared for the possibility of setbacks and learn how to respond effectively. This includes having a plan in place for managing difficult moments.
- Building self-efficacy: Clients develop confidence in their ability to manage anxiety and resist compulsions.
- Regular check-ins: Ongoing sessions focus on maintaining progress and addressing any emerging challenges. Booster sessions might be beneficial.
Relapse prevention is an ongoing process, not just a final step, ensuring long-term success and sustainable improvement in managing anxiety.
Q 7. Explain the role of psychoeducation in ERP therapy.
Psychoeducation plays a vital role in ERP therapy. It empowers clients with knowledge about their anxiety disorder, its mechanisms, and the rationale behind ERP. This includes explaining the cycle of obsessions and compulsions, why avoidance maintains the problem, and how ERP helps break this cycle.
Psychoeducation helps clients understand that their thoughts and feelings are not facts but interpretations of reality. It normalizes their experiences, reduces feelings of shame or guilt, and encourages active participation in the therapy. It also builds trust and collaboration, fostering a therapeutic relationship that is built on mutual understanding and shared goals. Effective psychoeducation sets the stage for a successful ERP journey and helps maintain long-term recovery.
Q 8. How do you collaborate with other healthcare professionals (e.g., psychiatrists, physicians) in the treatment of clients using ERP?
Collaboration with other healthcare professionals is crucial for holistic client care in ERP. I regularly consult with psychiatrists and physicians, especially when clients present with comorbid conditions. For instance, if a client has severe depression alongside OCD, I’d work closely with their psychiatrist to ensure their medication is optimally managed and doesn’t interfere with ERP’s effectiveness. We’d coordinate treatment plans, regularly discussing the client’s progress and adjusting strategies as needed. This collaborative approach ensures a comprehensive and integrated treatment approach, maximizing the chances of success. Open communication is key, sharing information about the client’s response to both medication and therapy. We might use a shared electronic health record system or regular meetings to maintain clear communication and a cohesive treatment plan.
Q 9. Describe a case where ERP was highly effective. What were the key factors that contributed to success?
I once worked with a young woman, Sarah, who suffered from severe contamination OCD. Her life was significantly impacted; she spent hours cleaning, avoiding public spaces, and experiencing intense anxiety. ERP was highly effective in her case. Key to her success was the careful development of a graduated exposure hierarchy. We started with relatively low-anxiety situations, like touching a doorknob after washing her hands, gradually progressing to more challenging scenarios. In-vivo exposure was central; we didn’t just talk about her fears, we confronted them directly. Another critical factor was Sarah’s active participation and commitment to the process. She meticulously tracked her anxiety levels and diligently completed her homework assignments between sessions. Finally, regular feedback and reinforcement of her progress were crucial. Seeing her anxiety decrease with each exposure boosted her confidence and motivation. By the end of treatment, Sarah was able to manage her OCD symptoms effectively and lead a much fuller life.
Q 10. Describe a case where ERP was less effective. What factors might have contributed to this outcome?
Not every case of ERP leads to complete remission. I recall a client, Mark, who struggled with severe checking rituals. While he initially engaged well, his progress plateaued after several months. Several factors likely contributed. Mark experienced significant avoidance, making consistent in-vivo exposure challenging. His perfectionism hindered his ability to tolerate uncertainty and accept the possibility of error – a fundamental aspect of ERP. He also struggled with depression, which seemed to significantly impact his motivation and ability to engage fully in therapy. In hindsight, integrating techniques to address his depression, such as cognitive restructuring, might have been beneficial. Early identification of these challenges could have allowed for timely adjustments to the treatment plan, perhaps incorporating additional strategies to address the underlying depression and enhance his motivation.
Q 11. How do you measure the effectiveness of ERP treatment?
