Unlock your full potential by mastering the most common Flexible Laryngoscopy interview questions. This blog offers a deep dive into the critical topics, ensuring you’re not only prepared to answer but to excel. With these insights, you’ll approach your interview with clarity and confidence.
Questions Asked in Flexible Laryngoscopy Interview
Q 1. Describe the procedure for performing a flexible laryngoscopy.
Flexible laryngoscopy is a minimally invasive procedure used to visualize the larynx (voice box) and surrounding structures. It involves inserting a thin, flexible endoscope—a long, thin tube with a camera and light source—through the nose or mouth. The procedure allows for a detailed examination of the vocal cords, pharynx, and other areas of the upper airway. Here’s a step-by-step breakdown:
- Preparation: The patient is positioned comfortably, either sitting or lying down. Topical anesthetic spray is applied to numb the nasal passages or throat, minimizing discomfort.
- Insertion: The flexible endoscope is gently inserted through either the nose (nasal approach) or mouth (oral approach). The nasal approach often provides a clearer view but may be less comfortable for some patients.
- Visualization: The endoscope is carefully advanced to visualize the larynx. The physician manipulates the scope to obtain optimal views of the vocal cords, arytenoids, epiglottis, and other structures. The image is displayed on a monitor.
- Examination: During the examination, the physician assesses the vocal cord mobility, mucosal integrity, the presence of any lesions (tumors, ulcers, polyps), and the overall health of the airway. The patient may be asked to phonate (make sounds) or perform other maneuvers to assess vocal cord function.
- Removal: Once the examination is complete, the endoscope is gently withdrawn.
Imagine it like using a tiny, flexible camera to look inside the voice box. The images are highly detailed and allow for precise diagnosis.
Q 2. What are the different types of flexible laryngoscopes available?
Several types of flexible laryngoscopes are available, differing primarily in their image quality, features, and size. Common types include:
- Standard flexible endoscopes: These are the most common type, offering good image quality and are relatively easy to use.
- High-definition (HD) endoscopes: These endoscopes provide significantly improved image resolution, allowing for finer detail and better diagnosis, particularly of subtle lesions.
- Endoscopes with integrated stroboscopy: Stroboscopy is a technique that uses intermittent flashes of light to create the illusion of slow-motion vocal cord movement, allowing for a more detailed assessment of vocal cord vibration. This is invaluable for diagnosing voice disorders.
- Endoscopes with narrow-band imaging (NBI): NBI enhances the visualization of surface capillaries, which helps in the identification of precancerous lesions and early-stage cancers.
The choice of endoscope depends on the specific clinical needs and the physician’s preference. For example, an HD endoscope with stroboscopy would be ideal for a patient with voice problems, while a standard endoscope might suffice for a routine examination.
Q 3. Explain the indications for flexible laryngoscopy.
Flexible laryngoscopy is indicated for a wide range of conditions affecting the larynx and upper airway. Some common indications include:
- Hoarseness or voice changes: To identify the cause of voice problems, such as vocal cord nodules, polyps, or paralysis.
- Suspected laryngeal cancer or precancerous lesions: For early detection and diagnosis of cancerous or precancerous changes in the larynx.
- Dysphagia (difficulty swallowing): To evaluate swallowing function and identify any structural abnormalities that may be contributing to swallowing difficulties.
- Chronic cough: To rule out laryngeal causes of chronic cough.
- Respiratory distress: To assess the airway for any obstructions or abnormalities.
- Evaluation of suspected laryngopharyngeal reflux (LPR): To visualize the larynx and pharynx for signs of acid reflux.
- Pre-operative assessment: To evaluate the anatomy of the larynx before surgery.
In essence, whenever there’s a concern about the function or structure of the larynx, a flexible laryngoscopy can provide valuable diagnostic information.
Q 4. What are the contraindications for flexible laryngoscopy?
While generally safe, there are some contraindications to flexible laryngoscopy:
- Severe coagulopathy (bleeding disorders): The procedure carries a small risk of bleeding, so patients with severe bleeding disorders should be carefully evaluated before undergoing the procedure.
