Interviews are opportunities to demonstrate your expertise, and this guide is here to help you shine. Explore the essential Esophagoscopy interview questions that employers frequently ask, paired with strategies for crafting responses that set you apart from the competition.
Questions Asked in Esophagoscopy Interview
Q 1. Describe the procedure of an esophagoscopy.
Esophagoscopy is a procedure where a thin, flexible tube with a camera and light (an esophagoscope) is inserted down the throat to visualize the esophagus, the tube that connects the mouth to the stomach. It allows for direct examination of the esophageal lining, enabling the detection of various abnormalities. The procedure usually involves the patient lying on their back, receiving a local anesthetic spray in the throat to numb the area and sometimes mild sedation. The doctor then gently advances the scope, observing the esophageal walls for any signs of disease. Biopsies (tissue samples) can be taken during the procedure for further investigation if needed. After the examination, the scope is carefully withdrawn.
Think of it like using a tiny, high-tech camera to inspect the inside of a pipe. The images are displayed on a monitor allowing the doctor to see exactly what’s happening inside the esophagus.
Q 2. What are the indications for performing an esophagoscopy?
Esophagoscopy is indicated for a wide range of esophageal conditions. Some key indications include:
- Dysphagia (difficulty swallowing): This is a common reason, as it can indicate blockages, narrowing, or inflammation.
- Odynophagia (painful swallowing): Painful swallowing warrants investigation to rule out serious issues like ulcers or tumors.
- Esophageal reflux disease (GERD): Esophagoscopy can help assess the severity of GERD and identify any complications like Barrett’s esophagus.
- Investigation of bleeding: If a patient is experiencing unexplained vomiting of blood or blood in their stool, esophagoscopy can pinpoint the source.
- Diagnosis of esophageal tumors or masses: Esophagoscopy allows for direct visualization of suspected lesions and allows for biopsies to be taken.
- Foreign body removal: If a patient has swallowed something they shouldn’t have (e.g., a coin, bone), an esophagoscopy can be used to remove it safely.
- Assessment of esophageal varices: These are swollen veins in the esophagus, often seen in patients with liver disease. Esophagoscopy helps assess their size and risk of bleeding.
The decision to perform an esophagoscopy is based on the patient’s symptoms, medical history, and other diagnostic test results.
Q 3. What are the contraindications for esophagoscopy?
While relatively safe, there are certain situations where esophagoscopy is contraindicated or should be approached with extreme caution. These include:
- Severe uncompensated cardiovascular disease: Patients with unstable heart conditions may not tolerate the procedure.
- Uncontrolled bleeding disorders: The risk of bleeding during and after the procedure would be significantly increased.
- Recent myocardial infarction (heart attack): The stress of the procedure could be detrimental.
- Severe respiratory distress: Patients with compromised respiratory function may have difficulty tolerating the procedure.
- Certain esophageal conditions that might increase the risk of perforation: For example, a very narrow or fragile esophagus.
- Patient refusal or inability to cooperate: The procedure requires patient cooperation.
In these cases, alternative diagnostic methods might be considered or the procedure might be postponed until the patient’s condition improves.
Q 4. List the potential complications associated with esophagoscopy.
Esophagoscopy, while generally safe, carries potential complications, although they are infrequent. These include:
- Perforation (hole in the esophagus): This is a serious complication requiring immediate intervention.
- Bleeding: Biopsies and manipulation of the scope can cause bleeding, usually minor but can be significant in some cases.
- Infection: Infection is a risk with any invasive procedure, though less common with proper sterilization techniques.
- Aspiration pneumonia: Accidental inhalation of fluids or secretions during the procedure.
- Tooth damage: This is possible during insertion of the scope.
- Adverse reactions to anesthesia or sedation: Reactions to medications used during the procedure can occur, although rare.
- Esophageal perforation can lead to mediastinitis (infection of the mediastinum) or sepsis (life-threatening blood infection).