Measuring the effectiveness of ERP involves a multifaceted approach. We utilize self-report measures such as the Yale-Brown Obsessive Compulsive Scale (Y-BOCS) and the Obsessive-Compulsive Inventory (OCI) to quantify symptom severity at baseline and throughout treatment. These provide objective data tracking changes in the frequency and intensity of obsessions and compulsions. We also conduct regular clinical interviews to assess the client’s overall functioning and subjective experience. This provides qualitative information alongside the quantitative data. Finally, functional analysis helps determine whether the reductions in symptoms translate into tangible improvements in the client’s daily life. This might involve tracking avoidance behaviors, time spent on rituals, and participation in previously avoided activities.
Q 12. What are the ethical considerations involved in using ERP?
Ethical considerations in ERP are paramount. Informed consent is essential, ensuring clients understand the nature of the treatment, potential risks and benefits, and their right to withdraw at any time. Respecting client autonomy means never pressuring them into exposures they’re not ready for. Maintaining confidentiality and establishing a strong therapeutic alliance built on trust and collaboration is crucial. Recognizing the potential for temporary increases in anxiety during exposure is vital, and proactively managing this through thorough preparation, support, and appropriate pacing is an ethical responsibility. Clinicians must be mindful of their own biases and ensure that their treatment is tailored to the individual client’s needs and preferences, avoiding a one-size-fits-all approach.
Q 13. How do you manage client resistance during ERP therapy?
Managing client resistance is a common challenge in ERP. It often stems from fear, avoidance, or a lack of understanding. Firstly, I address any misconceptions or concerns about the therapy using collaborative dialogue, creating a safe space for exploration. Building rapport and establishing trust is fundamental. I might utilize motivational interviewing techniques to help the client understand the benefits of facing their fears, and collaboratively establish achievable goals. Gradually increasing the intensity and duration of exposures reduces the feeling of being overwhelmed. Celebrating even small successes reinforces progress and motivation. Focusing on the client’s strengths and resources helps build self-efficacy and empowers them to navigate their challenges. Furthermore, regularly reviewing the therapy’s progress and adjusting the treatment plan as needed ensures ongoing engagement and alleviates feelings of stagnation.
Q 14. What modifications might you make to ERP for clients with comorbid conditions (e.g., depression, substance abuse)?
Adapting ERP for clients with comorbid conditions requires a tailored approach. For instance, a client with depression alongside OCD might benefit from integrating techniques to address the depression, such as cognitive behavioral therapy (CBT) for depression alongside ERP for OCD. The timing and sequence of interventions must be carefully considered. If substance abuse is present, addiction treatment should be a priority. ERP might be introduced after a period of stabilization. Collaboration with other specialists, such as psychiatrists or addiction specialists, is essential to create a comprehensive and coordinated treatment plan. Treatment progress should be carefully monitored, and the treatment plan adjusted as needed to accommodate the complexities of comorbid conditions. The pacing of ERP may need to be adjusted, given that a client’s energy levels and capacity to participate may be impacted by their other conditions.
Q 15. Describe your approach to working with clients who have difficulty tolerating distress.
Working with clients struggling to tolerate distress is central to ERP. It’s not about eliminating discomfort entirely, but about building the skill to manage it effectively. My approach focuses on collaborative goal setting, psychoeducation about anxiety, and gradual exposure to feared situations. We start by understanding the client’s experience of distress, validating their feelings, and collaboratively developing coping strategies. This might involve teaching mindfulness techniques, relaxation exercises like deep breathing or progressive muscle relaxation, or even just identifying and labeling their emotions. We then practice these coping mechanisms during less intense situations before gradually working up to more challenging exposures.
For example, if a client with OCD experiences intense anxiety when touching doorknobs, we wouldn’t jump straight to that. We might start with visualizing touching a doorknob, then imagining the feeling, then touching a clean, easily-wiped-down surface like a countertop. Each step builds tolerance and reduces the overall distress. Importantly, I emphasize that some discomfort is expected and even necessary for progress. The goal isn’t comfort, but rather learning to function effectively in the presence of discomfort.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you build a strong therapeutic alliance with clients undergoing ERP?