- Recent nasal surgery or trauma: A nasal approach may not be feasible if there’s recent nasal trauma or surgery.
- Uncooperative patient: The patient needs to be able to cooperate with the procedure; those who are severely agitated or uncooperative may require sedation or postponement.
- Severe airway obstruction: In cases of severe airway compromise, other methods of evaluation may be necessary.
Careful consideration of the patient’s overall health and specific situation is crucial in determining the suitability of the procedure.
Q 5. Describe the potential complications associated with flexible laryngoscopy.
Although rare, potential complications associated with flexible laryngoscopy include:
- Bleeding: Minor bleeding can occur from the nasal passages or throat, especially with the nasal approach.
- Infection: There’s a small risk of infection at the site of insertion.
- Laryngeal spasm: In rare instances, a spasm of the laryngeal muscles can occur, causing temporary difficulty breathing.
- Nausea or vomiting: This is more common with the oral approach and can be minimized with adequate topical anesthesia.
- Sinusitis (with nasal approach): Inflammation or infection of the sinuses can sometimes occur after a nasal examination.
- Adverse reaction to topical anesthetic: Although uncommon, some patients may experience allergic reactions to the anesthetic spray.
The physician should discuss these risks with the patient before the procedure. Most complications are minor and easily managed.
Q 6. How do you prepare a patient for a flexible laryngoscopy?
Patient preparation for flexible laryngoscopy is relatively straightforward but crucial for a successful and comfortable procedure. This usually involves:
- Informed consent: The physician should explain the procedure, risks, and benefits to the patient, and obtain informed consent.
- Fasting (if applicable): If sedation or general anesthesia is planned, the patient may need to fast for a specified period before the procedure.
- Medication review: The physician should review the patient’s medication list to identify any potential interactions or contraindications.
- Pre-procedure instructions: The patient should be instructed on what to expect during the procedure, including the use of topical anesthetic and any necessary post-procedure instructions.
For instance, explaining the sensation of the scope during nasal insertion can alleviate anxiety. Clear communication is key to a positive patient experience.
Q 7. How do you manage patient anxiety during a flexible laryngoscopy?
Managing patient anxiety is a critical aspect of providing a positive and safe experience during a flexible laryngoscopy. Strategies include:
- Thorough explanation: Clearly explaining the procedure, what the patient will feel, and what to expect can reduce anxiety significantly.
- Topical anesthesia: Adequate topical anesthesia can minimize discomfort and contribute to a more relaxed experience.
- Relaxation techniques: Teaching the patient simple relaxation techniques such as deep breathing can help reduce anxiety levels.
- Distraction techniques: Distraction techniques such as engaging in conversation or listening to music during the procedure can help minimize discomfort.
- Sedation (when appropriate): In cases of significant anxiety or if the patient has a low tolerance for discomfort, mild sedation may be appropriate.
I often find that a calm and reassuring approach, combined with clear communication and empathy, works best to build trust and alleviate anxiety. Remember, a relaxed patient tends to cooperate better, which improves the quality of the examination.
Q 8. Explain the different imaging techniques used with flexible laryngoscopy.
Flexible laryngoscopy, while primarily a visual examination, can be enhanced by incorporating various imaging techniques to improve diagnostic accuracy and visualization. The most common technique is still photography, capturing static images of the larynx. These images allow for detailed review and comparison over time. Beyond still images, videolaryngoscopy is extremely valuable. This records a video of the laryngeal structures during phonation (speech) and various maneuvers, providing a dynamic assessment of vocal fold movement and function. This is crucial for diagnosing voice disorders. Finally, stroboscopy is a highly specialized technique. It utilizes a rapidly pulsed light source synchronized with the vocal fold vibration, creating the illusion of slow-motion movement. This allows for precise analysis of vocal fold vibration patterns, identifying subtle asymmetries or abnormalities often missed with standard videolaryngoscopy.
Imagine trying to understand a hummingbird’s wings in flight – a still image wouldn’t suffice; you need the dynamic view of a video, and even then, stroboscopy offers the best slow-motion understanding.
