Every successful interview starts with knowing what to expect. In this blog, we’ll take you through the top Enteral Feeding interview questions, breaking them down with expert tips to help you deliver impactful answers. Step into your next interview fully prepared and ready to succeed.
Questions Asked in Enteral Feeding Interview
Q 1. What are the different types of enteral feeding tubes?
Enteral feeding tubes come in various types, each designed for specific needs and durations. The choice depends on factors like the patient’s anatomy, anticipated duration of feeding, and the risk of aspiration. Here are some key examples:
- Nasogastric (NG) tubes: These are inserted through the nose and pass down into the stomach. They are commonly used for short-term feeding (less than 4 weeks).
- Nasoduodenal (ND) and Nasojejunal (NJ) tubes: These tubes are passed through the nose and into the duodenum or jejunum (parts of the small intestine). They are preferred when there is a risk of aspiration, such as with patients who have impaired gastric emptying.
- Gastrostomy (G-tube) and Jejunostomy (J-tube): These are surgically placed tubes directly into the stomach (G-tube) or jejunum (J-tube). They are used for long-term feeding.
- Percutaneous Endoscopic Gastrostomy (PEG) and Percutaneous Endoscopic Jejunostomy (PEJ): These tubes are placed endoscopically (through a small incision in the abdomen) and are also used for long-term feeding, offering a less invasive approach than open surgery.
The choice of tube depends on individual patient assessment by a healthcare professional.
Q 2. Describe the process of initiating enteral nutrition.
Initiating enteral nutrition involves a systematic process to ensure patient safety and efficacy. It begins with a thorough assessment of the patient’s nutritional needs, medical history, and potential complications.
- Assessment: This includes evaluating the patient’s nutritional status (BMI, weight loss history), identifying underlying medical conditions, and assessing the ability to tolerate feedings.
- Tube placement: The appropriate tube is selected and placed by a trained healthcare professional, usually a physician or nurse. X-ray confirmation is typically required to ensure correct placement.
- Formula selection: The type and concentration of enteral formula are chosen based on the patient’s individual needs and tolerances. Formulas vary in protein, carbohydrate, and fat content.
- Initial feeding: The initial feeding begins at a low rate and is gradually increased as tolerated, monitoring for any signs of intolerance such as nausea, vomiting, diarrhea, or abdominal discomfort. This gradual increase minimizes complications.
- Monitoring: Close monitoring of the patient’s fluid balance, bowel function, and overall clinical status is essential during the initiation phase. This includes checking residual volumes (amount of formula remaining in the stomach) and assessing for signs of infection or intolerance.
For instance, a patient recovering from a stroke might start with a low-volume continuous feeding via an NG tube, gradually increasing the rate as they tolerate it. This helps prevent aspiration and digestive upset.
Q 3. Explain the differences between bolus, continuous, and intermittent feeding.
Enteral feeding can be delivered in three primary methods, each with distinct advantages and disadvantages:
- Bolus feeding: This involves administering a large volume of formula over a short period (e.g., 200-500 mL over 5-15 minutes). It’s often the most convenient method, but it can cause gastric distention and increased risk of aspiration if gastric emptying is slow.
- Continuous feeding: This method delivers formula continuously at a slow rate over 24 hours using a feeding pump. It provides a constant supply of nutrients and minimizes gastric distention. This method is better tolerated by most patients but requires a pump.
- Intermittent feeding: This method delivers a smaller volume of formula over a longer period (e.g., 250-500 mL over 30-60 minutes) several times a day. It is a good compromise between bolus and continuous feeding and doesn’t require a pump. However, it may cause more frequent gastric distention compared to continuous feeding.
The best method depends on the patient’s tolerance, gastric emptying rate, and overall clinical status. For example, a patient with a history of gastroparesis (slow gastric emptying) might benefit from continuous feeding, while a patient with a good tolerance might receive intermittent feedings.
Q 4. How do you calculate enteral feeding requirements?
Calculating enteral feeding requirements is crucial to providing adequate nutrition. It involves considering the patient’s energy needs (kcal/day), protein requirements (grams/day), and fluid requirements (mL/day).
Several methods exist, but a common approach involves using the patient’s ideal body weight (IBW) and activity level. For example, the Harris-Benedict equation can estimate resting energy expenditure (REE), which is then adjusted for activity level to determine total energy needs. Protein requirements are often calculated based on the patient’s condition and may range from 0.8 to 2.0 grams/kg/day. Fluid requirements are usually estimated based on the patient’s weight and medical condition.
Example: A 70kg patient with moderate activity might require roughly 25 kcal/kg/day = 1750 kcal/day. Protein requirements could be 1g/kg/day = 70 grams/day. Fluid requirements might be 30 mL/kg/day = 2100 mL/day. This information is used to select a commercially available enteral formula or to tailor a customized formula.
It’s important to note that these calculations are estimations. A registered dietitian or nutritionist should be consulted to accurately determine individual nutrient needs, accounting for specific health conditions and complications.
Q 5. What are the common complications associated with enteral feeding, and how are they managed?
Enteral feeding, while beneficial, can lead to various complications. Prompt identification and management are vital.
