Unlock your full potential by mastering the most common Sinonasal Surgery interview questions. This blog offers a deep dive into the critical topics, ensuring you’re not only prepared to answer but to excel. With these insights, you’ll approach your interview with clarity and confidence.
Questions Asked in Sinonasal Surgery Interview
Q 1. Describe your experience with functional endoscopic sinus surgery (FESS).
Functional Endoscopic Sinus Surgery (FESS) is a minimally invasive surgical technique used to treat chronic sinusitis and other sinonasal disorders. Instead of large incisions, FESS utilizes a specialized endoscope and small instruments inserted through the nostrils to access and repair the sinuses. My experience with FESS spans over [Number] years, encompassing a wide range of cases from simple ethmoid sinusitis to complex revision surgeries involving skull base pathologies. I’ve performed hundreds of FESS procedures, constantly refining my technique to minimize complications and maximize patient outcomes. For example, I’ve found that using image-guidance technology, like navigation systems, significantly improves precision and reduces the need for extensive tissue removal. This leads to faster recovery times and reduced post-operative discomfort for my patients. I’m proficient in all aspects of FESS, from pre-operative planning and patient education to intraoperative techniques and post-operative care, ensuring a holistic and patient-centered approach.
A typical FESS procedure involves identifying and removing diseased tissue, such as polyps or inflammatory mucosa, while preserving healthy sinus structures. The surgeon uses specialized instruments to create smaller openings between the sinuses and nasal cavity, improving drainage and ventilation. The overall goal is to restore proper sinus function, alleviating symptoms such as nasal congestion, facial pressure, and post-nasal drip. I always tailor the procedure to the individual needs of the patient, considering factors like the extent of disease, anatomical variations, and patient comorbidities.
Q 2. Explain the different types of nasal polyps and their management.
Nasal polyps are benign, soft, teardrop-shaped masses that form in the sinuses and nasal cavity due to chronic inflammation. There are several types, primarily classified by their size, location, and the underlying cause. For example, we see inflammatory polyps frequently associated with chronic rhinosinusitis, asthma, and aspirin sensitivity. Another common type is antrochoanal polyps, which originate in the maxillary sinus and extend into the posterior nasal cavity. These can sometimes be quite large, potentially obstructing breathing. Their management depends largely on their size, symptoms, and the patient’s overall health. Small, asymptomatic polyps may require only close observation and medical management with nasal corticosteroids. Larger polyps or those causing significant symptoms typically necessitate surgical removal, often performed using FESS as mentioned earlier. In cases of recurrent polyposis, we may consider additional therapies, such as biologics, targeting the underlying inflammatory process.
In my practice, a thorough history and physical examination, along with imaging studies like CT scans, help to accurately classify and assess the severity of nasal polyps. Pre-operative planning often involves discussing the risks and benefits of different treatment options with the patient, ensuring informed consent and establishing realistic expectations. Post-operative care includes meticulous follow-up appointments and often continued medical management to prevent recurrence.
Q 3. How do you diagnose and treat sinusitis?
Sinusitis, or inflammation of the sinuses, is diagnosed based on a combination of clinical findings and imaging studies. Symptoms typically include facial pain or pressure, nasal congestion, headache, and decreased sense of smell. The duration of symptoms helps classify sinusitis as acute (less than 4 weeks), subacute (4-12 weeks), or chronic (greater than 12 weeks). I often utilize a detailed patient history, including allergy status and recent upper respiratory infections, to assist in diagnosis. Physical examination includes careful inspection of the nasal passages and palpation of the sinuses for tenderness.
Imaging plays a crucial role, primarily through CT scans which provide detailed anatomical information. CT scans allow us to visualize the extent of inflammation, the presence of polyps or other abnormalities, and to assess for complications like mucoceles or fungal sinusitis. Treatment strategies vary depending on the severity and duration of symptoms. Acute sinusitis often resolves spontaneously with supportive measures such as nasal saline irrigation, decongestants, and pain relievers. Chronic or recurrent sinusitis may necessitate medical therapy including nasal corticosteroids, antibiotics (in select cases), and sometimes FESS or balloon sinuplasty, which will be discussed later.
Q 4. What are the indications for balloon sinuplasty?
