Unlock your full potential by mastering the most common Surgical First Assist interview questions. This blog offers a deep dive into the critical topics, ensuring you’re not only prepared to answer but to excel. With these insights, you’ll approach your interview with clarity and confidence.
Questions Asked in Surgical First Assist Interview
Q 1. Describe your experience assisting in laparoscopic procedures.
My experience assisting in laparoscopic procedures spans several years and encompasses a wide range of surgeries, including cholecystectomies, appendectomies, and colorectal procedures. I’m proficient in operating the laparoscopic instruments, including the camera, graspers, dissectors, and energy devices. I’m adept at maintaining pneumoperitoneum, retracting tissues, and providing precise tissue handling to the surgeon. For example, during a laparoscopic cholecystectomy, my role involves meticulously dissecting the cystic artery and duct, ensuring safe and efficient removal of the gallbladder while minimizing bleeding and injury to surrounding structures. I’m also experienced in managing complications like bleeding or inadvertent injury, quickly notifying the surgeon and assisting in their resolution.
Beyond technical skills, I emphasize meticulous attention to detail in instrument maintenance, fluid management, and ensuring a clear surgical field throughout the procedure. This consistent precision contributes to faster operating times, reduced patient complications, and improved overall surgical outcomes.
Q 2. Explain the difference between a surgical first assistant and a surgical technician.
While both surgical first assistants (SFAs) and surgical technicians work in the operating room and support the surgical team, their roles and responsibilities differ significantly. A surgical technician primarily focuses on maintaining the sterile field, preparing instruments, and assisting with equipment. They perform tasks under the direction of the surgeon or SFA and do not participate in the actual surgical procedure. Think of them as the crucial support system ensuring everything runs smoothly outside of the main surgical maneuvers.
In contrast, an SFA is a highly skilled professional who participates directly in the surgical procedure under the surgeon’s supervision. SFAs have advanced knowledge of surgical anatomy, procedures, and instrumentation. Their responsibilities extend beyond instrument handling to include tasks like tissue retraction, hemostasis (controlling bleeding), and suturing, all actions directly impacting the surgical outcome. They essentially act as an extension of the surgeon’s hands, providing critical support throughout the entire procedure. Essentially, the surgical technician sets the stage, while the SFA is a key actor in the surgery itself.
Q 3. How do you maintain a sterile field during a surgical procedure?
Maintaining a sterile field is paramount to preventing surgical site infections. This involves a multi-step process beginning before the procedure even starts, including proper hand hygiene, gowning and gloving, and appropriate environmental preparation of the operating room. During the procedure, meticulous attention is paid to avoiding contact between sterile and non-sterile items. This includes careful draping of the patient to create a sterile barrier, regular monitoring of the field for any breaches in sterility (e.g., a dropped instrument or a stray touch from a non-sterile item), and immediate rectification of any potential contamination. For example, if a non-sterile item touches the sterile field, the area needs to be immediately re-prepped and re-draped. Regular monitoring and proactive measures are crucial in preventing serious surgical complications.
The use of sterile drapes, instruments, and solutions is non-negotiable. Any movement within the sterile field needs to be deliberate and precise to minimize the risk of contamination. A strong awareness of surroundings and commitment to sterile principles is fundamental.
Q 4. What are the key responsibilities of a surgical first assistant?
The key responsibilities of a surgical first assistant are multifaceted and crucial to the success of any surgical procedure. They involve both technical skills and critical thinking. These responsibilities include:
- Direct participation in the surgical procedure: This involves tissue retraction, hemostasis (stopping bleeding), suturing, and assisting with the surgeon’s instrument needs.
- Maintaining hemostasis: Controlling bleeding using various techniques like cautery or surgical clips is vital to minimizing blood loss.
- Tissue handling and retraction: Precise and gentle handling of tissues, minimizing trauma during dissection and retraction.
- Instrument management: Anticipating the surgeon’s needs and having the necessary instruments ready.
- Wound closure: Assisting in the meticulous closure of the surgical wound, using appropriate sutures and techniques.
- Monitoring patient status: Observing the patient for any signs of distress or complications.
- Maintaining the sterile field: Protecting the sterile field from contamination throughout the procedure.
These duties require a deep understanding of surgical anatomy, techniques, and instrument usage. A successful SFA anticipates the surgeon’s needs, proactively addressing potential complications, and facilitating a smooth, efficient, and safe surgical experience.
Q 5. Describe your experience with various surgical instruments and their usage.
My experience with surgical instruments is extensive and diverse, ranging from basic dissecting instruments like scalpels and scissors to specialized laparoscopic instruments and energy devices. I’m proficient in using various types of forceps, retractors, clamps, and suture materials. For example, I’m experienced with the nuances of using different types of graspers in laparoscopic surgery, understanding the precision required for delicate tissue handling. I also have experience working with various energy devices, such as monopolar and bipolar cautery, and laser devices, understanding their capabilities and limitations, and adhering strictly to safety protocols.
