Cracking a skill-specific interview, like one for Swallowing Disorders, requires understanding the nuances of the role. In this blog, we present the questions you’re most likely to encounter, along with insights into how to answer them effectively. Let’s ensure you’re ready to make a strong impression.
Questions Asked in Swallowing Disorders Interview
Q 1. Describe the different phases of swallowing.
Swallowing, or deglutition, is a complex process involving multiple phases working in a coordinated manner to safely transport food and liquids from the mouth to the stomach. It’s often described in four phases:
- Oral Preparatory Phase: This is the voluntary phase where food is manipulated in the mouth. Saliva mixes with the bolus (the mass of chewed food), forming a cohesive substance ready for swallowing. Tongue movements are crucial for this phase, positioning the bolus for the next step. Think of it as the ‘preparation’ stage before the actual swallow.
- Oral Phase: This is also a voluntary phase. The tongue propels the bolus posteriorly (backward) toward the pharynx (throat). This phase is crucial for initiating the swallow reflex. If the bolus is too big or the tongue isn’t working properly, this phase can be impaired.
- Pharyngeal Phase: This is an involuntary phase initiated by sensory receptors in the pharynx once the bolus reaches the faucial arches (the arches at the back of the mouth). A complex series of events occurs: the soft palate elevates to prevent nasal regurgitation, the larynx elevates and moves forward protecting the airway, the epiglottis covers the laryngeal opening, and the pharyngeal constrictors propel the bolus down into the esophagus. This is where the body takes over; it’s a reflex action.
- Esophageal Phase: This is the final involuntary phase. Peristaltic waves (rhythmic contractions) move the bolus through the esophagus into the stomach. The lower esophageal sphincter relaxes to allow entry into the stomach and then contracts to prevent reflux.
Any disruption in any of these phases can lead to a swallowing disorder, or dysphagia.
Q 2. Explain the clinical presentation of oropharyngeal dysphagia.
Oropharyngeal dysphagia refers to difficulty swallowing in the oral and pharyngeal phases. The clinical presentation is highly variable, depending on the underlying cause and the specific phase affected. However, some common signs and symptoms include:
- Oral Phase Symptoms: Difficulty chewing, reduced tongue strength or coordination (leading to pocketing of food in the cheeks or inability to form a bolus), prolonged oral transit time.
- Pharyngeal Phase Symptoms: Coughing or choking during or after swallowing, nasal regurgitation (food coming out of the nose), frequent throat clearing, food sticking sensation in the throat, delayed or absent pharyngeal swallow reflex, wet vocal quality (due to aspiration – food entering the airway), recurrent pneumonia (due to aspiration).
- Other Symptoms: Weight loss, dehydration, difficulty managing secretions, food aversion, social isolation, and a feeling of fear while eating.
It’s important to note that the severity of these symptoms can range from mild to life-threatening. A thorough clinical evaluation, often followed by instrumental assessment, is necessary to determine the extent of the dysphagia and develop an appropriate treatment plan.
Q 3. What are the common instrumental assessments used to evaluate swallowing disorders?
Instrumental assessments provide objective information about the swallowing process, supplementing the clinical examination. Common methods include:
- Modified Barium Swallow Study (MBSS): A fluoroscopic (X-ray) examination where the patient swallows barium-mixed food and liquids of different consistencies. This allows for real-time visualization of the swallowing process, identifying anatomical and physiological abnormalities.
- Fiberoptic Endoscopic Evaluation of Swallowing (FEES): A flexible endoscope is passed through the nose into the pharynx and upper esophagus. This allows for direct visualization of the pharyngeal swallow and assessment of laryngeal function, helping to evaluate aspiration risk.
- Ultrasound: High-frequency sound waves generate images of the tongue, hyoid bone, and other structures involved in swallowing. This method is non-invasive and can be used to assess tongue movement, hyoid excursion, and bolus transit time.
The choice of assessment depends on the clinical presentation and suspected site of the problem. Sometimes a combination of these assessments is necessary for a complete evaluation.
Q 4. How do you differentiate between oropharyngeal and esophageal dysphagia?
Differentiating between oropharyngeal and esophageal dysphagia is crucial for appropriate management. Oropharyngeal dysphagia, as discussed earlier, involves problems in the oral cavity and pharynx. Esophageal dysphagia, on the other hand, involves problems in the esophagus – the tube connecting the pharynx to the stomach.
Key Differences:
- Location of Symptoms: Oropharyngeal dysphagia often presents with symptoms felt in the mouth or throat (choking, coughing, nasal regurgitation), while esophageal dysphagia involves symptoms felt in the chest (food sticking, heartburn, regurgitation).
- Timing of Symptoms: Oropharyngeal difficulties usually occur immediately after initiating the swallow, while esophageal problems often manifest later, sometimes even after the bolus has already passed the pharynx.