Building a strong therapeutic alliance is paramount in ERP, as it requires a high level of trust and collaboration. This starts from the initial sessions, where I focus on creating a safe, non-judgmental space for the client to share their anxieties and concerns openly. I actively listen, validate their fears, and emphasize the collaborative nature of the therapy. We work together to develop a personalized treatment plan, ensuring the client feels involved and in control of the process. Regularly checking in with the client regarding their experience and adjusting the treatment plan accordingly is crucial. Empathy, transparency, and demonstrating genuine concern for their well-being are essential in building this rapport.
For instance, I might share my understanding of the challenges they face by saying something like, “I can see how difficult it is to confront these fears, but I’m confident that with our work together, we can manage them effectively.” This demonstrates understanding and encourages continued engagement.
Q 17. What are some common misconceptions about ERP?
Several common misconceptions surround ERP. One is the belief that it involves confronting fears all at once. ERP is about gradual exposure, starting with less intense situations and gradually working up to more challenging ones. Another misconception is that avoiding feared situations is helpful. In fact, avoidance reinforces anxiety. Finally, some believe that ERP aims to eliminate anxiety entirely. While the goal is to reduce anxiety and improve functioning, some level of anxiety is normal and expected. The aim is to manage and cope with this anxiety, not eliminate it completely.
For instance, someone might think that if they have a fear of public speaking, ERP would involve immediately giving a speech in front of a large audience. This is incorrect. We would start with much smaller, less intimidating steps, perhaps practicing in front of a mirror, then a friend, and gradually increasing the size and formality of the audience.
Q 18. How do you address potential safety concerns during exposure exercises?
Addressing safety concerns is crucial in ERP, particularly with exposure exercises. A thorough safety planning process is implemented at the start of therapy. This involves identifying potential triggers, developing coping mechanisms, and creating a detailed plan to manage any unexpected events. This plan is co-created with the client and might involve having a support person present during exposures, identifying safe spaces to retreat to if needed, and establishing clear communication protocols. Furthermore, I emphasize that the client is in control at all times and can stop an exposure exercise if they feel overwhelmed. We regularly review the safety plan and make adjustments as needed throughout the therapy process.
For example, a client with social anxiety might initially practice approaching strangers in a familiar and safe environment, like their local park, with a friend nearby for support. If the anxiety becomes too overwhelming, they have the option to disengage and take a break, emphasizing that this is a normal and expected part of the process.
Q 19. Explain the hierarchy of fears used in ERP.
A fear hierarchy is a crucial component of ERP. It’s a ranked list of feared situations or objects, starting with those that cause minimal anxiety and progressing to those that provoke intense anxiety. This list is collaboratively created with the client and serves as a roadmap for the exposure therapy. The ordering is based on the client’s subjective experience of anxiety. We usually use a rating scale (e.g., 0-100) to quantify the level of anxiety associated with each item. The hierarchy allows for a gradual approach, ensuring that the client is challenged but not overwhelmed. Starting with less intense fears builds confidence and prepares the client for more challenging exposures.
An example of a fear hierarchy for someone with a fear of dogs might be: 1. Watching a video of a dog, 2. Looking at pictures of dogs, 3. Being in the same room as a dog behind a barrier, 4. Observing a dog from a distance, 5. Petting a small dog with a handler present, 6. Petting a dog independently. This systematic approach allows for incremental progress and reduces the risk of avoidance relapse.
Q 20. Discuss the role of homework assignments in ERP.
Homework assignments are an essential component of ERP because they provide the opportunity for clients to practice their coping skills and exposure exercises outside of the therapy session. This consistent practice is critical for generalization of treatment gains. Homework assignments are tailored to the client’s fear hierarchy and reflect the progress made in sessions. These might involve practicing relaxation techniques, completing graded exposure exercises, or engaging in activities previously avoided. Regular review and feedback on homework assignments in subsequent sessions are crucial to ensure progress and address any challenges the client might have encountered. This ongoing collaborative process builds skills and fosters autonomy.