My knowledge extends to understanding the mechanics and maintenance of these instruments. I know how to inspect instruments for damage before use and properly clean and sterilize them afterwards. This attention to detail ensures the instruments are in optimal condition and ready for use, contributing to both efficiency and safety in the operating room.
Q 6. How do you anticipate and respond to intraoperative complications?
Anticipating and responding to intraoperative complications requires a combination of experience, knowledge, and quick thinking. This includes having a thorough understanding of the surgical procedure, potential complications, and having a prepared plan of action. For instance, if unexpected bleeding occurs, I would immediately inform the surgeon, assist in identifying the bleeding source, and help with hemostasis techniques. Similarly, if there’s an unforeseen anatomic variation, I would assist the surgeon in adapting the surgical plan while maintaining patient safety. Preparation is key; knowing the patient’s history and anticipating possible issues allows for quicker responses to any unexpected events.
My approach is characterized by a calm, methodical response to emergencies. I prioritize effective communication with the surgical team, efficient implementation of corrective measures, and a constant focus on maintaining patient safety and a positive surgical outcome. Every instance is treated as a learning opportunity to further hone my skills in recognizing and reacting to unforeseen surgical complications.
Q 7. What is your understanding of surgical wound classification?
Surgical wound classification systems are used to standardize the assessment of surgical wound contamination and infection risk. The most common system is the classification developed by the Centers for Disease Control and Prevention (CDC). This system categorizes wounds based on the degree of contamination at the time of surgery. This classification is crucial because it helps determine the appropriate postoperative care and antibiotic prophylaxis (preventive antibiotics).
The categories generally include:
- Clean wounds: These are wounds created under sterile conditions with minimal inflammation. Examples include elective surgeries with no entry into the respiratory, alimentary, or genitourinary tracts.
- Clean-contaminated wounds: These wounds involve entering the respiratory, alimentary, or genitourinary tracts, but without significant contamination or inflammation.
- Contaminated wounds: These wounds have significant contamination from a break in sterile technique or spillage of contaminated contents (such as bowel contents).
- Dirty or infected wounds: These wounds show signs of existing infection before surgery.
Understanding wound classification is essential for choosing the best prophylactic measures to prevent postoperative infections, optimizing surgical outcomes and reducing patient complications.
Q 8. Explain your knowledge of different types of surgical dressings and their application.
Surgical dressings are crucial for wound healing and infection prevention. Different dressings cater to various wound types and stages of healing. My knowledge encompasses a wide range, including:
- Gauze dressings: These are the most common, absorbent, and relatively inexpensive. They’re ideal for draining wounds but require frequent changes. For example, a heavily draining abdominal incision might necessitate frequent gauze changes to prevent saturation and maceration of the surrounding skin.
- Non-adherent dressings: These prevent the dressing from sticking to the wound bed, minimizing trauma during removal. Telfa pads are a prime example, perfect for superficial wounds or those needing minimal disturbance. I’ve often used these post-operatively for preventing adhesion to a delicate skin graft.
- Hydrocolloids: These are self-adhesive dressings that create a moist wound healing environment. They are suitable for partial-thickness wounds and are excellent at absorbing exudate. I’ve successfully utilized hydrocolloids on pressure ulcers, facilitating faster healing and reducing pain during dressing changes.
- Hydrogels: These are water-based dressings that hydrate the wound and debride necrotic tissue. They’re beneficial for dry, necrotic wounds or burns. In one case, a patient with a severe burn had significant improvement using a hydrogel dressing combined with other treatments.
- Alginates: Derived from seaweed, these highly absorbent dressings are excellent for heavily draining wounds. Their ability to absorb large amounts of exudate while maintaining a moist environment makes them ideal for infected wounds. I remember using alginates on a patient with a post-surgical infection; they helped control the drainage and facilitated quicker healing.
Application involves careful wound assessment to select the appropriate dressing, meticulous cleaning and preparation of the wound site, and secure application to promote optimal healing. Proper documentation of the dressing type and the patient’s response is essential.
Q 9. How do you handle emergencies in the operating room?
Handling emergencies in the OR demands quick thinking, clear communication, and a thorough understanding of crisis management. My approach follows a structured framework:
- Immediate Assessment: Rapidly assess the patient’s condition, identifying the nature and severity of the emergency (e.g., cardiac arrest, massive hemorrhage, anaphylactic shock).
- Call for Help: Activate the code system (e.g., ‘Code Blue’ for cardiac arrest) to immediately alert the appropriate response team, including anesthesia, critical care, and potentially additional surgical staff.
- Initiate Life Support: Begin basic or advanced life support (BLS/ACLS) measures as needed, depending on the emergency. This may involve CPR, airway management, or hemorrhage control.
- Collaborate with the Team: Work seamlessly with the surgical team, clearly communicating the situation and the actions being taken. Effective teamwork is critical.
