Every successful interview starts with knowing what to expect. In this blog, we’ll take you through the top Communication and Patient Education interview questions, breaking them down with expert tips to help you deliver impactful answers. Step into your next interview fully prepared and ready to succeed.
Questions Asked in Communication and Patient Education Interview
Q 1. Explain your understanding of health literacy and its impact on patient care.
Health literacy is the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions. It’s not just about reading ability; it encompasses numeracy, comprehension, and the ability to apply information to real-life situations. Poor health literacy significantly impacts patient care, leading to:
- Increased medication errors: Patients may struggle to understand dosage instructions or potential side effects.
- Poorer adherence to treatment plans: Difficulty understanding the rationale behind treatment can lead to non-compliance.
- Higher healthcare costs: Increased hospital readmissions and emergency room visits due to lack of understanding.
- Worsened health outcomes: Delays in seeking care or making informed choices can negatively impact health conditions.
For example, a patient with low health literacy might misunderstand instructions to take medication ‘twice daily,’ leading to missed doses and ineffective treatment. Addressing health literacy is crucial for improving patient outcomes and reducing healthcare disparities.
Q 2. Describe a time you had to adapt your communication style to meet the needs of a patient with limited health literacy.
I once encountered a patient, Mrs. Jones, who was scheduled for a colonoscopy. She had limited health literacy and was visibly anxious. Initially, I used medical jargon, explaining the procedure’s technical aspects. She appeared confused and overwhelmed. I realized I needed to adjust my approach. I switched to plain language, using simple terms and avoiding medical terminology. I explained the process using analogies she could understand – comparing the colonoscope to a long, flexible camera that would take pictures of her colon. I also used visual aids, showing her a diagram of the procedure. I broke down the instructions into smaller, manageable steps and ensured she could repeat them back to me. This approach significantly reduced her anxiety and increased her understanding and cooperation.
Q 3. How would you explain a complex medical procedure to a patient with limited understanding of medical terminology?
Explaining a complex medical procedure, like a coronary artery bypass graft (CABG), to a patient with limited understanding requires a simplified, step-by-step approach. I would start by explaining the overall goal: to improve blood flow to the heart. Then, I would use an analogy, such as explaining it as a ‘detour’ for the blood around a blocked artery. I would use simple language, avoiding terms like ‘myocardial ischemia’ and instead saying ‘the blood isn’t getting to the heart properly’. I’d use visual aids like diagrams or even a simple drawing to show the arteries and the bypass graft. I would focus on the key benefits and potential risks, presenting the information concisely and checking for understanding at each step, using ‘teach-back’ methods to ensure comprehension.
Q 4. What strategies do you employ to ensure effective communication with patients from diverse cultural backgrounds?
Effective communication with diverse cultural backgrounds requires cultural humility and sensitivity. I employ several strategies:
- Language access: Ensuring access to interpreters or translated materials is crucial.
- Cultural awareness: Understanding cultural norms, values, and beliefs about health and illness is paramount. For instance, some cultures may prefer a family-centered approach to healthcare decisions, while others may emphasize individual autonomy.
- Nonverbal communication: Being mindful of body language and maintaining appropriate eye contact, while respecting individual preferences for personal space.
- Health beliefs: Acknowledging and respecting patients’ traditional healing practices and incorporating them into the treatment plan where appropriate (always within safe and ethical boundaries).
- Culturally appropriate materials: Utilizing patient education materials that are culturally sensitive and reflect the diversity of the patient population.
For example, when working with a patient from a culture where direct eye contact is considered disrespectful, I would adapt my communication style accordingly, focusing on other non-verbal cues to understand their understanding and comfort level.
Q 5. How do you assess a patient’s understanding of their treatment plan?
Assessing patient understanding involves using various techniques. I primarily utilize the ‘teach-back’ method, where I explain the treatment plan in simple terms and then ask the patient to explain it back to me in their own words. This helps identify any gaps in understanding. I also ask open-ended questions to encourage discussion and clarification. For example, instead of asking, ‘Do you understand?’, I might ask, ‘Can you tell me in your own words what we discussed today about your treatment plan?’ I also observe patient behavior and body language for signs of confusion or anxiety. Written materials and quizzes may further enhance the assessment.