- Nature of Symptoms: Oropharyngeal dysphagia may involve choking, coughing, and aspiration, while esophageal dysphagia often involves sensations of food sticking, difficulty initiating swallows, and regurgitation.
Instrumental assessments like MBSS and FEES are essential for precise localization and diagnosis, as symptoms can sometimes overlap.
Q 5. Describe the modified barium swallow study (MBSS) procedure and its interpretations.
The Modified Barium Swallow Study (MBSS) is a radiological procedure providing a dynamic view of the swallowing process. A radiologist or speech-language pathologist trained in interpreting MBSS performs this test.
Procedure: The patient is seated upright in front of a fluoroscopy machine and is given barium-mixed foods and liquids of varying consistencies (thin liquids, nectar-thick liquids, honey-thick liquids, pureed foods, and solid foods). The patient swallows these while the radiologist observes the movement of the barium through the oral, pharyngeal, and esophageal phases. Lateral and anterior-posterior views are typically used. The entire swallow is assessed for safety and efficiency.
Interpretations: The radiologist analyzes the MBSS recordings to identify any abnormalities in:
- Oral phase: Bolus preparation, oral transit time, tongue movement.
- Pharyngeal phase: Laryngeal elevation, epiglottic inversion, airway protection, pharyngeal transit time, presence of aspiration.
- Esophageal phase: Esophageal transit time, presence of esophageal reflux.
Based on these findings, the radiologist provides a report outlining the nature and severity of any swallowing impairment, along with recommendations for therapeutic interventions.
Q 6. What are the different types of dysphagia therapies?
Dysphagia therapy is individualized and depends on the cause, location, and severity of the swallowing disorder. Treatment modalities include:
- Compensatory strategies: These are techniques to improve swallowing safety and efficiency, without directly addressing the underlying cause. Examples include postural adjustments, dietary modifications, and swallowing maneuvers.
- Rehabilitative therapy: This involves exercises to improve muscle strength, coordination, and range of motion. Techniques may involve range-of-motion exercises for the tongue and jaw, strengthening exercises, and sensory stimulation.
- Surgical interventions: Surgery may be necessary in cases of anatomical abnormalities or severe esophageal dysphagia. Procedures can range from myotomy (cutting of muscles) to dilation of strictures.
- Pharmacological interventions: Medications can address underlying conditions such as GERD or neurological diseases that may contribute to dysphagia. They don’t directly treat swallowing difficulties, but address associated factors.
A multidisciplinary team, typically including a speech-language pathologist, physician, and dietitian, is often involved in developing and implementing a comprehensive treatment plan.
Q 7. Explain the principles of compensatory strategies for dysphagia.
Compensatory strategies aim to enhance the safety and efficiency of the swallow without directly addressing the underlying physiological cause. These strategies work around the limitations of the swallowing mechanism.
Principles:
- Postural Adjustments: Changing body position to improve swallowing safety and efficiency. For example, head tilt to one side to direct bolus flow away from a weakened side, head turned to reduce aspiration risk, chin tuck to narrow the airway.
- Dietary Modifications: Changing food consistency or texture to improve swallowability. This may involve pureeing foods, using thickeners for liquids, or avoiding certain foods that are difficult to manage.
- Swallowing Maneuvers: Using specific techniques to improve the timing and coordination of the swallow. These may include the Mendelsohn maneuver (prolonged elevation of the larynx), the supraglottic swallow (holding breath before swallowing to close the airway), and the effortful swallow (intentional increase in muscle force during swallowing).
The choice of compensatory strategies depends on the individual’s swallowing deficits and their ability to learn and implement the techniques. These strategies are often temporary, serving as a bridge until more permanent solutions, such as rehabilitative therapy or surgery, can be implemented.
Q 8. How do you manage aspiration pneumonia in patients with dysphagia?
Managing aspiration pneumonia in patients with dysphagia requires a multi-pronged approach focusing on prevention and treatment. Aspiration pneumonia occurs when food, liquid, or saliva enters the lungs, leading to infection. In dysphagia patients, impaired swallowing mechanics increase this risk.
Prevention is key. This involves thorough assessment of swallowing function using tools like a clinical bedside swallow examination (CSE) or Fiberoptic Endoscopic Evaluation of Swallowing (FEES). Based on the assessment, we tailor strategies to minimize aspiration risk. These include dietary modifications (e.g., thickened liquids, pureed foods), postural adjustments (e.g., head-forward posture, chin tuck), and swallowing maneuvers (e.g., Mendelsohn maneuver). Regular oral care is crucial to reduce bacterial load in the mouth.