- Post-Emergency Management: After the immediate crisis, participate in post-event debriefing to analyze the situation, identify areas for improvement, and prevent similar future events. Documentation of the entire event is crucial.
Experience has taught me the importance of remaining calm, prioritizing actions based on immediate patient need, and maintaining clear communication throughout the crisis. For instance, during a case where a patient experienced a sudden drop in blood pressure, my quick actions in assisting with fluid resuscitation and communicating the situation to the anesthesiologist helped stabilize the patient.
Q 10. What is your experience with tissue handling and hemostasis techniques?
Tissue handling and hemostasis are fundamental to surgical success. Gentle tissue manipulation is crucial to minimize trauma and promote healing. My experience involves a variety of techniques:
- Gentle Tissue Handling: Using appropriate instruments, such as delicate forceps and retractors, to avoid unnecessary trauma. I emphasize minimizing tissue tension and using proper surgical technique to reduce damage.
- Hemostasis Techniques: This includes a range of methods to control bleeding, such as direct pressure, electrocautery (mono/bipolar), surgical clips, ligatures (tying off blood vessels), and the use of topical hemostatic agents (e.g., thrombin, cellulose). The choice depends on the type and location of the bleeding. For instance, electrocautery is frequently used for smaller vessels, while larger bleeding vessels often require ligatures.
- Wound Closure: This includes suturing techniques (various types of sutures and patterns), stapling, and the use of surgical adhesives to facilitate proper wound healing and prevent complications.
Proper tissue handling prevents complications such as seromas, hematomas, and wound infections, which I have seen lead to prolonged recovery times and patient discomfort. For example, I have consistently used meticulous dissection techniques and precise hemostasis to improve patient outcomes and recovery times in a variety of surgical cases.
Q 11. How do you ensure effective communication with the surgical team?
Effective communication is the cornerstone of a safe and efficient surgical environment. I strive for clear, concise, and respectful communication using the following strategies:
- Active Listening: Paying close attention to the surgeon’s instructions, anticipating needs, and clarifying any uncertainties. Asking questions when needed shows proactive engagement.
- Clear Verbal Communication: Using precise language to convey information, such as reporting bleeding, tissue changes, or instrument needs promptly and accurately.
- Non-Verbal Communication: Maintaining appropriate body language, such as paying attention and anticipating needs through visual cues from the surgeon.
- Situational Awareness: Maintaining an awareness of the overall surgical process and anticipating the surgeon’s needs based on the stage of the procedure.
- Professional Demeanor: Always maintaining a professional and respectful attitude towards all team members, fostering a positive and collaborative surgical environment.
For instance, during a complex laparoscopic procedure, anticipating the surgeon’s need for a specific instrument before being asked demonstrated my proactive communication skills and contributed to the smooth progress of the surgery. Effective communication is essential for minimizing errors, promoting teamwork, and ensuring patient safety.
Q 12. Describe your understanding of surgical anatomy and physiology.
A solid understanding of surgical anatomy and physiology is paramount for a surgical first assistant. My knowledge encompasses:
- Regional Anatomy: Detailed knowledge of the anatomical structures relevant to the surgical procedures I assist with. This includes the location of major vessels, nerves, organs, and other anatomical landmarks.
- Physiological Processes: Understanding how the body’s systems function during surgery, such as blood flow, tissue repair, and the effects of anesthesia. This helps anticipate complications and enables effective responses.
- Surgical Pathology: Knowledge of common disease processes affecting specific anatomical regions. Understanding this aids in the identification of abnormal tissue and assists during the procedure.
- Anatomical Variations: Recognizing the variations that exist in anatomy between individuals, as this is vital in preventing iatrogenic injuries.
For example, during a cholecystectomy (gallbladder removal), a thorough understanding of the biliary anatomy—the cystic duct, hepatic ducts, and common bile duct— is critical to avoid accidental injury to these structures. My detailed anatomical knowledge helps me anticipate the surgeon’s needs and assist effectively and safely.
Q 13. How do you maintain patient safety during a surgical procedure?
Patient safety is my top priority. I employ various strategies throughout the surgical procedure to ensure this:
- Strict Sterile Technique: Adhering meticulously to sterile protocols, including proper gowning and gloving, instrument sterilization, and maintaining a sterile field to prevent infections.
- Monitoring Vital Signs: Assisting in monitoring the patient’s vital signs (heart rate, blood pressure, oxygen saturation) and reporting any abnormalities to the anesthesiologist and surgeon immediately.
- Preventing Surgical Site Infections (SSIs): Utilizing appropriate surgical techniques, including proper wound closure and wound dressing, to prevent SSIs. Preparing the patient’s skin according to hospital protocols is also vital.
- Safe Handling of Instruments and Equipment: Ensuring all equipment is functioning correctly and handling sharps safely to avoid patient injuries. Proper use of electrosurgical equipment is crucial to prevent burns.