Q 9. Describe the process of interpreting images obtained during flexible laryngoscopy.
Interpreting flexible laryngoscopy images requires a systematic approach. First, assess the overall laryngeal structure: Note the size, shape, and symmetry of the larynx, epiglottis, arytenoids, and vocal folds. Next, carefully examine the vocal folds themselves: Look for any lesions (masses, ulcers, nodules), redness, swelling, or any irregularities in their surface. Observe the color and mucosal wave (the wave-like motion of the vocal fold during vibration during stroboscopy). Assess the glottic closure: How well do the vocal folds come together during phonation? Any gaps or asymmetries could indicate a problem. We then correlate the findings with the patient’s symptoms (hoarseness, dysphagia, cough, etc.). For example, a reddish, swollen vocal fold with a reduced mucosal wave might suggest acute laryngitis, while a pale, irregular mass on the vocal fold might raise concerns for cancer.
Think of it as a detective work – gathering clues (visual findings) and putting them together to form a diagnosis.
Q 10. How do you differentiate between benign and malignant lesions using flexible laryngoscopy?
Differentiating benign and malignant lesions during flexible laryngoscopy is challenging and often requires a multidisciplinary approach. While flexible laryngoscopy provides crucial initial visual information, it alone is not definitive for cancer diagnosis. Benign lesions often appear as smooth, well-defined nodules or polyps, typically with a relatively normal vocal fold mucosa. Malignant lesions, conversely, tend to be irregular, ulcerated, or have an infiltrative appearance, often extending beyond the confines of the vocal fold. Their color can be varied, sometimes appearing white or pale. However, this is not always the case.
The key is to remember that suspicion of malignancy should prompt further investigations such as biopsy, computed tomography (CT) imaging, and magnetic resonance imaging (MRI) to confirm the diagnosis.
Q 11. How do you manage airway emergencies during flexible laryngoscopy?
Airway emergencies during flexible laryngoscopy are rare but require immediate action. The most common scenario involves laryngospasm or airway obstruction. The first step is to immediately remove the laryngoscope and reassure the patient. Administer oxygen by face mask. If the obstruction persists, cricothyroidotomy may be necessary in severe cases, or if other maneuvers like jaw thrust or suctioning are ineffective. Experienced medical personnel should be immediately alerted.
Preparation is key. Having emergency equipment readily available, such as suction, oxygen, and a tracheotomy kit, is crucial. The procedure should only be undertaken by suitably trained and experienced personnel with available support.
Q 12. What are the key anatomical landmarks visualized during a flexible laryngoscopy?
Key anatomical landmarks visualized during flexible laryngoscopy include: the epiglottis (the leaf-like structure at the entrance of the larynx), the arytenoid cartilages (small, paired cartilages that help regulate vocal fold movement), the vocal folds (the structures responsible for phonation), the ventricular folds (false vocal cords, superior to the true vocal folds), and the pyriform sinuses (lateral recesses of the hypopharynx). The valleculae, the spaces between the base of the tongue and epiglottis, are also visible. Understanding the relationships between these structures is fundamental to correct interpretation.
Think of it like learning a map – you need to know the main landmarks to navigate the territory.
Q 13. Explain the role of flexible laryngoscopy in diagnosing voice disorders.
Flexible laryngoscopy plays a pivotal role in diagnosing voice disorders. It allows direct visualization of the vocal folds, providing essential information about their structure, movement, and vibration. This helps identify various pathologies such as vocal nodules, polyps, cysts, laryngitis, and paralysis. The dynamic assessment offered by videostroboscopy is particularly useful in characterizing subtle abnormalities in vocal fold vibration, which are often the cause of voice disorders. For example, asymmetric vocal fold vibration can indicate muscle weakness or neurological problems. By linking the visual findings to the patient’s voice quality and symptoms, a precise diagnosis can be made.
Q 14. How does flexible laryngoscopy assist in diagnosing swallowing disorders?