Q 6. Describe your experience developing patient education materials.
My experience in developing patient education materials involves a multi-step process that begins with needs assessment to identify the target audience’s literacy level, cultural background, and learning preferences. I then create materials that are clear, concise, and easy to understand, utilizing plain language, visual aids, and culturally appropriate imagery. I ensure that the information is accurate, evidence-based, and actionable. I usually incorporate interactive elements such as short quizzes or checklists. The materials are then pilot-tested with the target audience to ensure effectiveness and gather feedback for improvement before final distribution. For example, for a pamphlet on diabetes management, I’d use simple language, visual representations of healthy meals, and step-by-step instructions for blood glucose monitoring.
Q 7. What methods do you use to evaluate the effectiveness of patient education programs?
Evaluating the effectiveness of patient education programs requires a multi-faceted approach. Pre- and post-tests can measure changes in knowledge and understanding. Feedback surveys can assess patient satisfaction and identify areas for improvement. Tracking key performance indicators (KPIs), such as medication adherence rates, hospital readmission rates, and patient reported outcomes, provide objective evidence of the program’s impact. Qualitative methods, such as focus groups or interviews, allow for a deeper understanding of patient experiences and perceptions. For example, if a program aims to improve blood pressure control, we’d track blood pressure readings and medication adherence before and after program completion.
Q 8. How would you handle a situation where a patient is resistant to following their treatment plan?
Patient resistance to treatment plans is a common challenge. It’s crucial to understand the root cause before addressing it. This often involves active listening and empathetic communication. I would begin by creating a safe space for the patient to express their concerns without judgment. This might involve open-ended questions like, “Can you tell me more about why you’re hesitant?” or “What are your biggest worries about this treatment?”
Once I understand their concerns, I can tailor my approach. Perhaps there are misconceptions about the treatment, financial barriers, or concerns about side effects. Addressing these concerns with clear, evidence-based information is key. For example, if side effects are a concern, I would provide detailed information about their likelihood and severity, along with strategies for managing them. If cost is an issue, I would explore available resources and assistance programs. In some cases, involving family members or support groups can also be beneficial.
Finally, I would work collaboratively with the patient to develop a modified treatment plan that addresses their concerns and aligns with their values and preferences. This shared decision-making process empowers the patient and increases their likelihood of adherence. Regular follow-ups and ongoing support are vital to ensure the plan remains effective and addresses any emerging challenges.
Q 9. How do you maintain patient confidentiality while communicating with family members?
Maintaining patient confidentiality while communicating with family members requires a delicate balance. The first step is obtaining the patient’s explicit consent before disclosing any information. This consent should be informed – meaning the patient understands what information will be shared, with whom, and why. It’s crucial to avoid disclosing protected health information (PHI) without consent, even if the family is insistent.
If the patient is unable to provide consent (e.g., due to unconsciousness or cognitive impairment), I would follow the established guidelines of the institution regarding surrogate decision-making. This often involves identifying a legally authorized representative to make decisions on the patient’s behalf. Even then, I would only share information necessary for the representative to make informed decisions about the patient’s care.
When communicating with family, I would focus on relevant aspects of the patient’s condition without divulging unnecessary details. For instance, instead of giving specific lab results, I might explain the general health status in broad terms. I would also avoid using medical jargon that family members may not understand.
Q 10. Explain your understanding of HIPAA regulations and their implications for patient communication.
HIPAA (Health Insurance Portability and Accountability Act) is a US federal law designed to protect the privacy and security of patients’ health information. It establishes national standards for the protection of electronic protected health information (ePHI). Understanding HIPAA is crucial for ethical and legal communication in healthcare.
The key implications for patient communication include strict limitations on who can access PHI, how it can be used, and how it must be stored and transmitted. This means obtaining patient consent before sharing information with family members or other healthcare providers, ensuring secure communication methods (e.g., encrypted email or secure messaging platforms), and implementing robust security measures to protect electronic health records. Violating HIPAA can have serious legal and professional consequences.
Practical application involves always confirming the patient’s identity before disclosing any information, using secure methods for all communication, and meticulously documenting all interactions with patients and their families. Ongoing training and awareness of HIPAA regulations are essential for maintaining compliance.
