Cracking a skill-specific interview, like one for Assessment and Diagnosis of Child Psychopathology, requires understanding the nuances of the role. In this blog, we present the questions you’re most likely to encounter, along with insights into how to answer them effectively. Let’s ensure you’re ready to make a strong impression.
Questions Asked in Assessment and Diagnosis of Child Psychopathology Interview
Q 1. Describe the diagnostic criteria for Attention-Deficit/Hyperactivity Disorder (ADHD) according to the DSM-5.
The Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5) defines Attention-Deficit/Hyperactivity Disorder (ADHD) as a neurodevelopmental disorder characterized by inattention, hyperactivity, and impulsivity. To receive a diagnosis, a child must exhibit symptoms across multiple settings (e.g., school, home) and the symptoms must have begun before age 12. The DSM-5 specifies two symptom categories:
- Inattention: Symptoms like difficulty sustaining attention, lack of attention to detail, poor organization, forgetfulness, and difficulty following instructions.
- Hyperactivity/Impulsivity: Symptoms include excessive fidgeting, restlessness, interrupting others, difficulty waiting their turn, and excessive talking.
The diagnosis further requires that the symptoms interfere with the individual’s social, academic, or occupational functioning. The severity of ADHD is rated as mild, moderate, or severe, based on the number and impact of symptoms. For example, a child might be diagnosed with predominantly inattentive ADHD if they struggle significantly with focusing but don’t show excessive hyperactivity. A child with combined presentation will display significant symptoms of both inattention and hyperactivity/impulsivity. Accurate diagnosis requires careful observation across multiple settings and often involves input from teachers, parents, and other caregivers.
Q 2. Explain the difference between Oppositional Defiant Disorder (ODD) and Conduct Disorder (CD).
Oppositional Defiant Disorder (ODD) and Conduct Disorder (CD) are both disruptive behavior disorders, but they differ significantly in severity and the types of behaviors exhibited. ODD is characterized by a persistent pattern of angry/irritable mood, argumentative/defiant behavior, and vindictiveness. These behaviors are typically directed towards authority figures, such as parents or teachers. Think of a child frequently arguing, refusing to comply with requests, or deliberately annoying others. CD, on the other hand, involves more serious violations of the rights of others and societal norms. This includes aggression towards people or animals, destruction of property, deceitfulness or theft, and serious violations of rules. A child with CD might engage in bullying, stealing, or even acts of physical violence.
The key difference lies in the level of severity and the types of behaviors. ODD primarily involves defiant and argumentative behaviors, while CD involves more serious antisocial and aggressive actions. A child can have ODD without CD, but CD often follows a history of ODD. Imagine a child who initially displays ODD (arguing, defiance) who then escalates to more severe behaviors such as physical aggression towards peers (CD).
Q 3. What are the key features of Autism Spectrum Disorder (ASD)?
Autism Spectrum Disorder (ASD) is a neurodevelopmental disorder characterized by persistent deficits in social communication and social interaction across multiple contexts, as well as restricted, repetitive patterns of behavior, interests, or activities. These symptoms are usually present from early childhood, even if they are not fully manifested until social demands exceed the child’s limited capacities. The key features include:
- Social Communication and Interaction Deficits: Difficulty with social reciprocity, nonverbal communication (e.g., eye contact, body language), and developing and maintaining relationships.
- Restricted, Repetitive Patterns of Behavior, Interests, or Activities: This might involve repetitive motor movements (e.g., hand flapping), insistence on sameness, highly restricted, fixated interests, or unusual sensory sensitivities.
The severity of ASD is determined by the level of support needed for daily functioning. Some individuals with ASD may require significant support, while others may function relatively independently. It’s crucial to remember that ASD is a spectrum, meaning that symptoms and their severity vary widely among individuals. For example, one child might primarily struggle with social interaction, while another might exhibit strong repetitive behaviors.
Q 4. Discuss the assessment tools you would utilize to evaluate a child suspected of having anxiety disorder.
Assessing a child suspected of having an anxiety disorder requires a multi-method approach. I would utilize a combination of tools to gain a comprehensive understanding. This typically involves:
- Clinical Interviews: Structured or semi-structured interviews with the child and their parents or caregivers to gather detailed information about the child’s symptoms, developmental history, and family dynamics. The Anxiety Disorders Interview Schedule for DSM-5 (ADIS-5) is a widely used example.
- Self-Report Measures: Age-appropriate questionnaires completed by the child to assess their anxiety symptoms, such as the Screen for Child Anxiety Related Emotional Disorders (SCARED) or the Spence Children’s Anxiety Scale (SCAS).