While primarily used for evaluating the larynx, flexible laryngoscopy also assists in diagnosing swallowing disorders (dysphagia). By visualizing the pharyngeal structures during swallowing (with the help of video), we can assess the movement of the soft palate, epiglottis, and base of the tongue. We look for any signs of reduced or abnormal movement, such as incomplete pharyngeal constriction or reduced epiglottic inversion, that could lead to aspiration (food or liquid entering the airway). In addition, it may demonstrate anatomical abnormalities that might contribute to swallowing problems. This assessment is often part of a comprehensive assessment of swallowing disorders, complementing other tests such as a videofluoroscopic swallowing study.
Q 15. How do you use flexible laryngoscopy to guide treatment?
Flexible laryngoscopy provides a dynamic view of the upper airway, guiding treatment in several ways. It allows precise visualization of vocal cord lesions, allowing for targeted biopsies or laser treatments. For example, during a procedure to remove a vocal polyp, the flexible scope allows the surgeon to see exactly where the polyp is attached and precisely remove it, minimizing damage to surrounding tissue. Similarly, in cases of airway obstruction caused by swelling or foreign bodies, it enables precise assessment and guided placement of tools or medications. The flexibility also permits navigation around difficult anatomical structures, ensuring safe and effective treatment.
During airway procedures, the flexible scope allows real-time monitoring of the treatment’s effects. For instance, during a laser treatment for vocal fold lesions, the surgeon can assess the extent of the tissue removal and adjust treatment parameters accordingly. The scope can also be used to precisely place stents or other airway devices under direct visualization.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What are the advantages and disadvantages of flexible laryngoscopy compared to rigid laryngoscopy?
Both flexible and rigid laryngoscopy offer valuable insights into the larynx, but their applications differ based on the procedure’s needs.
- Flexible Laryngoscopy Advantages: Its flexibility allows for a less invasive examination, often performed in an office setting or under sedation rather than general anesthesia. It provides a natural view of vocal cord movement during phonation and offers superior visualization of the entire larynx and hypopharynx. It’s also suitable for patients who cannot tolerate a rigid scope.
- Flexible Laryngoscopy Disadvantages: Image quality can be slightly less sharp than rigid laryngoscopy, and it may not be as suitable for procedures requiring precise instrumentation within the larynx, such as complex surgical procedures.
- Rigid Laryngoscopy Advantages: Provides superior surgical access for precise instrument manipulation and better visualization of the glottis, beneficial during procedures like microlaryngoscopy.
- Rigid Laryngoscopy Disadvantages: Requires greater patient cooperation or general anesthesia. Can be more uncomfortable for the patient and limits the visualization of areas beyond the larynx.
In essence, the choice between the two depends on the clinical context and the specific needs of the patient and procedure.
Q 17. Describe your experience with different types of anesthesia used during flexible laryngoscopy.
My experience encompasses a wide range of anesthesia techniques employed during flexible laryngoscopy, tailoring the approach to the individual patient’s needs and the complexity of the procedure.
- Topical Anesthesia: For simple examinations, topical anesthesia, such as lidocaine spray or viscous lidocaine, is often sufficient to minimize discomfort. This approach is quick and easy, suitable for brief procedures.
- Local Anesthesia with Sedation: For more complex procedures, local anesthesia combined with intravenous sedation provides adequate comfort and patient cooperation without the risks associated with general anesthesia. This allows for patient interaction and monitoring of their comfort level throughout the procedure.
- General Anesthesia: In cases requiring extensive procedures, such as complex laser treatments or surgeries, general anesthesia is necessary to ensure patient comfort and immobility. This approach requires a skilled anesthesiologist to monitor vital signs and manage the patient’s airway during the procedure.
Selecting the appropriate anesthetic technique involves careful consideration of the patient’s medical history, the planned procedure, and available resources. My approach always prioritizes patient safety and comfort.
Q 18. How do you handle difficult intubations during flexible laryngoscopy?
Difficult intubations, though rare with flexible laryngoscopy, can arise due to anatomical variations or underlying pathology. My approach involves a systematic strategy:
- Assessment: A thorough pre-procedural evaluation including history, physical examination, and relevant imaging (e.g., prior neck surgery, anticipated difficulty with airway) is crucial.