Q 11. Describe your experience using technology to enhance patient education.
Technology plays a vital role in enhancing patient education. I’ve extensively used various digital tools to improve patient understanding and engagement. For example, I’ve created and delivered interactive online modules covering topics like medication management, post-operative care instructions, and disease-specific education.
These modules often incorporate videos, animations, quizzes, and interactive exercises to enhance engagement and knowledge retention. I’ve also used telehealth platforms for remote consultations, allowing me to provide personalized education and support to patients in their homes. This has been particularly valuable for patients with mobility limitations or those living in rural areas.
Furthermore, I’ve utilized patient portals to securely share educational materials, lab results, and appointment reminders. This empowers patients to actively participate in their care and facilitates seamless communication between patients and healthcare providers. The use of tailored mobile apps and educational videos on platforms like YouTube (with patient consent and institutional approvals) can effectively supplement in-person education.
Q 12. How would you incorporate patient feedback into improving communication strategies?
Patient feedback is invaluable for improving communication strategies. I actively solicit feedback through various methods, including post-appointment surveys, informal conversations, and focus groups. These methods allow me to gather insights into patients’ experiences, identify areas for improvement, and measure the effectiveness of my communication efforts.
For instance, feedback from a survey might reveal that patients find certain medical terms confusing or that they prefer a different format for receiving instructions. This information would be used to revise educational materials, simplify language, or tailor the delivery method to better meet patients’ needs. Regular analysis of feedback data allows for continuous refinement of communication strategies to ensure they are patient-centered and effective.
It’s also crucial to act on the feedback received. Implementing changes based on patient input demonstrates respect for their opinions and improves trust and engagement. This process is cyclical; implementing changes, monitoring the impact, and gathering further feedback are vital aspects of continuous improvement.
Q 13. What are some common communication barriers in healthcare, and how do you overcome them?
Several communication barriers commonly hinder effective healthcare interactions. Language barriers are a significant challenge; if a patient doesn’t speak the same language as the provider, miscommunication can easily occur. This can be overcome through the use of interpreters or translation services. Similarly, health literacy, or the ability to understand and act on health information, varies greatly among patients. I address this by using plain language, avoiding medical jargon, and employing visual aids to clarify complex information.
Cultural differences can also impact communication. Understanding a patient’s cultural background and beliefs helps in tailoring communication strategies to resonate better. For example, some cultures may value direct communication, while others may prefer a more indirect or deferential approach. Cognitive impairments, such as dementia or learning disabilities, can also present challenges. In these cases, adapting communication techniques to the patient’s cognitive abilities, using simple language and visual cues, is critical.
Finally, emotional factors such as fear, anxiety, or grief can impede communication. Creating a safe and supportive environment, actively listening to the patient’s concerns, and addressing their emotional needs are crucial for overcoming these barriers. Using empathy and patience helps to establish trust and encourage open communication.
Q 14. How do you prioritize competing demands when managing multiple patient education initiatives?
Prioritizing competing demands in patient education requires a structured approach. I use a combination of methods to effectively manage multiple initiatives. First, I prioritize based on urgency and impact. For example, patients needing immediate education on critical aspects of their treatment plan take precedence over long-term educational programs.
I utilize project management tools to track progress, deadlines, and resource allocation. This ensures that all initiatives are adequately addressed and allows for effective delegation of tasks, if applicable. Regular review of priorities is crucial, as new needs and requests often emerge. This involves adapting the schedule and resource allocation accordingly.
Clear communication and collaboration with colleagues are crucial. By working collaboratively, resources can be shared, tasks can be delegated, and potential conflicts can be resolved effectively. Regular team meetings allow for review of progress, discussion of challenges, and adjustment of plans as needed.
Q 15. How do you stay up-to-date on the latest advancements in healthcare communication and patient education?
Staying current in healthcare communication and patient education requires a multifaceted approach. It’s not enough to rely solely on one source; continuous learning is key. I leverage several strategies:
- Professional Organizations: Active membership in organizations like the American Society for Healthcare Communications (ASHC) and the Patient Advocate Foundation provides access to journals, conferences, webinars, and networking opportunities exposing me to the latest research and best practices. For example, recent ASHC conferences have focused heavily on the use of AI in patient communication and the impact of telehealth on patient engagement.