- Preventing Medication Errors: Verifying medications before administration and reporting any discrepancies immediately.
For example, during a procedure where a patient was at high risk for bleeding, I meticulously monitored blood loss, closely communicated the patient’s hemodynamic status to the surgical team, and prepared for potential blood transfusions. Proactive measures like this protect the patient and contribute to successful surgical outcomes.
Q 14. Explain your experience with surgical counts and the importance of accuracy.
Surgical counts are a crucial safety check performed before, during, and after surgical procedures to ensure that all instruments, sponges, and needles are accounted for. Accuracy is paramount to prevent retained foreign bodies, a serious surgical complication.
- Pre-operative Count: This involves counting all instruments and sponges before the incision is made. This count is always performed by two people and meticulously documented.
- Intra-operative Count: Counts are performed at specific intervals during the procedure (e.g., closure of major structures, before wound closure) by the surgical technologist and the circulating nurse and verified by me. Any discrepancies require an immediate and thorough search.
- Post-operative Count: A final count is performed after wound closure to confirm that all items have been removed from the surgical site.
Inaccurate counts have potentially severe consequences, including the risk of retained surgical sponges or instruments that can lead to infections, internal damage, and even death. A patient’s post-operative pain, fever, and other signs could be a potential indication that a retained foreign object is still in the patient, leading to possible re-operation.
My experience emphasizes the meticulous attention to detail needed for accurate counts and the importance of immediately reporting any discrepancy to the entire team for resolution before proceeding. I can provide numerous case examples where thorough and timely counting prevented serious incidents.
Q 15. Describe your experience with various types of surgical suturing and knot tying.
Surgical suturing and knot tying are fundamental skills for a surgical first assistant. Proficiency involves understanding various suture materials (absorbable vs. non-absorbable, their tensile strength and tissue compatibility), needle types (cutting, taper, reverse cutting), and different suturing techniques (simple interrupted, continuous, running, locking, etc.).
My experience encompasses a wide range, from simple wound closures to intricate fascial repairs and vascular anastomoses. For instance, I’m highly skilled in using absorbable sutures like Vicryl for subcutaneous tissue, while preferring Prolene for skin closures due to its strength and cosmetic outcome. I’ve practiced and mastered various knot-tying techniques, including the square knot (the most common), surgeon’s knot, and instrument tie, each chosen based on the specific surgical situation and tissue being sutured. The goal is always to create strong, secure, and minimally reactive knots that minimize tissue trauma.
I regularly assess the tension and placement of each suture to ensure proper apposition of tissues and prevent complications like dead space or wound dehiscence (opening). The ability to adapt my suture technique based on the tissue characteristics and the surgical field is a crucial element of my skill set. For example, using a delicate needle and fine suture for delicate structures like the peritoneum, and a stronger suture for thicker tissues like fascia.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you manage and dispose of surgical waste and sharps?
Safe handling and disposal of surgical waste and sharps is paramount for maintaining a sterile surgical environment and preventing injuries to the surgical team. All sharps – needles, scalpels, etc. – are immediately placed into designated puncture-resistant containers. These containers are clearly labeled and sealed securely once they reach their capacity. No sharps are ever recapped manually.
Surgical waste is categorized according to its risk level (infectious vs. non-infectious). Infectious waste, including soiled dressings, surgical sponges, and potentially contaminated instruments, is placed in appropriately labeled red biohazard bags. These bags are then properly sealed and transported for incineration or other approved methods of sterilization. Non-infectious waste is managed separately, following all relevant guidelines and hospital protocols.
Throughout the surgical procedure, I meticulously follow the facility’s established protocols for waste disposal, ensuring compliance with all relevant safety regulations. Regular training and adherence to these protocols are crucial in minimizing the risk of exposure to infectious agents or accidental sharps injuries. I regularly review and remain current on best practices in waste management.
Q 17. What is your understanding of surgical asepsis?
Surgical asepsis refers to the techniques used to maintain a sterile field and prevent contamination of surgical wounds. This is crucial in minimizing the risk of surgical site infections (SSIs), which can have serious complications for the patient.
My understanding involves a comprehensive approach, starting with thorough hand hygiene using an approved antiseptic solution. The surgical field is carefully draped to create a sterile barrier, and all instruments, drapes, and gowns are rigorously sterilized prior to use. Strict adherence to sterile technique is practiced throughout the procedure, with careful attention to avoiding touching non-sterile surfaces and maintaining a sterile field around the surgical site. Any breach in sterile technique is immediately addressed.
Constant vigilance is maintained to prevent contamination. I will promptly alert the surgical team to any observed breach in sterile technique, such as a contaminated instrument or a compromised drape. My role involves continuous monitoring and maintaining the integrity of the sterile field, recognizing that any lapse can have significant consequences for the patient’s safety and outcome.