Treatment of aspiration pneumonia involves antibiotics, respiratory support (if needed), and close monitoring of respiratory status. We work closely with respiratory therapists and pulmonologists to ensure appropriate management. Continued dysphagia management remains crucial to prevent recurrence. For example, a patient with aspiration pneumonia following a stroke might require a temporary feeding tube for nutritional support while their swallowing recovers alongside intensive speech therapy.
Imagine a patient with Parkinson’s disease experiencing frequent coughing after swallowing. We’d assess their swallowing using FEES to visualize the aspiration and then implement strategies like thickened liquids and postural changes, closely monitoring for improvement.
Q 9. What are the nutritional considerations for patients with swallowing difficulties?
Nutritional considerations for patients with dysphagia are paramount to maintain their health and quality of life. Malnutrition and dehydration are common complications. The focus is on providing adequate nutrition while ensuring safety.
We consider several factors: The severity of the dysphagia dictates the diet consistency. Mild dysphagia might only require minor modifications like avoiding certain textures, while severe dysphagia might require a pureed or liquid diet. Nutritional needs vary based on the individual’s age, medical condition, and activity level. We use nutritional assessments to determine calorie and protein requirements. Food preferences and cultural factors are also taken into account to enhance compliance and satisfaction. We may involve a registered dietitian to create individualized meal plans.
Practical strategies include providing frequent, smaller meals to reduce fatigue, offering nutrient-dense foods and supplements to compensate for restricted diets, and encouraging hydration using thickened liquids if aspiration is a concern. We might also recommend enteral feeding (through a tube) if oral intake is insufficient or unsafe. For example, a patient with head and neck cancer who experiences severe dysphagia may require a nasogastric tube for nutritional support during treatment.
Q 10. How do you assess the patient’s swallowing safety?
Assessing swallowing safety involves a multi-faceted approach aimed at identifying the presence and severity of dysphagia and determining the risk of aspiration and penetration.
We begin with a clinical bedside swallow examination (CSE), a screening tool evaluating oral-motor skills, vocal quality, cough strength, and swallowing patterns. The CSE might involve observing the patient swallowing different consistencies of food and liquids. This helps us determine the need for further evaluation.
If the CSE shows potential risk or a need for more detailed information, we proceed with a more advanced assessment technique like Fiberoptic Endoscopic Evaluation of Swallowing (FEES). FEES allows direct visualization of the swallowing process. It’s a powerful tool for identifying the precise location and nature of swallowing impairments. Other techniques, such as videofluoroscopic swallow study (VFSS), can also be employed.
The ultimate goal is to determine the patient’s ability to safely consume food and liquids, identifying any potential aspiration risks and developing strategies to mitigate those risks.
Q 11. Describe your experience with FEES (Fiberoptic Endoscopic Evaluation of Swallowing).
FEES (Fiberoptic Endoscopic Evaluation of Swallowing) is a crucial part of my assessment and management of dysphagia. It’s a flexible endoscopic procedure that allows direct visualization of the pharynx and larynx during swallowing. I have extensive experience using FEES to identify the exact anatomical location and nature of swallowing problems.
My experience spans various patient populations, including individuals with neurological disorders (stroke, Parkinson’s disease, multiple sclerosis), head and neck cancer, and aging-related swallowing difficulties. I use FEES to identify pharyngeal residue, aspiration, penetration, and other signs of impaired swallowing.
For example, a patient with a history of stroke might present with reduced pharyngeal contraction. Using FEES, I can precisely visualize this weakness and determine the optimal strategies to improve their swallowing safety, like postural modifications or compensatory swallowing techniques. The real-time visualization of FEES aids in customizing therapy plans and monitoring treatment effectiveness.
Q 12. How do you tailor treatment plans to individual patient needs?
Tailoring treatment plans for dysphagia is crucial because each patient’s condition, needs, and preferences are unique. We don’t use a ‘one-size-fits-all’ approach. My approach centers around creating a patient-centered plan by considering several factors.
Diagnosis and severity: The nature and extent of the swallowing difficulty influences the treatment. A patient with mild dysphagia might benefit from simple dietary modifications and swallowing exercises, whereas someone with severe dysphagia might require more intensive therapy, including postural adjustments and possibly even a feeding tube.
Medical history and co-morbidities: Co-existing medical conditions can impact treatment choices. For example, a patient with dementia might require simpler instructions and strategies compared to someone with a higher cognitive capacity.
Patient preferences and goals: I collaborate closely with the patient and their family to establish realistic and attainable goals, considering their lifestyle, dietary preferences, and cultural background.
Monitoring and adjustments: Treatment plans are dynamic, not static. We regularly monitor progress and modify the plan as needed to ensure effectiveness and safety. For instance, a patient’s swallowing might improve over time, allowing us to gradually introduce more varied textures into their diet.