- Alternative Airway Strategies: Familiarization with alternative airway management techniques, such as fiberoptic intubation with a rigid bronchoscope, is key.
- Image Guided Intubation: Flexible laryngoscopy itself facilitates visualization for guided intubation attempts.
- Experienced Team: Working with an experienced anesthesia team is critical in managing difficult intubations.
- Surgical Airway: If intubation fails despite attempts, a surgical airway may become necessary, a critical skill that necessitates preparation and a collaborative surgical team.
I prioritize a stepwise approach, escalating interventions only when necessary to ensure patient safety and the successful completion of the procedure. Every difficult intubation serves as a learning opportunity to refine my approach and enhance my skill set.
Q 19. Explain your proficiency in using advanced imaging techniques such as Narrow Band Imaging (NBI).
Narrow Band Imaging (NBI) significantly enhances the diagnostic capabilities of flexible laryngoscopy. NBI uses specific wavelengths of light to highlight the microvascular structure of tissues. This allows for the identification of subtle vascular patterns that are otherwise invisible with standard white light. This is particularly valuable for differentiating benign and malignant lesions. For example, NBI can help in detecting early signs of dysplasia or cancer in the larynx. The improved visualization of microvessels helps the clinician to distinguish subtle differences in vascularity, which can be indicative of pathology. This technology facilitates better diagnosis, improved treatment planning and, consequently, better patient outcomes.
My proficiency in using NBI includes not just performing the examination but also interpreting the images and integrating the findings with other clinical information to make a comprehensive diagnosis. It’s crucial to understand the limitations of NBI and use it in conjunction with other diagnostic modalities, like biopsy when necessary, to reach a conclusive diagnosis.
Q 20. Describe your experience with performing flexible laryngoscopy on pediatric patients.
Performing flexible laryngoscopy on pediatric patients requires specialized skills and a patient-centered approach. The key differences compared to adult procedures include:
- Smaller Instruments: Pediatric scopes are significantly smaller and more flexible than adult scopes, designed to accommodate the smaller airway of children.
- Anesthesia: General anesthesia is commonly used to ensure patient comfort and cooperation. The choice of anesthesia and the monitoring protocols are closely collaborated with pediatric anesthesiologists.
- Parental Involvement: Parental presence and reassurance during the procedure can reduce anxiety for both the child and the parent. Open and honest communication is crucial.
- Gentle Technique: A gentle and minimally invasive approach is essential to prevent trauma and ensure the child’s comfort and cooperation.
My experience working with pediatric patients includes performing various procedures, including evaluating vocal cord dysfunction, assessing airway patency and guiding treatment planning in cases of pediatric airway issues.
Q 21. How do you maintain the sterility and hygiene of the flexible laryngoscope?
Maintaining the sterility and hygiene of a flexible laryngoscope is paramount to prevent infection transmission. This involves a rigorous multi-step process:
- Pre-procedure Cleaning: Before each use, the scope undergoes a thorough cleaning with enzymatic detergent. This process aims to remove organic materials which are an essential step for effective disinfection.
- High-Level Disinfection: After cleaning, high-level disinfection is performed using a validated sterilant such as glutaraldehyde or a peracetic acid-based solution. This process ensures the inactivation of a wide range of microorganisms. Adherence to manufacturers’ instructions for contact time is crucial.
- Drying: Thorough drying is essential to prevent damage to the scope and to avoid potential contamination through residual moisture.
- Storage: The scope is then stored in a clean, dry, and dust-free environment to prevent contamination before the next use.
- Regular Maintenance: Regular checks of the scope’s integrity, including the light source and optics, are critical to ensure optimal performance and prevent potential infection risks.
Stringent adherence to these protocols is not only essential for patient safety but also ensures the longevity and effective use of the valuable equipment.
Q 22. What are the post-procedure instructions for patients undergoing flexible laryngoscopy?
Post-procedure instructions following a flexible laryngoscopy are crucial for patient comfort and recovery. They typically include advice on:
- Hydration: Encouraging plenty of fluids to help soothe the throat and prevent dehydration. I often recommend warm fluids like tea with honey (if tolerated) to ease any discomfort.