Balloon sinuplasty is a minimally invasive procedure used to improve sinus drainage and ventilation. It’s a less invasive alternative to FESS and is particularly well-suited for patients with chronic sinusitis who haven’t responded adequately to medical management. The procedure involves inserting a small balloon catheter into the sinus ostia (the natural openings of the sinuses). The balloon is then inflated to widen the ostia, creating a larger opening for improved drainage. This procedure is especially helpful in patients with smaller or more easily accessible sinus ostia. Patients with more extensive disease or anatomical variations might benefit more from FESS, providing the surgeon access to larger areas of inflammation.
Indications for balloon sinuplasty typically include chronic sinusitis that has not responded to medical therapy, minimal polyposis and anatomical changes, and a desire for a less invasive procedure with a potentially faster recovery time than FESS. However, it’s crucial to carefully select patients suitable for this approach. Pre-operative evaluation ensures that the patient’s sinus anatomy is suitable for the procedure and that there are no contraindications. It’s important to emphasize that balloon sinuplasty is not suitable for all cases of sinusitis.
Q 5. Discuss the surgical management of nasal septal deviation.
Nasal septal deviation refers to a displacement of the nasal septum, the cartilage and bone that divides the nasal cavity. This can cause nasal obstruction, difficulty breathing, and sometimes, sinusitis. Surgical correction, or septoplasty, is indicated when the deviation causes significant functional impairment or symptoms. My approach to septoplasty involves a thorough pre-operative assessment, including a detailed history and physical examination, along with nasal endoscopy and often, CT scan to evaluate the septal anatomy and any associated sinus pathology.
During the procedure, I aim to straighten the septum while preserving as much of the nasal structure as possible. I use a variety of techniques depending on the nature and severity of the deviation. Submucosal resection (SMR), for example, is frequently employed to remove deviated cartilage and bone from beneath the nasal lining. The goal is to create a straight, well-supported nasal septum, improving airflow and alleviating nasal obstruction. Post-operatively, careful monitoring of bleeding, swelling, and pain management is crucial. Nasal packing and splints are typically used to maintain the corrected septal position. I provide patients with detailed post-operative instructions to help ensure a smooth recovery.
Q 6. Explain your approach to managing epistaxis.
Epistaxis, or nosebleed, is a common problem with various causes ranging from minor trauma to serious underlying conditions. My approach to managing epistaxis is systematic and depends heavily on the severity and cause of the bleeding. For anterior bleeds, which are usually less severe and originate in the anterior part of the nose, simple measures are usually sufficient. This often involves direct pressure to the soft part of the nose, often using a cold compress, for at least 10-15 minutes. Nasal packing with various materials (gauze, absorbable materials, etc.) may be necessary to control more persistent bleeding.
Posterior epistaxis, originating from higher in the nasal cavity, is more serious and requires prompt and often more aggressive management. It might necessitate posterior nasal packing, balloon catheters, or even endovascular embolization. In cases where bleeding is severe or uncontrolled, I may recommend immediate referral to an otolaryngology emergency room or interventional radiology for advanced treatment. Identifying and treating the underlying cause, such as hypertension or coagulopathy, is also crucial to prevent recurrence. Patient education on preventative measures such as avoiding nose picking and maintaining adequate hydration is also part of my management strategy.
Q 7. Describe the imaging techniques used in sinonasal pathology.
Imaging plays a critical role in the diagnosis and management of sinonasal pathology. The most commonly used imaging technique is computed tomography (CT) scanning. CT scans provide high-resolution images of the bony structures and soft tissues of the sinuses and nasal cavity, enabling detailed visualization of anatomical variations, inflammatory changes, polyps, and other pathologies. This allows for precise pre-operative planning and post-operative assessment. I routinely use CT scans to evaluate the extent of sinusitis, the presence of polyps, the location and size of any tumors, and the status of the skull base.
Other imaging modalities may be used depending on the clinical scenario. Magnetic resonance imaging (MRI) can be helpful in evaluating certain soft tissue lesions and assessing for intracranial extension of disease. Ultrasound may be used for a quick initial assessment in some situations. The selection of imaging modality depends on the specific clinical question and the information needed to guide diagnosis and treatment planning. A careful correlation between imaging findings and clinical presentation is essential for accurate diagnosis and effective management.
Q 8. How do you differentiate between benign and malignant sinonasal tumors?