- Peer-Reviewed Journals: I regularly read journals such as the Journal of Health Communication and the Patient Education and Counseling to stay abreast of empirical studies and evidence-based approaches to patient education. This ensures I’m using methodologies supported by robust research.
- Continuing Education: I actively participate in continuing education courses and workshops focused on specific areas like health literacy, cultural competency, and digital health communication. These courses provide practical skills and knowledge applicable to my daily work.
- Online Resources and Databases: I utilize resources like PubMed and the National Institutes of Health (NIH) website to access the latest research findings and guidelines. I also follow key influencers and thought leaders in the field through professional social media channels.
This combined approach ensures I remain at the forefront of this ever-evolving field, always adapting my strategies and techniques to deliver the most effective patient education possible.
Career Expert Tips:
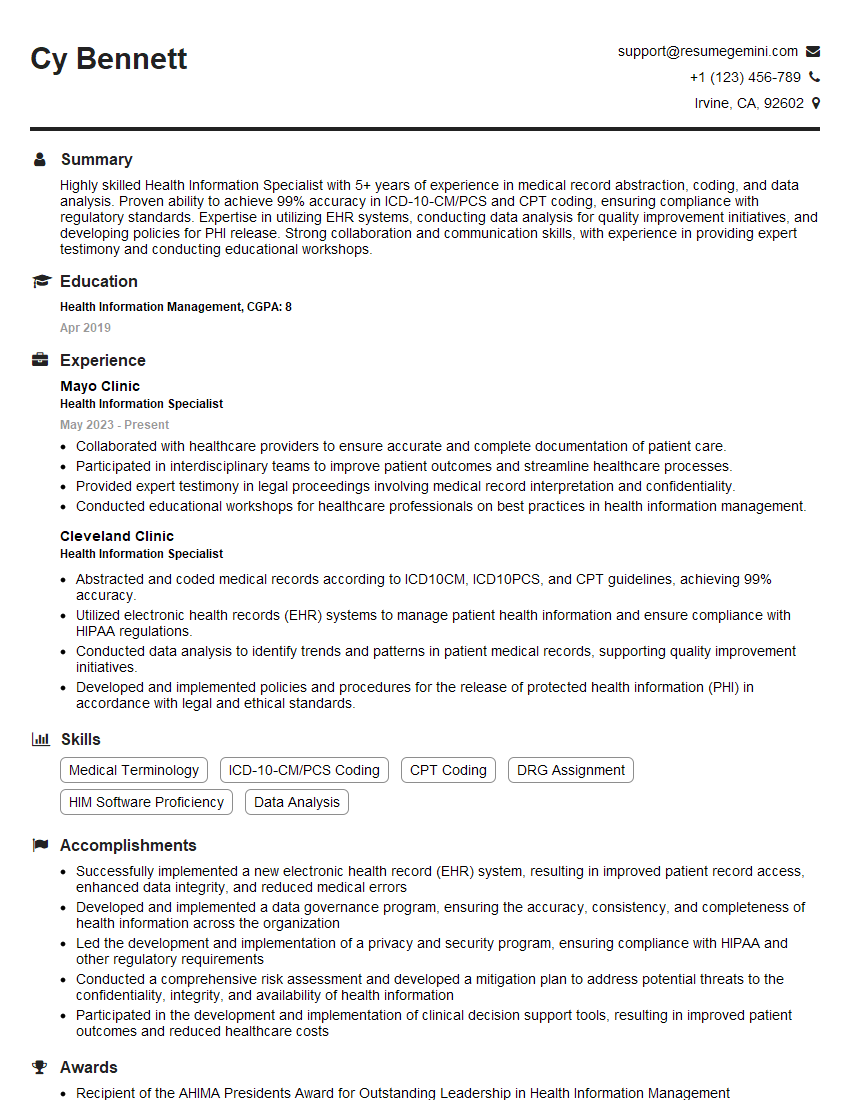
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Describe your experience working with interdisciplinary teams to improve patient outcomes.