- Diet: Initially recommending a soft, bland diet to avoid irritating the throat. Spicy, acidic, or crunchy foods should be avoided for at least a few hours, and sometimes longer depending on the procedure and the patient’s response. I explain this clearly to each patient, tailoring the recommendation based on their specific needs.
- Voice Rest: Advising patients to minimize voice use for a specified period, usually several hours to a day, depending on the examination’s nature. Whispering can actually be more damaging than speaking normally, so I carefully explain the importance of complete rest.
- Pain Management: Providing guidance on managing any throat discomfort. This might include over-the-counter pain relievers like acetaminophen. If more significant pain occurs, I advise seeking further medical attention.
- Follow-up: Scheduling a follow-up appointment to review results and discuss any concerns. I ensure patients understand the importance of contacting my office if they experience unusual symptoms like bleeding, excessive pain, or difficulty breathing.
These instructions are always given verbally, confirmed in writing, and tailored to the individual patient’s circumstances and any pre-existing conditions.
Q 23. How do you document findings from a flexible laryngoscopy procedure?
Documentation of a flexible laryngoscopy is critical for patient care and legal protection. My documentation meticulously includes:
- Patient Demographics: Name, date of birth, medical record number.
- Reason for Procedure: Clearly stating the indication for the laryngoscopy – e.g., hoarseness, dysphagia, suspected vocal cord pathology.
- Procedure Details: The date, time, and type of anesthesia (if any) used. This also includes a note if it was a transnasal or transoral approach.
- Findings: A detailed description of the larynx’s appearance, including the vocal cords, epiglottis, arytenoids, and any other relevant structures. I use standardized terminology to ensure clarity. For example, instead of using subjective terms like ‘redness’, I will note ‘erythema’ and its location, and specify the vocal cord movement as ‘normal’, ‘limited’, or ‘absent’ and note if asymmetry is present.
- Images: If images or videos were taken during the procedure, I will always make sure they are correctly labelled and stored in the patient’s file. I usually provide a brief description of what each image is showing and correlate it with my written findings.
- Impression and Diagnosis: My interpretation of the findings and a provisional or confirmed diagnosis.
- Recommendations: Any recommended further investigations or treatment plans.
- Physician Signature and Date: Ensuring accurate attribution and accountability.
Using a structured approach to documentation ensures thoroughness, clarity, and minimizes the risk of errors or omissions.
Q 24. Describe your experience with troubleshooting equipment malfunctions during a flexible laryngoscopy.
Troubleshooting equipment malfunctions is an inherent part of flexible laryngoscopy. My approach is methodical and prioritizes patient safety. I’ve encountered situations like:
- Camera Issues: If the camera malfunctions (e.g., blurry image, no image), I first check the connections, ensuring proper attachment of the camera to the scope and the scope to the light source. I then assess the light source, checking for sufficient brightness and proper functionality. If the issue persists, I have a backup camera and scope readily available.
- Light Source Problems: If the light source fails, I immediately switch to a backup light source. This is a crucial step to ensure clear visualization of the larynx.
- Scope Malfunction: If the endoscope itself malfunctions (e.g., bending difficulties), I carefully and systematically assess the scope for visible damage. I always have a spare scope, and if needed, I would immediately terminate the procedure and reschedule.
My training emphasizes anticipating potential problems and having contingency plans in place. Patient safety is paramount – a compromised procedure is better than a compromised result, especially if an alternative assessment method (e.g. rigid laryngoscopy) can be employed.
Q 25. How do you stay updated on the latest advancements in flexible laryngoscopy techniques?
Staying current in flexible laryngoscopy necessitates continuous professional development. I actively engage in:
- Professional Organizations: Membership in organizations like the American Academy of Otolaryngology provides access to journals, conferences, and educational resources.
- Continuing Medical Education (CME): Regular participation in CME courses and webinars focused on advanced laryngoscopy techniques, image interpretation, and new technologies.
