Feeling uncertain about what to expect in your upcoming interview? We’ve got you covered! This blog highlights the most important Colonoscopy with Polypectomy interview questions and provides actionable advice to help you stand out as the ideal candidate. Let’s pave the way for your success.
Questions Asked in Colonoscopy with Polypectomy Interview
Q 1. Describe the indications for colonoscopy with polypectomy.
Colonoscopy with polypectomy is indicated primarily for the detection and removal of polyps in the colon and rectum. These polyps, while often benign, can sometimes be precancerous (adenomas) or cancerous. Therefore, removing them is crucial for preventing colorectal cancer. Indications include:
- Abnormal screening results: Positive fecal occult blood test (FOBT), positive stool DNA test, or abnormal findings on a prior colonoscopy.
- Surveillance for adenomas: Regular colonoscopies are recommended for individuals with a history of adenomas to detect and remove new polyps.
- Symptomatic patients: Patients experiencing symptoms such as rectal bleeding, changes in bowel habits, abdominal pain, or anemia may undergo colonoscopy with polypectomy if polyps are discovered.
- Family history of colorectal cancer or polyps: Individuals with a strong family history are at increased risk and often require more frequent surveillance colonoscopies with polypectomy if needed.
Essentially, any time a polyp is visualized during a colonoscopy, removal is usually recommended, especially if it’s large or has concerning features.
Q 2. Explain the different types of colonoscopic polypectomy techniques.
Several techniques are employed for colonoscopic polypectomy, depending on the polyp’s size, location, and morphology. The most common methods include:
- Snare polypectomy: This is the most frequently used technique for larger polyps (generally >5mm). A wire snare is looped around the polyp’s base, and the polyp is resected using electrocautery.
- Hot biopsy forceps polypectomy: This method uses heated biopsy forceps to remove smaller polyps (<5mm) and sessile (flat) polyps. The heat seals the blood vessels, reducing the risk of bleeding.
- Cold biopsy forceps polypectomy: Used for very small, flat polyps where the risk of bleeding is minimal, this technique involves using standard biopsy forceps without electrocautery.
- Endoscopic mucosal resection (EMR): This advanced technique is used for larger, flat, or laterally spreading lesions that cannot be safely removed with snare polypectomy. It involves submucosal injection to elevate the lesion before resection.
- Endoscopic submucosal dissection (ESD): This is the most extensive technique and is reserved for very large and/or deeply invasive lesions. It involves the dissection of the lesion from the submucosa, allowing for en bloc resection.
The choice of technique depends on individual polyp characteristics and the endoscopist’s expertise.
Q 3. What are the contraindications for colonoscopy with polypectomy?
Contraindications for colonoscopy with polypectomy are generally relative rather than absolute, meaning the procedure may still be performed with careful consideration and management. These include:
- Severe active inflammatory bowel disease (IBD): The risk of perforation is significantly increased in patients with active colitis or Crohn’s disease.
- Uncontrolled bleeding diathesis: Patients with uncontrolled bleeding disorders (e.g., hemophilia) may be at higher risk of significant bleeding during and after the procedure.
- Severe cardiac or pulmonary disease: The procedure requires sedation, and patients with severe cardiac or pulmonary compromise may experience adverse events.
- Severe infection: Active infection, especially sepsis, increases surgical risk and may worsen due to the procedure.
- Recent abdominal surgery: The risk of perforation is elevated following recent abdominal surgery.
Careful risk-benefit assessment is critical in patients with these conditions. For example, a patient with well-controlled IBD might undergo the procedure with close monitoring, while one with severe, uncontrolled bleeding would likely be deferred.
Q 4. Detail the steps involved in performing a snare polypectomy.
Snare polypectomy is a common technique for removing larger polyps. Here’s a step-by-step description:
- Polypectomy snare placement: The snare is carefully placed around the base of the polyp, ensuring that the snare is completely encircling the polyp’s base to prevent incomplete resection.
- Suction and lifting: Gentle suction is often applied through the scope’s channels to help lift the polyp away from the bowel wall, providing better visualization.