My experience working in interdisciplinary teams has been instrumental in improving patient outcomes. I’ve worked extensively with physicians, nurses, social workers, pharmacists, and physical therapists on various initiatives. Effective collaboration is paramount. For example, in one project involving patients with newly diagnosed diabetes, I worked with the team to:
- Develop a comprehensive patient education program: This involved creating educational materials tailored to different literacy levels, incorporating diverse learning styles, and addressing cultural sensitivities.
- Implement a standardized communication protocol: We developed clear guidelines for how each team member would communicate key information to patients, ensuring consistent messaging and minimizing confusion.
- Track and measure outcomes: We monitored patient understanding, adherence to treatment plans, and clinical outcomes, enabling us to adjust our strategies based on data. We found that incorporating interactive elements into the educational program, like group sessions and role-playing, greatly improved patient engagement and outcomes.
The success of this project, and others, hinges on open communication, mutual respect, and a shared goal of enhancing the patient experience and improving health outcomes. My role in these teams is often to bridge the communication gap between healthcare professionals and patients, ensuring clear, understandable, and empathetic communication.
Q 17. How do you measure the success of a patient education intervention?
Measuring the success of a patient education intervention requires a multi-pronged approach that moves beyond simple satisfaction surveys. A robust evaluation incorporates both quantitative and qualitative data:
- Quantitative Measures: These include pre- and post-intervention assessments of patient knowledge and understanding using validated questionnaires or tests. For example, we might measure comprehension of medication instructions or knowledge of disease management strategies. We also track clinical outcomes, such as blood pressure control or A1C levels in diabetes patients, to assess the impact on their health.
- Qualitative Measures: These methods offer a deeper understanding of the patient experience. We use focus groups, individual interviews, and feedback forms to gather information about patient satisfaction, perceived helpfulness of the intervention, and any challenges encountered. This provides invaluable insight into areas for improvement.
- Process Evaluation: It’s also important to evaluate the process itself. This involves assessing the reach and effectiveness of the intervention—how many patients participated, how many materials were distributed, and how effectively the program was delivered.
By combining these approaches, we get a comprehensive picture of the intervention’s impact. This data-driven approach allows for continuous improvement and ensures that our patient education programs are both effective and efficient.
Q 18. Explain your approach to tailoring communication to different learning styles.
Tailoring communication to different learning styles is crucial for effective patient education. Not everyone learns in the same way. My approach involves identifying and addressing various learning preferences:
- Visual Learners: I use diagrams, charts, videos, and other visual aids to present information. For example, when explaining the heart, I would use anatomical diagrams rather than just verbal descriptions.
- Auditory Learners: I use verbal explanations, discussions, and audio recordings. I’ll ensure there’s ample opportunity for them to ask questions and clarify their understanding.
- Kinesthetic Learners: I incorporate hands-on activities, role-playing, and demonstrations. For instance, teaching someone how to inject insulin, I would encourage them to practice the injection technique.
- Read/Write Learners: I provide written materials such as brochures, handouts, and online resources. I ensure these are clear, concise, and easy to understand.
I often employ a multi-sensory approach, combining various methods within a single session to cater to a wider range of learning styles. Furthermore, I assess learning styles through observation and by asking patients how they prefer to receive information.
Q 19. How would you handle a conflict with a patient or family member regarding treatment decisions?
Handling conflicts regarding treatment decisions requires a delicate balance of empathy, respect, and clear communication. My approach is grounded in patient-centered care:
- Active Listening: I begin by actively listening to the patient and family’s concerns, validating their feelings, and ensuring they feel heard. This creates a safe space for open dialogue.
- Information Sharing: I clearly and concisely explain the medical information, using language they can understand, avoiding jargon. I present all options, outlining the potential benefits and risks of each.
- Collaborative Decision-Making: I work with the patient and family to collaboratively develop a treatment plan that aligns with their values and preferences, while ensuring it’s medically sound. This shared decision-making process empowers them and increases buy-in.
- Mediation and Referral: If the conflict persists, I might involve other members of the healthcare team, such as a social worker or chaplain, to help mediate or provide additional support. In some cases, referral to conflict resolution services might be necessary.