It is important to note that these complications are relatively rare, and the benefits of the procedure usually outweigh the risks.
Q 5. How do you manage a perforation during an esophagoscopy?
Esophageal perforation during esophagoscopy is a serious medical emergency. Management requires immediate action. The first step involves stopping the procedure immediately. The patient needs to be stabilized, which involves monitoring vital signs, managing pain, and administering intravenous fluids. The next step involves a thorough assessment of the perforation’s location and severity. This usually involves imaging studies such as a chest x-ray and computed tomography (CT) scan. Treatment strategies depend on the severity and location of the perforation. Options include:
- Conservative management: In some cases, with small perforations and no signs of infection, conservative management with intravenous antibiotics, bowel rest (nothing by mouth), and close monitoring might be sufficient.
- Surgical repair: For larger perforations or those with signs of infection, surgical repair is usually necessary to close the hole and prevent complications like mediastinitis.
- Endoscopic intervention: In select cases, endoscopic techniques such as placement of clips or stents might be used to close the perforation.
The patient’s condition, the size and location of the perforation and the presence or absence of infection will dictate the most appropriate management strategy.
Q 6. What are the different types of esophagoscopes?
Esophagoscopes come in different types, primarily categorized by their flexibility and features:
- Rigid esophagoscopes: These are older, less flexible scopes offering better visualization in some cases. They are usually used for procedures requiring more precision, such as foreign body removal.
- Flexible esophagoscopes: These are the more commonly used type today. Their flexibility allows for easier navigation of the esophagus and makes the procedure less uncomfortable for the patient. They allow for better visualization and are better suited for procedures involving taking biopsies.
- Video esophagoscopes: These are flexible scopes equipped with a small camera and a light source, providing real-time images on a monitor. The video image significantly improves visualization and documentation.
The choice of esophagoscope depends on the indication of the procedure and the doctor’s preference.
Q 7. Explain the process of preparing a patient for esophagoscopy.
Preparing a patient for esophagoscopy is crucial for a successful and safe procedure. The process typically involves:
- Informed consent: The patient needs to understand the procedure, its benefits, risks, and potential complications. They must sign a consent form before proceeding.
- Fasting: Patients are usually instructed to fast for at least 6-8 hours before the procedure to minimize the risk of aspiration (inhalation of stomach contents into the lungs).
- Medications: The physician may request that the patient stops taking certain medications, such as anticoagulants (blood thinners), if appropriate. This reduces the risk of bleeding.
- Sedation (optional): Sedation can be used to help patients relax and make the procedure more comfortable. It is typically a mild sedative administered intravenously.
- Preoperative assessment: A complete medical history, physical examination, and review of relevant laboratory results are necessary to assess the patient’s fitness for the procedure.
- Monitoring vital signs: Patient vital signs (heart rate, blood pressure, oxygen saturation) are monitored during and after the procedure.
Thorough preparation significantly contributes to patient comfort and safety during the procedure.
Q 8. How do you interpret the findings of an esophagoscopy?
Interpreting esophagoscopy findings involves a systematic approach, combining direct visualization with any collected biopsies. We start by assessing the overall esophageal mucosa – its color, texture, and integrity. We look for any abnormalities such as:
- Lesions: Ulcers, strictures (narrowing), masses, or varices (swollen veins). Their location, size, and appearance are meticulously documented. For example, a shallow, well-demarcated ulcer might suggest a benign condition, while a deep, irregular ulcer could raise suspicion for malignancy.
- Inflammation: Erythema (redness), edema (swelling), friability (easy bleeding), or the presence of exudates (pus) indicate inflammation, potentially from reflux, infection, or other causes. The extent and distribution of inflammation are crucial.
- Structural abnormalities: We assess for esophageal rings or webs, which are tissue constrictions; hiatal hernias, where part of the stomach protrudes into the chest; and esophageal diverticula, which are pouch-like outpouchings of the esophageal wall.
