Interviews are more than just a Q&A session—they’re a chance to prove your worth. This blog dives into essential Neuropsychological Evaluation interview questions and expert tips to help you align your answers with what hiring managers are looking for. Start preparing to shine!
Questions Asked in Neuropsychological Evaluation Interview
Q 1. Describe the process of administering and interpreting the Wechsler Adult Intelligence Scale (WAIS).
The Wechsler Adult Intelligence Scale (WAIS) is a comprehensive neuropsychological test battery assessing various cognitive abilities. Administering the WAIS involves a structured, one-on-one session where the examiner follows a standardized protocol. Each subtest is presented in a specific order, with clear instructions and demonstrations. The examiner carefully observes the examinee’s performance, noting not only the accuracy of responses but also their approach to problem-solving, speed, and any unusual behaviors. After completing all subtests, raw scores are converted into scaled scores and index scores (e.g., Verbal Comprehension, Perceptual Reasoning, Working Memory, Processing Speed), which allow for a comprehensive profile of the individual’s cognitive strengths and weaknesses. Interpretation goes beyond simply looking at the Full Scale IQ (FSIQ). We analyze the pattern of scores across different indices, identifying significant discrepancies that may indicate specific cognitive impairments. For example, a significant difference between Verbal Comprehension and Perceptual Reasoning indices might suggest a right hemisphere deficit, which would require further investigation. We also consider the individual’s background, medical history, and the reason for referral when interpreting the results, providing a nuanced and individualized report.
Consider a patient referred due to a suspected TBI. Their FSIQ might be within the average range; however, a significantly lower score on the Processing Speed index, coupled with observations of slow response time during the testing session, would suggest difficulties with information processing speed, potentially related to the brain injury. This informs treatment recommendations significantly more than the FSIQ alone.
Q 2. Explain the differences between different types of memory (e.g., working memory, long-term memory, procedural memory).
Memory is a complex cognitive function with various types. Think of it like a filing system for your brain. Working memory is your short-term, active workspace. It’s like the desk where you temporarily hold information you’re currently using, like remembering a phone number long enough to dial it. Long-term memory is the vast storage system containing your past experiences, facts, and skills. This is akin to your entire filing cabinet. It’s further divided into explicit (consciously recalled) and implicit (unconsciously influencing behavior) memory. Explicit memory includes episodic memory (personal events like your last vacation) and semantic memory (general knowledge like the capital of France). Implicit memory encompasses procedural memory (skills like riding a bike) and priming (exposure to a stimulus influences later responses). Procedural memory is like muscle memory – you don’t consciously think about how to ride a bike; you just do it.
Damage to different brain regions can affect different types of memory. For example, damage to the hippocampus often impacts episodic memory, leading to difficulties remembering recent events, while damage to the cerebellum can affect procedural memory, hindering the learning of new motor skills.
Q 3. How do you assess executive functions in a neuropsychological evaluation?
Executive functions are a set of higher-order cognitive skills that allow us to plan, organize, initiate, and inhibit behavior. Think of them as the ‘CEO’ of your brain. We assess these functions using a variety of tests targeting different aspects. The Wisconsin Card Sorting Test (WCST) assesses abstract reasoning, set-shifting, and cognitive flexibility. The Trail Making Test (TMT) measures visual attention, task switching, and processing speed. The Stroop Color-Word Test assesses interference control and selective attention. In addition, tasks involving planning and problem-solving, such as verbal fluency tasks or complex figure copying, are used. Interpretation involves looking at the efficiency and accuracy of performance on these tasks. For instance, difficulties with the WCST can suggest problems with abstract reasoning and adapting to changing demands, which might be seen in patients with frontal lobe damage. Slow and inaccurate performance on the TMT may be indicative of attentional deficits.
For instance, a patient struggling with organization and planning in their daily life might demonstrate difficulty on tasks requiring planning and sequencing of actions. This would warrant a more detailed assessment of their executive functions using the aforementioned tests.
Q 4. What are some common neuropsychological tests used to assess visuospatial skills?
Visuospatial skills involve the ability to perceive, analyze, and manipulate visual information in space. Tests evaluating these skills often include tasks that assess visual perception, spatial relationships, and constructional abilities. Common tests include the Rey-Osterrieth Complex Figure Test (ROCF), which assesses visual perception, memory, and constructional praxis; the Block Design subtest of the WAIS, evaluating spatial reasoning and visual-motor integration; and the Visual Reproduction subtest of the WMS-IV, focusing on visual memory and reproduction. The Judgment of Line Orientation test assesses visual perception of spatial relationships. Interpretation depends on the specific test, but typically involves considering accuracy, speed, and the strategies used by the individual during the task. For example, difficulties on the ROCF might be indicative of right parietal lobe damage, often associated with constructional apraxia (difficulty in drawing and assembling objects).
A patient experiencing difficulties with map reading or assembling furniture might be showing signs of visuospatial deficits, warranting a more thorough neuropsychological evaluation.
Q 5. Describe your approach to interpreting results from a Halstead-Reitan Neuropsychological Battery.