Q 13. What are the ethical considerations in treating patients with dysphagia?
Ethical considerations in treating patients with dysphagia are significant. We prioritize patient autonomy, beneficence, non-maleficence, and justice.
Autonomy: Patients have the right to make informed decisions about their care, even if it means accepting risks. We ensure they understand their condition and treatment options before making choices about their diet and feeding methods.
Beneficence: We aim to do good for our patients, providing the most effective and safe interventions to improve their nutritional status and quality of life. This involves staying current with the latest evidence-based practices.
Non-maleficence: We avoid causing harm. This requires careful consideration of the potential risks and benefits of each treatment option, especially when considering invasive procedures such as placing a feeding tube.
Justice: Ensuring equitable access to high-quality dysphagia care regardless of socioeconomic status, ethnicity, or other factors is essential. We aim to provide compassionate and respectful care to all our patients.
Q 14. Explain the role of interprofessional collaboration in dysphagia management.
Interprofessional collaboration is critical in dysphagia management. A successful outcome hinges on the coordinated efforts of a team of professionals.
The team typically includes: Speech-language pathologists (SLPs), who lead the assessment and treatment of swallowing disorders; physicians (e.g., gastroenterologists, neurologists) who address underlying medical conditions; registered dietitians who develop tailored nutritional plans; occupational therapists who can address the patient’s functional skills; nursing staff who provide day-to-day care and monitor for complications; and radiologists for imaging studies like VFSS.
Effective communication and collaboration among these professionals are vital to creating a comprehensive and personalized plan, ensuring timely interventions and optimal patient outcomes. For instance, the SLP might identify aspiration risk through FEES, which the physician then considers when managing the patient’s medication, while the dietitian modifies the diet based on the SLP’s findings.
Q 15. How do you document your findings and treatment progress?
Documenting findings and treatment progress in dysphagia is crucial for effective patient care and tracking improvement. My documentation meticulously records all aspects of the patient’s swallowing journey. This begins with a comprehensive initial assessment, detailing the patient’s medical history, symptoms, and the results of objective tests like a clinical swallowing examination (CSE), videofluoroscopic swallow study (VFSS), or fiberoptic endoscopic evaluation of swallowing (FEES).
The CSE involves observing the patient’s oral-motor skills, such as lip closure, tongue movement, and the coordination of these actions during swallowing. VFSS uses fluoroscopy (X-ray) to visualize the swallow in real-time, allowing for detailed analysis of the bolus’s (food or liquid) movement through the pharynx (throat) and esophagus. FEES provides an endoscopic view of the pharynx and larynx (voice box) to assess the integrity and function of these structures. Post-assessment, my documentation includes the diagnosis, treatment plan (including diet modifications, compensatory strategies, and exercises), and the rationale behind each intervention.
I meticulously track the patient’s progress throughout therapy. This includes noting their tolerance for different food consistencies and volumes, improvements in their swallowing efficiency, any adverse events (like aspiration – food entering the airway), and the patient’s subjective experience of their swallowing. I regularly update the treatment plan based on this ongoing assessment, ensuring the interventions remain effective and tailored to the patient’s evolving needs. This structured documentation is essential for communication with other members of the healthcare team, for insurance purposes, and for facilitating continuous improvement of care.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you educate patients and families about dysphagia?
Educating patients and families about dysphagia is paramount for successful therapy. I use a multi-faceted approach that combines clear, simple explanations with visual aids and practical demonstrations. First, I explain the condition in terms they easily understand. For instance, I might say, “Imagine your swallowing mechanism as a team of players working together to get food safely down. With dysphagia, some players are struggling, and we need to help them function better.”
I use visual aids like diagrams or videos showing the normal swallowing process and how it is affected in dysphagia. I then explain the specific difficulties the patient is experiencing, relating them back to the visual aids. For example, if a patient has difficulty with bolus control, I might show them a video of a normal swallow alongside one of their own swallow demonstrating the difference. I provide individualized education about their specific swallowing issues, explaining the rationale behind their prescribed diet modifications and swallowing exercises. For instance, I’d explain why a thickened liquid diet is necessary or demonstrate specific exercises to strengthen their tongue muscles.
I emphasize the importance of active patient participation in the treatment plan. Family involvement is also key. I encourage families to practice exercises with their loved ones at home, observe for any changes in swallowing, and report any concerns promptly. I provide written materials reinforcing the information, and I’m always available to answer their questions and address their concerns. This collaborative approach ensures that patients and their families are well-informed and empowered to participate in their recovery journey.
Q 17. What are the common causes of dysphagia in stroke patients?
Dysphagia, or difficulty swallowing, is a common complication after stroke. Several factors contribute to this:
- Neurological Damage: Stroke disrupts brain pathways that control swallowing. Depending on the location and extent of the brain damage, various aspects of swallowing can be impaired, from the initiation of the swallow to the coordination of muscle movements.