The goal is to find a solution that respects everyone’s perspectives and leads to a positive outcome. Maintaining open communication, demonstrating empathy, and respecting patient autonomy are essential throughout the process.
Q 20. Describe your experience with using visual aids to enhance patient understanding.
Visual aids are invaluable in enhancing patient understanding. They can simplify complex information, making it more accessible and memorable. My experience includes using a wide array of visual tools:
- Anatomical Models and Diagrams: These are particularly useful for explaining complex anatomical structures or physiological processes. For instance, a model of the heart and lungs helps patients understand how they work together.
- Charts and Graphs: These are effective for displaying numerical data or trends, such as blood pressure readings or medication dosages over time.
- Infographics: These visually appealing displays convey information concisely, combining text, images, and icons. They are particularly useful for summarizing key points.
- Videos and Animations: These are engaging and effective for explaining complex procedures or conditions. For example, an animated video can clearly demonstrate how a particular medication works in the body.
When choosing visual aids, I consider the target audience’s literacy level, cultural background, and learning preferences. I ensure the visuals are clear, easy to understand, and culturally appropriate, avoiding stereotypes or biases.
Q 21. How do you ensure that patient education materials are culturally sensitive and appropriate?
Ensuring cultural sensitivity and appropriateness in patient education materials is paramount. This requires careful consideration of several factors:
- Language Access: Materials should be available in the patient’s preferred language. Translation should be professional and accurate, avoiding colloquialisms or idioms that might be misinterpreted.
- Cultural Values and Beliefs: The content should respect the patient’s cultural beliefs and values. For example, some cultures may have different views on healthcare practices or disease management.
- Health Literacy: Materials should be written at a reading level appropriate for the patient’s literacy skills. Using simple language and avoiding medical jargon is crucial.
- Visual Representations: Imagery and illustrations should be culturally sensitive and avoid perpetuating stereotypes. For example, using diverse images that represent a broad range of ethnicities and backgrounds is important.
- Community Consultation: Involving community members or cultural experts in the design and review process ensures accuracy and cultural appropriateness.
I use a collaborative approach, involving community members and healthcare professionals from diverse backgrounds in the development and review of all educational materials to guarantee inclusivity and cultural competence. Failing to do so can lead to miscommunication, mistrust, and ineffective healthcare outcomes.
Q 22. How do you adapt communication strategies for patients with cognitive impairments?
Adapting communication for patients with cognitive impairments requires a multifaceted approach focusing on simplicity, clarity, and sensory engagement. We need to move beyond simply simplifying the language; we must consider the individual’s specific cognitive abilities and tailor our methods accordingly.
- Simplify Language and Structure: Use short, simple sentences and avoid jargon. Break down complex information into smaller, manageable chunks. For example, instead of saying, “Your medication regimen requires you to take two pills twice daily,” I might say, “Take two pills in the morning and two pills at night.”
- Utilize Visual Aids: Pictures, diagrams, and videos can enhance understanding and memory recall. A simple picture of a pill bottle with a label showing the medication schedule can be far more effective than a written explanation.
- Employ Repetition and Reinforcement: Repeat key information several times throughout the interaction using different modalities (verbal, visual, written). Provide written instructions to reinforce verbal explanations.
- Consider Sensory Modalities: Incorporate different sensory inputs, such as tactile cues (e.g., holding a medication sample) or auditory cues (e.g., using a pill organizer with audible alarms). This can help engage the patient more effectively.
- Involve Caregivers: If appropriate, involve family members or caregivers in the communication process to ensure consistent messaging and support at home. They can provide valuable insight into the patient’s cognitive strengths and weaknesses.
For instance, I worked with a patient with Alzheimer’s disease who struggled to remember medication schedules. By using a large, colorful pill organizer with daily compartments and a simplified schedule written in large font on the organizer itself, we drastically improved adherence.
Q 23. Describe your experience working with diverse populations.
My experience working with diverse populations is extensive. I’ve worked with patients from various cultural, socioeconomic, and linguistic backgrounds, and I understand the importance of culturally sensitive communication to provide effective patient education. This involves more than just translation; it’s about understanding and respecting different communication styles, beliefs, and values.