Biopsy results are then integrated. Histopathology (microscopic examination of tissue) reveals the cellular composition of any suspicious lesions, allowing for definitive diagnosis of conditions such as Barrett’s esophagus, esophagitis, or cancer. The entire process is carefully documented with photos and videos for later review and comparison.
Q 9. Describe the process of obtaining biopsies during esophagoscopy.
Biopsy acquisition during esophagoscopy is a straightforward yet crucial procedure. Once a suspicious area is identified, the endoscope’s biopsy forceps are carefully advanced. The process involves:
- Target selection: The area requiring biopsy is carefully visualized and selected.
- Forceps insertion: The biopsy forceps are gently introduced into the esophagus, avoiding excessive pressure to prevent perforation (a hole in the esophageal wall).
- Tissue acquisition: The forceps are opened and closed to obtain a tissue sample. Multiple biopsies might be needed depending on the lesion’s size and characteristics. The goal is to obtain representative samples while minimizing trauma.
- Specimen handling: The biopsy is carefully removed and placed in a suitable container with fixative, ensuring proper labeling to maintain sample integrity and facilitate accurate pathological analysis.
The procedure is typically well-tolerated, but it’s crucial to take precautions to avoid complications. The procedure is frequently guided by chromoendoscopy, where dye is used to highlight suspicious tissue, making biopsy more efficient and precise.
Q 10. How do you manage bleeding during an esophagoscopy?
Managing bleeding during esophagoscopy depends on the severity and source. Mild bleeding can often be managed conservatively with careful observation. More significant bleeding necessitates intervention:
- Hemostasis with clips or injections: Small bleeding vessels can often be controlled by placing endoscopic clips or injecting hemostatic agents (like epinephrine) directly into the bleeding site. This is a minimally invasive technique.
- Thermal coagulation: Using heat (argon plasma coagulation or bipolar electrocautery) can seal off the bleeding vessels. This method is effective for smaller vessels and superficial bleeding.
- Surgical intervention: In cases of uncontrollable or severe bleeding, immediate surgical intervention might be necessary to control the bleeding and repair the esophageal wall.
The approach is tailored to the individual patient, considering factors such as the patient’s overall health, the extent of bleeding, and the underlying cause. Post-procedure monitoring is vital, especially for patients with significant bleeding.
Q 11. What are the key differences between upper endoscopy and esophagoscopy?
Upper endoscopy and esophagoscopy are closely related but distinct procedures. Upper endoscopy examines the entire upper gastrointestinal tract, including the esophagus, stomach, and duodenum (the first part of the small intestine). Esophagoscopy focuses solely on the esophagus.
- Scope used: Both use endoscopes, but the length and design may differ slightly, optimizing visualization for the specific region.
- Extent of examination: Upper endoscopy provides a broader view of the upper GI tract, while esophagoscopy is limited to the esophagus. This means an esophagoscopy might be part of a broader upper endoscopy.
- Indications: Esophagoscopy is usually performed when there is a specific concern about the esophagus, such as dysphagia (difficulty swallowing), esophageal pain, or abnormal findings on imaging studies. Upper endoscopy has a wider range of indications including investigation of gastrointestinal bleeding, abdominal pain, and suspected ulcers.
Think of it like this: esophagoscopy is a focused exam of the esophagus, while upper endoscopy is a more comprehensive exam of the upper GI tract.
Q 12. Explain the use of different imaging modalities in conjunction with esophagoscopy.
Various imaging modalities can enhance esophagoscopy. They often provide additional information or aid in guiding the procedure:
- Fluoroscopy: Real-time X-ray imaging allows for visualization of the endoscope’s position and the esophageal anatomy, especially helpful in identifying and navigating through strictures or abnormal structures. It is particularly useful when dealing with foreign bodies or perforation.