- Parent/Teacher Report Measures: Questionnaires completed by parents and/or teachers providing their perspectives on the child’s behavior and symptoms. These provide valuable contextual information that may not be apparent during a clinical interview.
- Observation: Observing the child’s behavior in different settings (e.g., playroom, classroom) to assess their anxiety levels and coping mechanisms. This might involve direct observation or review of school records and other relevant documents.
The combination of these assessment tools provides a richer picture than relying on any single method. For instance, a child might underreport their anxiety during an interview, but a parent-report questionnaire might reveal the extent of their worries and avoidant behaviors. A comprehensive assessment allows for a more accurate diagnosis and informs the development of an effective treatment plan.
Q 5. How would you differentiate between depression and normal sadness in a child?
Differentiating between depression and normal sadness in a child can be challenging, but several key factors are crucial. Normal sadness is a temporary emotional state, typically triggered by a specific event (e.g., a disappointment or loss). It is usually short-lived and accompanied by other normal emotional responses. On the other hand, depression is a more persistent and pervasive mood disorder. It is characterized by a combination of symptoms that significantly impair the child’s functioning for several weeks or more.
Key differentiating factors include:
- Duration: Normal sadness is temporary, while depressive symptoms persist for an extended period (typically two weeks or more).
- Severity: Depressive symptoms are typically more intense and pervasive, interfering with daily life. This may include changes in sleep, appetite, weight, energy levels, concentration, and activity levels.
- Presence of other symptoms: Depression often involves additional symptoms such as feelings of worthlessness or excessive guilt, recurrent thoughts of death or suicide, anhedonia (loss of interest or pleasure), and psychomotor retardation or agitation.
- Impact on functioning: Depression significantly impacts a child’s academic performance, social interactions, and overall well-being, unlike normal sadness.
For example, a child feeling sad after losing a pet is different from a child who experiences persistent low mood, withdrawal from friends, loss of interest in activities, difficulty sleeping, and changes in appetite for weeks, significantly affecting their school performance. The latter is indicative of potential depression.
Q 6. What are the ethical considerations when assessing and diagnosing a child?
Ethical considerations are paramount when assessing and diagnosing a child. These include:
- Informed Consent/Assent: Obtaining informed consent from parents or legal guardians is crucial. For older children, obtaining assent (their agreement to participate) is also necessary. This involves explaining the assessment process, its purpose, and potential risks and benefits in a way they can understand.
- Confidentiality: Protecting the child’s privacy and confidentiality is vital, while also balancing the need to share relevant information with parents and other involved professionals when necessary. This involves clear communication about the limits of confidentiality.
- Cultural Competence: Recognizing and addressing cultural differences in behavior and symptom presentation is essential for avoiding misdiagnosis. This might involve considering the child’s cultural background, family beliefs, and practices.
- Avoiding Bias: Clinicians must remain objective and avoid biases based on the child’s gender, race, ethnicity, or socioeconomic status. Bias can lead to inaccurate assessments and inappropriate treatment recommendations.
- Beneficence and Non-maleficence: The assessment process should always benefit the child and avoid causing harm. This includes choosing appropriate assessment methods and interpreting results accurately.
- Justice: Ensuring that all children have access to fair and equitable assessment and treatment services, regardless of their background or circumstances.
For example, a clinician must be aware that some cultural groups might express distress differently than others, potentially leading to misinterpretations if not considered carefully. Similarly, clinicians should be mindful of potential biases that could affect their assessment of a child from a disadvantaged socioeconomic background.
Q 7. Explain the importance of considering cultural factors in child psychopathology assessments.
Cultural factors significantly influence the presentation, understanding, and interpretation of child psychopathology. Ignoring these factors can lead to misdiagnosis and ineffective treatment. For instance, certain behaviors might be considered normative within one culture but pathological in another. The expression of emotional distress also varies across cultures. Some cultures might encourage emotional restraint, while others might be more expressive.
Considering cultural factors involves:
- Understanding cultural norms: Familiarity with the child’s cultural background, including family structure, communication styles, and beliefs about mental health, is essential.
- Assessing symptom presentation within cultural context: Determining whether the child’s behaviors are consistent with cultural norms or indicative of a clinical disorder requires careful consideration.
- Using culturally sensitive assessment tools: Selecting assessment tools that are appropriate for the child’s cultural background and language is important. Some standardized measures might not be valid or reliable across different cultures.
- Collaborating with cultural experts: If needed, consult with experts in cultural psychiatry or community leaders to ensure that the assessment and diagnosis are culturally sensitive and accurate.
For example, a child from a culture that emphasizes obedience might exhibit passive-aggressive behaviors rather than openly defiant ones, potentially leading to a misdiagnosis of depression rather than ODD if cultural context is not carefully considered. Culturally sensitive assessment ensures that the child receives appropriate and effective care that respects their cultural background.