- Electrocautery activation: After confirming the snare placement, electrocautery is applied using a slow, controlled resection technique; continuous cutting/coagulation mode is usually preferred.
- Resection of the polyp: The polyp is gradually resected by tightening the snare while continuing the electrocautery. The goal is a clean resection with minimal bleeding.
- Examination of the resection site: After resection, the site is carefully examined for any residual polyp tissue or active bleeding. Additional electrocautery may be used for hemostasis (bleeding control).
- Specimen retrieval: The resected polyp is retrieved for pathological examination to determine its histology (type of tissue).
Throughout the procedure, close monitoring of the patient’s vital signs and continuous assessment of bleeding is crucial. Experienced endoscopists use various techniques to minimize the risk of complications. For example, careful snare placement and slow, controlled resection minimize the chances of perforation.
Q 5. How do you manage bleeding complications during polypectomy?
Bleeding complications during polypectomy can range from minor oozing to significant hemorrhage. Management depends on the severity of bleeding:
- Minor bleeding: Often managed with direct epinephrine injection (with or without a hemostatic clip) and close observation. The patient may be monitored for a short period before discharge.
- Moderate bleeding: May require argon plasma coagulation (APC), bipolar electrocoagulation, or the use of hemostatic clips. Patients usually require observation in a post-procedure unit.
- Severe bleeding: This is a rare but serious complication requiring immediate intervention. Techniques include injection of epinephrine with additional hemostasis methods or, in extreme cases, surgical intervention may be necessary. Patients require close monitoring in an inpatient setting, sometimes in the ICU.
Prophylactic measures such as using appropriate resection techniques, meticulous hemostasis, and careful post-procedure monitoring are crucial to minimize bleeding complications.
Q 6. Describe your approach to managing perforation during colonoscopy.
Colonoscopic perforation is a serious complication that requires immediate management. The approach depends on the location and extent of the perforation:
- Small, contained perforation: May be managed conservatively with bowel rest, intravenous fluids, antibiotics, and close monitoring. Repeat colonoscopy may be necessary to assess healing.
- Large perforation or free air in the abdomen: Requires urgent surgical intervention. This may involve primary repair, resection, and anastomosis, or possibly a colostomy depending on the severity and location of the perforation.
Early recognition is vital. Signs and symptoms may include sudden, severe abdominal pain, fever, tachycardia, and hemodynamic instability. Immediate consultation with a surgeon is crucial in suspected perforation cases.
Q 7. What are the risk factors for colonoscopic perforation?
Several factors increase the risk of colonoscopic perforation during polypectomy:
- Size and location of the polyp: Large polyps, particularly those located in areas with thin colonic walls (e.g., cecum), are associated with increased risk.
- Type of polypectomy technique: EMR and ESD carry a higher perforation risk compared to simple snare polypectomy.
- Patient-related factors: Conditions like IBD, prior abdominal surgery, and advanced age increase susceptibility to perforation.
- Operator experience: Inexperienced endoscopists have higher perforation rates; therefore, ongoing education and training are critical.
- Use of aggressive energy settings: Improper use of electrocautery can lead to perforation.
Minimizing these risk factors through careful patient selection, employing appropriate techniques, and maintaining high-quality endoscopy skills are crucial for reducing perforation rates.
Q 8. How do you assess the completeness of polypectomy?
Assessing the completeness of a polypectomy is crucial to prevent recurrence and ensure patient safety. It’s not simply about removing the polyp; it’s about ensuring complete resection of the polyp’s base and stalk. We assess completeness using several methods.
- Visual Inspection: During the procedure, careful observation of the resection site is paramount. A completely resected polyp will leave a flat, smooth base with no visible remnants or overhanging tissue. Any visible residual polyp tissue is a sign of incomplete resection.
- Endoscopic Imaging: High-definition endoscopes and chromoendoscopy (using dyes to highlight abnormal tissue) can help identify subtle residual polyps that may be missed with standard white light.