Differentiating between benign and malignant sinonasal tumors relies on a multi-faceted approach combining imaging, biopsy results, and clinical presentation. Benign tumors, like inverted papillomas or angiofibromas, typically grow slowly and have well-defined borders on imaging (CT or MRI). Their microscopic appearance (histology) shows orderly cellular growth without invasion into surrounding tissues. Malignant tumors, such as squamous cell carcinomas or adenocarcinomas, exhibit aggressive growth patterns, often with poorly defined borders on imaging. Histologically, they show disordered cellular growth, invasion into adjacent structures (bone, soft tissue), and potentially metastasis to lymph nodes or distant organs. For example, a slow-growing mass in the maxillary sinus seen on CT with a well-defined border and subsequently showing a benign histology on biopsy would be classified as benign. In contrast, a rapidly enlarging mass with bone destruction, irregular margins on imaging, and a malignant histology on biopsy is clearly malignant. The clinical presentation (e.g., persistent unilateral nasal obstruction, epistaxis, facial pain) can also provide clues, but definitive diagnosis relies heavily on the biopsy and imaging.
Q 9. What are the complications associated with FESS?
Functional endoscopic sinus surgery (FESS) is generally a safe procedure, but complications can occur. These range from minor to life-threatening. Minor complications include bleeding, postoperative pain, nasal crusting, and temporary anosmia (loss of smell). More significant complications are less frequent but include orbital injury (damage to the eye or its surrounding structures), cerebrospinal fluid (CSF) rhinorrhea (leakage of CSF into the nasal cavity), intracranial complications (rare, but potentially life-threatening such as meningitis or brain abscess), and perforation of the nasal septum. The risk of these complications is influenced by factors such as surgeon experience, patient anatomy, and the complexity of the surgery. Proper preoperative planning, meticulous surgical technique, and close postoperative monitoring are crucial in minimizing these risks. For example, meticulous dissection around the lamina papyracea (thin bone separating the orbit from the ethmoid sinus) is essential to prevent orbital injury. Similarly, careful attention to the skull base during surgery is vital to prevent CSF rhinorrhea.
Q 10. Explain your understanding of the anatomy of the paranasal sinuses.
The paranasal sinuses are air-filled cavities within the bones of the skull surrounding the nasal cavity. They are lined with respiratory mucosa and contribute to humidification and warming of inspired air, as well as voice resonance. The major sinuses include the maxillary sinuses (largest, located in the maxillary bones), frontal sinuses (located in the frontal bone), ethmoid sinuses (a complex group of small air cells between the eyes), and sphenoid sinuses (located in the sphenoid bone behind the ethmoid sinuses). The ostiomeatal complex (OMC) is a critical anatomical region where the drainage pathways of the frontal, anterior ethmoid, and maxillary sinuses converge. Obstruction of the OMC is a major factor in the development of chronic rhinosinusitis. Understanding this complex anatomy is paramount in functional endoscopic sinus surgery to ensure effective drainage and aeration of the sinuses. Think of it like a system of interconnected pipes; a blockage in one area can affect the entire system. Detailed knowledge of anatomical variations is crucial for safe and effective surgery.
Q 11. Discuss the management of CSF rhinorrhea.
Management of CSF rhinorrhea depends on the severity and location of the leak. Conservative management with bed rest, head elevation, and lumbar drainage may suffice for small, self-limiting leaks. However, most cases require surgical repair. The goal of surgery is to identify and seal the defect in the skull base. Techniques include endoscopic repair (using small incisions and endoscopes), craniofacial surgery (involving a larger incision and direct visualization of the skull base), or a combined approach. The choice of surgical approach depends on the location and size of the leak, as well as the patient’s overall health. Postoperatively, close monitoring for meningitis is crucial. Failure to repair can lead to recurrent meningitis or other intracranial infections, highlighting the critical need for prompt and appropriate intervention. A patient presenting with clear rhinorrhea following trauma would immediately raise suspicion for CSF rhinorrhea, and a proper diagnostic workup (including beta-2 transferrin testing of the fluid) would be essential before proceeding with management.
Q 12. How do you approach a patient with chronic rhinosinusitis?
Managing chronic rhinosinusitis (CRS) is a stepwise process beginning with a thorough history and examination. This includes assessing the duration and severity of symptoms (nasal congestion, rhinorrhea, facial pressure, loss of smell), along with identifying any potential contributing factors (allergies, nasal polyps, anatomical abnormalities). Initial management typically focuses on medical therapy, including nasal saline irrigation, topical corticosteroids, and oral decongestants. If medical management fails, imaging (CT scan) is often obtained to assess the extent of sinonasal disease and identify anatomical abnormalities. If significant disease is present and medical therapy is ineffective, FESS might be considered. For patients with nasal polyposis, biologic therapies may also be considered. The approach is tailored to the individual patient based on their specific symptoms, response to medical therapy, and presence of anatomical abnormalities. For instance, a patient with mild CRS and good response to medical therapy may continue with medical management alone, while a patient with severe CRS and significant anatomical abnormalities might require surgical intervention.