Q 8. Describe your approach to conducting a comprehensive psychological assessment of a child.
A comprehensive psychological assessment of a child is a multifaceted process aiming to understand their developmental trajectory, emotional state, behavioral patterns, and cognitive abilities. My approach involves a systematic integration of various methods to create a holistic picture. This begins with a thorough intake interview with the parents or caregivers to gather information about the child’s history, developmental milestones, current concerns, and family dynamics. This is followed by direct assessment of the child through clinical interviews tailored to their age and developmental level, utilizing age-appropriate language and techniques.
Next, I employ standardized psychological tests to assess cognitive functioning (e.g., WISC-V, Stanford-Binet), academic achievement (e.g., Woodcock-Johnson IV), and adaptive behavior (e.g., Vineland Adaptive Behavior Scales). Depending on the presenting concerns, I may also use projective techniques (with caution and interpretation informed by other data) and behavioral rating scales completed by parents and teachers. Finally, I often conduct behavioral observations, either in a structured setting or naturalistic observation to directly assess the child’s behavior in different contexts. The entire process is guided by ethical considerations, ensuring informed consent and confidentiality.
For example, with a child presenting with anxiety, I might use a combination of the Child Anxiety Sensitivity Index, direct clinical interview focused on their anxiety triggers and coping mechanisms, and behavioral observations during play therapy to assess their anxiety levels and response to different situations. The integration of all these data points allows for a more accurate and nuanced diagnosis and treatment plan.
Q 9. What are some common challenges encountered in the assessment of child psychopathology and how do you address them?
Assessing child psychopathology presents unique challenges. Children’s communication skills vary greatly depending on age and developmental stage, which can impact their ability to accurately report their internal experiences. For younger children, reliance on parental or teacher report becomes crucial, but this information can be biased or incomplete. Furthermore, children may be reluctant or unable to articulate complex emotions or thoughts. The presence of comorbid conditions, where multiple disorders coexist, further complicates diagnosis and treatment planning.
To address these challenges, I use a multi-method approach, incorporating multiple sources of information (parents, teachers, child) and various assessment methods. For example, if a child is nonverbal or has limited communication skills, I might rely heavily on observational data, play therapy, and parent/teacher reports. When dealing with comorbidity, a careful differential diagnosis process is essential, often involving consultation with other professionals.
Another significant challenge is the child’s developmental stage. What is considered normal behavior at age 5 might be problematic at age 10. Therefore, a thorough understanding of developmental norms is critical in interpreting assessment findings and ruling out developmental delays or variations.
Q 10. Discuss the role of parental involvement in the assessment and treatment process.
Parental involvement is paramount in the assessment and treatment of child psychopathology. Parents are the primary caregivers and often possess invaluable insights into the child’s behavior, developmental history, and family dynamics. Their perspective is essential for a comprehensive understanding of the child’s difficulties. Parents can provide crucial contextual information that may not be apparent during direct assessment with the child. Furthermore, their cooperation is vital for the successful implementation of any treatment plan.
I involve parents throughout the assessment process. This includes initial interviews to gather history, participation in behavioral observations (where appropriate), and feedback on assessment results. During treatment, parental collaboration is essential, especially with therapies such as parent-child interaction therapy (PCIT) or family therapy. However, it’s crucial to balance parental input with the child’s own perspectives and rights, particularly as the child matures.
For instance, a parent’s report of a child’s defiance might reveal a broader pattern of power struggles within the family. Understanding this context is crucial for developing an effective intervention that addresses both the child’s behavior and the family dynamics contributing to it.
Q 11. How do you interpret projective tests like the Rorschach or the Thematic Apperception Test (TAT) in children?
Projective tests like the Rorschach and TAT are used cautiously and in conjunction with other assessment methods in child assessment. These tests are not considered diagnostic tools on their own but rather as supplemental sources of information that can offer insights into a child’s unconscious thoughts, feelings, and perceptions. Interpretation is complex and requires considerable clinical experience and training.
With children, the interpretation focuses on understanding their developmental level and the context of their responses. For example, a child’s response to a Rorschach card might reveal their emotional state, their perception of relationships, and their coping mechanisms. The use of narrative and play-based projective techniques is often more beneficial with children than traditional methods, as it allows for more natural expression.
It’s important to note that interpretations should be anchored in other data from clinical interviews, behavioral observations, and standardized tests. These projective tests provide qualitative information that supplements quantitative data from other assessments, providing a more comprehensive understanding of the child’s emotional world. Over-reliance on projective tests in isolation is inappropriate and potentially misleading.
Q 12. Explain the use of behavioral observations in assessing a child’s behavior.