- Aspiration pneumonia: This occurs when formula enters the lungs. Prevention involves careful tube placement verification, proper positioning (head of bed elevated), and slow feeding rates.
- Diarrhea: This can be caused by formula intolerance, bacterial overgrowth, or medication interactions. Management involves changing the formula, administering antidiarrheal medication if appropriate, and managing electrolytes.
- Constipation: This can result from decreased mobility or certain formulas. Management involves increasing fluid intake, adding fiber to the formula, and stool softeners.
- Nausea and vomiting: This can indicate formula intolerance or rapid feeding rate. Management includes slowing the feeding rate, changing the formula, or administering antiemetics.
- Tube displacement or blockage: Regular assessment of tube placement and flushing with water can prevent this. If blocked, enzymatic solutions may help. If displaced, repositioning or replacement may be necessary.
- Electrolyte imbalances: These imbalances can result from formula composition or poor absorption. Monitoring serum electrolytes and adjusting the formula or providing supplements are crucial.
For example, a patient developing diarrhea might require a change to a formula with a lower osmolality (reducing the concentration of solute) or the addition of fiber.
Q 6. How do you monitor for complications of enteral feeding?
Monitoring for complications of enteral feeding requires a multi-faceted approach. Regular assessment should include:
- Daily weight monitoring: To assess fluid balance and overall nutritional status.
- Vital signs: Monitoring heart rate, blood pressure, temperature, and respiratory rate for any signs of infection or dehydration.
- Bowel sounds and abdominal assessment: To assess for distention, tenderness, or ileus (intestinal obstruction).
- Gastric residual volumes (GRV): Measuring the amount of formula remaining in the stomach helps determine gastric emptying and adjust feeding rate.
- Electrolyte levels: Regular blood tests to monitor for imbalances such as hyponatremia, hypokalemia, or hyperglycemia.
- Stool consistency and frequency: To assess for diarrhea or constipation.
- Nutritional status: Monitoring albumin and pre-albumin levels helps assess overall nutritional response to enteral nutrition.
A nurse or other healthcare professional would be responsible for these measurements and would take action as needed. For instance, consistently high gastric residual volumes might necessitate a reduction in the feeding rate or a switch to a continuous feeding method.
Q 7. What are the indications for enteral feeding versus parenteral feeding?
Enteral and parenteral nutrition are both methods of providing nutrition when oral intake is insufficient or impossible. The choice depends on the patient’s gastrointestinal tract function and overall health.
- Enteral nutrition is preferred when the gastrointestinal tract is functional, even if partially. It uses the natural route of digestion and absorption, maintaining gut integrity and reducing the risk of infections associated with parenteral nutrition.
- Parenteral nutrition (PN) involves administering nutrients directly into the bloodstream, bypassing the gastrointestinal tract. It’s indicated when the gastrointestinal tract is non-functional or severely compromised (e.g., short bowel syndrome, severe pancreatitis, intestinal failure).
Example: A patient with a functioning gut but impaired swallowing ability following a stroke would be a candidate for enteral nutrition. A patient with severe inflammatory bowel disease and intestinal failure would require parenteral nutrition to maintain adequate nutrition.
The decision to use enteral or parenteral nutrition is a collaborative one made by a team of healthcare professionals, including physicians, dieticians, and nurses, after thorough patient assessment.
Q 8. How do you assess the patient’s tolerance to enteral feeding?
Assessing a patient’s tolerance to enteral feeding is crucial for ensuring safe and effective nutrition delivery. We monitor for several key indicators. Think of it like introducing a new food – you wouldn’t go from nothing to a whole feast at once!
- Gastrointestinal Symptoms: We closely watch for diarrhea, constipation, nausea, vomiting, abdominal distension, and cramping. These are telltale signs of intolerance. For example, if a patient experiences persistent diarrhea after starting enteral feeding, we might need to slow down the rate or change the formula.
- Residual Volume: We regularly check the residual volume (the amount of formula left in the stomach) using a syringe. High residual volumes (generally >250ml) can indicate gastric emptying issues, potentially leading to aspiration (food entering the lungs) and necessitating a reduction in feeding rate or formula type change.
- Weight and Nutritional Status: We monitor weight changes, calorie intake, and laboratory values like albumin and pre-albumin to assess nutritional status and the effectiveness of the feeding. Weight gain is a positive sign; consistent weight loss warrants investigation.
- Electrolyte Balance: We pay close attention to blood electrolyte levels, as some formulas can affect electrolyte balance. Any imbalances require adjustments to the feeding plan or supplemental electrolyte solutions.
- Patient’s Subjective Report: Importantly, we actively involve patients in their care. We regularly ask them about any discomfort or changes they’ve noticed.
By systematically monitoring these aspects, we can fine-tune the feeding regimen to optimize tolerance and nutritional outcomes. We may need to adjust feeding rates, formula types, or even the feeding route based on the patient’s response.
Q 9. Explain the importance of proper tube placement verification.
Proper tube placement verification is paramount to prevent life-threatening complications like aspiration pneumonia. Imagine pouring milk into the wrong pipe – it’s disastrous! We use several methods to confirm correct tube placement:
- X-ray Confirmation: This is the gold standard. A chest x-ray visually confirms that the tube is in the stomach or small intestine and not in the lungs.