The Halstead-Reitan Neuropsychological Battery (HRNB) is a comprehensive and lengthy battery providing a detailed assessment of various cognitive domains. Interpreting the HRNB is a complex process, and I follow a multi-step approach. First, I carefully review the individual’s performance on each subtest, noting both quantitative scores and qualitative observations. Next, I analyze the pattern of scores, identifying any significant strengths or weaknesses. The HRNB’s strength lies in its ability to identify lateralized deficits (left vs. right hemisphere) and diffuse impairments. I then integrate these findings with the individual’s history, including medical records, behavioral observations during testing, and collateral information from family and friends. Finally, I generate a comprehensive report that includes a description of the individual’s cognitive strengths and weaknesses, potential explanations for the findings, and recommendations for further assessment or intervention. Simply looking at individual test scores is insufficient; I always focus on the pattern of findings and its implications for the individual’s daily functioning.
For example, a patient showing impairments across multiple domains, with particular deficits in verbal fluency and memory but relatively preserved perceptual skills, would suggest a different profile than a patient with isolated visuospatial deficits. The combination of these findings and clinical context allows for targeted diagnosis and treatment planning.
Q 6. How do you differentiate between symptoms of depression and cognitive impairment?
Differentiating between depression and cognitive impairment can be challenging because both can present with similar symptoms, such as slowed processing speed, difficulty concentrating, and memory problems. The key is to look for a pattern of symptoms. Depression is often associated with subjective complaints of cognitive difficulties (the patient reports these), rather than objective evidence on neuropsychological testing. Cognitive impairment, on the other hand, often reveals demonstrable deficits on standardized tests, impacting specific cognitive domains rather than being a generalized slowing of cognitive functions. For example, a patient with depression might report significant memory problems but perform within normal limits on objective memory tests. A patient with cognitive impairment would more likely show consistent performance deficits across various tests assessing memory and other cognitive domains. In addition, the presence of other depressive symptoms (e.g., low mood, anhedonia, sleep disturbances) would point towards a depressive etiology. Finally, a thorough history and exploration of the onset and course of symptoms are vital.
A careful examination of the patient’s history, reported symptoms, and objective neuropsychological findings is crucial in making a differential diagnosis, often requiring multiple sessions and possibly collaboration with other healthcare professionals.
Q 7. How do you account for premorbid functioning in your assessments?
Accurating for premorbid functioning—that is, the level of cognitive functioning before the onset of illness or injury—is crucial for accurate interpretation of neuropsychological test results. We aim to determine the individual’s baseline cognitive abilities to compare them to their current performance. Several methods exist: Demographic estimates use variables like education and occupation to estimate premorbid IQ. Holden’s method and other similar methods incorporate information about education, age, and current cognitive status to predict premorbid IQ. Using standardized tests specifically designed to estimate premorbid abilities, such as the National Adult Reading Test (NART), is crucial. The NART is a relatively insensitive to brain injury or dementia. By comparing the estimated premorbid abilities to the current test results, we can determine the extent of cognitive decline or impairment. It’s important to note that no method perfectly determines premorbid functioning, and these estimates should be considered within the context of the entire assessment.
For instance, if a patient scores lower than their estimated premorbid IQ on tests assessing memory but performs normally on tasks assessing executive function and vocabulary, it can help to focus on the specific memory deficits and possible causes.
Q 8. Explain the concept of malingering and how you would assess for it.
Malingering refers to the intentional fabrication or exaggeration of symptoms for external gain, such as avoiding work, obtaining disability benefits, or influencing legal proceedings. It’s a crucial consideration in neuropsychological evaluations because it can significantly distort the results and lead to inaccurate diagnoses and treatment plans.
Assessing for malingering involves a multifaceted approach. I employ a combination of strategies, including:
- Review of collateral information: Discrepancies between the patient’s self-report and information from family members, medical records, or other sources can be red flags. For instance, a patient reporting severe memory problems might be observed by family members to function normally in daily life.
- Use of validity tests: These are specifically designed to detect inconsistent or exaggerated responses. Examples include the Test of Memory Malingering (TOMM) and the Reliable Digit Span (RDS). These tests assess performance on tasks that are relatively easy for someone without cognitive impairment, and poor performance despite ease suggests intentional underperformance.
- Careful observation of the patient’s behavior: Inconsistencies between reported symptoms and observed behavior during testing can be indicative of malingering. For example, a patient claiming severe fatigue might show high levels of energy and engagement during the evaluation.
- In-depth interview: A thorough interview exploring the patient’s history, presenting symptoms, and motivations for seeking evaluation can often uncover inconsistencies or suggestive patterns.
It’s important to note that a low score on a validity test doesn’t automatically confirm malingering; it warrants further investigation. The interpretation of validity test scores must always be considered within the context of the overall clinical picture.
Q 9. What are the ethical considerations involved in conducting a neuropsychological evaluation?
Ethical considerations in neuropsychological evaluation are paramount. My practice adheres strictly to the guidelines set by professional organizations like the American Psychological Association (APA). Key ethical considerations include:
- Confidentiality: Maintaining the privacy of patient information is crucial. I ensure all information shared during the evaluation is kept confidential, unless legally required to disclose it.