- Pathology Report: The final confirmation comes from the pathology report. The pathologist examines the resected specimen and provides a description of the polyp’s features, including its size, type, and importantly, whether the resection margins are clear (meaning no polyp tissue remains at the edges of the removed specimen). A finding of ‘clear margins’ signifies complete resection.
For example, imagine removing a pedunculated polyp (one attached by a stalk). Complete resection means removing the entire polyp, including its stalk, leaving a clean, flat area. If a portion of the stalk remains, it could regrow, requiring a repeat procedure.
Q 9. Explain the importance of polyp pathology reports.
The polyp pathology report is the cornerstone of post-polypectomy management. It provides critical information guiding subsequent treatment and surveillance. The report details several key aspects:
- Polyp Histology: This identifies the type of polyp (e.g., adenoma, hyperplastic, inflammatory). Adenomas, particularly those with high-grade dysplasia (precancerous changes), carry a significantly higher risk of developing into colorectal cancer.
- Size and Morphology: The report describes the polyp’s size, shape, and microscopic structure, which can influence risk assessment and future surveillance.
- Resection Margins: As mentioned previously, this is essential to determine the completeness of the polypectomy. ‘Clear margins’ are ideal, while ‘involved margins’ indicate incomplete removal and necessitate further intervention.
- Grading and Staging: For cancerous or precancerous polyps, the report provides a grading and staging based on the extent of abnormal cells and invasion. This informs prognosis and the need for additional treatment (e.g., surgery, chemotherapy).
Imagine a patient with a large, villous adenoma with high-grade dysplasia. The pathology report might indicate the need for colonoscopic surveillance at shorter intervals, or even a surgical resection to reduce the risk of cancer development. This information allows for personalized, proactive management tailored to individual risk profiles.
Q 10. What are the key differences between cold snare and hot snare polypectomy?
Both cold snare and hot snare polypectomy are used to remove polyps, but they differ significantly in their mechanism and applications:
- Cold Snare Polypectomy: Uses a loop of wire to encircle the polyp and then applies a mechanical cutting force to remove it. It is generally preferred for smaller, pedunculated polyps because it allows for precise dissection and minimizes thermal damage to the surrounding mucosa.
- Hot Snare Polypectomy: Uses a heated loop of wire to simultaneously cut and coagulate the polyp’s base. The heat cauterizes blood vessels, reducing bleeding. It’s better suited for larger and flatter polyps but carries a slightly higher risk of perforation.
The choice between cold and hot snare depends on the polyp’s size, morphology, and location. A small, pedunculated polyp might be easily removed with a cold snare, while a larger, sessile polyp often necessitates a hot snare to achieve hemostasis (control of bleeding). Selecting the right technique minimizes complications and optimizes resection.
Q 11. Discuss the role of endoscopic mucosal resection (EMR) in polypectomy.
Endoscopic mucosal resection (EMR) is an advanced technique used for the removal of larger and flatter polyps, particularly those that are too large or sessile (flat and broad-based) for standard snare polypectomy. It involves injecting a solution underneath the polyp to elevate it and then resecting it en bloc (in one piece) using a specialized instrument.
EMR offers several advantages: it allows for complete resection of larger lesions, minimizes the risk of incomplete removal, and provides better specimen quality for pathological evaluation. EMR is typically performed in stages to minimize the risk of complications such as perforation or bleeding.
For instance, a large, flat adenoma that is unsuitable for hot snare polypectomy would be an ideal candidate for EMR. The stepwise resection helps mitigate the risks associated with removing such a large area of mucosa at once.
Q 12. How do you manage large or sessile polyps?
Managing large or sessile polyps requires a strategic approach and often involves advanced endoscopic techniques. Simple snare polypectomy is typically inadequate. Here’s a common approach:
- Assessment: Thorough evaluation of the polyp’s size, location, and surrounding anatomy is crucial to determine the best course of action.
- Piecemeal Resection (if appropriate): If the polyp is too large for en bloc resection, piecemeal resection may be necessary using EMR or snare techniques. This involves removing the polyp in sections, ensuring all sections are retrieved for pathology.