- Muscle Weakness: Stroke can cause weakness or paralysis of the muscles involved in swallowing, including those in the mouth, throat, and esophagus. This weakness can lead to difficulty moving food around in the mouth, inadequate bolus formation, and impaired transport of the bolus down the throat.
- Reduced Sensation: Damage to the sensory pathways can affect the feeling of food in the mouth and the awareness of its position. This can lead to difficulties in initiating the swallow, controlling the bolus, and sensing the presence of food remaining in the mouth or throat.
- Coordination Problems: The intricate coordination of muscles during swallowing relies on precise neural signals. Stroke can disrupt this coordination, leading to incoordinated movements that compromise the safety and efficiency of swallowing.
- Aspirations: Due to the above problems, a significant risk associated with post-stroke dysphagia is aspiration, the entry of food or liquid into the airway which can lead to pneumonia.
The specific swallowing difficulties a stroke patient experiences depend on the location and severity of the brain damage. A comprehensive assessment is crucial to determine the exact nature of the problem and develop a tailored treatment plan.
Q 18. Describe the swallowing difficulties associated with Parkinson’s disease.
Parkinson’s disease, a neurodegenerative disorder, often presents with characteristic swallowing difficulties due to its impact on the nervous system’s control over the muscles of swallowing. The hallmark feature is a slowing and reduced coordination of swallowing movements, often described as bradykinesia (slow movement) and dyskinesia (difficulty with movement).
Patients with Parkinson’s often exhibit:
- Delayed initiation of swallowing: There may be a noticeable delay in starting the swallow reflex.
- Reduced tongue mobility: This impacts the manipulation of the bolus in the mouth and the transfer of food to the pharynx.
- Poor oral-pharyngeal coordination: The coordinated movement of the tongue, soft palate, and pharyngeal muscles required for efficient transport of the bolus is often compromised.
- Reduced pharyngeal pressure: Weak pharyngeal muscles result in incomplete bolus clearance from the throat, leading to residue.
- Increased risk of aspiration: The combination of slow movement, reduced pharyngeal pressure, and impaired coordination increases the risk of food or liquid entering the airway (aspiration).
The severity of these swallowing difficulties varies among patients, impacting their quality of life and nutritional status. Management focuses on improving oral motor skills through exercises, optimizing food consistency, and employing compensatory strategies to enhance the safety and efficiency of swallowing. In advanced cases, non-oral feeding methods like gastrostomy tubes might be necessary.
Q 19. How do you manage dysphagia in patients with head and neck cancer?
Managing dysphagia in patients with head and neck cancer requires a multidisciplinary approach given the challenges posed by the disease itself and its treatment. Cancer, surgery, radiation, and chemotherapy can all severely impact swallowing function.
Pre-Treatment Assessment: A thorough swallowing evaluation is crucial before initiating treatment to establish a baseline and identify existing swallowing difficulties. This helps anticipate potential problems and plan for interventions.
Treatment-Specific Interventions: During and after treatment, interventions are tailored to address the specific swallowing problems that arise. For example, if surgery involves the removal of a portion of the tongue, post-operative therapy will focus on strengthening remaining muscles and compensatory strategies to overcome the loss of function. Similarly, radiation therapy may cause mucositis (inflammation of the mucous membranes), requiring strategies for managing pain and facilitating swallowing comfort.
Nutritional Support: Maintaining adequate nutrition and hydration is critical, especially when swallowing is severely compromised. This might involve dietary modifications (e.g., pureed diets, thickened liquids), nutritional supplements, and in some cases, the placement of a feeding tube (e.g., PEG tube).
Swallowing Therapy: This is a cornerstone of management and involves techniques aimed at improving strength, coordination, and efficiency of swallowing. Exercises might include range-of-motion exercises for the tongue and jaw, exercises to improve bolus manipulation, and maneuvers to improve pharyngeal pressure.
Ongoing Monitoring: Regular monitoring of swallowing function is essential throughout the treatment and recovery period. This often involves serial swallowing assessments to track progress and adjust the treatment plan as needed. It is very much a team approach with oncologists, surgeons, and speech-language pathologists all coordinating to ensure comprehensive care.
Q 20. What are the early warning signs of dysphagia in children?
Recognizing early warning signs of dysphagia in children is crucial for timely intervention and preventing long-term consequences. These signs can be subtle and often overlooked, so vigilance is essential.
Early warning signs may include:
- Difficulty feeding: Frequent choking or coughing during feeding, prolonged feeding times, arching back, or pushing food away.
- Poor weight gain or failure to thrive: Insufficient caloric intake due to swallowing difficulties can lead to significant weight loss or lack of growth.