- pH Testing: Aspiration of gastric contents reveals a pH of less than 5.5. This provides a quick check, although it’s less definitive than an X-ray and doesn’t reliably differentiate between the stomach and duodenum.
- Air Bolus Insufflation and Auscultation: While less accurate than x-ray or pH testing, this involves injecting a small amount of air into the tube and listening for gurgling sounds over the stomach using a stethoscope. It’s a quick, bedside method, but is prone to errors.
- Visual Confirmation (if possible): For nasogastric tubes, visualization of the tube entering the stomach during insertion is possible, but should be supported by further verification methods.
Regardless of the method used, documentation is critical. We meticulously record the method used, the findings, and any actions taken. This ensures transparency and accountability in patient care. Failure to confirm proper placement can have severe, and potentially fatal consequences.
Q 10. How do you manage medication administration via enteral feeding tubes?
Administering medications through enteral feeding tubes requires careful attention to detail to ensure accurate dosing and avoid drug interactions. Think of it as careful recipe following!
- Check for Compatibility: Not all medications can be administered through enteral feeding tubes. Some medications may be inactivated or cause clogging. We always consult a drug reference to verify compatibility before administration. Certain medications shouldn’t be crushed, so an alternate delivery method must be sought.
- Crush and Dissolve: If the medication can be crushed, we crush the tablet to a fine powder and mix it thoroughly with a small amount of lukewarm water. If possible, avoid mixing with the entire feeding volume, as this might lead to uneven distribution.
- Flush Before and After: Before and after administering medication, we flush the tube with sterile water (typically 15-30ml) to prevent clogging and ensure complete delivery of the medication. We’re trying to prevent the medication from sticking to the tube wall!
- Hold Feeding: We may temporarily hold the feeding before and after medication administration to allow for absorption and prevent interference with drug absorption. This duration depends on the specific medication and patient’s needs.
- Medication Administration Record: Accurate and diligent documentation is essential. We carefully note the medication administered, the dose, the time of administration, and the flushing procedure.
Improper medication administration via enteral feeding tubes can result in inaccurate dosing, drug interactions, and other complications. Adhering to these guidelines and thoroughly documenting every step is paramount.
Q 11. Describe the process of weaning a patient off enteral feeding.
Weaning a patient off enteral feeding is a gradual process that aims to safely transition them back to oral intake. It’s like slowly adjusting to a new diet after a long illness. We carefully monitor the patient’s progress throughout the process:
- Assessment of Oral Intake: We assess the patient’s ability to swallow safely and their appetite. A speech therapist may be involved in this assessment to ensure there’s no risk of aspiration.
- Gradual Reduction of Enteral Feedings: We begin by slowly decreasing the volume and/or frequency of enteral feedings while simultaneously increasing the amount of oral intake. We might start by supplementing small oral meals, then progress to more substantial food amounts as tolerated.
- Monitoring Tolerance: We closely monitor the patient’s tolerance for oral intake and watch for any signs of gastrointestinal distress. This includes stool consistency, abdominal pain, nausea, and vomiting.
- Nutritional Adequacy: We ensure that the patient is receiving adequate nutrition and hydration through a combination of oral and enteral intake during the weaning process. This might involve nutritional supplementation if needed.
- Discontinuation of Enteral Feeding: When the patient is able to maintain adequate nutritional intake orally and demonstrates consistent tolerance for several days, we can safely discontinue the enteral feeding.
The weaning process must be tailored to each patient’s individual needs and capabilities, ensuring a safe and effective transition from enteral to oral nutrition.
Q 12. How do you handle tube clogging or dislodgement?
Tube clogging and dislodgement are common challenges in enteral feeding. It’s a bit like dealing with plumbing issues! We have strategies to address both situations:
- Tube Clogging: The first step is to try flushing the tube with warm water or a commercially available enzymatic solution. If this is unsuccessful, we might try using a smaller-diameter catheter to gently break up the clog. If these methods fail, the tube might need to be replaced.
- Tube Dislodgement: If the tube is dislodged, we immediately assess the patient’s condition and check for any signs of distress. We then notify the physician and follow facility protocols for tube replacement. This often requires re-verification of tube placement through an X-ray.
Prevention is key. We instruct patients and caregivers on how to prevent clogging (e.g., flushing frequently) and dislodgement (e.g., secure taping). Early detection and prompt action can minimize complications and ensure continued safe nutrition.
Q 13. What are the different types of enteral formulas, and when are they indicated?
Enteral formulas are designed to meet various nutritional needs. Choosing the right formula is like selecting ingredients for a specific recipe. There’s not a one-size-fits-all approach.
- Standard Formulas: These provide a balanced mix of macronutrients (protein, carbohydrates, fats) suitable for patients with normal digestive function. They are cost-effective and widely available.
- Elemental Formulas: These formulas contain pre-digested nutrients, making them suitable for patients with malabsorption issues or impaired digestion. They’re easy to digest, but less palatable and more costly.
- Specialty Formulas: These formulas address specific nutritional needs. Examples include formulas for renal failure, diabetes, or pulmonary disease. These formulas are tailored to address specific needs, but also more expensive.
- Fiber-Enriched Formulas: These formulas help promote regular bowel movements, which is particularly important for patients prone to constipation. They support gut health.