- EMR or ESD: Endoscopic submucosal dissection (ESD) is another advanced technique that can be utilized for larger, flat lesions. It involves dissecting the polyp from the underlying submucosa layer with greater precision, minimizing the risk of incomplete removal. This is often done for very large or high risk polyps.
- Surgical Resection: In some cases, particularly for very large or deeply invasive lesions, surgical resection (colectomy) may be necessary to ensure complete removal and minimize the risk of recurrence or metastasis.
The decision of which approach to use depends on a number of factors, including the polyp’s size, location, and the endoscopist’s expertise. Safety and complete removal are always the top priorities.
Q 13. Describe your experience with advanced polypectomy techniques (e.g., EMR, ESD).
I have extensive experience performing both EMR and ESD, having successfully completed numerous procedures on patients with a wide range of polyp sizes and morphologies. My expertise lies in careful pre-procedural planning, meticulous technique during the procedure, and thorough post-procedural assessment. I’m proficient in using advanced imaging modalities, including chromoendoscopy and narrow-band imaging (NBI), to improve visualization and identify subtle mucosal abnormalities. My experience includes managing complications effectively, such as bleeding and perforation, should they arise. I regularly participate in continuing medical education to stay abreast of the latest advancements and best practices in these advanced polypectomy techniques.
For instance, I recently utilized ESD to successfully remove a large, laterally spreading tumor, achieving en bloc resection with clear margins. The patient recovered well with no complications. This highlights the importance of choosing the most appropriate technique to achieve optimal outcomes.
Q 14. What are the appropriate pre- and post-procedure instructions for patients undergoing colonoscopy with polypectomy?
Pre- and post-procedure instructions are crucial for patient safety and a successful outcome. Clear communication is key.
Pre-Procedure Instructions:
- Bowel Preparation: Patients need to follow a strict bowel preparation regimen to ensure the colon is thoroughly cleansed, allowing for optimal visualization during the procedure. This usually involves a clear liquid diet and laxative medications.
- Medications: Patients need to inform their physician about all medications they are taking, as some may need to be adjusted or temporarily discontinued.
- Anesthesia: Patients should be aware of the type of anesthesia used (conscious sedation is common) and any potential side effects.
- Transportation: Because conscious sedation is frequently utilized, they must arrange for a responsible adult to drive them home.
Post-Procedure Instructions:
- Diet: A gradual return to a regular diet is recommended, starting with clear liquids and progressing as tolerated.
- Activity: Light activity is usually encouraged, while strenuous activity should be avoided for a few days.
- Medication: Patients may be prescribed pain relievers or antibiotics, depending on their needs.
- Follow-up: A follow-up appointment is scheduled to discuss the pathology report and plan further management.
- Monitoring for Complications: Patients are educated on potential complications (bleeding, perforation) and instructed to seek immediate medical attention if they experience concerning symptoms such as severe abdominal pain, rectal bleeding, or fever.
Providing clear, concise, and personalized instructions to patients ensures they are well-prepared and able to actively participate in their care.
Q 15. How do you handle a difficult or unexpected situation during a colonoscopy?
Handling unexpected situations during a colonoscopy requires quick thinking, adaptability, and a strong foundation in advanced endoscopic techniques. For instance, encountering a large sessile polyp that’s difficult to remove completely might necessitate piecemeal resection, using techniques like snare polypectomy combined with argon plasma coagulation (APC) to minimize bleeding and ensure complete removal. Another scenario could involve perforation. If a perforation is suspected, immediate assessment is crucial – this includes checking for signs of pneumoperitoneum (air in the abdomen) and instantly stopping the procedure. Then, I’d immediately consult with a surgeon, potentially requiring an emergency laparotomy depending on the severity. In cases of uncontrollable bleeding, epinephrine injection at the base of the polyp and the use of hemostatic clips or bipolar coagulation could be vital, followed by close monitoring of vital signs and potential blood transfusion. The key is to prioritize patient safety, and if unsure, to consult senior colleagues for immediate support.