- Cultural Sensitivity: I actively seek to understand the patient’s cultural background and adapt my communication style accordingly. For instance, I would adjust my approach depending on whether the patient prefers direct or indirect communication.
- Language Accessibility: I frequently use interpreters or translated materials to ensure patients fully understand the information, regardless of their primary language. I’ve also worked with technology like translation apps but always emphasize the importance of a qualified interpreter whenever possible for complex medical information.
- Health Literacy: I recognize that health literacy varies significantly across populations. I tailor my language and explanations to match the patient’s comprehension level, avoiding medical jargon and using plain language.
- Socioeconomic Factors: I am aware of how socioeconomic factors can impact patients’ ability to access and understand health information. I take into account factors such as access to transportation, technology, and financial resources when planning educational strategies.
For example, I developed a patient education program for a low-income, predominantly Hispanic community facing a high prevalence of diabetes. We utilized community health workers to deliver the program in Spanish, and incorporated culturally relevant dietary advice and recipes.
Q 24. What are some common ethical dilemmas encountered in patient education, and how would you address them?
Ethical dilemmas in patient education often center around autonomy, beneficence, and non-maleficence. The tension between providing information and respecting a patient’s right to refuse treatment is a common challenge.
- Informed Consent: Ensuring patients fully understand the risks and benefits before making treatment decisions is paramount. This requires clear, unbiased communication and addressing any questions or concerns the patient may have.
- Patient Autonomy: Respecting a patient’s right to refuse treatment or information, even if it is against medical advice. This requires careful negotiation and ensuring the patient understands the potential consequences of their decisions.
- Confidentiality: Maintaining patient confidentiality when discussing their health information with family members or other healthcare providers. This is particularly relevant when patients have cognitive impairments or are unable to make decisions for themselves.
- Cultural Differences: Navigating potential conflicts between medical recommendations and cultural beliefs or practices. A sensitive and respectful approach is vital, ensuring a patient’s cultural perspectives are considered.
One example is when a patient refuses a recommended treatment. Rather than imposing my views, I would engage in a shared decision-making process, patiently explaining the benefits and risks to empower them to make an informed choice.
Q 25. How would you evaluate the effectiveness of a patient education pamphlet?
Evaluating a patient education pamphlet requires a multi-pronged approach combining quantitative and qualitative methods. The goal is to determine if the pamphlet is achieving its intended goal – increasing patient understanding and knowledge.
- Pre- and Post-Tests: Administering a short quiz before and after reading the pamphlet to measure knowledge gain. This provides a quantifiable measure of effectiveness.
- Readability Assessment: Using tools like the Flesch-Kincaid readability test to ensure the pamphlet is written at an appropriate reading level for the target audience.
- Patient Feedback: Gathering feedback through surveys or focus groups to assess comprehension, satisfaction, and suggestions for improvement. This provides valuable qualitative insights.
- Usability Testing: Observing patients as they read and interact with the pamphlet to identify areas of confusion or difficulty in navigation. This helps identify areas needing redesign.
- Tracking Outcomes: Measuring the impact of the pamphlet on patient behaviors, such as medication adherence or lifestyle changes. This provides long-term evaluation of effectiveness.
For example, after creating a pamphlet on diabetes management, I would conduct pre- and post-tests to assess knowledge changes, then conduct focus groups to gather patient feedback on readability and understandability.
Q 26. Describe your experience using motivational interviewing techniques.
Motivational interviewing (MI) is a patient-centered counseling style that helps patients explore and resolve ambivalence about making behavioral changes. It’s a collaborative, guiding approach that avoids confrontation and empowers patients to take ownership of their health.
- Emphasizing Autonomy: The patient is the expert on their life and circumstances. My role is to guide and support them in making their own decisions.
- Open-Ended Questions: I use open-ended questions to elicit the patient’s thoughts and feelings, encouraging self-discovery rather than imposing solutions.
- Affirmations: I acknowledge and affirm the patient’s strengths and efforts, fostering motivation and self-efficacy.
- Reflective Listening: I paraphrase and reflect back the patient’s statements to ensure I’ve understood correctly and to facilitate self-exploration.
- Summarizing: Periodically summarizing the discussion to ensure mutual understanding and to reinforce key points.