- Recurrent respiratory infections: Aspiration (food or liquid entering the lungs) increases the risk of pneumonia and other respiratory illnesses.
- Frequent vomiting or regurgitation: This may indicate problems with esophageal emptying or reflux.
- Excessive drooling: Increased drooling can be a sign of poor oral motor skills and difficulty managing saliva.
- Gurgly voice or nasal regurgitation: These indicate that food or liquid may be entering the nasal cavity or the airway.
- Changes in behaviour during feeding: Fussiness, irritability, or avoidance of feeding are often indicators of swallowing difficulties.
If you observe any of these signs in a child, it’s vital to consult a pediatrician or a speech-language pathologist specializing in pediatric dysphagia for a thorough evaluation.
Q 21. How do you assess and manage pediatric dysphagia?
Assessing and managing pediatric dysphagia requires a specialized approach, considering the child’s developmental stage and unique needs. The assessment typically involves a detailed history, including feeding history, medical history, and developmental milestones.
Assessment Techniques: A thorough clinical examination assesses oral-motor skills, such as lip closure, tongue movement, and sucking ability. Instrumental evaluations, like VFSS or FEES, are frequently employed for a detailed view of the swallowing process. The choice of instrument depends on factors such as the child’s age, tolerance level, and the specific clinical questions being addressed.
Management Strategies: Interventions are customized to the child’s specific needs and may include postural changes during feeding, modifying food consistency, employing specialized feeding techniques, implementing oral-motor exercises, and utilizing specialized equipment (e.g., adaptive feeding utensils).
Collaboration: A multidisciplinary team approach is often crucial, involving pediatricians, gastroenterologists, speech-language pathologists, occupational therapists, and dieticians. Parents are integral to the treatment process, receiving education and training to implement strategies at home.
Ongoing Monitoring: Regular monitoring of the child’s progress is important, ensuring interventions are effective and addressing any emerging challenges. Consistent communication among the healthcare team and family members is key to maintaining the child’s safety and maximizing treatment outcomes. The goal is always to optimize the child’s feeding and nutrition, while fostering healthy eating behaviors and minimizing the risk of aspiration.
Q 22. Explain the differences between aspiration and penetration.
Aspiration and penetration are two distinct, yet often related, events that occur during swallowing. Both involve material entering the airway, but their location differs significantly, impacting the severity of the consequences.
Penetration refers to the entry of food or liquid into the larynx (voice box) above the vocal cords. This material does not pass below the vocal cords into the trachea (windpipe). While penetration can cause coughing or choking, it doesn’t necessarily lead to lung infection (pneumonia). Think of it like food briefly touching the doorway to the lungs but not entering the house itself.
Aspiration, on the other hand, is the entry of food or liquid into the trachea and below the vocal cords, potentially reaching the lungs. This is far more serious, as it can cause choking, pneumonia, and other respiratory complications. Imagine this as the food actually entering the house (lungs) and potentially causing damage.
For example, a patient might exhibit penetration by coughing after a swallow, clearing their airway successfully. However, a patient who aspirates might show signs of decreased oxygen saturation, wet vocal quality, or recurrent pneumonia without overt coughing immediately after each swallow. Distinguishing between these two is crucial for appropriate intervention.
Q 23. Discuss the role of diet modifications in managing dysphagia.
Diet modifications are a cornerstone of dysphagia management. The goal is to adjust food consistency and texture to improve the safety and efficiency of swallowing. This isn’t about restricting the patient’s diet but about making it safer.
- Level 1 (Pureed): Foods are completely smooth and homogeneous, like pudding or applesauce. Ideal for patients with very poor oral motor skills.
- Level 2 (Minced and Moist): Foods are soft and moist, easily mashed with a fork, like scrambled eggs or well-cooked vegetables.
- Level 3 (Soft and Bite-Sized): Foods are soft enough to be easily chewed and swallowed, but still require some mastication, such as soft cooked chicken or well-cooked pasta.
- Level 4 (Regular): Regular diet with appropriate consideration given to portion size and food choices to minimize risks.
We also consider other factors such as temperature (avoiding very hot or cold foods), liquid viscosity (thickened liquids are often safer), and food presentation (smaller portions, limiting distractions). Diet modification strategies are tailored to each patient’s specific needs and swallowing abilities. For example, a patient with limited tongue movement might benefit from pureed foods, whereas a patient with decreased chewing ability may be managed with minced and moist consistency.
Q 24. What are some common swallowing exercises you use?
Swallowing exercises aim to improve muscle strength, coordination, and range of motion involved in swallowing. The specific exercises chosen depend on the patient’s individual needs and the underlying cause of their dysphagia.
- Masako Maneuver: The patient holds their tongue between their teeth while swallowing to strengthen the base of the tongue.