Ultimately, experience plays a significant role in managing such scenarios. Regular training, simulations, and participation in case reviews help develop the necessary decision-making skills and build confidence in navigating these challenges.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Explain your approach to informed consent for colonoscopy with polypectomy.
Informed consent for colonoscopy with polypectomy is a crucial ethical and legal aspect of the procedure. My approach involves a detailed, patient-centered discussion that covers all relevant aspects. This starts with explaining the procedure itself in straightforward language, avoiding medical jargon. I’ll illustrate with analogies to make it easier to understand; for example, I compare the colonoscope to a long, flexible camera that allows visualization of the colon’s lining. I carefully explain the reasons for the procedure, emphasizing the potential benefits, such as early detection and prevention of colorectal cancer. I then thoroughly discuss potential risks, including bleeding, perforation, and infection, explaining the likelihood of each and the measures taken to minimize them. The possibility of needing further procedures, like surgery, is also transparently addressed. I’ll answer all the patient’s questions patiently and encourage them to voice any concerns they have. Finally, I ensure the patient understands their right to refuse the procedure and that their consent is voluntary. The process is meticulously documented, with the patient signing a consent form after fully comprehending the information.
Q 17. What are the common complications associated with colonoscopy with polypectomy, and how do you manage them?
Complications from colonoscopy with polypectomy are relatively rare but can be serious. Common complications include bleeding, perforation, and infection. Post-polypectomy bleeding can range from minor oozing requiring observation to significant hemorrhage needing intervention like endoscopic hemostasis (e.g., clipping, coagulation), angiographic embolization, or even surgery. Perforation is a more serious complication; its management depends on the location and size of the perforation, ranging from conservative management with bowel rest and intravenous antibiotics to surgical repair. Infections are less frequent and typically treated with antibiotics. Other less common complications include adverse reactions to sedation, delayed bleeding, and retained polyp fragments, requiring close follow-up and, if necessary, further intervention. Proper pre-procedural patient selection, careful technique during polypectomy, meticulous hemostasis, and post-procedure monitoring significantly minimize the risk of complications.
Q 18. What is your experience with different types of endoscopic equipment used in polypectomy?
My experience encompasses a wide range of endoscopic equipment used in polypectomy, including various types of endoscopes (standard colonoscopes, narrow-band imaging [NBI] endoscopes, and chromoendoscopy endoscopes), snares (hot snares, cold snares), and energy sources (monopolar, bipolar electrocautery, argon plasma coagulation [APC]). The choice of equipment depends on factors such as the polyp’s size, location, morphology, and the endoscopist’s preference and expertise. For example, small, pedunculated polyps are easily removed with a hot snare, while large, sessile polyps may necessitate piecemeal resection using a combination of snare polypectomy and APC to minimize the risk of perforation and achieve complete resection. Experience with different technologies allows for a tailored approach optimizing safety and efficacy for each patient.
Q 19. How do you differentiate between benign and malignant polyps during colonoscopy?
Differentiating between benign and malignant polyps during colonoscopy relies on several factors. Visual characteristics such as size, shape, and color play a role, as do the findings of advanced imaging techniques like chromoendoscopy and NBI. For instance, large (>1cm), sessile polyps with irregular borders and villous features are considered high-risk for malignancy. However, visual assessment alone is not sufficient for definitive diagnosis. Biopsy is essential for any polyp suspicious for malignancy, or any polyp larger than a certain size (usually defined by guidelines). Histopathological examination of the biopsy tissue is crucial for determining the nature of the polyp and for guiding subsequent management.
Q 20. What is your understanding of the adenoma-carcinoma sequence?
The adenoma-carcinoma sequence is a widely accepted model explaining colorectal carcinogenesis. It posits that most colorectal cancers arise from precancerous adenomatous polyps. The progression involves a series of genetic and epigenetic changes that transform normal colonic mucosa into an adenoma, which can then progress to carcinoma over time. This stepwise progression highlights the importance of early detection and removal of adenomas through colonoscopy to interrupt this sequence and prevent colorectal cancer. Understanding this sequence informs our screening recommendations and treatment strategies.