- Endoscopic ultrasound (EUS): EUS combines endoscopy with ultrasound, offering detailed images of the esophageal wall and surrounding tissues. This is invaluable in staging esophageal cancer or detecting early lesions that might be missed on standard endoscopy.
- Narrow band imaging (NBI): NBI enhances the visualization of mucosal microvessels, aiding in the detection of subtle changes suggestive of dysplasia (precancerous changes) or early neoplasia (tumors).
- Chromoendoscopy: The use of dyes such as methylene blue or indigo carmine improves the visualization of lesions by highlighting abnormal areas, aiding in biopsy targeting.
The choice of imaging modality depends on the clinical scenario and the specific information needed. For example, EUS is crucial in staging esophageal cancer, while NBI can be useful in the surveillance of Barrett’s esophagus.
Q 13. How do you address patient anxiety before an esophagoscopy?
Addressing patient anxiety before esophagoscopy is crucial for a successful procedure. It involves a combination of strategies:
- Thorough explanation: Clearly explaining the procedure, its purpose, and the expected sensations helps alleviate anxiety by reducing uncertainty. Using simple language and avoiding medical jargon are key. A demonstration of the equipment can be helpful for some patients.
- Pre-procedure sedation: Offering appropriate sedation medication, such as midazolam, can significantly reduce anxiety and discomfort during the procedure.
- Empathetic communication: Active listening, validating patient concerns, and addressing their questions with patience and understanding create a trusting environment. Providing emotional support and reassuring the patient of their safety is essential.
- Distraction techniques: During the procedure, distraction techniques such as conversation or music may help the patient relax.
A calm and reassuring demeanor from the healthcare team is vital in minimizing patient anxiety. Preparing the patient thoroughly is a vital aspect of minimizing anxiety and leading to a smooth and successful procedure.
Q 14. What are the post-procedure instructions for patients after esophagoscopy?
Post-procedure instructions are critical for patient safety and recovery after esophagoscopy. These typically include:
- Diet: A clear liquid diet initially, gradually progressing to a soft diet as tolerated, helps prevent discomfort or injury to the esophagus. This is gradually advanced to normal foods unless there is a reason not to do so.
- Medication: Any prescribed medications, such as pain relievers or antibiotics, should be taken as directed.
- Activity: Rest is recommended initially, with gradual resumption of normal activities as tolerated. Strenuous activity should be avoided until completely recovered.
- Monitoring for complications: Patients should be aware of potential complications such as bleeding, perforation (hole in the esophagus), or infection and seek immediate medical attention if they experience any concerning symptoms, such as severe abdominal pain, difficulty breathing or swallowing, or signs of infection.
- Follow-up: A follow-up appointment is usually scheduled to discuss the results and further management.
Clear and concise instructions, provided both verbally and in writing, help patients understand and follow the recommendations, promoting a safe and comfortable recovery.
Q 15. Describe your experience with difficult intubations during esophagoscopy.
Difficult intubations during esophagoscopy can be challenging, often stemming from anatomical variations, patient factors (e.g., obesity, cervical spine disease), or previous surgeries. I’ve encountered situations where the esophagus was unusually narrow or tortuous, making advancement of the endoscope difficult. In such cases, careful manipulation with gentle pressure is crucial. I utilize various techniques including adjusting the endoscope’s insertion angle, employing different endoscopes (e.g., thinner endoscopes or those with better maneuverability), and utilizing topical anesthesia and sedation as needed to optimize patient comfort and tolerance. If I encounter significant resistance, I always prioritize patient safety and may consider alternative approaches such as fluoroscopy guidance or seeking a second opinion from a more experienced colleague before proceeding if a safe advancement is impossible. One particularly memorable case involved a patient with severe cervical spondylosis, where using fluoroscopy was essential for navigating the challenging anatomy.
My approach always emphasizes a patient-first strategy focusing on minimizing discomfort and avoiding trauma. A systematic assessment of the patient’s history, including prior procedures or conditions affecting the upper gastrointestinal tract, is crucial for anticipating potential difficulties.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you differentiate between esophageal varices and other lesions during esophagoscopy?