Q 13. What is your experience with image-guided surgery in sinonasal procedures?
Image-guided surgery has revolutionized sinonasal surgery, improving precision and minimizing complications. Navigation systems using CT or MRI scans allow surgeons to visualize the intricate anatomy in three dimensions, providing real-time guidance during the procedure. This is especially beneficial in complex cases involving close proximity to critical structures like the orbit, skull base, and intracranial contents. Image-guidance helps to avoid unintentional injury to these structures and improve the completeness of surgical resection. It’s particularly useful in revision sinus surgery where previous scarring and anatomical distortion can make standard endoscopic surgery challenging. For example, during resection of a tumor adjacent to the orbit, image guidance helps to define the tumor margins precisely while ensuring minimal risk to the eye. In my experience, image-guided surgery offers a significant advantage over traditional approaches in terms of safety and surgical accuracy.
Q 14. Describe your experience with revision sinus surgery.
Revision sinus surgery is significantly more challenging than primary surgery due to scar tissue, anatomical distortion, and potential inflammation from previous procedures. Preoperative planning is crucial, typically involving a thorough review of previous operative reports, imaging studies, and the patient’s clinical presentation. Careful attention must be paid to identifying the areas of persistent disease and planning the surgical approach to minimize further complications. Image-guided surgery and the use of advanced surgical tools are often essential in these cases. The presence of significant scarring and fibrosis can make dissection difficult and increase the risk of complications. Therefore, meticulous surgical technique, extensive knowledge of anatomy and pathology, and a high level of surgical skill are necessary to achieve successful outcomes. The approach is always tailored to the individual patient’s history and specific anatomical findings. For example, a patient with recurrent polyposis and significant scarring may require a more extensive procedure than a patient with recurrent infection and minimal scarring.
Q 15. Explain the principles of nasal airway reconstruction.
Nasal airway reconstruction aims to restore proper airflow through the nose. This often involves addressing structural issues like deviated septums, nasal valve collapse, or turbinate hypertrophy. The principles revolve around restoring the framework of the nose, improving airflow dynamics, and minimizing turbulence.
For example, a deviated septum, a common cause of nasal obstruction, can be corrected surgically using septoplasty. This procedure straightens the septum, allowing for better airflow. In cases of nasal valve collapse, techniques like spreader grafts or batten grafts are used to support the weakened cartilage, preventing collapse and improving airflow. Turbinate reduction, either through surgical resection or radiofrequency ablation, can decrease the size of enlarged turbinates, reducing obstruction. The goal is always to create a wide, straight airway, with minimal resistance to air flow. Careful assessment of the nasal anatomy, using both clinical examination and imaging like CT scans, is crucial for successful reconstruction.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you manage orbital complications of sinusitis?
Orbital complications of sinusitis, such as orbital cellulitis or subperiosteal abscess, are serious and require urgent intervention. The management depends on the severity. Mild cases of preseptal cellulitis, characterized by eyelid swelling and erythema without proptosis or visual changes, may be managed with intravenous antibiotics. However, more severe cases requiring hospitalization, such as orbital cellulitis or abscesses, necessitate immediate surgical intervention. This usually involves performing functional endoscopic sinus surgery (FESS) to drain the infected sinuses and relieve the pressure on the orbit. Broad-spectrum intravenous antibiotics are critical, tailored to the suspected pathogens. Close monitoring of visual acuity, extraocular movements, and neurological status is paramount. In severe cases, an ophthalmologist should be consulted for potential decompression of the orbit.
For instance, I recently managed a patient with orbital cellulitis secondary to ethmoid sinusitis. The patient presented with significant proptosis and decreased visual acuity. Immediate FESS with drainage of the ethmoid sinuses was performed, followed by intravenous antibiotics. The patient responded well to treatment and recovered fully, highlighting the importance of prompt and aggressive management.
Q 17. What are your preferred surgical instruments for FESS?
My preferred surgical instruments for FESS are carefully selected based on the specific surgical need and anatomical considerations. However, a standard set usually includes a 0° and 30° endoscope, various sized microdebriders, a selection of curettes, snares, and small biting forceps. The use of image-guided surgery and navigation systems has significantly enhanced precision and reduced invasiveness. I find that the ability to visualize the surgical field clearly is paramount, so the quality of optics in the endoscope is crucial. The selection of appropriate microdebriders allows for meticulous removal of diseased tissue while preserving the surrounding healthy anatomy. The use of smaller instruments minimizes trauma to the surrounding structures.