Q 21. How do you document your findings and procedures during a colonoscopy with polypectomy?
Documentation of findings and procedures during colonoscopy with polypectomy is meticulous and comprehensive, employing a standardized reporting system. This includes detailed description of the bowel preparation, the extent of colonoscopy achieved, the number and characteristics of any polyps found (size, location, morphology), and the technique used for polypectomy. The pathology report, indicating the histologic type and features of the removed polyp(s), is an integral part of the documentation. Any complications encountered are also carefully documented, along with the management strategy employed. Detailed documentation is crucial for patient care, quality assurance, and research purposes, ensuring accurate medical records and facilitating seamless communication among healthcare professionals.
Q 22. What is your familiarity with different bowel preparation methods?
Bowel preparation is crucial for a successful colonoscopy, ensuring optimal visualization of the colon. I’m familiar with a range of methods, each with its pros and cons. These include split-dose polyethylene glycol (PEG)-based preparations, which are commonly used and generally well-tolerated. They involve taking a large volume of liquid over several hours, usually divided into two doses. Another approach uses sodium phosphate solutions, which are more concentrated and require a smaller volume, but can sometimes cause nausea or vomiting. More recently, low-volume polyethylene glycol solutions have gained popularity, aiming to improve patient compliance by reducing the amount of liquid needed. Finally, I also have experience with bowel preparation using bisacodyl, a stimulant laxative, often used in conjunction with PEG preparations.
- PEG-based preparations: These are generally well-tolerated and effective, but can be cumbersome due to the large volume of liquid required.
- Sodium phosphate solutions: These are effective but can have more side effects.
- Low-volume PEG solutions: Aim to improve patient compliance, but may not be as effective for all patients.
- Bisacodyl: Often used as an adjunct to other bowel preparations.
The choice of preparation depends on several factors including patient comorbidities, such as renal or cardiac function, and individual preferences. I always discuss the options with each patient to tailor the preparation to their specific needs and ensure the best possible outcome.
Q 23. Describe your experience with sedation and monitoring during colonoscopy.
Sedation is a key component of a comfortable and safe colonoscopy. I am proficient in administering and monitoring various levels of sedation, from moderate sedation with propofol or midazolam to deeper sedation under the supervision of an anesthesiologist. My experience encompasses the use of different monitoring techniques including pulse oximetry, electrocardiography (ECG), and blood pressure monitoring to ensure patient safety and well-being throughout the procedure. I always assess the patient’s medical history before administering sedation to determine the appropriate level and type of sedation required. During the procedure, I meticulously monitor the patient’s vital signs and level of consciousness, adjusting the sedation as needed to maintain patient comfort and safety while ensuring optimal procedural conditions. Post-procedure, I closely monitor patients until they have fully recovered from sedation, before discharging them with appropriate aftercare instructions.
Q 24. What are the quality indicators you monitor for colonoscopy with polypectomy?
Quality indicators for colonoscopy with polypectomy are critical to ensuring both patient safety and the effectiveness of the procedure. I meticulously monitor several key metrics. Adherence to bowel preparation guidelines is paramount; inadequate preparation compromises visualization. Cessation rate of polypectomy is tracked; this measures the number of polyps completely removed. Complete adenoma detection rate (ADR) is a crucial indicator of our ability to identify precancerous lesions. A high ADR means more polyps are detected, thereby reducing colorectal cancer risk. Post-polypectomy bleeding rate is a key safety indicator. Finally, I monitor perforation rate, an extremely serious complication that must be minimized. Regular review and analysis of these indicators enable continuous quality improvement and refinement of our techniques.
Q 25. How do you ensure patient safety during the procedure?