- Informed consent: Before starting any evaluation, I obtain informed consent from the patient (or their legal guardian) ensuring they understand the purpose, procedures, risks, and benefits of the assessment. This includes explaining the potential limitations of the testing and the confidentiality aspects.
- Competence: I only undertake evaluations for which I have the necessary training and experience. If a case requires specialized expertise, I will refer the patient to a qualified colleague.
- Objectivity: Maintaining objectivity and avoiding bias in the evaluation process is critical. I strive to interpret test data impartially, considering all relevant information and avoiding personal opinions or beliefs.
- Fairness: Ensuring fair and equitable access to neuropsychological services, irrespective of background or circumstances, is a fundamental ethical principle.
- Responsibility: Reporting the findings accurately and clearly, avoiding sensationalism or misinterpretations. I provide recommendations and ensure they are clinically appropriate and aligned with the patient’s best interest.
Ethical dilemmas can arise, for example, when there are conflicts of interest or pressure from external parties. In such situations, I prioritize the patient’s well-being and adhere to ethical guidelines to resolve any conflict.
Q 10. How do you communicate complex neuropsychological findings to patients and their families?
Communicating complex neuropsychological findings effectively requires sensitivity, patience, and clear communication skills. I tailor my approach to the patient’s and family’s understanding and emotional state.
My approach includes:
- Using plain language: I avoid technical jargon as much as possible, opting for simple, understandable terms. I use analogies and examples to illustrate complex concepts. For instance, instead of saying ‘executive dysfunction,’ I might explain it as ‘difficulty planning, organizing, and following through on tasks.’
- Visual aids: Graphs and charts can help illustrate test results in a more accessible way. I might use a profile of their cognitive strengths and weaknesses.
- Breaking down information into manageable chunks: I avoid overwhelming the patient and family with too much information at once. I present findings in stages and allow time for questions and clarification.
- Addressing emotions: I acknowledge the emotional impact of the findings, allowing space for the patient and family to process their feelings and concerns. I offer empathy and support.
- Collaboration: I involve the patient and family in the process, encouraging them to actively participate in understanding the results and developing a treatment plan. I answer all their questions honestly and patiently.
I usually schedule a follow-up appointment to review the report and answer further questions. I create written summaries that supplement the detailed report, ensuring everyone understands the key findings and recommendations.
Q 11. Describe your experience with different populations (e.g., pediatric, geriatric, traumatic brain injury).
My experience spans various populations, including pediatric, geriatric, and individuals with traumatic brain injury (TBI). Each population presents unique challenges and considerations.
- Pediatric neuropsychology: Working with children requires adapting assessment methods to their developmental level and using age-appropriate tests. It often involves collaboration with parents, teachers, and other professionals to gather a comprehensive understanding of the child’s functioning. I am experienced in evaluating learning disabilities, ADHD, and the impact of developmental disorders on cognitive abilities. A recent case involved a young child with suspected ADHD, where careful observation and parent-teacher interviews were crucial in forming a diagnosis.
- Geriatric neuropsychology: Assessing older adults requires sensitivity to age-related changes in cognitive functioning. It is important to differentiate age-related cognitive decline from neurological conditions such as dementia or Alzheimer’s disease. I use assessments sensitive to the normal changes that occur with aging and look for patterns indicative of disease. A recent case involved an older adult experiencing memory problems; by employing appropriate testing methods, we could distinguish age-related memory changes from early signs of Alzheimer’s disease.
- Traumatic brain injury (TBI): Evaluating individuals with TBI often requires attention to both cognitive and emotional sequelae of the injury. I utilize specific assessment methods to identify the presence and severity of cognitive deficits, and consider the impact of emotional and behavioral changes on daily living. A recent case involved a patient with a TBI and moderate cognitive impairment. Our evaluation identified their specific challenges, allowing the development of a tailored rehabilitation plan which targeted specific areas affected by the TBI.
I continually update my knowledge and skills to ensure I am proficient in the assessment and treatment of diverse populations.
Q 12. What are the limitations of neuropsychological testing?
Neuropsychological testing, while a valuable tool, has limitations. It’s crucial to understand these limitations to avoid misinterpretations.
- Test performance influenced by factors other than neurologic disease: Factors like motivation, anxiety, education, cultural background, and premorbid abilities can affect test scores. For example, anxiety could lead to underperformance even if there is no underlying neurological impairment.
- Tests are not direct measures of brain function: They infer brain function based on observed performance. The test results provide insights into cognitive functioning, but do not directly image the brain.
- Limited sensitivity and specificity: Some tests may not be sensitive enough to detect subtle cognitive impairments or specific to certain neurological conditions. A negative result might not rule out a condition, and a positive result doesn’t always indicate a specific cause.
- Subjectivity in interpretation: While striving for objectivity, there is always some degree of professional judgment involved in interpreting test results and formulating conclusions. This subjectivity means that there is room for interpretation that might differ between professionals.