The choice of instruments is often tailored to the individual case. For example, in cases involving significant bone removal, a powered drill can be useful, but requires caution to avoid damage to critical structures. Similarly, for smaller areas, microinstruments allow for greater precision and control. Overall, the priority is to select instruments that provide the best visibility, precision, and control for the specific procedure and anatomical situation.
Q 18. How do you counsel patients regarding risks and benefits of sinonasal surgery?
Counseling patients regarding sinonasal surgery involves a comprehensive discussion of the risks and benefits. I begin by thoroughly explaining the patient’s condition, using clear and simple language, avoiding medical jargon. We discuss the potential benefits, such as improved breathing, reduced sinus infections, and resolution of other related symptoms. However, it is equally crucial to discuss potential complications, including bleeding, infection, anosmia (loss of smell), cerebrospinal fluid leak, and orbital complications, albeit rare. The likelihood of these complications is discussed, alongside strategies to mitigate them. Realistic expectations must be set, and it’s important to emphasize that surgery isn’t always a guaranteed cure. The use of visual aids, such as CT scans or anatomical models, can aid in understanding. Shared decision-making is key; the patient’s preferences and understanding of the risks and benefits guide the decision-making process.
For instance, I recently had a patient hesitant about surgery due to concerns about potential anosmia. We had a detailed discussion about the risk, the possibility of temporary vs. permanent loss, and alternative management options. Understanding her concerns allowed for a more informed shared decision, ultimately leading to her deciding to proceed.
Q 19. Describe your approach to managing post-operative pain and bleeding.
Postoperative pain and bleeding management is a crucial aspect of sinonasal surgery. Pain is usually controlled with analgesics, such as acetaminophen or NSAIDs, often combined with opioids in the initial postoperative period. The choice of analgesics depends on the patient’s individual pain tolerance and medical history. Packing is rarely used nowadays; instead, the focus is on meticulous haemostasis during the procedure. Active bleeding is managed with nasal packing, cautery, or occasionally, angiographic embolization for significant bleeding. Post-operative bleeding is usually minimal and can be managed conservatively with nasal saline irrigation and regular monitoring. Patients are instructed to avoid strenuous activities and nasal blowing for several days postoperatively to minimize the risk of bleeding. Regular follow-up appointments allow for assessment of healing and early identification and management of complications.
For example, most patients experience mild discomfort managed with simple analgesics. In cases where pain is more severe, we adjust the pain medication regimen appropriately and consider additional interventions to improve comfort and healing. Post-operative bleeding is uncommon, however, if it occurs, it is typically addressed with appropriate strategies to prevent re-occurrence.
Q 20. What are the common causes of anosmia and how do you investigate it?
Anosmia, or loss of smell, can have various causes, including upper respiratory infections, trauma, nasal polyps, and neurological conditions. In sinonasal surgery, it can be a complication, although usually temporary. The investigation begins with a thorough history, including the onset, duration, and associated symptoms of anosmia. A detailed physical examination of the nose and sinuses is essential, looking for any signs of obstruction or inflammation. Olfactory testing using standardized smell tests (e.g., the Sniffin’ Sticks test) quantifies the severity of the anosmia. Imaging studies, such as CT scans of the paranasal sinuses, help to identify any structural abnormalities that may be contributing to the anosmia. In cases of persistent anosmia following surgery, further investigation, potentially including referral to an otolaryngologist or neurologist, may be required to rule out other underlying causes.
In my practice, I often see temporary anosmia after FESS that resolves within a few weeks as the nasal mucosa heals. However, persistent anosmia necessitates further evaluation to identify the underlying cause and explore potential management strategies.
Q 21. Discuss your experience with the treatment of fungal sinusitis.
Fungal sinusitis is a challenging condition to manage, requiring a multidisciplinary approach. The treatment strategy depends on the type and severity of fungal infection. Allergic fungal rhinosinusitis (AFRS) is often managed medically with corticosteroids and antifungal agents, and sometimes requires surgical debridement to remove fungal debris and improve sinus ventilation. Invasive fungal sinusitis, however, is a life-threatening condition that requires aggressive treatment with intravenous antifungal agents and surgical debridement to remove infected tissue. The choice of antifungal agent is determined by the identified fungal species and the patient’s medical history. Regular monitoring, including imaging and blood tests, is essential to assess treatment response and identify potential complications.