The choice of formula is determined by the patient’s underlying medical condition, digestive capabilities, and specific nutritional requirements. A registered dietitian plays a key role in selecting the most appropriate formula and adjusting it as needed.
Q 14. What are the nutritional needs of a patient receiving enteral feeding?
The nutritional needs of a patient receiving enteral feeding vary depending on several factors, including age, weight, activity level, and underlying medical conditions. Meeting these needs is akin to building a strong house – you need the right materials and construction!
- Macronutrients: Adequate intake of carbohydrates, proteins, and fats is crucial for energy production, tissue repair, and overall body function. The precise ratios will depend on the individual’s condition.
- Micronutrients: Vitamins and minerals are essential for various metabolic processes. Formulas often provide these, but supplementation may be necessary based on individual assessments.
- Fluid Balance: Maintaining adequate hydration is essential. The amount of fluid needed will depend on the patient’s condition, fluid losses (e.g., fever, diarrhea), and other factors.
- Energy Requirements: Calculating the patient’s daily energy requirements is vital for providing sufficient calories to support their metabolic needs. This often involves considering resting energy expenditure (REE) and activity levels.
- Individualized Needs: Patients with specific medical conditions may require adjustments to meet their unique nutritional needs. For instance, a patient with kidney disease will need a formula that considers their renal function.
A registered dietitian conducts a thorough nutritional assessment to determine the patient’s specific needs and develops a feeding plan accordingly. Regular monitoring and adjustments are vital to ensure optimal nutritional support.
Q 15. How do you monitor the effectiveness of enteral feeding?
Monitoring the effectiveness of enteral feeding involves a multifaceted approach, focusing on both the physiological response of the patient and the technical aspects of the feeding process. We want to ensure the patient is receiving adequate nutrition and that there are no complications.
- Weight monitoring: Regular weight checks are crucial. A consistent, gradual weight gain is a positive sign. Unexpected weight loss warrants investigation.
- Laboratory values: Blood tests, such as complete blood counts (CBC) and serum albumin levels, help assess nutritional status and identify potential deficiencies. Electrolyte levels are also closely monitored to detect imbalances.
- Clinical observations: We look for signs of adequate hydration (good skin turgor, urine output), bowel function (regular stools), and the absence of complications like diarrhea or nausea. Patient tolerance, such as the absence of abdominal cramping or distension, is also important.
- Feeding residual volume: Measuring the amount of formula remaining in the stomach before the next feeding helps assess gastric emptying. Elevated residuals may indicate a problem such as intolerance or delayed gastric emptying.
- Caloric intake and nutritional markers: We assess whether the patient is receiving the prescribed amount of calories and nutrients. This often involves comparing the prescribed formula to the patient’s daily requirements.
For instance, a patient with low albumin levels despite adequate caloric intake might indicate a protein deficiency, requiring a formula adjustment or supplementation. Similarly, consistently high residual volumes could signify a need for slowing the infusion rate or changing the formula.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What are the key components of an enteral feeding plan?
A comprehensive enteral feeding plan is essential for patient safety and successful nutritional support. Key components include:
- Patient assessment: Thorough assessment of the patient’s nutritional needs, medical history, and current condition is paramount. This includes calculating their caloric and macronutrient requirements.
- Formula selection: Choosing the right formula depends on the patient’s individual needs. Factors considered include age, disease state, allergies, and tolerance. Formulas vary in nutrient density, fiber content, and osmolality.
- Administration route: Determining the appropriate access route (nasogastric, nasoduodenal, or jejunal) depends on factors such as gastric emptying, risk of aspiration, and the patient’s anatomy. Nasogastric tubes are commonly used for short-term feeding, whereas jejunal tubes might be necessary for patients with impaired gastric emptying.
- Feeding schedule and rate: The feeding schedule (continuous, intermittent, or bolus) and rate are crucial for optimizing nutrient delivery and minimizing complications. The rate should be gradually increased as tolerated to prevent intolerance.
- Monitoring plan: A detailed monitoring plan, including frequency of weight checks, laboratory tests, and residual volume measurements, is vital. This plan is tailored to the patient’s individual needs and risk factors.
- Education and support: Educating the patient and their family on all aspects of the feeding process is crucial for successful home management and adherence to the plan.
For example, a patient with pancreatitis might require a low-fat formula, while a patient with diabetes needs a formula that manages blood glucose levels effectively.
Q 17. What are the legal and ethical considerations surrounding enteral feeding?
Enteral feeding raises several legal and ethical considerations, particularly concerning patient autonomy and capacity. It is crucial to respect a patient’s right to refuse treatment, even if that means forgoing potentially life-sustaining nutrition.
- Informed consent: Patients or their legal guardians must provide informed consent before initiating enteral feeding. This involves a thorough explanation of the procedure, benefits, risks, and alternatives.
- Capacity assessment: If a patient lacks capacity to make decisions, their wishes should be determined through consultation with family members, advance directives (if any), and ethical review boards.
- End-of-life care: Enteral feeding may become ethically problematic in end-of-life situations. If it prolongs suffering without substantial benefit, it might be considered medically futile and ethically questionable.