- Cultural bias: Tests may be culturally biased and may not accurately reflect the cognitive abilities of individuals from diverse cultural backgrounds. Therefore, using culturally-sensitive assessments and interpreting results cautiously are critical.
To address these limitations, I incorporate multiple sources of information, carefully consider individual factors, and use clinical judgment to integrate the data into a comprehensive assessment.
Q 13. How do you integrate information from different sources (e.g., medical records, collateral information) into your assessment?
Integrating information from multiple sources is vital for a comprehensive and accurate neuropsychological assessment. It allows me to build a holistic picture of the patient’s functioning and potential cognitive deficits.
My approach includes:
- Medical records review: This provides a detailed history of the patient’s medical conditions, treatments, and previous test results. It helps contextualize the neuropsychological findings and identify potential confounding factors.
- Collateral interviews: Gathering information from family members, caregivers, or other significant individuals can provide valuable insights into the patient’s daily functioning and behavioral changes, potentially detecting inconsistencies between self-reported symptoms and observed behaviors.
- Review of educational and occupational history: This provides insights into the patient’s premorbid abilities and academic or occupational achievements which helps to establish a baseline of cognitive functioning.
- Symptom checklists and rating scales: These instruments provide quantitative data on the patient’s subjective experience of symptoms and can help identify the severity and impact of cognitive difficulties. These are often paired with more formal testing measures.
I carefully analyze the information from these sources, looking for consistencies and inconsistencies that can inform my interpretation of the neuropsychological test results. This integrative approach helps me provide a more accurate and comprehensive assessment, which leads to more effective and personalized recommendations.
Q 14. Describe your experience with neuropsychological report writing.
Neuropsychological report writing is a crucial aspect of my practice. A well-written report communicates the findings clearly, concisely, and in a manner accessible to both medical professionals and the patient and their family. My reports typically follow a standard format including:
- Identifying information: Demographic details about the patient and referral source.
- Reason for referral: A clear statement of the questions the evaluation aims to answer.
- History: A summary of the patient’s medical, social, and developmental history; this section includes relevant details from medical records and collateral information.
- Behavioral observations: Documentation of the patient’s behavior during the testing process.
- Test results: A detailed description of the tests administered and the patient’s performance on each, including numerical scores and qualitative observations.
- Interpretation and integration: A synthesis of the findings from various sources, addressing the referral questions and offering a clinical interpretation of the results.
- Summary and conclusions: A concise summary of the key findings and diagnostic impressions.
- Recommendations: Specific, actionable recommendations for treatment, rehabilitation, or further assessment, including referrals to appropriate professionals.
I strive to write clear, concise reports using plain language and avoiding jargon whenever possible. I provide the reports in a timely manner, ensuring clarity and accessibility to all parties involved. The format enables easy understanding of the findings, facilitating informed decision-making for treatment and care planning.
Q 15. How do you stay current with the latest research and developments in neuropsychology?
Staying current in the rapidly evolving field of neuropsychology requires a multifaceted approach. I regularly read peer-reviewed journals like the Journal of the International Neuropsychological Society and Neuropsychology, attending conferences such as the annual meeting of the American Academy of Clinical Neuropsychology (AACN). Participation in professional organizations like the AACN provides access to continuing education opportunities and networking with leading experts. I also actively seek out and critically evaluate new research published online, through platforms such as PubMed and Google Scholar. Finally, I maintain a network of colleagues with whom I regularly discuss new findings and clinical challenges, fostering a collaborative learning environment.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What is your approach to case management and collaboration with other healthcare professionals?
My approach to case management is highly collaborative and patient-centered. I believe in a holistic model, integrating information from various sources. This starts with a thorough initial evaluation, incorporating relevant historical data and collateral information from family members or caregivers. I then actively consult with other healthcare professionals – neurologists, psychiatrists, primary care physicians, therapists – to obtain a comprehensive understanding of the patient’s condition and treatment trajectory. We discuss findings, treatment options, and goals in regular team meetings. My communication is clear, concise, and readily accessible to all involved, ensuring we’re all on the same page regarding the patient’s best interests. This multidisciplinary approach leads to more effective and tailored interventions.
Q 17. Explain the difference between a cognitive impairment and a cognitive disorder.
While often used interchangeably, ‘cognitive impairment’ and ‘cognitive disorder’ are distinct concepts. Cognitive impairment refers to a decline in one or more cognitive domains – such as memory, attention, or executive function – below what is expected for an individual’s age and education. It’s a broader term encompassing a range of severity, from mild, transient difficulties to more significant deficits. Cognitive disorder, conversely, represents a clinically significant decline in cognitive function that interferes with daily life, causing impairment in social or occupational functioning. It’s a more serious condition that meets specific diagnostic criteria, such as those outlined in the DSM-5 or ICD-11. For instance, a person might experience mild cognitive impairment in memory but not meet the criteria for a cognitive disorder like Alzheimer’s disease until the impairment significantly affects their ability to manage their finances or remember appointments.
Q 18. What are some common causes of cognitive decline?