I have managed numerous cases of fungal sinusitis, employing various treatment strategies depending on the specific circumstances. For instance, a patient with AFRS responded well to medical management with corticosteroids and antifungal nasal sprays, resulting in significant symptom improvement and resolution of the disease. In contrast, a patient with invasive fungal sinusitis required aggressive treatment with intravenous antifungal agents and multiple surgical debridements, emphasizing the importance of tailoring the management strategy to the specific type and severity of infection. Close collaboration with infectious disease specialists is often crucial in managing severe cases.
Q 22. How do you evaluate a patient with suspected sinonasal malignancy?
Evaluating a patient with suspected sinonasal malignancy requires a multidisciplinary approach combining a thorough history, meticulous physical examination, and advanced imaging techniques. The history should focus on symptoms like nasal obstruction, epistaxis (nosebleeds), facial pain, changes in smell (anosmia), and any masses or lesions. The physical exam includes a careful rhinoscopic examination to visualize the nasal cavity and paranasal sinuses, assessing for any visible lesions, ulcerations, or masses. This is often complemented by palpation to detect any facial swelling or bony abnormalities.
Imaging plays a crucial role. CT scans with thin cuts are essential for visualizing the extent of the lesion, its relationship to surrounding structures (like the orbit, skull base, and intracranial space), and any evidence of bone destruction. MRI may be used to better delineate soft tissue involvement and assess for intracranial extension. Biopsy is paramount for definitive diagnosis. This usually involves obtaining tissue samples under endoscopic guidance to minimize morbidity and ensure accurate sampling of the suspicious area. The biopsy results are then analyzed by a pathologist, who determines the type and grade of malignancy, guiding treatment decisions.
For example, a patient presenting with unilateral nasal obstruction and a persistent, non-healing ulcer in the nasal cavity would warrant a high suspicion for malignancy. A combination of CT scan demonstrating bone destruction and a biopsy confirming squamous cell carcinoma would lead to a comprehensive treatment plan, which might include surgery, radiation, and/or chemotherapy.
Q 23. Explain the role of minimally invasive techniques in sinonasal surgery.
Minimally invasive techniques have revolutionized sinonasal surgery, offering significant advantages over traditional open approaches. These techniques, primarily utilizing endoscopes, allow for precise visualization and manipulation within the complex sinonasal anatomy with smaller incisions, leading to reduced trauma, faster recovery times, and improved cosmetic outcomes. Examples include functional endoscopic sinus surgery (FESS), which involves removing diseased tissue and improving sinus drainage through small incisions in the nose. Endoscopic approaches also facilitate the removal of nasal polyps, tumors, and foreign bodies with precision.
Minimally invasive techniques are particularly beneficial in cases where preserving normal anatomical structures is crucial, such as in cases involving the orbit or skull base. Image-guided surgery, often integrated with minimally invasive approaches, provides further precision and accuracy, particularly in complex anatomical situations. The reduced trauma translates to less postoperative pain, bleeding, and infection, allowing for quicker patient recovery and return to normal activities. A comparison of traditional open approaches versus minimally invasive endoscopic approaches clearly shows the benefits of the latter with less tissue disruption, smaller scars, and improved patient satisfaction.
Q 24. Describe your familiarity with different types of nasal stents.
Nasal stents are used to maintain the patency of the nasal passages after surgery or trauma. Various types exist, each with specific advantages and disadvantages. They can be broadly categorized by material: silicone, polyethylene, and absorbable materials (e.g., polyglycolic acid). Silicone stents are common due to their flexibility and durability; however, they can cause discomfort and require removal after a set period. Polyethylene stents offer similar benefits but may be less flexible. Absorbable stents eliminate the need for removal but may not provide as robust support.
The choice of stent depends on the surgical procedure and individual patient factors. For example, after a septoplasty (surgical correction of a deviated nasal septum), a flexible silicone stent is often used to prevent septal deviation recurrence and maintain nasal airway patency. Following FESS, a stent might be used to keep the surgical site open and promote healing. The size and shape of the stent are customized to fit the individual patient’s nasal anatomy. Careful patient education on stent care, including cleaning and potential complications (like irritation or infection), is crucial.
Q 25. What are your strategies for managing difficult cases of nasal polyps?