For example, a client working on their fear of social interactions might be assigned homework to initiate short conversations with cashiers or make small talk with colleagues. The difficulty of these assignments would gradually increase over time, mirroring the progression through their fear hierarchy.
Q 21. How do you adapt ERP for different age groups (children, adolescents, adults)?
Adapting ERP for different age groups requires adjusting the language, techniques, and level of involvement based on the individual’s developmental stage. With children, ERP often incorporates play therapy, storytelling, and age-appropriate metaphors to explain concepts. The fear hierarchy might involve drawings or puppets. Parental involvement is often essential. Adolescents benefit from collaborative goal setting, focusing on social situations relevant to their peer groups. Treatment might integrate technology-based exposure exercises. Adults, in contrast, can engage in more complex discussions about cognitive restructuring and relapse prevention strategies.
For instance, with a child, we might use a game to practice deep breathing or create a story about a character facing a similar fear. With an adolescent, we might use a social media scenario for exposure practice. With an adult, we might delve deeper into the cognitive aspects of their anxiety and develop advanced coping mechanisms.
Q 22. Describe your experience using different exposure techniques (e.g., graded exposure, flooding).
Exposure techniques are the cornerstone of Exposure and Response Prevention (ERP). My experience encompasses both graded exposure and flooding, tailored to individual client needs and anxiety levels. Graded exposure involves gradually confronting feared situations, starting with less anxiety-provoking stimuli and gradually progressing to more intense ones. Think of it like climbing a ladder, one step at a time. For example, a client with social anxiety might start by practicing making eye contact with one person, then engaging in brief conversations, and eventually participating in group settings. Flooding, on the other hand, involves immediate and intense exposure to the feared stimulus. This is usually reserved for clients who are highly motivated and have a strong therapeutic alliance. For instance, a client with a fear of dogs might spend an extended period in a room with a dog, under controlled conditions and with my guidance. I always carefully assess a client’s readiness before using flooding, as it can be more intense and challenging.
The choice between these methods depends on various factors such as the client’s level of anxiety, their personality, and the specific phobia or obsession. I find that a collaborative approach, where the client participates in creating the exposure hierarchy, is crucial for success.
Q 23. How do you differentiate between ERP and other anxiety treatment modalities (e.g., Cognitive Restructuring)?
While both ERP and cognitive restructuring (CR) are effective anxiety treatments, they differ significantly in their approach. ERP focuses on behavioral modification through repeated exposure to feared stimuli and the prevention of compulsive responses. It’s about changing behavior patterns directly. CR, conversely, focuses on identifying and challenging negative or irrational thoughts that contribute to anxiety. It’s about changing the way a person thinks.
Imagine a client with obsessive-compulsive disorder (OCD) and a fear of contamination. ERP would involve repeatedly touching contaminated surfaces (e.g., doorknobs, public restrooms) and resisting the urge to perform compulsive handwashing rituals. CR, on the other hand, would involve helping the client identify and challenge their irrational thoughts about contamination risk (e.g., ‘If I touch this, I’ll get sick’). Often, I find the most effective treatment integrates both approaches. Addressing maladaptive thoughts through CR can facilitate the effectiveness of ERP by making exposure more tolerable and meaningful.
Q 24. Explain the concept of response prevention and its importance in ERP.
Response prevention is the crucial component of ERP that distinguishes it from other therapies. It involves actively preventing or resisting the urge to engage in compulsive behaviors or avoidance strategies that temporarily relieve anxiety. It’s the ‘R’ in ERP. This is not about suppressing feelings but rather about disrupting the negative reinforcement cycle that maintains anxiety disorders. By preventing the response, the individual learns that the feared outcome does not actually occur and the anxiety gradually diminishes.