Cognitive decline has diverse etiologies. Neurodegenerative diseases like Alzheimer’s disease, Parkinson’s disease, and frontotemporal dementia are major culprits. Vascular causes, such as stroke or multiple small vessel disease, can disrupt blood flow to the brain, impacting cognitive function. Traumatic brain injury (TBI), resulting from accidents or physical trauma, can lead to lasting cognitive impairments. Infections, like encephalitis or meningitis, can cause brain inflammation and cognitive deficits. Substance abuse, particularly long-term alcohol misuse, significantly contributes to cognitive decline. Finally, certain genetic conditions predispose individuals to earlier-onset cognitive decline. It’s crucial to note that often, cognitive decline is multifactorial, involving a combination of these factors.
Q 19. How do you assess for aphasia and what are the different types?
Aphasia is a language disorder affecting the ability to communicate. Assessment involves a comprehensive evaluation of spoken and written language skills. This includes assessing fluency (how easily words flow), comprehension (understanding spoken and written language), repetition (repeating phrases), naming (finding words for objects), and reading and writing abilities. Various standardized tests are used, such as the Boston Diagnostic Aphasia Examination (BDAE) and the Western Aphasia Battery (WAB). The types of aphasia are numerous and vary based on the brain region affected. For example, Wernicke’s aphasia often involves fluent but nonsensical speech with poor comprehension, while Broca’s aphasia presents as nonfluent, effortful speech with relatively intact comprehension. Conduction aphasia is characterized by difficulty repeating words, while global aphasia involves severe impairments in all language modalities. Precise identification of the aphasia type is critical for tailoring appropriate intervention strategies.
Q 20. Describe the role of neuropsychological testing in dementia diagnosis.
Neuropsychological testing plays a vital role in dementia diagnosis, providing a detailed profile of cognitive strengths and weaknesses. Tests assess various cognitive domains including memory, attention, executive function, language, and visuospatial abilities. Standardized measures like the Mini-Mental State Examination (MMSE), Montreal Cognitive Assessment (MoCA), and more comprehensive neuropsychological batteries help differentiate dementia from other conditions mimicking cognitive decline. The patterns of cognitive impairment identified through testing can assist in differentiating various dementia subtypes (e.g., Alzheimer’s disease, vascular dementia, frontotemporal dementia), guiding differential diagnosis and treatment planning. For example, memory impairment is a hallmark of Alzheimer’s disease, while executive dysfunction might be more prominent in frontotemporal dementia. This detailed assessment allows clinicians to formulate a more accurate diagnosis and develop a tailored management plan.
Q 21. How do you approach the assessment of individuals with traumatic brain injury?
Assessing individuals with traumatic brain injury (TBI) requires a multifaceted approach considering the acute and chronic effects of the injury. The initial assessment focuses on the immediate physical and cognitive consequences, often involving bedside evaluations to assess consciousness level and orientation. As the patient stabilizes, more comprehensive neuropsychological testing is conducted. This examines a broad range of cognitive functions, including attention, memory, executive functions, processing speed, and language. The assessment also considers the impact on adaptive functioning, such as daily living skills and social interaction, using standardized measures like the Galveston Orientation and Amnesia Test (GOAT) or the Scales of Cognitive Ability for Traumatic Brain Injury (SCATBI). Furthermore, assessment considers the pre-injury functioning to determine the severity of the deficits. This comprehensive evaluation provides a detailed picture of the cognitive impairments caused by the TBI, informing rehabilitation planning and predicting prognosis.
Q 22. Explain your experience with various neuropsychological software and databases.
Throughout my career, I’ve extensively utilized a range of neuropsychological software and databases. This includes popular assessment platforms like CogState, which offers computerized cognitive tests for efficient screening and monitoring, and ImPACT, a concussion management system providing baseline testing and post-injury evaluations. I’m also proficient with Test publishers’ online platforms (e.g., Pearson Assessments) for accessing and scoring standardized tests. Beyond individual software, I’m comfortable navigating large databases, such as those used for normative data comparisons. For example, I frequently reference databases containing extensive normative data for various cognitive tests, crucial for accurately interpreting individual patient results within the context of their age, education, and other demographic factors. My experience extends to managing and analyzing data from these systems, ensuring data integrity and appropriate utilization for clinical decision-making. This includes generating comprehensive reports that clearly communicate test findings to referring physicians and other healthcare professionals.
Q 23. Discuss your familiarity with different theoretical models of cognitive functioning.
My understanding of cognitive functioning is grounded in several theoretical models. I frequently utilize the Luria-Nebraska model, which emphasizes the localization of cognitive functions within specific brain regions. This model provides a valuable framework for understanding the neuroanatomical basis of cognitive deficits. I also incorporate aspects of the information processing model, which focuses on the stages of cognitive processing, allowing for a more detailed analysis of cognitive strengths and weaknesses. For example, understanding how attention, working memory, and executive functions interact is critical in assessing complex cognitive tasks. Additionally, I consider the connectionist model, acknowledging the distributed and interconnected nature of cognitive processes. This holistic approach allows for a more nuanced interpretation of test results and better informs recommendations for treatment and rehabilitation. In practice, I often integrate these models, adapting my approach based on the individual patient’s presentation and the specific clinical questions at hand.