- Tongue-to-Palate Exercises: Repeatedly touching the tongue to the hard palate (roof of the mouth) improves tongue elevation and strength.
- Chin-Tuck Postures: Tilting the chin downwards narrows the airway, facilitating swallowing safety.
- Mendelsohn Maneuver: Sustaining the upward movement of the larynx during swallowing strengthens the laryngeal muscles.
- Effortful Swallow: Increased effort during the swallow attempts improves posterior movement of the bolus.
It’s crucial to supervise these exercises closely and adjust them based on the patient’s response. For example, if a patient struggles with the Masako maneuver, we may modify it or focus on other exercises that target similar muscle groups.
Q 25. How do you use technology to assess or treat dysphagia?
Technology plays an increasingly important role in both assessing and treating dysphagia. Fiberoptic endoscopic evaluation of swallowing (FEES) is a widely used procedure that allows visualization of the swallowing process through a flexible endoscope passed through the nose. This provides real-time feedback on bolus transit and helps to identify the exact location and nature of the swallowing difficulties.
Videofluoroscopic Swallow Study (VFSS) or Modified Barium Swallow Study (MBSS) is another important diagnostic tool; it involves using X-rays to visualize the swallow. This is particularly helpful in identifying aspiration or penetration. This is also important for seeing anatomical structures.
Beyond diagnostics, technology also assists in therapy. There are software programs and apps that provide biofeedback on swallowing exercises, helping patients to improve their technique. Virtual reality (VR) is being explored as a tool to train patients in the safe performance of swallowing exercises in a simulated environment.
Q 26. How do you determine if a patient needs a referral to another specialist?
The decision to refer a patient to another specialist depends on various factors. If a patient presents with persistent and severe dysphagia despite appropriate management, a referral may be necessary.
- ENT (Ear, Nose, and Throat) Specialist: If there’s a suspected structural issue in the throat or vocal cords, such as a tumor or vocal cord paralysis.
- Gastroenterologist: If there is a suspicion of gastroesophageal reflux disease (GERD) or other esophageal issues impacting swallowing.
- Neurologist: For patients with neurological conditions impacting swallowing such as stroke, Parkinson’s disease, or multiple sclerosis.
- Speech-Language Pathologist (SLP) specializing in dysphagia: Depending on the level of expertise needed, more advanced cases may require referral to a specialist within the field of SLP, such as those experienced in treating pediatric dysphagia, or neurogenic dysphagia.
Any indication of aspiration pneumonia, rapid weight loss, severe dehydration or ongoing concerns that are outside the scope of my expertise warrant immediate referral to the appropriate specialist.
Q 27. What are some challenges you’ve faced in managing dysphagia cases, and how did you overcome them?
One major challenge is the variability in patients’ responses to treatment. What works for one patient might not work for another. For example, some patients respond well to simple diet modifications, while others require intensive therapy and technology-assisted approaches. This requires flexibility and ongoing assessment to adapt strategies as needed.
Another challenge is managing patients with complex medical histories. Often, dysphagia is just one symptom among many, and addressing the underlying medical conditions is crucial. This necessitates effective interprofessional collaboration with other specialists, ensuring a holistic approach to the patient’s care.
I overcome these challenges by staying updated on the latest research and best practices, meticulously documenting each patient’s progress, and actively seeking consultation with colleagues when needed. Open communication with the patient and their family helps create a collaborative environment that facilitates successful management.
Q 28. Describe a challenging case involving dysphagia and your approach to resolving it.
I once worked with an elderly patient who had suffered a severe stroke resulting in significant left-sided weakness and dysphagia. She exhibited frequent aspiration, difficulty initiating swallows, and significant food residue in her mouth. Initial efforts focused on postural adjustments (chin tuck) and thickened liquids showed minimal improvement.
My approach involved a multi-pronged strategy: we conducted a FEES to precisely identify the location of her swallowing difficulties. This revealed significant weakness in her pharyngeal muscles. We then implemented a tailored program combining the Mendelsohn maneuver, effortful swallows, and intensive oral motor exercises. We also worked closely with the occupational therapist to improve her head and neck control. We monitored her progress closely using regular FEES examinations. Through perseverance and a collaborative approach, she gradually improved her swallowing safety and eventually progressed to a less restricted diet. While she always required some degree of assistance, her quality of life improved remarkably due to our collaborative and tailored intervention.
Key Topics to Learn for Swallowing Disorders Interview
- Anatomy and Physiology of Swallowing: Understand the intricate neuromuscular mechanisms involved in each phase of swallowing (oral, pharyngeal, esophageal).
- Dysphagia Assessment Techniques: Master the clinical skills involved in conducting a thorough bedside swallow evaluation, including clinical examination, instrumental assessments (e.g., FEES, VFSS), and interpretation of results.