Behavioral observations involve systematically observing and recording a child’s behavior in different settings, such as a playroom, classroom, or home. This provides valuable information about the frequency, duration, intensity, and context of specific behaviors. The observations can be structured (using pre-defined checklists) or unstructured (observing freely and noting all behaviors). This technique allows for direct assessment of the child’s behavior, complementing self-report measures and parent/teacher reports, which can be subjective.
For example, observing a child’s interactions with peers during playtime might reveal patterns of aggression, social withdrawal, or prosocial behaviors. These observations can be crucial in identifying specific triggers and maintaining patterns of problem behaviors. The detailed nature of observational data helps to validate or challenge assumptions based on other assessment tools, leading to a more accurate diagnosis and treatment planning.
Ethical considerations are essential. Informed consent and respecting the child’s privacy must be prioritized. Involving parents and teachers, as appropriate, enhances the accuracy and applicability of observations.
Q 13. What are the limitations of standardized assessments in evaluating child psychopathology?
While standardized assessments offer valuable quantitative data and normative comparisons, they have limitations in evaluating child psychopathology. Firstly, they may not capture the nuances of individual experiences and cultural contexts. A standardized test score doesn’t tell the whole story. Secondly, the rigid structure of standardized tests may not be suitable for all children, particularly those with developmental delays or communication difficulties. Some children may struggle to engage with the tasks, leading to inaccurate or unreliable results.
Another limitation is the reliance on self-report or parent-report, which can be influenced by biases or inaccurate recall. Standardized tests may not adequately assess the complexity of human behavior, missing contextual factors that significantly impact a child’s functioning. For example, a standardized test may identify an intellectual disability, but a thorough assessment will need to explore the context of that disability to assess its impact and plan the best possible support. Finally, the focus on psychometric properties, such as reliability and validity, can sometimes overshadow the clinical relevance of findings. A perfectly reliable test may still not accurately reflect the child’s lived experience.
Q 14. Discuss the importance of utilizing a multi-method assessment approach.
A multi-method assessment approach is crucial in the evaluation of child psychopathology because it utilizes a variety of data sources and methods to obtain a comprehensive and holistic understanding. This approach reduces reliance on any single source of information, thereby mitigating the limitations of each individual method. It allows for triangulation of findings – where information from multiple sources converges – increasing the confidence in the diagnosis and treatment recommendations.
For instance, combining clinical interviews, standardized tests, behavioral observations, and parent/teacher reports creates a robust assessment that provides a richer understanding of the child’s strengths and challenges. This approach is particularly important when working with complex cases or when there are discrepancies between different sources of information. It allows the clinician to identify potential biases, limitations of specific methods, and develop a well-rounded understanding.
Imagine assessing a child for ADHD. A multi-method approach might involve parent and teacher rating scales (e.g., Conners’ Rating Scales), direct observation of the child’s behavior in a structured setting, cognitive testing to rule out other conditions, and a detailed clinical interview with the child and parents. By integrating all this data, a more accurate diagnosis and personalized treatment plan can be developed.
Q 15. How do you ensure confidentiality during the assessment and treatment process?
Confidentiality is paramount in child psychopathology. It’s not just a legal requirement; it’s ethically crucial for building trust and fostering open communication with the child and family. I adhere to strict confidentiality protocols throughout the assessment and treatment process, ensuring all information shared is protected. This includes:
- HIPAA compliance: I strictly follow the Health Insurance Portability and Accountability Act guidelines to protect Protected Health Information (PHI).
- Informed consent: Before any assessment begins, parents or legal guardians are provided with detailed information about the process, including how their child’s data will be stored and used. They must provide informed consent before we proceed.
- Secure record-keeping: All records are kept in locked cabinets and electronic files are password-protected and encrypted. Access is limited to authorized personnel only.
- Limited disclosure: I only disclose information to other professionals involved in the child’s care (e.g., therapists, educators) with explicit parental consent and only the information absolutely necessary for their involvement. I always prioritize the child’s best interests.
- Data anonymization: When presenting research or case studies, I always anonymize identifying information to protect the child’s privacy.
For example, I recently worked with a family where the child disclosed sensitive information during a session. I reassured the child of the confidentiality of our conversations and only shared relevant details with other professionals directly involved in their care with explicit parental permission, ensuring their privacy was maintained throughout.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Describe your approach to communicating diagnostic information to parents and caregivers.
Communicating diagnostic information requires sensitivity and careful consideration of the family’s emotional state. My approach is collaborative and focuses on shared understanding. I avoid technical jargon and instead use clear, age-appropriate language. I begin by acknowledging the family’s feelings and concerns, creating a safe space for questions and anxieties. The communication unfolds in stages:
- Summarize observations: I begin by summarizing my observations and findings in a non-judgmental way, highlighting the child’s strengths alongside challenges.