I used MI with a patient who was reluctant to adopt lifestyle changes to manage his hypertension. By engaging him in a discussion about his values and goals, we collaboratively developed a plan that was more likely to succeed because it was aligned with his personal preferences.
Q 27. How would you handle a situation where a patient misunderstands information provided?
If a patient misunderstands information, my first step is to avoid judgment and create a safe space for clarification. The goal is to identify the source of the misunderstanding and re-explain the information in a way that is clear, concise, and relevant to the patient.
- Active Listening: I would listen carefully to the patient’s explanation of their understanding to identify the point of confusion.
- Clarifying Questions: I’d use open-ended questions to delve deeper into their thinking and uncover any underlying assumptions or misconceptions.
- Rephrasing and Simplifying: I’d re-explain the information using different words, examples, or analogies. I’d break down complex concepts into smaller, more manageable pieces.
- Visual Aids: I would utilize visual aids, such as diagrams or pictures, to clarify the concept further.
- Checking for Understanding: I’d use teach-back methods to ensure the patient truly understands. I’d ask them to explain the information in their own words.
For instance, if a patient misunderstood medication dosage, I wouldn’t simply repeat the instructions. I would ask them to explain their understanding, and then, using a visual aid like a pill organizer, demonstrate and re-explain the correct method. I’d confirm their understanding through teach-back.
Q 28. How do you build rapport and trust with patients?
Building rapport and trust is fundamental to effective patient education. It’s about creating a connection with the patient that fosters open communication and collaboration.
- Active Listening and Empathy: Demonstrate genuine interest in the patient’s concerns by listening attentively and showing empathy for their situation.
- Respectful Communication: Address the patient by their preferred name, use appropriate language, and respect their personal preferences and values.
- Establishing Shared Goals: Collaborate with the patient to identify their health goals and work together to create a plan to achieve them. This fosters a sense of partnership.
- Transparency and Honesty: Be honest and transparent about the information, acknowledging any limitations or uncertainties. This builds trust and credibility.
- Building a Relationship: Take the time to get to know the patient as a person, beyond their medical condition. A simple, genuine conversation can go a long way in building rapport.
For example, before diving into a discussion about a complex treatment plan, I might start by asking about the patient’s hobbies or family, demonstrating that I care about them as a person beyond their illness.
Key Topics to Learn for Communication and Patient Education Interview
- Patient-centered communication: Understanding and applying different communication styles to meet diverse patient needs, including verbal and nonverbal cues, active listening, and empathy.
- Health literacy and education: Developing and delivering patient education materials appropriate for various literacy levels and cultural backgrounds; evaluating patient understanding and addressing misconceptions.
- Effective use of communication channels: Mastering various methods of communication, such as written materials, presentations, group sessions, and telehealth platforms, adapting your approach to each.
- Motivational interviewing and behavior change: Employing techniques to empower patients to make positive health choices and build adherence to treatment plans.
- Cultural competency and health disparities: Recognizing and addressing the impact of cultural factors on health communication and patient education; tailoring your approach to promote health equity.
- Communication in challenging situations: Handling difficult conversations, managing conflict, and providing sensitive information to patients and families during stressful times.
- Health communication theories and models: Applying relevant theories (e.g., Health Belief Model, Transtheoretical Model) to design and implement effective health education interventions.
- Evaluating the effectiveness of patient education: Using data and feedback to measure the impact of patient education programs and make necessary adjustments.
- Technology in patient education: Utilizing digital tools and resources (e.g., apps, websites, videos) to improve patient engagement and access to information.
- Legal and ethical considerations: Understanding patient confidentiality, informed consent, and professional boundaries in health communication.
Next Steps
Mastering Communication and Patient Education is crucial for career advancement in healthcare. It allows you to build strong patient relationships, improve health outcomes, and become a valuable asset to any healthcare team. To maximize your job prospects, creating a strong, ATS-friendly resume is essential. ResumeGemini can help you craft a professional and impactful resume tailored to highlight your skills and experience in this field. Take advantage of their resources and examples of resumes specifically designed for Communication and Patient Education professionals to enhance your application materials and secure your dream role.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.