For example, a client with a fear of germs might have a compulsion to wash their hands repeatedly. In ERP, we would encourage them to resist this urge, gradually increasing the exposure time to situations where they might feel the need to wash. The anxiety initially increases during exposure, but then it decreases as the client learns that nothing bad happens when they don’t perform the ritual. Over time, the compulsive behavior loses its power, leading to sustained reductions in anxiety.
Q 25. How do you handle client crises or setbacks during treatment?
Setbacks are an inevitable part of ERP therapy. When a client experiences a crisis or relapse, I prioritize validating their feelings and collaboratively problem-solving. We examine what might have triggered the setback and adjust the treatment plan accordingly. This may involve reviewing the exposure hierarchy, slowing the pace of exposure, or incorporating additional coping skills training. It’s important to emphasize that setbacks are learning opportunities, not failures. We use these moments to build resilience and reinforce the client’s commitment to the treatment process. For example, if a client relapses into compulsive checking, we might discuss potential triggers and refine the exposure plan to address these more systematically.
Open communication, support, and collaborative problem-solving are essential during challenging times. It might also involve reassessing any underlying issues or co-occurring mental health conditions that may have impacted the treatment’s progress.
Q 26. What are your preferred methods for documenting ERP treatment progress?
My preferred method for documenting ERP treatment progress is a combination of session notes and standardized outcome measures. Session notes capture the details of each session, including the exposures performed, the client’s response, and any adjustments to the treatment plan. I use standardized measures such as the Yale-Brown Obsessive Compulsive Scale (Y-BOCS) or the Obsessive-Compulsive Inventory-Revised (OCI-R) to track symptom severity over time. These provide quantitative data that complements my qualitative observations.
I use a structured format for my notes, documenting the session date, specific exposures undertaken, client’s subjective units of distress (SUDs) ratings before, during, and after exposure, any coping strategies employed, and any homework assignments. Regular monitoring with outcome measures enables us to track progress effectively and makes it easier to identify when adjustments in treatment are needed.
Q 27. What continuing education or professional development activities have you undertaken to stay current in ERP techniques?
Staying current in ERP requires ongoing professional development. I regularly attend workshops and conferences focused on anxiety disorders and evidence-based treatments. I also actively participate in continuing education courses that cover the latest research findings and treatment innovations in ERP. I actively seek supervision from experienced ERP clinicians to refine my skills and address complex clinical challenges. Reading peer-reviewed journals and staying abreast of new publications is equally important for me to ensure I’m using the most up-to-date and effective methods.
Recently I completed a specialized training program on the application of ERP to specific anxiety disorders such as social anxiety disorder and post-traumatic stress disorder (PTSD). I also actively engage in online communities and discussion forums of ERP professionals for sharing knowledge and best practices.
Q 28. Describe your understanding of the current research in Exposure and Response Prevention.
Current research in ERP continues to expand our understanding of its mechanisms of action and its effectiveness across various anxiety disorders. Recent studies have focused on the role of neurobiology in response to ERP, providing insights into how exposure therapy modifies brain circuits associated with fear and anxiety. There is also increasing research on the integration of technology into ERP, such as virtual reality exposure therapy, which offers innovative and accessible ways to deliver exposure treatment.
Researchers are also investigating personalized approaches to ERP, tailoring treatments to individual patient needs and characteristics to maximize effectiveness. The ongoing exploration of factors contributing to treatment response and relapse prevention helps refine and adapt treatment methods to enhance outcomes further. Research is also expanding into integrating mindfulness and acceptance-based techniques within ERP.
Key Topics to Learn for Exposure and Response Prevention (ERP) Interview
- The Theoretical Foundations of ERP: Understand the underlying principles of the cognitive-behavioral model and its application to anxiety disorders. This includes a solid grasp of classical and operant conditioning principles as they relate to the development and maintenance of anxiety.
- Exposure Hierarchy Development: Learn how to collaboratively create a graded exposure hierarchy with clients, considering individual needs and anxieties. Be prepared to discuss the rationale behind different hierarchy construction methods.