- Resource allocation: The cost-effectiveness of enteral feeding must be considered. This is particularly relevant in resource-constrained settings, where the financial burden of long-term enteral nutrition must be weighed against potential benefits.
- Legal documentation: All decisions relating to the initiation, continuation, or cessation of enteral feeding should be meticulously documented.
A delicate balance needs to be struck between respecting patient autonomy and providing the best possible medical care. Ethical consultation is often valuable in resolving complex cases.
Q 18. How do you educate patients and families about enteral feeding?
Educating patients and families about enteral feeding is crucial for successful outcomes and compliance. The process involves clear, concise communication tailored to their understanding.
- Initial explanation: Start with a clear and simple explanation of why enteral feeding is necessary, its purpose, and the expected duration. Use visuals and analogies to improve understanding.
- Practical demonstrations: Demonstrate how to prepare and administer the formula, clean and maintain the feeding tube and pump, and identify potential complications. Role-playing can be helpful.
- Troubleshooting guidance: Teach patients and families how to identify and manage common problems such as clogged tubes, leaks, or formula intolerance. Provide written instructions and contact information for support.
- Ongoing support: Provide regular follow-up to answer questions, address concerns, and adjust the feeding plan as needed. A support group can help patients feel less isolated and build community.
- Cultural sensitivity: Be mindful of cultural beliefs and practices that may impact patient understanding and acceptance of enteral feeding.
For example, providing a written checklist and step-by-step instructions makes it easier for caregivers to understand the feeding routine at home. Regular phone calls and follow-up appointments provide continued support and address any arising questions.
Q 19. What is the role of the interdisciplinary team in managing enteral feeding?
Managing enteral feeding effectively requires a coordinated effort from an interdisciplinary team. Each member plays a crucial role in ensuring patient safety and optimal nutritional outcomes.
- Physician: Prescribes the enteral feeding plan, monitors the patient’s progress, and makes necessary adjustments to the regimen.
- Registered Dietitian (RD): Calculates the patient’s nutritional requirements, selects the appropriate formula, and monitors nutritional status through laboratory values and clinical observations.
- Nurse: Administers the enteral feeding, monitors for complications, and provides education to patients and families.
- Pharmacist: Ensures safe medication administration through the enteral route and monitors for potential drug interactions.
- Speech-Language Pathologist (SLP): Evaluates the patient’s swallowing function and assesses the risk of aspiration, especially if the patient is also receiving oral intake.
- Physical/Occupational Therapist: Addresses mobility and functional limitations and works to improve the patient’s overall strength and well-being.
Effective communication and collaboration among these professionals are essential to optimize patient care and achieve the best possible outcomes. Regular team meetings and shared documentation systems facilitate this collaboration.
Q 20. Describe your experience with different types of enteral feeding pumps.
I have extensive experience with various enteral feeding pumps, including both volumetric and peristaltic pumps. The choice of pump depends on the patient’s needs and clinical context.
- Volumetric pumps: These pumps deliver a predetermined volume of formula over a specific period. They are commonly used for continuous or intermittent feeding. They are generally more affordable but require more careful monitoring to prevent over-infusion or bolus delivery if not set correctly.
- Peristaltic pumps: These pumps use a roller mechanism to propel formula through the tube. They are more precise, gentler on the gut, and better at handling thicker formulas. They are typically used for patients with higher risk of aspiration or intolerance.
- Syringe pumps: These are simpler pumps used for intermittent bolus feeding, where a set volume of formula is delivered over a short period. They are suitable for some patients but lack the precision and flexibility of volumetric and peristaltic pumps.
For example, a patient with a history of gastroparesis (delayed gastric emptying) might benefit from a peristaltic pump delivering the formula at a slow, continuous rate to minimize the risk of nausea and vomiting. A patient with a simple feeding need might do well with a less expensive volumetric pump with intermittent feeding delivery.
Q 21. How do you troubleshoot common problems with enteral feeding pumps?
Troubleshooting enteral feeding pumps often involves a systematic approach to identify and resolve the problem.
- Check for obvious issues: Ensure the pump is properly plugged in, the tubing is correctly connected, and the formula bag is full and not leaking. Check for kinks or blockages in the tubing.
- Review pump settings: Confirm that the pump is programmed correctly with the correct volume, rate, and duration. Incorrect programming is a common source of errors.
- Assess the feeding tube: Check the feeding tube for patency and ensure that it is not clogged. If a blockage is suspected, try flushing the tube with warm water according to established protocols. If the blockage persists, consult with a healthcare provider.
- Examine the formula: Inspect the formula for any signs of spoilage or clumping that could cause blockages. Ensure the formula is at the correct temperature and mixed properly.
- Check for alarms: Note any alarms triggered by the pump and refer to the manufacturer’s instructions for troubleshooting. Alarms indicate possible malfunctions or problems that require attention.
If the problem persists despite these troubleshooting steps, contact the equipment supplier or healthcare provider for assistance. It is crucial to act promptly to avoid delaying or interrupting the feeding.
Q 22. What are the signs and symptoms of aspiration?