- Explain diagnosis clearly: I explain the diagnosis using plain language, avoiding overly technical terms. I provide concrete examples illustrating the diagnosis to enhance understanding.
- Discuss treatment options: I collaboratively discuss potential treatment options, weighing their pros and cons, and tailoring recommendations to the family’s needs and preferences. I involve the family in decision-making.
- Provide resources and support: I always provide families with relevant resources and support networks, including contact information for community organizations and support groups.
- Follow-up: I schedule a follow-up meeting to answer any questions that might arise after the initial discussion. This provides an opportunity to clarify any misunderstandings and reinforce support.
Imagine explaining an ADHD diagnosis. Instead of saying ‘attention-deficit/hyperactivity disorder,’ I might say something like, ‘It seems [child’s name] has difficulty focusing and staying still at times, which can make things challenging at school and home. We believe this is due to differences in how their brain processes information.’ This approach makes the information more accessible and less frightening.
Q 17. What is your preferred approach to collaboration with other professionals involved in the child’s care?
Collaboration is fundamental in child psychopathology. A multidisciplinary approach significantly enhances the effectiveness of interventions. I believe in a team-based approach centered on the child and family’s needs. My collaboration typically involves:
- Regular communication: Maintaining open and regular communication with other professionals, such as teachers, pediatricians, therapists, and social workers, via email, phone, or meetings. This ensures everyone is on the same page.
- Shared information: Sharing relevant assessment data and treatment plans with other professionals with parental consent, focusing on aspects directly relevant to their roles.
- Joint case planning: Participating in collaborative case planning meetings to coordinate interventions and ensure a consistent approach to the child’s care.
- Case conferences: Attending case conferences to discuss the child’s progress, challenges, and adjustments needed to the intervention plan.
- Respectful communication: Maintaining respectful communication and valuing the expertise of all professionals involved.
For example, in a case involving a child with behavioral challenges, I collaborated closely with the school psychologist and teacher to implement strategies in the classroom, ensuring consistency between home and school environments. This integrated approach significantly improved the child’s outcomes.
Q 18. How do you manage a situation where a child is reluctant to participate in the assessment?
Reluctance to participate in an assessment is common, particularly in children. My approach focuses on building rapport and creating a safe, comfortable environment. I prioritize the child’s feelings and adapt my techniques accordingly:
- Building rapport: I start by building a positive relationship with the child, using play therapy techniques, age-appropriate activities, and engaging conversation to create a comfortable atmosphere.
- Flexible assessment methods: I employ flexible assessment methods, such as play-based assessment or observation, instead of relying solely on structured interviews or tests.
- Involving the child: I involve the child in the process as much as possible, offering choices and control over the assessment. This gives them a sense of agency.
- Gradual approach: I might start with shorter assessment sessions, gradually increasing the duration as the child becomes more comfortable.
- Positive reinforcement: I use positive reinforcement and praise to encourage participation and build confidence.
- Collaboration with parents/guardians: I work closely with the parents or guardians to understand the child’s anxieties and develop strategies to address them.
For instance, if a child is hesitant to talk, I might start by engaging in a playful activity, gradually transitioning to conversation. If a child is resistant to structured tests, I might use observational methods instead.
Q 19. How would you address the potential for bias in your assessment process?
Bias can significantly impact the accuracy of assessments. Mitigating bias is crucial for ethical and effective practice. My approach involves:
- Self-reflection: Regularly reflecting on my own biases, cultural background, and personal experiences to identify potential sources of bias in my assessment process.
- Culturally sensitive assessment: Using culturally sensitive assessment tools and methods that are appropriate for the child’s background and experiences.
- Multiple assessment methods: Employing multiple assessment methods (e.g., interviews, observations, standardized tests) to obtain a comprehensive and multifaceted understanding of the child’s behavior and functioning.
- Seeking consultation: Consulting with colleagues or supervisors when I am unsure about how to interpret data or when I suspect my own bias might be influencing my judgments.
- Ongoing training: Actively engaging in ongoing training and professional development to learn about cultural competence, bias awareness, and best practices in assessment.
For example, I might be aware of my own biases regarding certain cultural practices and therefore actively seek to understand those practices and how they might influence a child’s behavior before making any judgments.
Q 20. What are the common developmental milestones and how would you assess delays?
Developmental milestones are age-related achievements in various domains (physical, cognitive, social-emotional, and language). Assessing delays involves comparing a child’s performance to established norms. Common milestones include:
- Physical: Gross motor skills (walking, running, jumping), fine motor skills (grasping, writing), and self-care skills (eating, dressing).