Differentiating esophageal varices from other lesions during esophagoscopy relies on a combination of visual characteristics and clinical context. Esophageal varices typically appear as bluish, tortuous, dilated submucosal veins, often located in the lower esophagus. They tend to bleed easily. Other lesions, such as ulcers, tumors, or inflammatory lesions, present with distinct appearances. Ulcers often have a central crater, while tumors may have irregular borders and may protrude into the esophageal lumen. Inflammatory changes can manifest as erythema, edema, or friability of the esophageal mucosa. I use high-resolution endoscopy, including chromoendoscopy (dye-enhanced imaging), to better visualize vascular patterns, enhancing the differentiation. The size, location, and appearance of the lesion in conjunction with the patient’s history and other clinical findings, such as liver function tests, are crucial in reaching the correct diagnosis. For example, a patient with cirrhosis and portal hypertension makes esophageal varices a far more likely diagnosis than other types of lesions. Biopsy is often necessary for definitive diagnosis, especially in ambiguous cases.
Q 17. Explain your experience with esophageal stenting procedures.
I have extensive experience with esophageal stenting procedures, primarily for malignant esophageal strictures and benign esophageal obstructions. The procedure involves careful selection of the appropriate stent type and size, guided by the lesion’s location, length, and shape, as well as the patient’s overall health. The procedure requires meticulous placement to ensure adequate coverage of the stricture without causing undue pressure or complications such as perforation. I utilize fluoroscopy to guide stent placement, ensuring accurate positioning and avoiding unnecessary complications. Post-procedure monitoring is crucial to assess stent patency and identify any complications such as migration, bleeding, or infection. Follow-up endoscopy is often scheduled to evaluate the stent’s effectiveness and address any issues that may arise. For instance, I recall a case where a patient with a malignant esophageal stricture experienced significant dysphagia relief following stent placement, allowing for improved quality of life.
Q 18. How do you manage esophageal foreign bodies during esophagoscopy?
Management of esophageal foreign bodies during esophagoscopy depends heavily on the nature of the foreign body, its location, and the patient’s clinical status. For simple, easily grasped objects, direct removal with forceps or a retrieval basket is often possible. More challenging cases, involving sharp or irregular objects, may require specialized techniques or the use of a snare or other specialized instruments for safe removal. Careful attention is paid to avoiding perforation during the retrieval process. In cases of impacted objects, gentle manipulation and dilation may be necessary. The patient’s overall condition and vital signs are monitored throughout the procedure. I recall a case where a child swallowed a coin that was lodged in the mid-esophagus. It was removed easily with forceps under direct visualization.
Q 19. What is your approach to diagnosing and treating esophageal cancer using esophagoscopy?
Esophagoscopy plays a vital role in the diagnosis and staging of esophageal cancer. During the procedure, suspicious lesions are identified visually. Biopsies are taken for histopathological examination to confirm malignancy and determine the type and grade of the cancer. Endoscopic ultrasound (EUS) can then be used to assess the depth of tumor invasion and the involvement of surrounding lymph nodes. This helps to determine the stage of the cancer, guiding treatment decisions. Treatment options can range from surgery and chemotherapy to radiation therapy or a combination of these modalities. Esophagoscopy also plays an important role in assessing treatment response and in detecting recurrence. This is a complex multi-disciplinary approach, and I always work closely with surgeons, oncologists, and radiologists to ensure optimal patient care.
Q 20. How do you document the findings of an esophagoscopy?
Documentation of an esophagoscopy is crucial for accurate medical record-keeping and continuity of care. My reports always include a detailed description of the endoscopic findings, noting the presence of any lesions, their location, size, appearance, and any other significant observations. Biopsy results and any other procedures performed, such as stent placement or foreign body removal, are documented meticulously. Findings are correlated with the pre-procedure indications and clinical context. High-quality images are also included as part of the report to support the findings. The report concludes with a summary of the findings, diagnosis, and recommendations for further management. This comprehensive approach guarantees consistent, clear communication among medical professionals involved in the patient’s care.