Aspiration, the entry of gastric contents into the lungs, is a serious complication of enteral feeding. Signs and symptoms can range from subtle to dramatic. Subtle signs might include coughing during or after feeding, increased respiratory rate, or a change in oxygen saturation. More overt signs include choking, cyanosis (bluish discoloration of the skin), and frank respiratory distress. Patients may also experience fever, pneumonia, or altered mental status. It’s crucial to remember that the absence of overt symptoms doesn’t rule out aspiration; silent aspiration can occur.
- Coughing: A frequent sign, especially immediately after feeding.
- Wheezing or rales (crackles): Sounds heard upon auscultation (listening to the lungs with a stethoscope).
- Fever: Indicative of infection due to aspiration.
- Increased respiratory rate or difficulty breathing: A hallmark of respiratory compromise.
- Cyanosis: A bluish discoloration of the lips and fingertips, indicating low oxygen levels.
Early detection is vital for prompt intervention and preventing further complications.
Q 23. How do you prevent aspiration during enteral feeding?
Preventing aspiration during enteral feeding is paramount. A multi-faceted approach is essential. This includes accurate tube placement verification (X-ray confirmation is the gold standard), proper head-of-bed elevation (at least 30 degrees), and careful monitoring of residual volume (the amount of feeding remaining in the stomach). We should also assess the patient’s swallowing ability and level of consciousness regularly. Using a small-bore feeding tube can also minimize the risk of aspiration. Furthermore, bolus feedings (giving the entire volume at once) carry a higher risk than continuous feedings. Slowing the rate of administration, especially with thicker formulas, is crucial. Thickened formulas themselves help reduce the likelihood of reflux and aspiration.
- Confirm Tube Placement: Always verify tube placement using an X-ray before initiating feedings and periodically if there’s any concern.
- Head-of-Bed Elevation: Keep the patient’s head elevated to at least 30 degrees to facilitate gravity-assisted emptying of the stomach.
- Monitor Residual Volume: Regularly check gastric residual volume. If it’s excessively high, it suggests poor gastric emptying, indicating a need to slow the feeding rate or hold the feeding temporarily.
- Appropriate Feeding Method: Continuous feedings are generally safer than bolus feedings.
- Thickened Feedings: Consider using thickened feeding formulas if aspiration risk is high.
Q 24. How do you assess a patient’s ability to tolerate different feeding rates?
Assessing a patient’s tolerance to different feeding rates involves careful observation and monitoring. We start with a slow rate, gradually increasing it based on the patient’s response. Signs of intolerance include abdominal distension (a swollen belly), nausea, vomiting, diarrhea, or increased gastric residual volumes. We should monitor vital signs for any changes that might indicate distress. If any of these signs occur, the feeding rate needs to be slowed or temporarily stopped. Regularly checking the patient’s weight and assessing their nutritional status provide valuable data about their tolerance and effectiveness of the feeding regime. Each individual responds differently, requiring individualized titration. Imagine a car engine – you wouldn’t push it to full throttle right away; the same principle applies to enteral feeding.
- Start Slow: Begin with a low feeding rate and gradually increase it over time.
- Monitor for Intolerance: Watch for signs of intolerance, such as abdominal distension, vomiting, diarrhea, or high gastric residual volumes.
- Assess Vital Signs: Monitor heart rate, blood pressure, and respiratory rate.
- Regular Weight Checks: Track the patient’s weight to assess the effectiveness of nutrition delivery.
- Individualized Approach: Feeding rate adjustments are essential based on patient response.
Q 25. Explain the importance of regular tube flushing.
Regular tube flushing is crucial for maintaining patency (keeping the tube open) and preventing blockages. Formula can thicken and clog the tube, especially with certain types of enteral formulas. Flushing with water after each feeding and before and after medication administration helps prevent blockages. Using a sufficient amount of water is also important; using too little is not effective. Regular flushing helps to ensure that the patient receives the complete prescribed volume of nutrition. A clogged tube would significantly delay nutrient delivery. Think of it like regularly cleaning a water pipe to prevent blockages.
- After Each Feeding: Flush the tube with water to clear any residual formula.
- Before and After Medication: Flush the tube to ensure medication administration and prevent clogging.
- Appropriate Volume: Use an adequate volume of water to effectively flush the tube.
- Prevent Blockages: Regular flushing helps prevent clogging and ensures proper nutrient delivery.
Q 26. What is your experience with different types of enteral access?
My experience encompasses a wide range of enteral access methods. Nasogastric (NG) tubes are commonly used for short-term access, inserted through the nose and into the stomach. Nasoduodenal (ND) and naso-jejunal (NJ) tubes are advanced further into the small intestine, reducing the risk of aspiration, but require X-ray confirmation of placement. Gastrostomy (G-tube) and jejunostomy (J-tube) tubes offer long-term access surgically placed directly into the stomach or jejunum (part of the small intestine), respectively. The choice depends on factors like the patient’s condition, anticipated duration of feeding, and risk of aspiration. Each method has specific insertion and care procedures that require meticulous attention to detail and adherence to infection control guidelines.
- Nasogastric (NG) Tubes: Short-term access, inserted through the nose.
- Nasoduodenal (ND) and Nasojejunal (NJ) Tubes: Reduce aspiration risk, require X-ray confirmation.
- Gastrostomy (G-Tube) and Jejunostomy (J-Tube): Long-term access, surgically placed.