- Cognitive: Problem-solving, memory, attention, and language comprehension.
- Social-emotional: Emotional regulation, social interaction, and self-awareness.
- Language: Speech, understanding language, and communication.
I assess delays using a combination of methods:
- Developmental screening tools: Standardized screening tools such as the Ages and Stages Questionnaires (ASQ) or the Denver Developmental Screening Test (DDST) provide a quick overview of developmental progress.
- Parent interviews: Detailed interviews with parents or caregivers provide valuable insights into the child’s developmental history and current functioning.
- Observations: Direct observations of the child’s behavior in various settings (home, school, clinic) provide crucial information about their skills and challenges.
- Formal assessments: Depending on the suspected area of delay, formal psychological or developmental assessments may be necessary.
Any significant deviations from age-appropriate milestones would warrant further investigation and potential intervention.
Q 21. Discuss your understanding of trauma-informed care in child psychopathology.
Trauma-informed care acknowledges the pervasive impact of trauma on a child’s development and behavior. It recognizes that many mental health challenges in children stem from adverse childhood experiences (ACEs). It shifts the focus from what’s wrong with the child to understanding the impact of their experiences. Key principles include:
- Safety: Creating a safe and predictable environment where the child feels secure and protected.
- Trustworthiness and transparency: Building trust through open communication and clear expectations.
- Choice, collaboration, and empowerment: Involving the child and family in decision-making and empowering them to take control of their lives.
- Peer support: Utilizing peer support networks and creating opportunities for connection and support.
- Collaboration: Working collaboratively with other professionals, community agencies, and family members to ensure comprehensive support.
In practice, a trauma-informed approach might involve using calming techniques during assessment, avoiding triggering questions or activities, and validating the child’s feelings and experiences. It’s crucial to emphasize safety and control, allowing the child to set the pace of the assessment and creating a therapeutic alliance built on trust and respect.
Q 22. Describe your experience with different therapeutic interventions for children.
My experience encompasses a wide range of therapeutic interventions for children, tailored to their specific needs and diagnoses. I’ve extensively utilized evidence-based approaches like Cognitive Behavioral Therapy (CBT), Play Therapy, and Trauma-Focused Cognitive Behavioral Therapy (TF-CBT).
- CBT helps children identify and change negative thought patterns and behaviors. For example, I’ve worked with children experiencing anxiety, teaching them relaxation techniques and cognitive restructuring to challenge anxious thoughts.
- Play Therapy is invaluable for younger children who may struggle to articulate their feelings verbally. Through play, they can express emotions, process trauma, and develop coping mechanisms. I remember a case where a child experiencing significant parental separation used play to act out their feelings, leading to breakthroughs in understanding and processing their emotions.
- TF-CBT is specifically designed for children who have experienced trauma. It combines CBT principles with trauma-specific techniques to help children process their traumatic experiences and develop healthy coping skills. I’ve used this extensively with children who have experienced abuse or witnessed domestic violence.
Beyond these core modalities, I also incorporate elements of family therapy, parent training, and art therapy, depending on the individual child’s needs and family dynamics. The selection of interventions is always guided by a thorough assessment and a collaborative approach with the child, family, and other relevant professionals.
Q 23. How do you adapt your assessment and therapeutic approaches to different age groups?
Adapting my approach to different age groups is crucial. My methods change significantly based on a child’s developmental stage and cognitive abilities.
- Preschoolers (ages 3-5): With this age group, play therapy is often the primary method. I use toys, games, and creative activities to build rapport and understand their experiences. Communication is largely nonverbal, so keen observation is key.
- School-aged children (ages 6-12): This group benefits from a combination of play therapy and more structured CBT techniques. I can introduce cognitive restructuring exercises and behavioral experiments in age-appropriate ways, often using stories or games as illustrative tools.
- Adolescents (ages 13-18): Adolescents are more capable of abstract thinking and self-reflection. CBT, Dialectical Behavior Therapy (DBT), and other more verbally-oriented therapies are more effective. Building a strong therapeutic alliance built on trust and respect is paramount.
Regardless of age, I always prioritize creating a safe and supportive environment where children feel comfortable expressing themselves. I adjust my language, activities, and the overall therapeutic structure to be developmentally appropriate and engaging.
Q 24. Explain your understanding of evidence-based practices in child psychopathology.
Evidence-based practices are the cornerstone of my work. This means relying on research-supported methods and interventions that have demonstrated effectiveness in treating specific child psychopathologies. It’s not just about using the latest trendy therapies; it’s about selecting the most appropriate and effective approach based on the available scientific evidence.