Q 24. How do you handle situations where test results are inconsistent with clinical observations?
Inconsistencies between test results and clinical observations are a common challenge in neuropsychology. My approach involves a systematic investigation to resolve these discrepancies. First, I meticulously review the test administration and scoring procedures to rule out any methodological errors. Next, I explore potential contributing factors such as patient effort, symptom fluctuation (especially relevant in conditions like depression or anxiety), or the impact of medication. For example, a patient might underperform on a test due to fatigue or anxiety, which would be reflected in their clinical interview. I’d then consider alternative explanations for the findings. This might involve conducting additional assessments or consulting other professionals, such as psychiatrists or primary care physicians, for a more comprehensive understanding. Ultimately, the goal is to arrive at a well-supported interpretation that integrates all available information, and if necessary, modify the initial interpretation.
Q 25. Describe your experience working with diverse populations and cultural considerations.
I have extensive experience working with diverse populations, and I am acutely aware of the importance of cultural considerations in neuropsychological assessment. This includes understanding how cultural background can influence performance on neuropsychological tests. For example, certain tests may rely on cultural knowledge or specific linguistic skills, potentially leading to biased results if not carefully considered. I employ culturally sensitive assessment strategies and interpret findings within the context of the individual’s cultural background and experiences. This may involve selecting culturally appropriate test materials or adapting testing procedures as needed. Furthermore, I make sure to establish rapport and trust with patients from all backgrounds, creating a comfortable and inclusive testing environment. It is essential to consider cultural factors in diagnosis, treatment recommendations, and communication with families.
Q 26. What are your strengths and weaknesses as a neuropsychologist?
My strengths lie in my ability to integrate complex information from multiple sources, developing comprehensive and nuanced interpretations of neuropsychological data. I pride myself on my strong clinical judgment and my ability to build strong therapeutic relationships with patients, fostering trust and collaboration. I’m also highly organized and detail-oriented, ensuring the accuracy and reliability of my assessments. However, like any professional, I have areas for ongoing development. I strive to constantly update my knowledge of the latest research and advancements in neuropsychology. In terms of time management, I recognize the importance of prioritizing tasks effectively, ensuring sufficient time for each aspect of assessment and report writing.
Q 27. Where do you see yourself in 5 years in the field of neuropsychology?
In five years, I envision myself as a leading expert in my field, potentially specializing in a specific area such as traumatic brain injury or neurodegenerative diseases. I aspire to further develop my expertise in research and contribute to the advancement of neuropsychological knowledge through publications and presentations. I also hope to mentor other neuropsychologists and contribute to the training of future professionals. This includes taking on a supervisory role within a clinical setting and engaging in more collaborative research initiatives.
Q 28. Describe a challenging case and how you successfully navigated it.
One particularly challenging case involved a young adult who presented with persistent cognitive difficulties following a mild traumatic brain injury. Initial testing revealed inconsistent findings, with some tests suggesting significant impairments and others showing relatively normal performance. The patient also reported significant emotional distress and anxiety. To address this, I broadened the assessment to include measures of emotional functioning and conducted a more in-depth clinical interview to explore potential psychological factors contributing to their symptoms. This revealed significant anxiety and post-traumatic stress, significantly impacting their cognitive performance. The case highlighted the importance of considering psychological factors in conjunction with neuropsychological findings. By integrating the results of the expanded assessment and coordinating care with a psychiatrist specializing in trauma, we developed a comprehensive treatment plan addressing both cognitive and emotional difficulties. The patient showed significant improvement in both areas following a targeted treatment plan.
Key Topics to Learn for Neuropsychological Evaluation Interview
- Neuropsychological Assessment Instruments: Understand the principles, administration, scoring, and interpretation of common tests like the Wechsler scales, Bender-Gestalt, and Trail Making Test. Consider the strengths and limitations of each.
- Cognitive Domains: Develop a strong understanding of the key cognitive domains assessed (attention, memory, executive functions, language, visuospatial skills) and how they interrelate. Be prepared to discuss how specific deficits might manifest in daily life.
- Neuroanatomy and Neuropsychology: Connect brain regions to cognitive functions. Be able to discuss how lesions or damage in specific areas might impact performance on neuropsychological tests.
- Differential Diagnosis: Practice differentiating between various neurological and psychiatric conditions based on neuropsychological test findings. Understand the limitations of neuropsychological testing in making definitive diagnoses.
- Report Writing and Interpretation: Familiarize yourself with the structure and content of a comprehensive neuropsychological report. Practice interpreting test results and translating them into clinically meaningful summaries.
- Ethical Considerations: Understand the ethical implications of neuropsychological assessment, including confidentiality, informed consent, and cultural sensitivity. Be prepared to discuss potential biases and limitations.
- Practical Applications: Be ready to discuss how neuropsychological evaluations inform treatment planning, rehabilitation, and legal contexts (e.g., personal injury cases).