Selecting the appropriate method is paramount for patient safety and optimal nutrition.
Q 27. How do you manage diarrhea associated with enteral feeding?
Diarrhea associated with enteral feeding can be a significant concern, potentially leading to dehydration and electrolyte imbalances. Managing it requires a systematic approach. First, we investigate the cause – it could be related to the formula’s osmolarity (the concentration of dissolved substances), bacterial contamination, or medication interactions. We might adjust the formula, slow the feeding rate, or change to a different formula. In some cases, medications like loperamide may be necessary, but only with careful consideration of potential side effects and in consultation with a physician. Frequent monitoring of the patient’s hydration status and electrolytes is critical.
- Identify Cause: Investigate potential causes, such as formula osmolarity, bacterial contamination, or medication interactions.
- Adjust Feeding Rate: Slowing the feeding rate can sometimes alleviate diarrhea.
- Formula Change: Switching to a different formula may be necessary.
- Medication: In some cases, anti-diarrheal medication may be prescribed under medical supervision.
- Hydration and Electrolyte Monitoring: Closely monitor hydration status and electrolyte levels.
Proactive management of diarrhea ensures the patient maintains adequate hydration and nutritional support.
Q 28. How do you address concerns about patient and family education related to enteral feeding?
Patient and family education is crucial for successful enteral feeding. I approach this with a patient-centered, empathetic approach, using clear, simple language and avoiding jargon. Education starts with explaining the rationale for enteral nutrition and the specific feeding regimen. I demonstrate proper tube care, medication administration, and troubleshooting techniques. I provide written materials and answer any questions the patient and family may have. I encourage participation in the process and empower them to manage their loved one’s care effectively. Follow-up sessions address any ongoing concerns and reinforce learned skills. Remember, patient and family understanding leads to better adherence and outcomes. It’s like learning to drive – thorough instruction leads to confident driving. In this case, it’s confident caregiving.
- Clear Explanation: Use simple language and avoid technical jargon.
- Demonstration: Show proper tube care, medication administration, and troubleshooting techniques.
- Written Materials: Provide handouts or other materials that reiterate key information.
- Q&A Session: Allow time for questions and address any concerns.
- Follow-up: Schedule follow-up sessions to reinforce learning and answer any further questions.
Key Topics to Learn for Enteral Feeding Interview
- Indications and Contraindications: Understanding the patient populations appropriate for enteral nutrition and those for whom it’s contraindicated. Consider various medical conditions and their impact on enteral feeding decisions.
- Types of Enteral Access: Become proficient in the different methods of enteral access (e.g., nasogastric, nasoduodenal, jejunostomy tubes) and their respective advantages and disadvantages. Be prepared to discuss insertion techniques and complications.
- Formula Selection and Administration: Master the principles of selecting appropriate enteral formulas based on patient needs (e.g., nutritional requirements, allergies, disease states). Discuss safe administration techniques and monitoring for complications.
- Monitoring and Assessment: Familiarize yourself with the essential parameters for monitoring patients receiving enteral nutrition, including weight, bowel sounds, residual volumes, and laboratory values. Understand how to assess tolerance and address potential complications.
- Troubleshooting and Problem Solving: Be ready to discuss common problems encountered during enteral feeding (e.g., tube displacement, aspiration, diarrhea, constipation) and effective strategies for their management. Consider practical solutions and appropriate interventions.
- Ethical and Legal Considerations: Understand the ethical and legal implications surrounding enteral feeding, including informed consent, patient autonomy, and end-of-life care.
- Medication Administration via Enteral Route: Be prepared to discuss the safe and effective administration of medications through enteral feeding tubes, including compatibility issues and potential drug interactions.
- Documentation and Record Keeping: Understand the importance of accurate and thorough documentation of enteral feeding procedures, patient responses, and any complications encountered.