- Journal Articles: Regularly reviewing peer-reviewed journals like the American Journal of Otolaryngology and other relevant publications.
- Conferences and Workshops: Attending national and international conferences and workshops to learn from leading experts and network with colleagues.
- Mentorship and Collaboration: Engaging with experienced colleagues and mentors to share best practices and discuss challenging cases.
This multi-faceted approach ensures I’m consistently informed about innovations and best practices in the field.
Q 26. Discuss a challenging case involving flexible laryngoscopy and how you overcame the challenges.
One challenging case involved a patient with severe trismus (jaw stiffness) making transoral laryngoscopy extremely difficult. The initial attempt was unsuccessful due to the limited access. Instead of persisting with a method clearly causing the patient more distress, I collaborated with the anesthesiologist to carefully consider alternative approaches. We decided to attempt a transnasal approach. This required meticulous attention to detail and precise maneuvering of the endoscope to visualize the larynx adequately. The transnasal view was slightly more limited but sufficient to achieve the diagnostic goal. This ultimately allowed us to make a diagnosis and initiate appropriate treatment. This experience highlighted the importance of adaptability, collaboration, and prioritizing patient comfort.
Q 27. Explain your understanding of relevant legal and ethical considerations related to flexible laryngoscopy.
Legal and ethical considerations in flexible laryngoscopy are paramount. These include:
- Informed Consent: Obtaining informed consent from the patient, ensuring they understand the procedure, risks, benefits, and alternatives. I use plain language and answer all questions thoroughly.
- Confidentiality: Maintaining patient confidentiality, complying with HIPAA regulations, and protecting sensitive medical information. All patient information is treated with the strictest confidentiality.
- Proper Documentation: Maintaining accurate and complete medical records as already mentioned, which are essential for legal protection and continuity of care.
- Professional Boundaries: Maintaining professional boundaries and appropriate patient interactions.
- Competence: Ensuring competence and proficiency in performing the procedure. I regularly update my skills and participate in continued professional education.
- Appropriate use of sedation/anesthesia: If sedation or anesthesia is used, it must be administered by appropriately qualified medical personnel and the patient monitored appropriately.
Adherence to these ethical and legal standards is essential for responsible medical practice.
Q 28. Describe your teamwork skills within the context of a flexible laryngoscopy procedure.
Teamwork is vital in flexible laryngoscopy. Effective teamwork ensures patient safety and a smooth procedure. My role involves:
- Clear Communication: Maintaining open and clear communication with the anesthesiologist, nurses, and other medical personnel involved in the procedure. This includes pre-procedure planning, intra-procedure communication during the procedure, and post-procedure debriefing. Effective communication prevents miscommunication and ensures the safety of the patient.
- Coordination: Coordinating with the team to ensure everything runs smoothly and efficiently. This includes coordinating equipment, personnel and workflow.
- Respectful Collaboration: Respecting the expertise of each team member and valuing their contributions. I work as part of the team, rather than independently from them, and value and respect every member’s input.
- Delegation: Delegating tasks appropriately to qualified personnel.
A collaborative and respectful team dynamic creates a safe and efficient environment for the patient and enhances the overall quality of care. I believe a strong team leads to better outcomes.
Key Topics to Learn for Flexible Laryngoscopy Interview
- Anatomy and Physiology of the Larynx: Thorough understanding of the larynx’s structure, function, and relevant anatomical relationships.
- Flexible Laryngoscopy Technique: Mastering the proper insertion, manipulation, and withdrawal techniques for optimal visualization.
- Image Interpretation: Accurately identifying normal and abnormal laryngeal findings, including vocal cord pathology, masses, and inflammation.
- Indications and Contraindications: Knowing when flexible laryngoscopy is appropriate and when alternative procedures should be considered.
- Patient Preparation and Post-Procedure Care: Understanding the necessary steps to ensure patient comfort and safety before, during, and after the procedure.
- Troubleshooting Common Issues: Developing problem-solving skills to address challenges such as difficult intubation, equipment malfunction, or patient discomfort.
- Comparative Analysis with Rigid Laryngoscopy: Understanding the advantages and limitations of flexible laryngoscopy compared to rigid techniques.