For instance, when assessing a child for Attention-Deficit/Hyperactivity Disorder (ADHD), I rely on standardized diagnostic tools like the Conner’s Rating Scales and clinical interviews to gather comprehensive information, ensuring alignment with DSM-5 criteria. Similarly, when considering treatment, I would prioritize interventions like behavioral therapy and medication management, backed by robust research demonstrating their efficacy in ADHD management.
Staying updated on the latest research through professional development and peer-reviewed journals is crucial for maintaining competence in evidence-based practices. This ensures I’m providing the best possible care, informed by the most current scientific findings.
Q 25. Describe your experience with crisis intervention in a child mental health setting.
Crisis intervention in child mental health requires immediate action and a calm, reassuring approach. My experience includes working with children experiencing acute anxiety, suicidal ideation, self-harm, and severe emotional distress.
My approach involves first ensuring the child’s safety. This may involve contacting emergency services if there is an immediate risk of harm to self or others. Then, I focus on de-escalating the situation by creating a safe and predictable environment, using active listening and validation to help the child feel understood. I help them identify and express their feelings, providing coping strategies in the moment. Finally, I collaboratively develop a safety plan with the child and their family, including strategies for managing future crises.
One example involved a teenager experiencing a severe panic attack. I used grounding techniques, deep breathing exercises, and reassuring communication to help her calm down. We then collaboratively developed a plan to manage future anxiety episodes, which included identifying triggers and practicing coping skills.
Q 26. How do you prioritize cases involving children with immediate risk to self or others?
Cases involving immediate risk to self or others are always my top priority. My response follows a structured protocol emphasizing immediate safety and risk mitigation.
- Assessment of Immediacy: First, I conduct a thorough risk assessment to determine the level and immediacy of the danger. This involves careful consideration of the child’s statements, behaviors, and history.
- Safety Intervention: If the risk is immediate (e.g., active suicidal ideation, plans for self-harm or harming others), I immediately involve emergency services and/or child protective services to ensure the child’s safety.
- Collaboration: I work closely with the child’s family, school, and other relevant professionals to develop a comprehensive safety plan, ensuring continuous monitoring and support.
- Ongoing Monitoring: Following the acute crisis, I provide ongoing therapeutic intervention, focusing on addressing the underlying issues contributing to the risky behaviors. Regular follow-up is essential.
Ethical considerations and legal mandates dictate the swift and decisive action required in such cases, always prioritizing the child’s safety and well-being above all else.
Q 27. How would you document your assessment findings and recommendations?
Documentation is vital for providing comprehensive and ethical care. My documentation meticulously outlines every aspect of the assessment and intervention process.
My records include:
- Presenting Problem: A detailed description of the reason for referral and the presenting concerns.
- Developmental History: Information about the child’s developmental milestones, medical history, and family history.
- Behavioral Observations: Detailed observations of the child’s behavior during the assessment sessions.
- Assessment Results: A summary of the results from any standardized assessments used.
- Diagnosis: A clear and concise statement of the diagnostic impression based on the DSM-5 criteria.
- Treatment Plan: A detailed outline of the recommended treatment interventions, goals, and expected outcomes. This includes planned frequency of sessions, specific techniques, and measurable goals.
- Progress Notes: Regular updates documenting the child’s progress, any changes in the treatment plan, and any significant events or challenges.
All documentation adheres to HIPAA and other relevant legal and ethical guidelines, ensuring confidentiality and accuracy. Clear, concise, and objective language is always used.
Q 28. Describe a situation where you had to make a difficult clinical judgment regarding a child’s diagnosis.
One challenging case involved a young girl who presented with symptoms consistent with both Oppositional Defiant Disorder (ODD) and Conduct Disorder (CD). Differentiating between the two was crucial for guiding treatment.
While she exhibited significant defiance and irritability (consistent with ODD), she also engaged in serious acts of aggression and vandalism (more aligned with CD). I carefully reviewed her history, conducting multiple sessions with the child, parents, and teachers. I also utilized standardized assessments to objectively measure her behaviors.
After thorough evaluation, I concluded that her symptoms aligned more closely with ODD, given the absence of persistent and severe violations of societal norms typically seen in CD. However, her aggressive behaviors required focused intervention. This diagnosis guided the selection of therapy, focusing on parent training to address family dynamics and CBT to help manage anger and defiant behaviors. Regular monitoring and adjustments to the treatment plan were essential to address the evolving nature of her challenges.
Key Topics to Learn for Assessment and Diagnosis of Child Psychopathology Interview
- Developmental Psychopathology: Understanding typical and atypical child development, including milestones and risk factors across various developmental domains (cognitive, social-emotional, language).