Managing difficult cases of nasal polyps often requires a multi-pronged approach. Large, recurrent polyps can significantly obstruct nasal airflow, impacting breathing, smell, and quality of life. Initial management involves medical therapy with intranasal corticosteroids, aiming to reduce inflammation and polyp size. If medical management fails, surgical intervention is necessary. FESS is the primary surgical technique, but for extensive polyposis, more aggressive techniques might be needed. These may include extensive polypectomy and sometimes, adjuvant therapies like topical steroids or immunomodulators after surgery.
In some cases, revision surgery is necessary for recurrent polyposis. Careful attention to the underlying causes of polyp formation—including aspirin sensitivity, cystic fibrosis, and other immune dysregulation issues—is crucial to prevent recurrence. For instance, in a patient with recurrent polyps and known aspirin sensitivity, avoiding aspirin and other NSAIDs is critical. A collaborative approach with allergologists and immunologists is often necessary to address the underlying disease and ensure long-term management.
Q 26. Discuss the use of corticosteroids in the management of sinusitis.
Corticosteroids are the cornerstone of medical management for sinusitis, both acute and chronic. They act by reducing inflammation and edema within the sinus mucosa, improving mucociliary clearance and promoting sinus drainage. They can be administered topically (intranasal sprays or drops) or systemically (oral or intravenous). Topical administration is preferred for its localized effect, minimizing systemic side effects. Intranasal corticosteroids are generally well-tolerated but can cause local side effects, such as nosebleeds and dryness.
The choice of corticosteroid and dosage depends on the severity and chronicity of the sinusitis. In acute sinusitis, a short course of oral corticosteroids might be used to provide rapid symptom relief. Chronic sinusitis, however, typically requires long-term topical corticosteroid therapy. For instance, fluticasone, mometasone, and budesonide are commonly used intranasal corticosteroids. Careful monitoring for side effects and adherence to prescribed medication regimens are essential for effective management.
Q 27. How do you approach a patient with recurrent sinusitis after previous surgery?
Recurrent sinusitis after previous surgery requires a thorough investigation to identify the underlying cause. This includes a detailed history, including the type of previous surgery, and a comprehensive physical examination with rhinoscopy. Imaging studies, such as CT scans, are crucial to assess the status of the sinuses, identifying any residual disease, anatomical variations, or postoperative complications. It’s essential to rule out any underlying systemic conditions that could contribute to recurrent sinusitis, such as immunodeficiency.
Management may involve repeat surgery to address any residual disease or anatomical abnormalities. However, this decision is made cautiously, considering the risks and benefits. Functional endoscopic sinus surgery (FESS) is commonly employed in revision surgery, aiming for precise and complete disease removal while minimizing further damage to surrounding structures. Pre- and post-operative management often includes systemic and/or topical corticosteroids to reduce inflammation and prevent recurrence. In selected patients, alternative therapeutic strategies such as biologic therapies might be considered.
Q 28. Describe your experience with the surgical management of sinonasal trauma.
Sinonasal trauma can range from minor injuries to severe, life-threatening conditions. Management depends on the severity of the injury and involves a careful assessment of the patient’s airway, breathing, and circulation (ABCs). Initial assessment includes a detailed history, physical exam, and imaging studies (CT scans are invaluable). The aim of surgical management is to restore the integrity of the nasal bones and cartilages, repair any fractures, and manage any intracranial complications.
Surgical techniques vary according to the specific injury. Open reduction and internal fixation (ORIF) may be required for significant fractures. Endoscopic approaches can be utilized to manage certain types of nasal septal injuries and reduce the need for extensive open surgical incisions. In cases involving cerebrospinal fluid rhinorrhea (CSF leakage from the nose), neurosurgical consultation is essential, as a watertight repair of the skull base is required to prevent infection (meningitis). Post-operative care emphasizes preventing infection, managing pain, and ensuring the patient’s airway is adequately maintained.
Key Topics to Learn for Sinonasal Surgery Interview
- Anatomy and Physiology: Mastering the intricate anatomy of the sinonasal region, including the paranasal sinuses, nasal cavity, and surrounding structures. Understanding the physiological processes involved in nasal airflow, mucociliary clearance, and olfactory function is crucial.
- Endoscopic Sinus Surgery (ESS) Techniques: Develop a thorough understanding of various ESS techniques, including their indications, contraindications, and potential complications. Practice explaining the surgical steps and rationale behind specific choices during procedures.
- Diagnosis and Imaging: Become proficient in interpreting relevant imaging studies such as CT scans and MRI scans to accurately diagnose sinonasal pathologies. Discuss your experience with different imaging modalities and their clinical applications.