- Types of Swallowing Disorders: Become proficient in differentiating various dysphagia etiologies (neurological, structural, functional) and their impact on swallowing function.
- Management Strategies: Explore a range of therapeutic interventions, such as compensatory techniques, rehabilitative exercises, and nutritional modifications, tailored to individual patient needs.
- Medical Complications of Dysphagia: Understand the potential consequences of untreated dysphagia, such as aspiration pneumonia, malnutrition, dehydration, and their management.
- Interprofessional Collaboration: Discuss the importance of working effectively with other healthcare professionals (speech-language pathologists, physicians, dieticians, nurses) to provide holistic patient care.
- Evidence-Based Practice in Dysphagia: Familiarize yourself with current research and best practices in the assessment and management of swallowing disorders.
- Case Study Analysis: Practice analyzing complex cases, formulating differential diagnoses, and developing appropriate treatment plans.
- Ethical Considerations: Understand the ethical implications of providing care for patients with dysphagia, particularly regarding decision-making and informed consent.
Next Steps
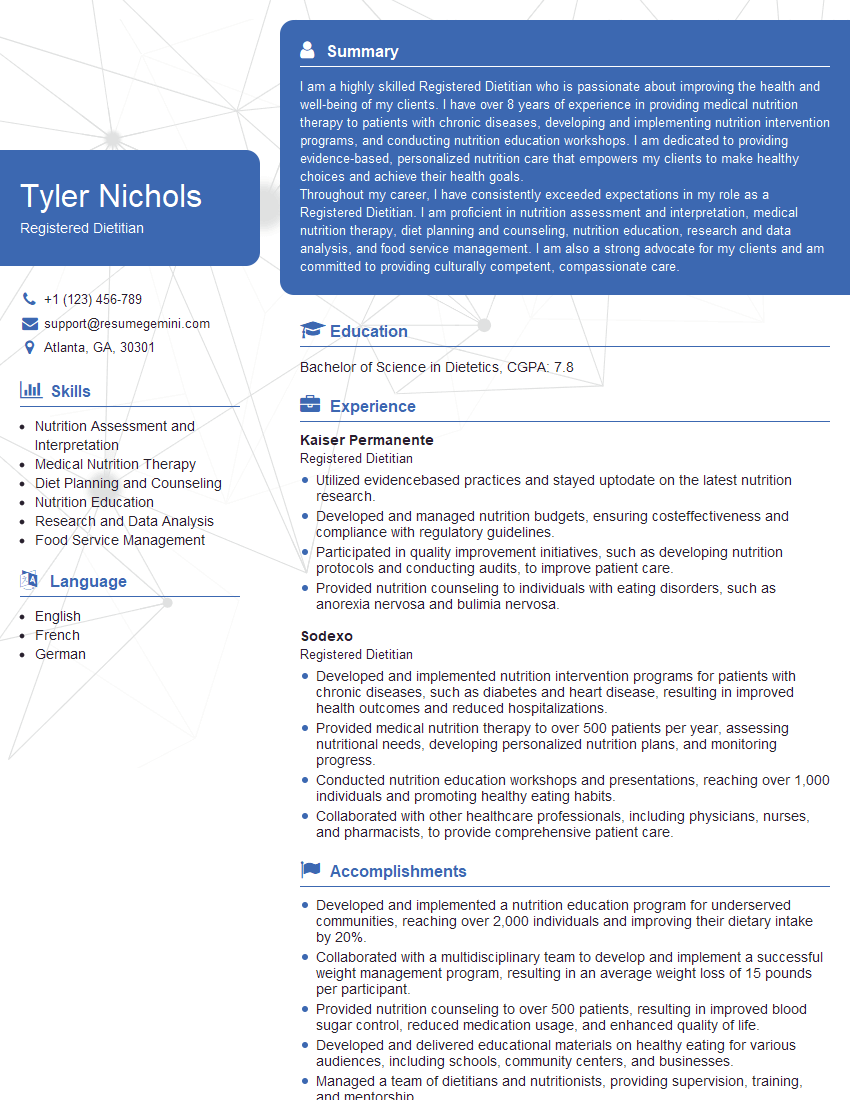
Mastering the complexities of swallowing disorders is crucial for a successful and rewarding career in this specialized field. A strong understanding of these concepts will significantly enhance your interview performance and open doors to exciting opportunities. To further strengthen your candidacy, crafting a compelling and ATS-friendly resume is paramount. ResumeGemini is a trusted resource that can help you build a professional resume that highlights your skills and experience effectively. Examples of resumes tailored to Swallowing Disorders professionals are available to guide you through the process. Invest time in building a strong resume – it’s your first impression and a key to unlocking your career potential.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.