Q 18. How do you handle challenging surgical situations?
Handling challenging surgical situations requires a combination of quick thinking, technical expertise, and effective communication. I approach these situations systematically, prioritizing patient safety above all else. The first step is to accurately assess the situation and understand the nature of the challenge. This often involves clearly identifying the problem and its potential impact.
My approach then focuses on problem-solving and decision-making. I rely on my clinical experience, knowledge of surgical anatomy and physiology, and understanding of various surgical techniques to identify the best course of action. Communication with the surgical team is essential, keeping them informed of the situation and my proposed solutions. This collaborative approach is critical to efficiently address unexpected complications and ensure a successful outcome.
For example, in a situation involving unexpected bleeding, my immediate response would focus on quickly identifying the source and controlling the bleeding. I would utilize appropriate techniques, including surgical clamping, suturing, and the application of hemostatic agents, while simultaneously alerting the surgeon and other members of the surgical team. The focus always remains on maintaining patient stability and mitigating further risks.
Q 19. Describe your experience with robotic-assisted surgery (if applicable).
While I haven’t had extensive experience with robotic-assisted surgery, I am familiar with the principles and techniques involved. I have assisted in several procedures where the robotic surgical system was used. My role involved preparing the robotic instruments, managing the camera system, and assisting the surgeon in manipulating the robotic arms to carry out the surgical maneuvers.
Working in a robotic surgery environment requires specific skills, such as an understanding of the robotic console and its various controls, as well as the ability to anticipate the surgeon’s needs. I am adept at translating the surgeon’s actions and needs within the robotic setting. I found that precision and dexterity are even more critical with robotic assistance because of the magnified surgical field and the potential for very small movements to have significant consequences. This experience has broadened my understanding of minimally invasive surgical techniques and expanded my skillset.
I am eager to further develop my skills in this area, as robotic-assisted surgery is becoming increasingly prevalent and offers significant benefits to patients. I recognize the importance of continuous learning and am actively seeking opportunities to gain further experience in this rapidly evolving field.
Q 20. How do you stay updated on the latest advancements in surgical techniques?
Staying updated on advancements in surgical techniques is an ongoing commitment. I actively participate in professional development activities such as attending surgical conferences, workshops, and seminars. This provides me with exposure to new techniques, technologies, and best practices.
I also regularly review peer-reviewed surgical journals and professional publications, focusing on areas relevant to my surgical specialty. Staying current with research findings is invaluable for enhancing my skills and adopting innovative approaches in surgical procedures. I regularly attend departmental Grand Rounds, Journal Club meetings, and engage in active participation in our hospital’s Continuing Medical Education (CME) program.
Furthermore, I maintain memberships in professional organizations dedicated to surgical technology and advances. Through these affiliations, I have access to the latest research, guidelines, and networking opportunities with leading surgical professionals.
Q 21. What is your understanding of informed consent in surgical procedures?
Informed consent is a cornerstone of ethical surgical practice. It’s a process ensuring that a patient understands the risks, benefits, and alternatives of a proposed surgical procedure before giving permission to proceed.
My understanding involves ensuring that the patient is fully informed about all aspects of the procedure, including the potential complications and the likelihood of success. This requires clear and understandable communication, using language that the patient can easily comprehend. It’s crucial that the patient feels comfortable asking questions and expressing any concerns they may have before giving consent.
While I am not directly involved in obtaining informed consent, I understand the importance of this process and its impact on patient safety and trust. I would always be respectful of the patient’s autonomy and make sure that the surgical team has adequately explained the procedure and obtained valid consent before proceeding. Any doubts or concerns about a patient’s understanding of the procedure would be immediately brought to the attention of the surgeon and the appropriate medical staff.
Q 22. Describe your experience with different types of anesthesia.
My experience encompasses a wide range of anesthesia types, from general anesthesia, where the patient is completely unconscious, to regional anesthesia, which numbs a specific area of the body, allowing the patient to remain awake. I’m also proficient in working with monitored anesthesia care (MAC), a lighter form of sedation, and spinal/epidural anesthesia used for lower body procedures. Understanding the nuances of each type is crucial; for instance, the effects of general anesthesia on muscle relaxation are vital for surgical exposure, while with regional anesthesia, maintaining patient comfort and monitoring for potential complications like hypotension are paramount. I’ve worked extensively with anesthesiologists across various specialties, learning to anticipate their needs and react appropriately to intraoperative changes in the patient’s condition. For example, during a lengthy laparoscopic cholecystectomy under general anesthesia, I was alert to signs of decreased oxygen saturation and immediately assisted the anesthesiologist in adjusting ventilation settings.
Q 23. How do you prioritize tasks during a complex surgical case?