- Surgical Planning and Decision-Making: Develop strong problem-solving skills by practicing formulating surgical plans based on patient-specific presentations and imaging findings. Be ready to justify your choices and discuss alternative approaches.
- Management of Complications: Familiarize yourself with the common complications associated with sinonasal surgery and develop strategies for their prevention and management. Be prepared to discuss your approach to managing intraoperative and postoperative challenges.
- Medical and Surgical Treatment of Sinonasal Diseases: Gain a comprehensive understanding of the various medical and surgical treatments available for common sinonasal diseases, such as rhinosinusitis, nasal polyps, and tumors. Be able to compare and contrast different treatment options based on clinical scenarios.
- Advanced Techniques and Technologies: Explore advanced techniques and technologies used in sinonasal surgery, such as image-guided surgery and minimally invasive approaches. Understanding the latest advancements demonstrates your commitment to staying current in the field.
Next Steps
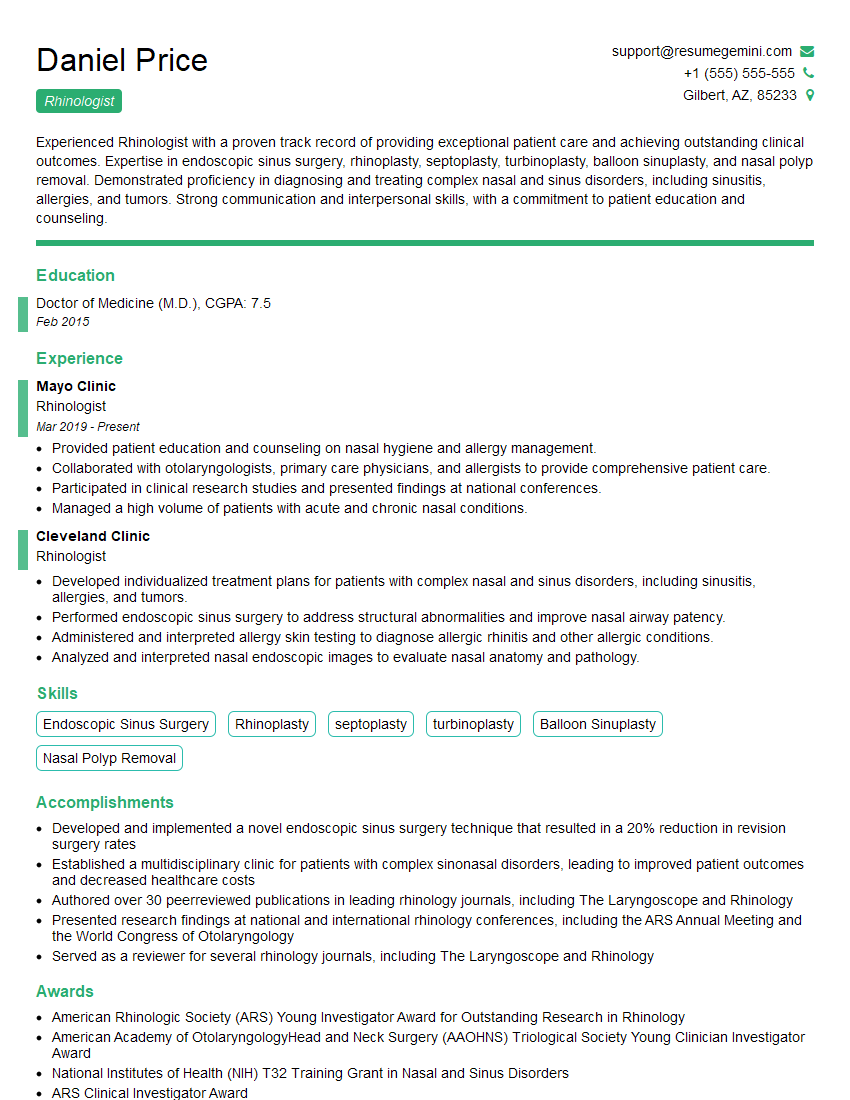
Mastering Sinonasal Surgery opens doors to exciting career advancements, including specialized fellowships, leadership roles, and opportunities for research and innovation. To significantly enhance your job prospects, crafting a compelling and ATS-friendly resume is essential. ResumeGemini is a trusted resource that can help you build a professional resume that highlights your skills and experience effectively. ResumeGemini provides examples of resumes tailored to Sinonasal Surgery, ensuring your application stands out. Invest time in building a strong resume – it’s a critical step towards securing your dream position.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.