Next Steps
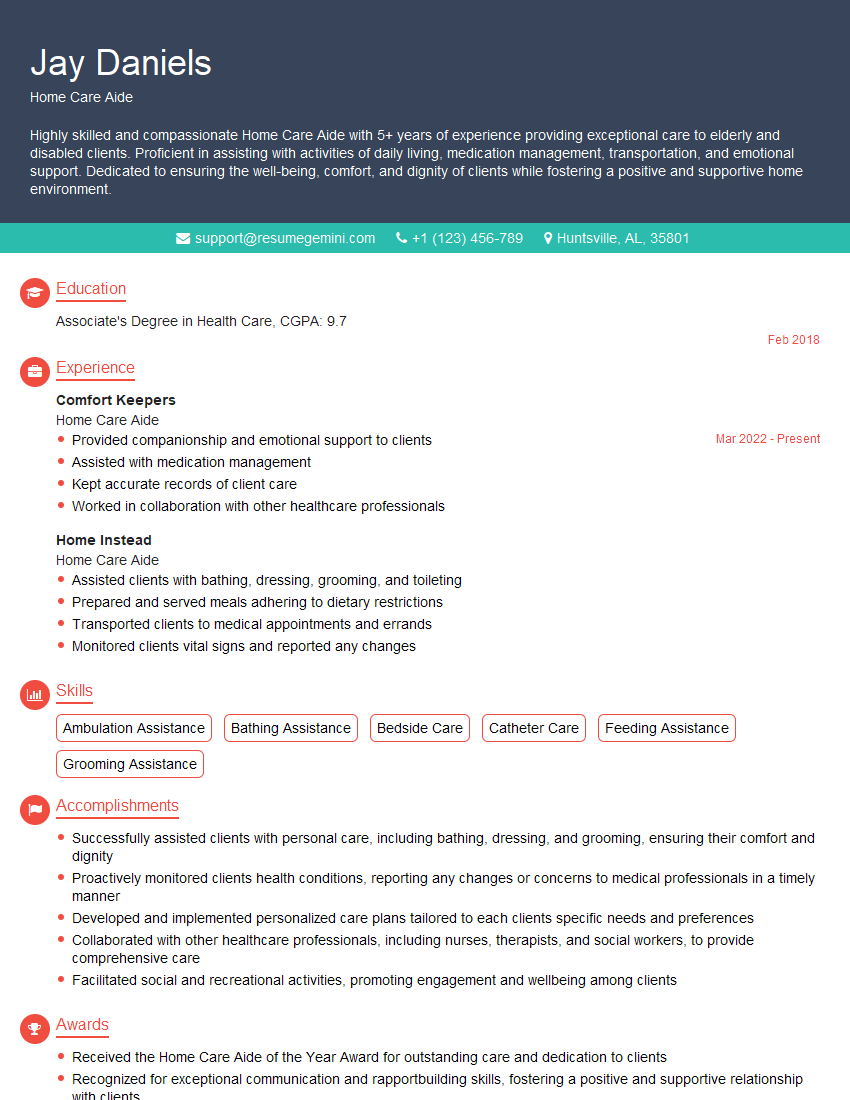
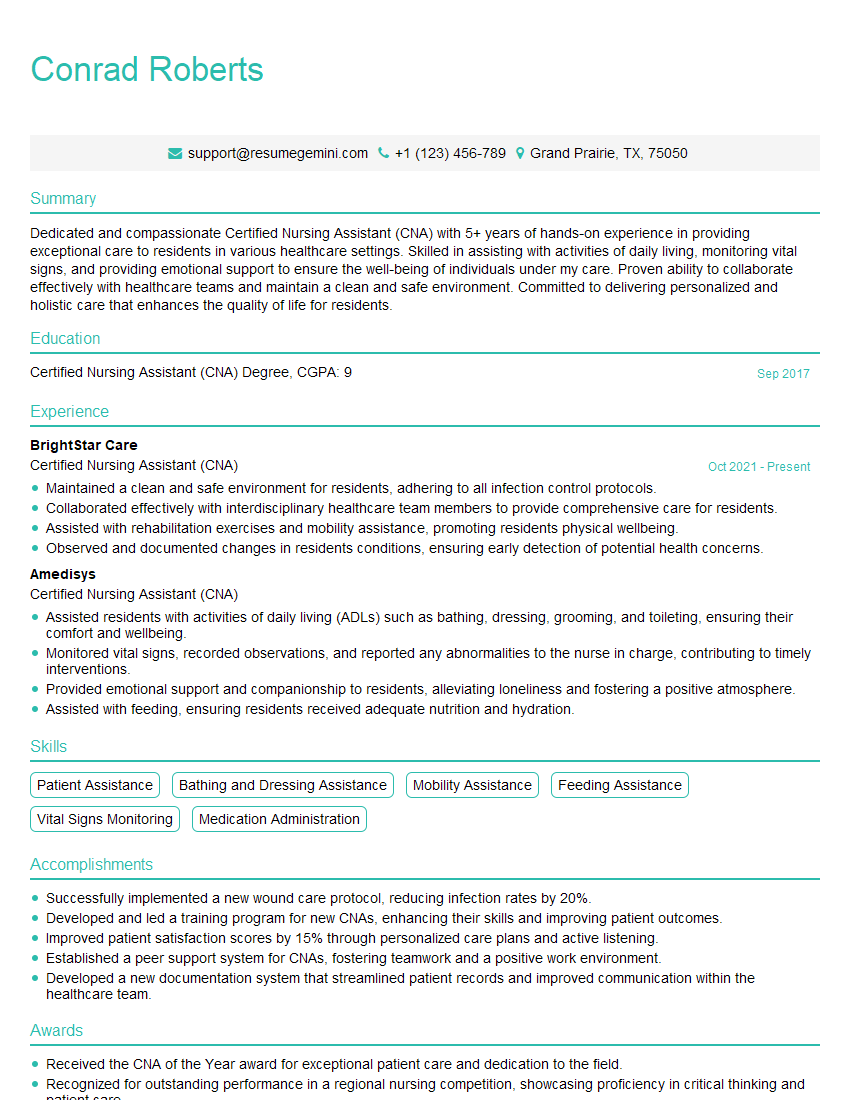
Mastering enteral feeding demonstrates a critical skill set highly valued in healthcare settings, opening doors to specialized roles and career advancement. To maximize your job prospects, crafting a strong, ATS-friendly resume is essential. ResumeGemini is a trusted resource to help you build a professional resume that showcases your skills and experience effectively. Examples of resumes tailored to Enteral Feeding are available, allowing you to create a compelling application that stands out from the competition.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.