- Case Conceptualization: Practice integrating information from various sources (e.g., medical history, collateral information) to develop a comprehensive understanding of a patient’s cognitive strengths and weaknesses.
Next Steps
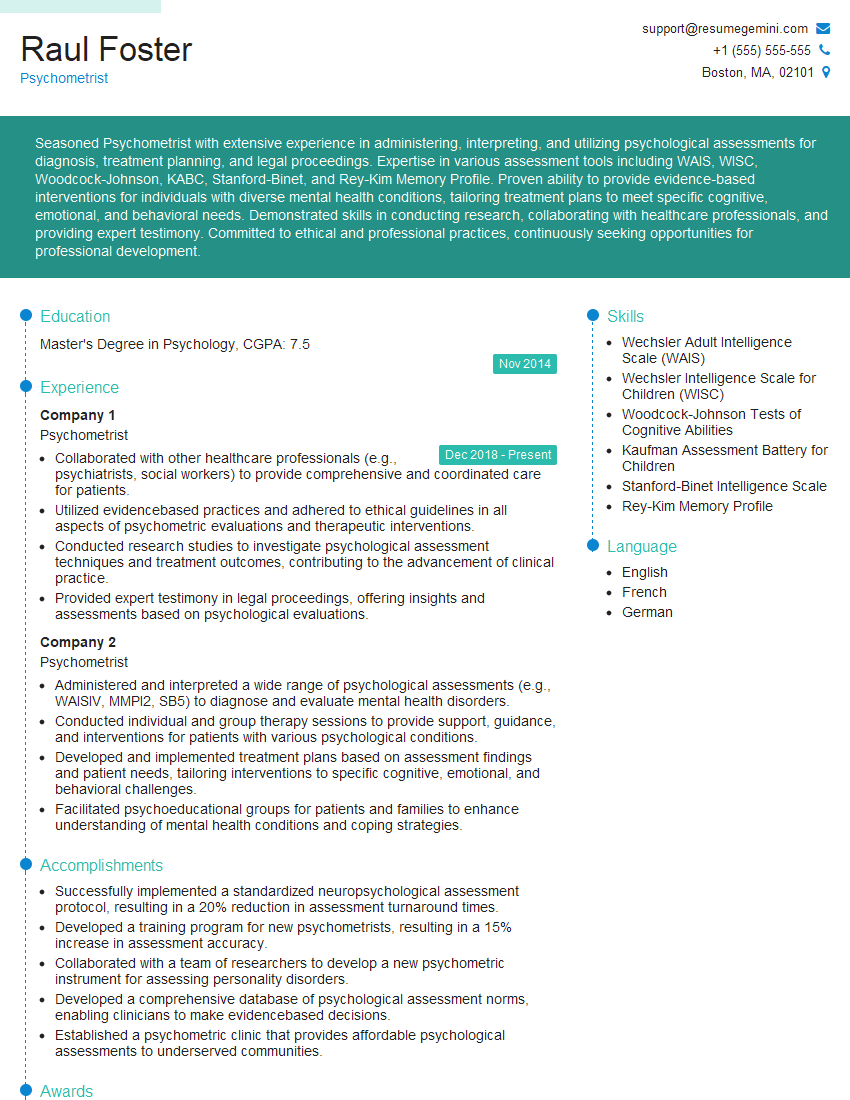
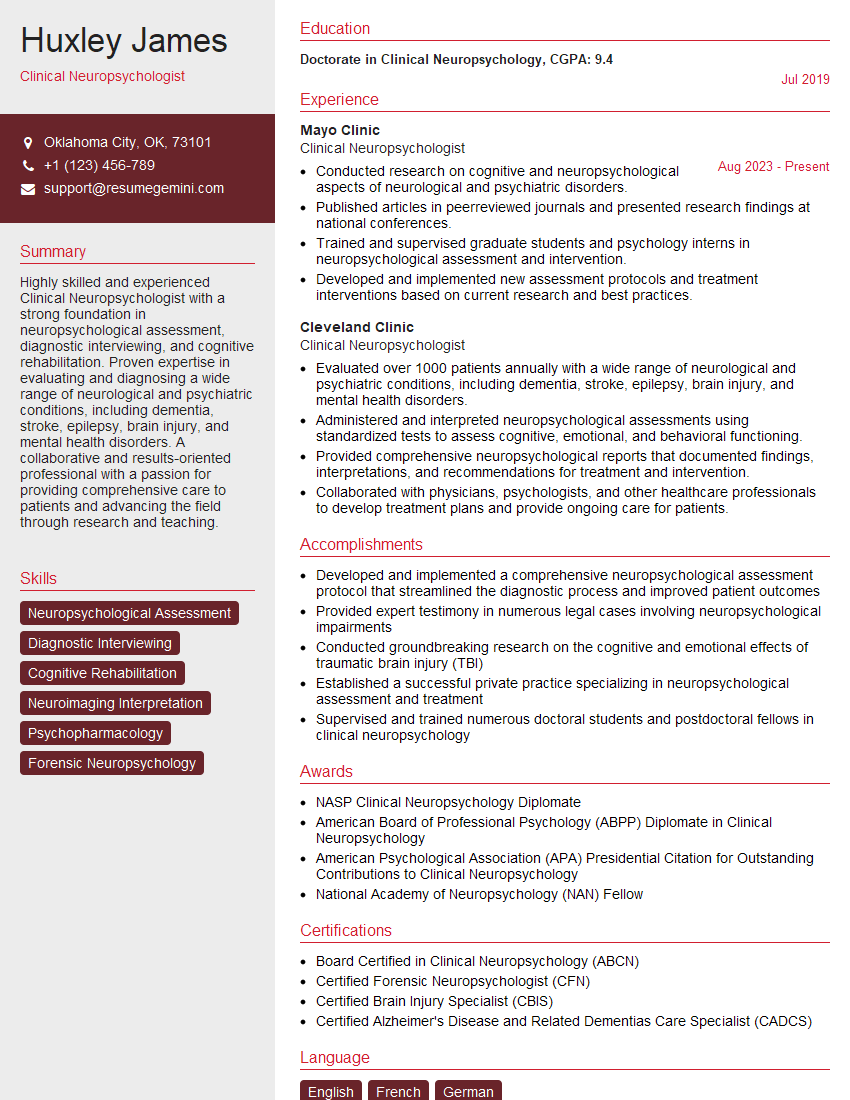
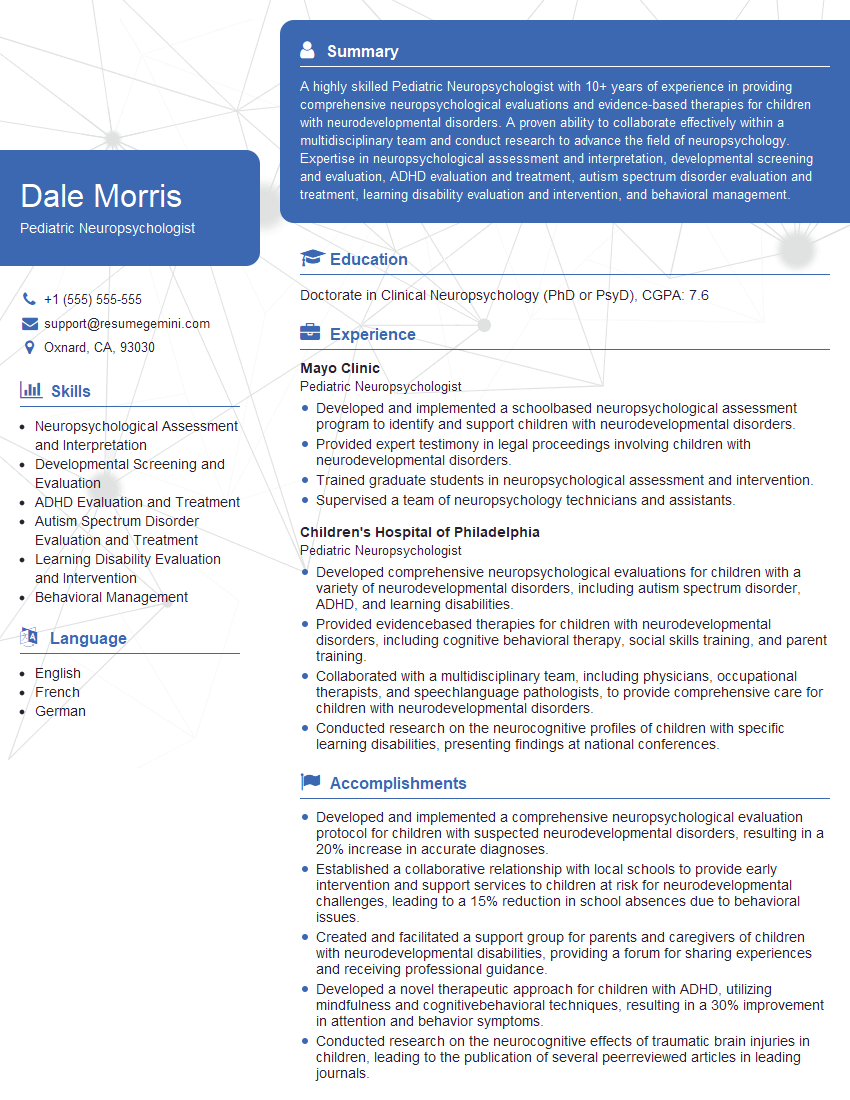
Mastering Neuropsychological Evaluation is crucial for career advancement in this specialized field. A strong understanding of these concepts will significantly enhance your interview performance and open doors to exciting opportunities. To maximize your job prospects, create a compelling and ATS-friendly resume that highlights your skills and experience. ResumeGemini is a trusted resource for building professional resumes, and we provide examples specifically tailored to Neuropsychological Evaluation to help you present yourself effectively to potential employers. Invest time in crafting a powerful resume – it’s your first impression!
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.