- Documentation and Reporting: Accurately documenting findings and communicating effectively with colleagues and referring physicians.
- Safety Protocols and Infection Control: Adhering to strict safety protocols and infection control measures to minimize risks.
- Ethical Considerations: Understanding and applying ethical principles related to patient consent, confidentiality, and informed decision-making.
Next Steps
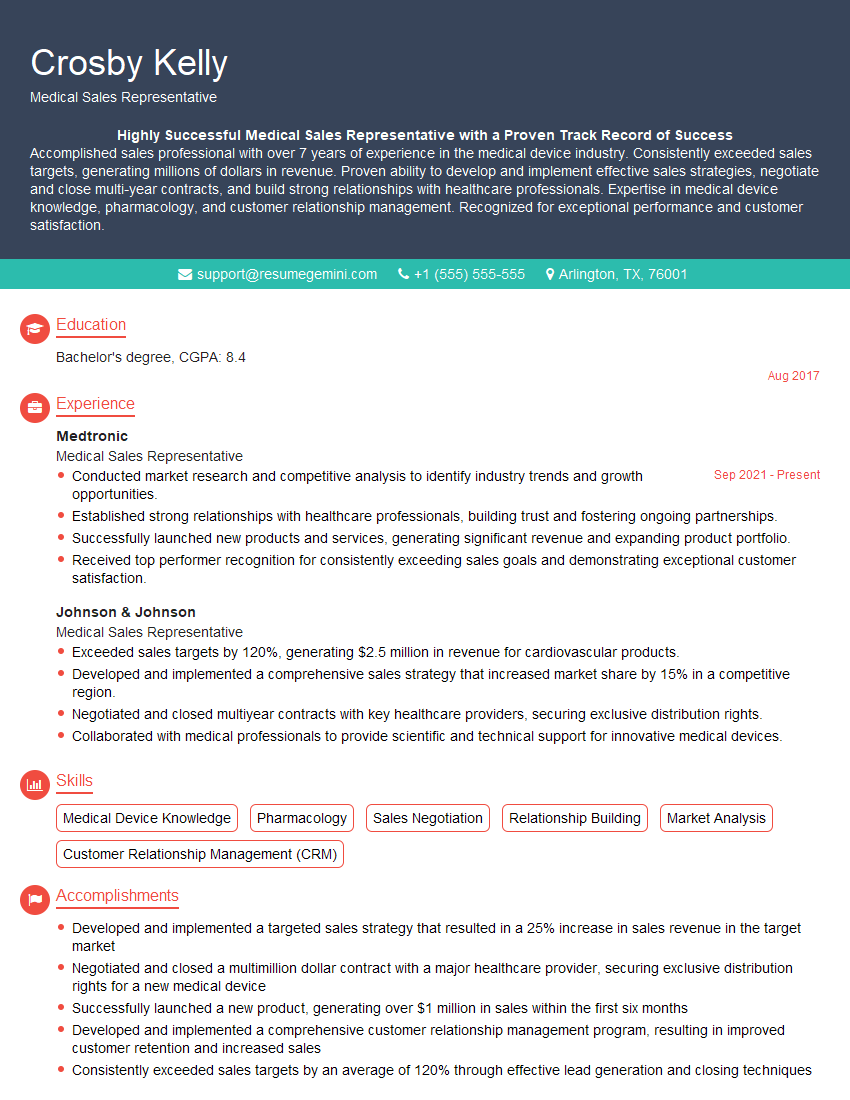
Mastering flexible laryngoscopy significantly enhances your career prospects in various medical fields. It opens doors to specialized roles and demonstrates advanced clinical skills. To maximize your chances of securing your dream position, it’s crucial to have a well-crafted, ATS-friendly resume that highlights your expertise. We strongly encourage you to leverage ResumeGemini, a trusted resource for building professional resumes. ResumeGemini can help you present your qualifications effectively, and we provide examples of resumes tailored to flexible laryngoscopy to help guide you. Invest time in crafting a compelling resume – it’s your first impression with potential employers.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.