Q 21. Describe your experience with various types of esophageal disorders.
My experience encompasses a wide range of esophageal disorders. I’ve managed patients with various conditions including esophageal reflux disease (GERD), Barrett’s esophagus, eosinophilic esophagitis, peptic strictures, esophageal varices, diverticula, and a variety of benign and malignant tumors. Each condition requires a tailored approach based on the patient’s symptoms, the endoscopic findings, and the results of any further investigations. This may involve medical therapy, endoscopic interventions, or surgical management. I approach each case with a patient-centered philosophy, involving them in the decision-making process and providing clear explanations about the condition and the best course of action. For example, a patient with GERD may respond well to lifestyle modifications and medication, whereas a patient with a significant esophageal stricture might require dilation or stent placement.
Q 22. Explain your experience with esophageal dilation procedures.
Esophageal dilation is a procedure I perform frequently to treat esophageal strictures – narrowings of the esophagus that can make swallowing difficult. The process involves carefully widening the narrowed section using specialized dilators, gradually increasing the size until a satisfactory diameter is achieved. I use various techniques depending on the stricture’s severity and location. For example, pneumatic dilation uses an inflatable balloon to widen the stricture, while bougie dilation involves passing progressively larger dilators through the narrowed area. The choice depends on factors such as the length and severity of the stricture, and the patient’s overall health. I always prioritize patient comfort and safety, ensuring adequate anesthesia and meticulous monitoring throughout the procedure. For instance, in a patient with a long, complex stricture, I might prefer a phased approach using bougie dilation over several sessions to minimize the risk of perforation. Post-procedure, I closely monitor the patient for any signs of bleeding, perforation, or dysphagia. Regular follow-up endoscopies are essential to assess the effectiveness of the dilation and manage any recurrence.
Q 23. What are the key safety measures to prevent complications during esophagoscopy?
Safety during esophagoscopy is paramount. My key safety measures begin with a thorough patient assessment to identify any potential risks. This includes reviewing the patient’s medical history, current medications, and coagulation status. We utilize advanced equipment such as high-resolution endoscopes with improved maneuverability and visualization. Proper sedation and monitoring are crucial. I use a combination of monitored anesthesia care (MAC) or general anesthesia tailored to the patient’s condition and the procedure’s complexity. During the procedure, gentle manipulation of the endoscope is key to minimize trauma to the esophageal mucosa. Continuous monitoring of vital signs including heart rate, blood pressure, oxygen saturation, and end-tidal CO2 are essential. Furthermore, we strictly adhere to sterile techniques to prevent infection. Immediate availability of emergency equipment and personnel, including trained personnel skilled in airway management, is vital. Finally, a comprehensive post-procedure assessment, including careful observation for bleeding or perforation, is a critical safety measure.
Q 24. How do you maintain the equipment used for esophagoscopy?
Maintaining the equipment used for esophagoscopy is vital for ensuring accurate diagnostics and patient safety. After each procedure, the endoscope undergoes a thorough cleaning and disinfection process, following strict guidelines established by the manufacturer and infection control protocols. This involves enzymatic cleaning, high-level disinfection, and rinsing. The endoscope is then carefully inspected for any damage. Regular calibration and maintenance checks are scheduled to ensure optimal performance. We use automated endoscope reprocessors (AERs) to ensure consistent and effective cleaning and disinfection. Documentation of all cleaning and maintenance procedures is meticulously maintained for quality control and tracking purposes. Any malfunctioning equipment is immediately taken out of service and sent for repair or replacement.
Q 25. What are your preferred methods for sedation during esophagoscopy?