Prioritizing during complex surgical cases requires a systematic approach. I utilize a modified version of the ABCDE framework, adapting it from trauma care to the surgical setting. Airway is always primary, though less critical in many planned procedures; it’s about maintaining optimal breathing during critical moments. Bleeding control is next, especially in cases with high risk of significant hemorrhage. Cardiac status – monitoring vital signs and responding to changes – is always essential. Disinfection and sterility are paramount to prevent infection, while Exposure and appropriate tissue handling ensures optimal surgical visualization and prevents injury. This is a dynamic process; priorities shift based on the situation. For example, during a complex vascular reconstruction, while maintaining sterile technique, the immediate priority might shift rapidly from good surgical exposure to hemorrhage control should an unexpected vessel bleed occur.
Q 24. What are your strengths and weaknesses as a surgical first assistant?
My strengths lie in my meticulous attention to detail, strong surgical skills honed over years of experience, and my ability to anticipate the surgeon’s needs. I’m adept at quickly adapting to unexpected situations and maintaining a calm demeanor under pressure, vital in a high-stakes environment. For instance, during a complicated appendectomy, I seamlessly assisted in handling unexpected adhesions, contributing to a faster, safer procedure. However, I constantly work on improving my efficiency, particularly in situations involving intricate microsurgery, where precision and speed are equally important. Regular practice and seeking feedback from experienced surgeons helps address this.
Q 25. Explain your understanding of post-operative care related to surgical first assisting.
Post-operative care, from a surgical first assistant’s perspective, involves ensuring proper wound closure and hemostasis before the patient leaves the operating room. This includes meticulous attention to detail in securing sutures, preventing seroma formation and identifying any potential sources of bleeding. I contribute to the patient’s early recovery by accurately documenting the procedure, including the type and amount of fluid used, any complications encountered, and the details of wound closure. Accurate documentation is crucial for the postoperative care team, allowing them to anticipate any potential issues.
Q 26. Describe a time you had to make a quick critical decision during a surgery.
During a laparoscopic cholecystectomy, an unexpected massive bleed occurred due to an unforeseen cystic artery injury. The surgeon was focused on controlling the bleeding, but I quickly realized the need to suction blood effectively, maintaining visibility of the surgical field. Rapidly identifying the appropriate suction device and efficiently clearing the blood allowed the surgeon to quickly clamp and ligate the artery, preventing further complications. This situation highlighted the importance of proactive anticipation and decisive action under pressure.
Q 27. How do you contribute to a positive team dynamic in the operating room?
Contributing to a positive team dynamic hinges on clear communication, active listening, and mutual respect. I ensure all instructions are clearly understood and confirmed, and I proactively anticipate needs, reducing the pressure on the surgical team. For example, I ensure instruments are readily available, and anticipating the surgeon’s next steps, I can efficiently and smoothly hand them instruments as needed, maintaining an appropriate sterile field. A positive, calm demeanor fosters an efficient and safe surgical environment.
Q 28. Describe your experience working with different surgical specialties.
My experience spans various surgical specialties, including general surgery, vascular surgery, and minimally invasive surgery. Working across specialties has broadened my understanding of different surgical techniques and approaches. Adapting to the distinct needs and preferences of each specialty has refined my adaptability and efficiency. For example, the precision required in vascular surgery differs from the speed and efficiency needed in a laparoscopic cholecystectomy, demonstrating my versatility and comprehensive skills.
Key Topics to Learn for Surgical First Assist Interview
- Surgical Site Preparation and Drape Techniques: Understanding sterile field principles, proper draping techniques for various surgical procedures, and identification of potential contamination risks.
- Hemostasis and Wound Closure: Practical application of different hemostasis methods (e.g., electrocautery, ligation), proficiency in wound closure techniques (sutures, staples), and knowledge of appropriate suture materials.
- Instrument Handling and Passing: Mastering efficient instrument passing techniques, understanding instrument nomenclature, and maintaining sterility during the surgical procedure.
- Tissue Handling and Retraction: Gentle tissue handling to minimize trauma, effective retraction techniques, and understanding the anatomical structures involved in various surgical procedures.
- Understanding Surgical Procedures: Demonstrating a foundational understanding of common surgical procedures relevant to your specialization. This includes pre-operative, intra-operative, and post-operative considerations.
- Surgical Anatomy and Physiology: A solid grasp of relevant anatomical structures and physiological processes crucial for safe and effective first assisting.
- Aseptic Technique and Infection Control: Deep understanding and strict adherence to aseptic techniques to prevent surgical site infections.
- Communication and Teamwork: Demonstrating effective communication skills with the surgical team, including clear and concise reporting of observations.
- Troubleshooting and Problem-Solving: Ability to anticipate potential complications, react appropriately to unexpected situations, and contribute to effective problem-solving within the operating room.
- Safety Protocols and Emergency Response: Knowledge of emergency protocols and the ability to respond effectively to unexpected events within the operating room environment.