- Response Prevention Techniques: Master various response prevention strategies and their application in different clinical contexts. Discuss the importance of therapist support and strategies for managing client resistance.
- Practical Application in Specific Disorders: Demonstrate your knowledge of applying ERP to various anxiety disorders, such as OCD, PTSD, social anxiety disorder, and specific phobias. Be ready to discuss nuances in treatment based on the specific diagnosis.
- Measuring Treatment Progress and Outcome: Discuss different methods for assessing treatment progress and outcome in ERP, including self-report measures, behavioral observations, and clinician-rated scales. Understand the importance of data-driven decision making.
- Ethical Considerations and Challenges: Understand potential ethical considerations and challenges in ERP therapy, including client safety, managing treatment resistance, and navigating difficult therapeutic relationships.
- Integration with Other Therapies: Discuss the potential for integrating ERP with other therapeutic approaches, such as mindfulness-based techniques or acceptance and commitment therapy.
Next Steps
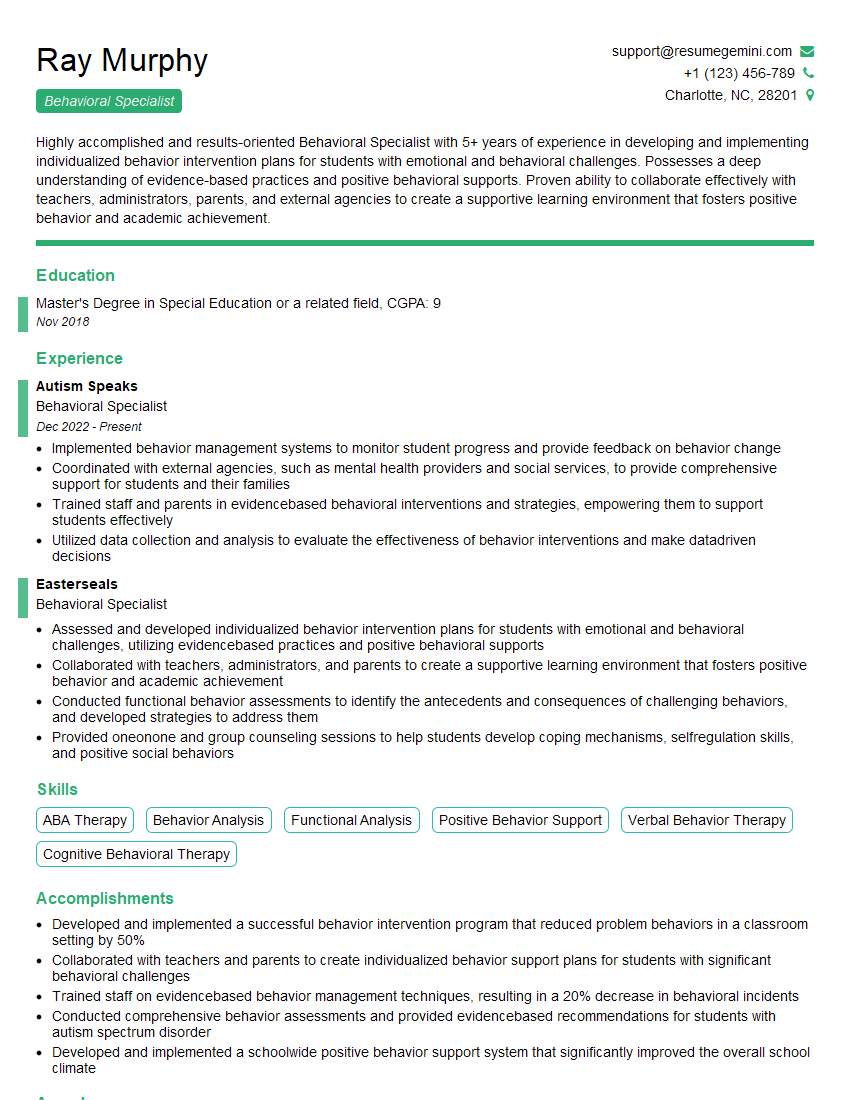
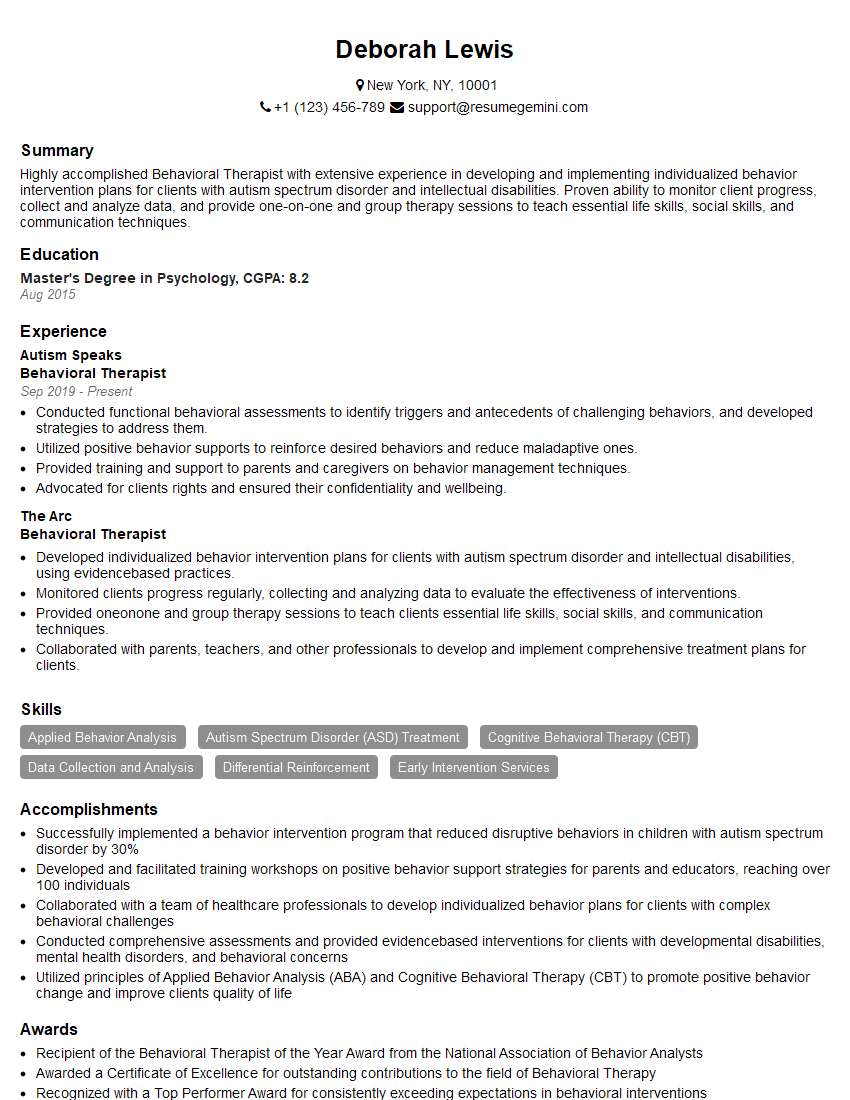
Mastering Exposure and Response Prevention (ERP) opens doors to a rewarding career helping individuals overcome debilitating anxiety. To maximize your job prospects, a strong resume is crucial. An ATS-friendly resume, optimized for Applicant Tracking Systems, significantly increases your chances of getting noticed by potential employers. We highly recommend using ResumeGemini to build a professional and impactful resume that showcases your ERP expertise. ResumeGemini provides examples of resumes tailored specifically to Exposure and Response Prevention (ERP) roles, giving you a head start in crafting your perfect application.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.