My preferred methods for sedation during esophagoscopy depend on individual patient needs and the procedure’s complexity. For straightforward procedures, I often use monitored anesthesia care (MAC) with intravenous sedation, allowing patients to remain responsive while minimizing discomfort. This commonly involves a combination of midazolam and fentanyl. For more complex procedures or patients with anxiety, general anesthesia is employed. The choice is made in consultation with the anesthesiologist based on a comprehensive assessment of the patient’s physical status, medical history, and psychological profile. The goal is always to provide the optimal level of sedation to ensure patient comfort and safety without compromising the procedure’s successful completion.
Q 26. How do you assess patient suitability for esophagoscopy?
Assessing patient suitability for esophagoscopy involves a comprehensive evaluation. This includes a thorough review of the patient’s medical history, focusing on conditions such as bleeding disorders, recent myocardial infarction, or uncontrolled hypertension, all of which can increase the risk of complications. A physical examination is performed to assess the patient’s overall health. We also consider their ability to cooperate with the procedure, as well as any potential swallowing difficulties. Appropriate blood tests may be necessary to evaluate coagulation status and liver function. In some cases, a chest X-ray or other imaging studies may be needed to evaluate the anatomy and rule out any unexpected findings. Informed consent is obtained after explaining the procedure, its benefits, risks, and potential complications. Patients are made fully aware of the alternative options available.
Q 27. Describe a challenging esophagoscopy case and how you handled it.
One challenging case involved a patient with a very long and tortuous esophageal stricture secondary to corrosive ingestion years prior. Standard dilation techniques were ineffective and posed a significant risk of perforation. To overcome this, I utilized a combination of techniques. Initially, we used a small-caliber guide wire to carefully navigate the stricture. Then, we used sequential dilation with multiple sizes of bougies, gradually increasing the diameter while closely monitoring for signs of perforation or bleeding. We spread the dilation sessions over several weeks to allow for healing and tissue remodeling between sessions. This multi-stage approach, coupled with close post-procedure monitoring and careful management of potential complications, resulted in a successful outcome, restoring the patient’s ability to swallow normally. This highlights the importance of a flexible approach and the adaptation of techniques to individual patient needs.
Q 28. What are your continuing education efforts related to esophagoscopy?
Continuing education is critical in the rapidly evolving field of esophagoscopy. I actively participate in professional conferences and workshops, staying current with the latest advancements in endoscopic techniques, instrumentation, and treatment modalities. I also regularly review peer-reviewed journals and publications to expand my knowledge base. Furthermore, I participate in case-based discussions and collaborative learning sessions with colleagues to share experiences and improve our collective expertise. These ongoing efforts ensure that I consistently maintain the highest standards of care for my patients.
Key Topics to Learn for Esophagoscopy Interview
- Instrumentation and Technique: Understanding the various types of endoscopes, insertion techniques, and maneuvering within the esophagus. Practice explaining the procedure step-by-step.
- Patient Assessment and Preparation: Discuss pre-procedure evaluations, including patient history, medication reconciliation, and informed consent. Explain how to identify and mitigate potential risks.
- Indications and Contraindications: Clearly articulate the medical reasons for performing an esophagoscopy and situations where it’s contraindicated. Be prepared to discuss differential diagnoses.
- Complications and Management: Review potential complications such as perforation, bleeding, and aspiration. Explain how to recognize and manage these complications effectively.
- Diagnostic Applications: Describe how esophagoscopy is used to diagnose esophageal disorders, such as Barrett’s esophagus, esophageal cancer, and esophageal varices. Discuss the interpretation of findings.
- Therapeutic Applications: Explain the therapeutic uses of esophagoscopy, including dilation of strictures, removal of foreign bodies, and laser therapy.
- Biopsy and Histopathology: Understand the techniques for obtaining esophageal biopsies and interpreting histological results. Discuss the importance of proper sample collection and handling.