- Diagnostic Classification Systems: Mastering the DSM-5 and ICD-11 criteria for childhood disorders, including differential diagnosis and comorbidity.
- Assessment Methods: Proficiency in various assessment techniques such as clinical interviews (child and parent), behavioral observations, standardized psychological tests (e.g., intelligence tests, projective tests, adaptive behavior scales), and neuropsychological assessments.
- Ethical Considerations: Understanding ethical principles in assessment and diagnosis, including informed consent, confidentiality, and cultural sensitivity.
- Case Conceptualization: Developing a comprehensive understanding of a child’s presenting problem by integrating information from multiple sources to formulate a coherent explanation and treatment plan.
- Practical Application: Analyzing case studies, interpreting assessment data, and formulating diagnoses based on presented information. Consider the impact of cultural background and family dynamics.
- Treatment Planning and Intervention: Understanding different therapeutic approaches and selecting appropriate interventions based on diagnosis and individual needs. Discuss evidence-based practices.
- Working with Families and Caregivers: Understanding the role of family systems in child psychopathology and strategies for effective collaboration with parents and other caregivers.
Next Steps
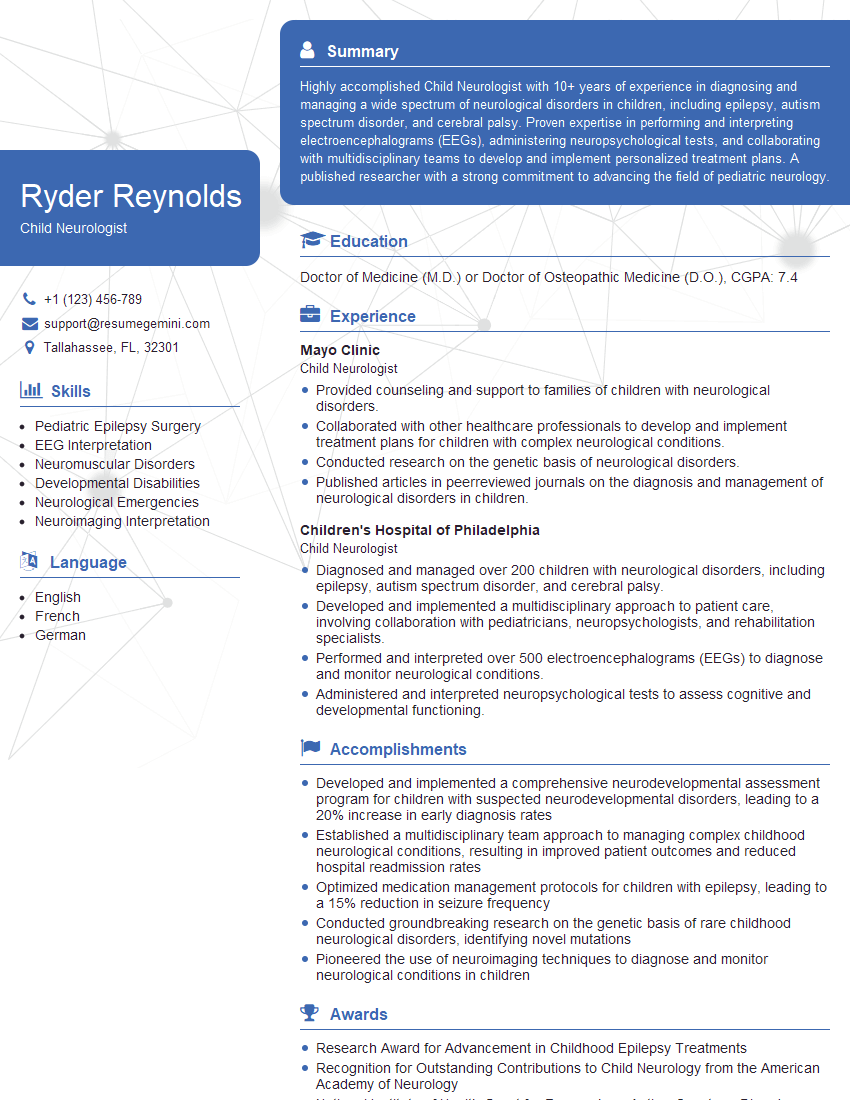
Mastering Assessment and Diagnosis of Child Psychopathology is crucial for career advancement in this specialized field. A strong understanding of these concepts will significantly enhance your credibility and marketability to potential employers. To maximize your job prospects, it’s essential to create an ATS-friendly resume that effectively showcases your skills and experience. We recommend leveraging ResumeGemini, a trusted resource, to build a compelling and professional resume. ResumeGemini provides examples of resumes tailored to Assessment and Diagnosis of Child Psychopathology to guide you through the process.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.