Next Steps
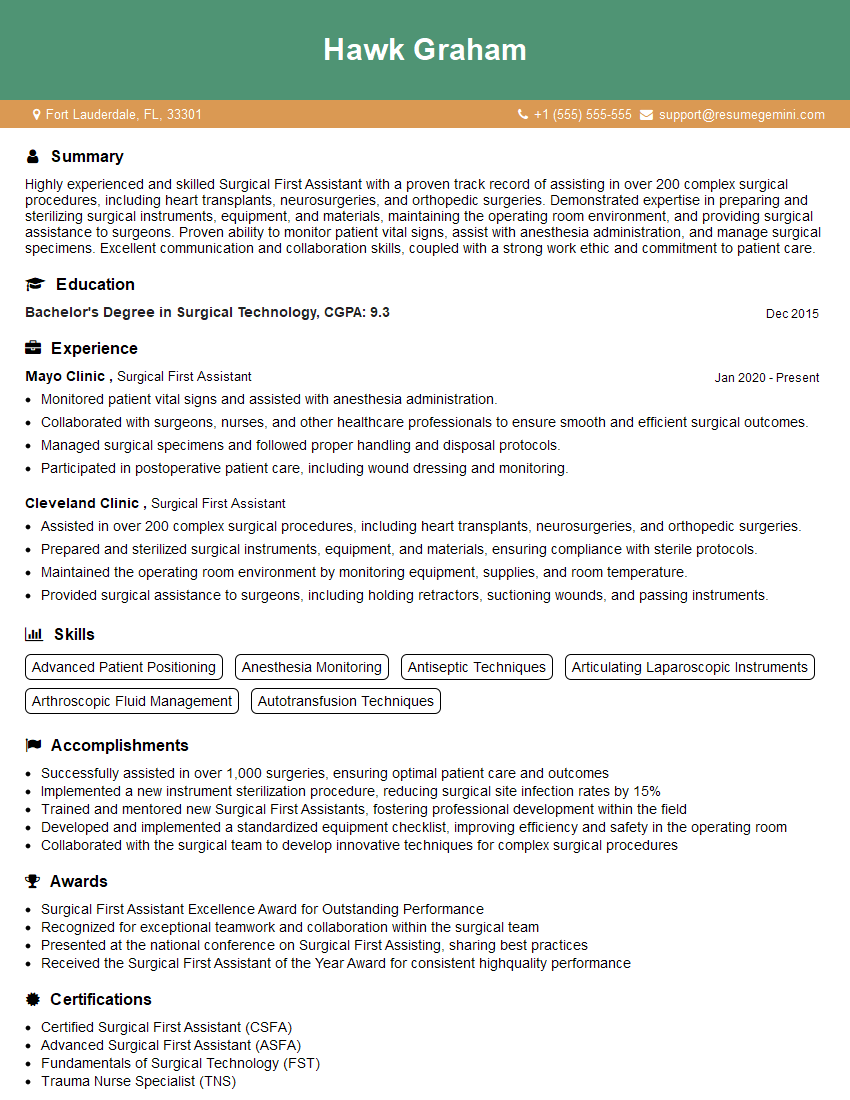
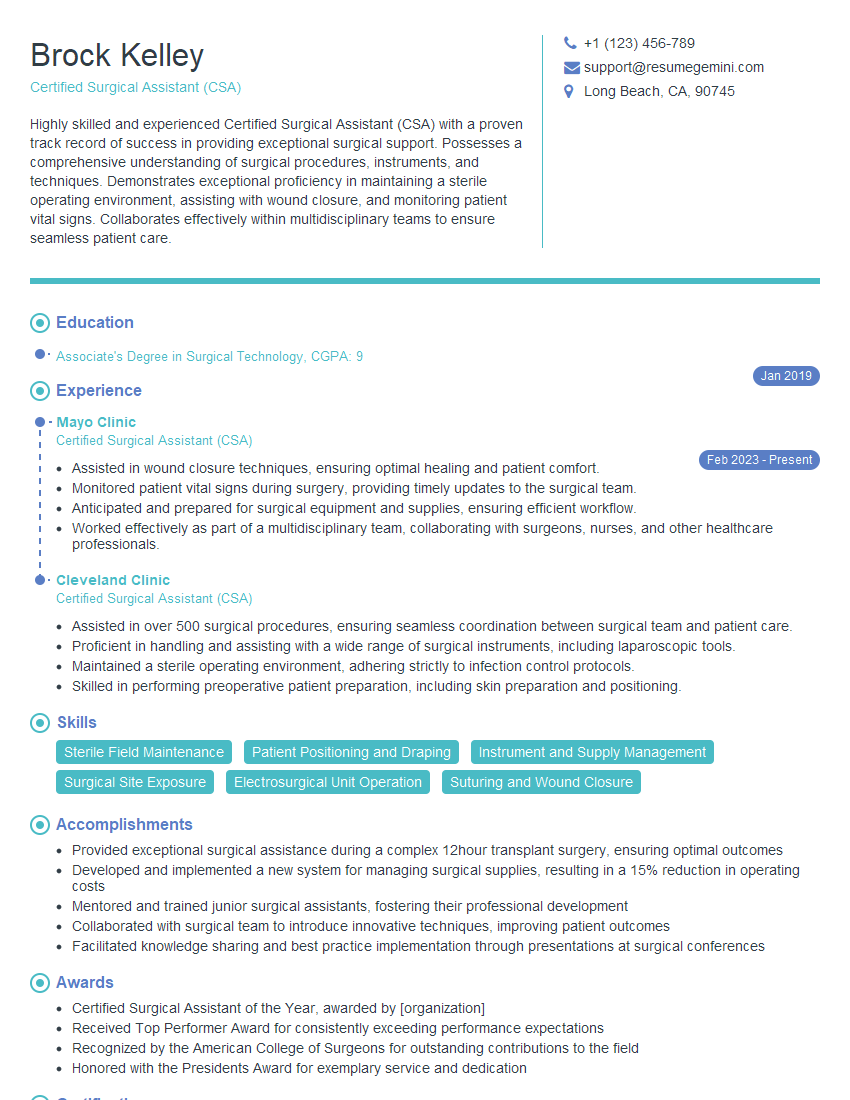
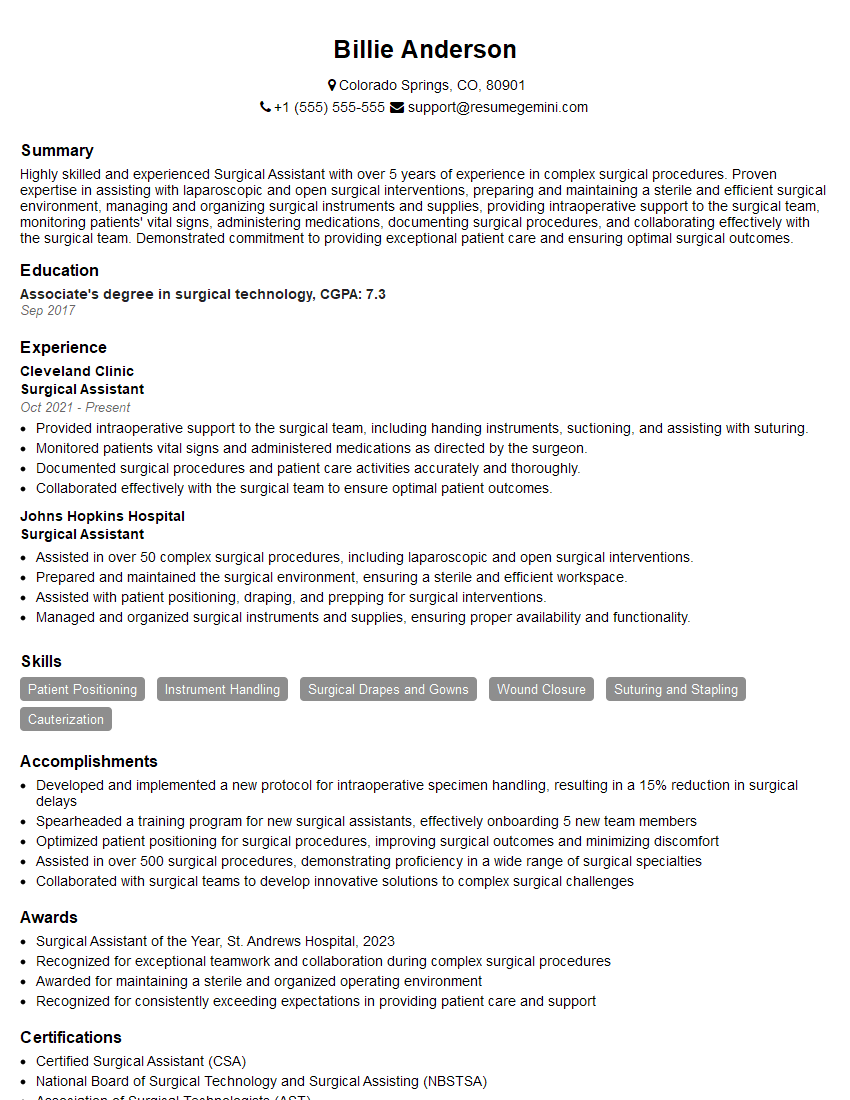
Mastering Surgical First Assist is crucial for career advancement, opening doors to specialized roles and increased responsibility within the surgical team. A well-crafted resume is your key to unlocking these opportunities. An ATS-friendly resume ensures your qualifications are effectively communicated to potential employers. To create a truly impactful resume, we recommend using ResumeGemini, a trusted resource for building professional resumes. ResumeGemini provides examples of resumes tailored to Surgical First Assist, helping you showcase your skills and experience effectively. Take the next step towards your career goals – build a resume that gets noticed.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.