- Post-Procedure Care: Describe the necessary post-procedure monitoring and instructions for patients. Discuss potential recovery complications and their management.
- Advanced Techniques: Explore more advanced techniques such as endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD) if applicable to your experience level.
- Ethical and Legal Considerations: Understand the ethical implications of the procedure and relevant legal aspects regarding informed consent and patient confidentiality.
Next Steps
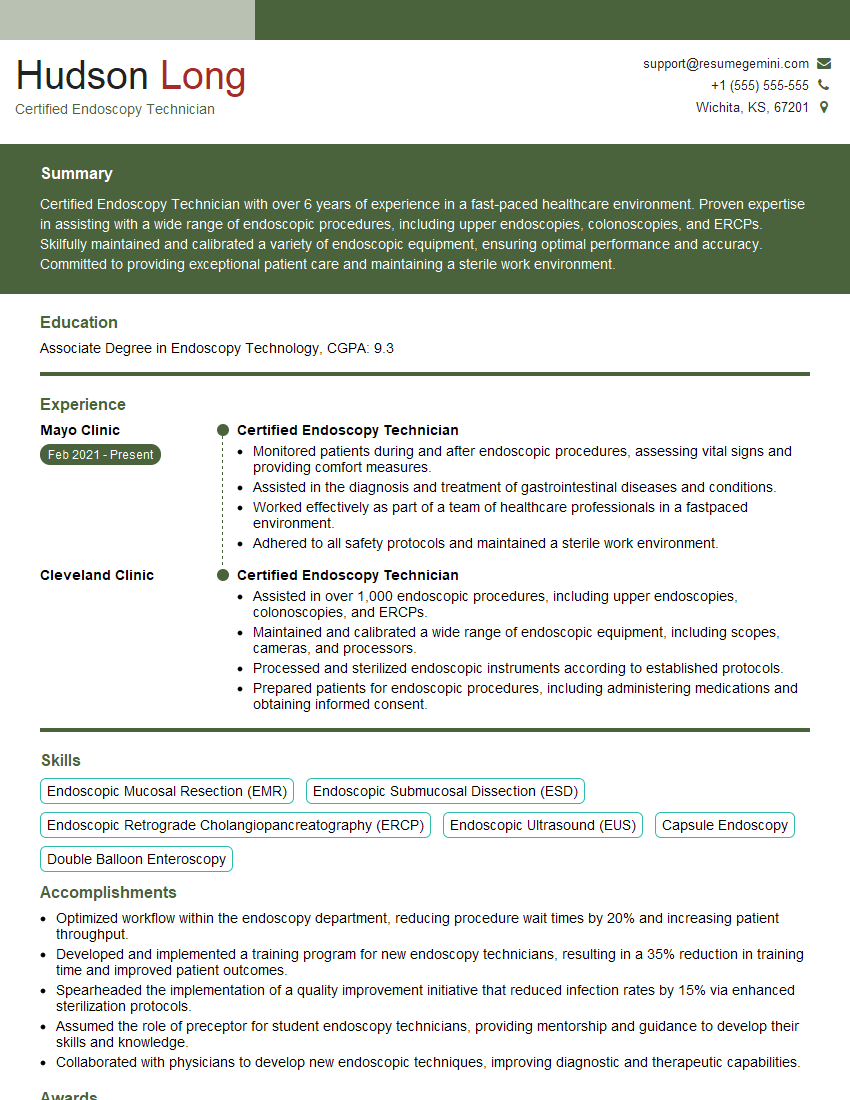
Mastering Esophagoscopy significantly enhances your career prospects in gastroenterology and related fields. It opens doors to specialized roles and positions of greater responsibility. To maximize your chances of landing your dream job, a strong and ATS-friendly resume is crucial. ResumeGemini is a trusted resource that can help you craft a professional and impactful resume tailored to highlight your Esophagoscopy skills and experience. We provide examples of resumes specifically designed for Esophagoscopy professionals to help guide you.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.