Patient safety is my top priority. This starts with a thorough pre-procedure assessment, including a detailed review of medical history and medication list to identify any potential risks. Careful selection of sedation type and level, along with continuous monitoring during the procedure, is essential. Strict adherence to sterile techniques during polypectomy minimizes the risk of infection. Appropriate post-procedure monitoring ensures a safe recovery. Furthermore, clear and concise communication with the patient and their family is vital, ensuring they understand the procedure and any potential risks and complications. We utilize standardized protocols and checklists to maintain consistent quality and safety across all procedures.
Q 26. What is your approach to patient education before and after the procedure?
Patient education is crucial for a positive experience. Before the procedure, I explain the procedure in detail, emphasizing the importance of bowel preparation and what to expect during and after the procedure. I address their questions and concerns to alleviate anxiety. This includes a detailed description of the sedation process and what they will experience. Post-procedure, I provide clear instructions about diet, activity levels, and signs to watch out for (e.g., bleeding, abdominal pain). I emphasize the importance of follow-up appointments to review the pathology reports and discuss any necessary next steps. I offer written materials and contact information for additional support and reassurance. I believe that well-informed patients are more likely to cooperate fully, contributing to a successful procedure and a smoother recovery.
Q 27. Describe a challenging case you encountered during a colonoscopy with polypectomy, and explain how you handled it.
One particularly challenging case involved a patient with severe diverticulitis and multiple large, sessile polyps in a difficult-to-access area of the sigmoid colon. The inflamed colon made navigation and polyp removal extremely difficult. Initial attempts at snare polypectomy were hampered by the fragile nature of the colonic mucosa. To address this, I carefully adjusted the technique, using lower energy levels during cautery and meticulously dissecting the polyps to minimize trauma to the surrounding tissue. After careful consideration, I also opted for piecemeal polypectomy to ensure the safest removal. Post-procedure, I closely monitored the patient for any signs of bleeding or perforation. Fortunately, the patient recovered well, and pathological examination confirmed the complete removal of all polyps. This case highlighted the importance of adapting techniques to individual patient needs and the value of careful post-procedure monitoring.
Q 28. What are the latest advancements in colonoscopy and polypectomy techniques?
Recent advancements in colonoscopy and polypectomy include the use of high-definition (HD) endoscopes, which provide significantly improved visualization, especially for smaller polyps. Narrow-band imaging (NBI) enhances the detection of subtle vascular patterns in polyps, facilitating more accurate diagnosis and removal. Chromoscopies, using dyes to enhance polyp visibility, also contribute. Advanced polypectomy techniques, such as endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD), are increasingly used for larger or more complex polyps, allowing for en bloc resection and minimizing the need for surgery. The development of artificial intelligence (AI) algorithms for polyp detection and characterization is promising and holds the potential to significantly improve the accuracy and efficiency of colonoscopy.
Key Topics to Learn for Colonoscopy with Polypectomy Interview
- Patient Preparation and Bowel Cleansing: Understanding different bowel preparation regimens, their effectiveness, and potential complications.
- Colonoscopy Technique: Mastering the procedural steps, including insertion, navigation, and withdrawal techniques. Emphasis on safe and efficient polyp identification and removal.
- Polypectomy Techniques: Detailed knowledge of different polypectomy methods (snare, hot biopsy forceps), indications for each, and potential risks and complications.
- Polyp Pathology and Histology: Understanding different types of polyps (adenomas, hyperplastic, etc.), their significance, and the importance of proper specimen handling for accurate pathology.
- Complications and Management: Proficiency in recognizing and managing potential complications such as perforation, bleeding, and adverse reactions to sedation.
- Post-Procedure Care: Understanding the necessary instructions and follow-up care for patients after colonoscopy with polypectomy.
- Advanced Polypectomy Techniques: Familiarity with advanced techniques like endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD) – if applicable to your experience level.
- Sedation and Anesthesia: Understanding the different types of sedation used, monitoring techniques, and potential complications.
- Quality Assurance and Improvement: Knowledge of quality indicators and best practices for colonoscopy and polypectomy procedures.
- Ethical Considerations and Informed Consent: Understanding the importance of patient autonomy and obtaining informed consent.
Next Steps
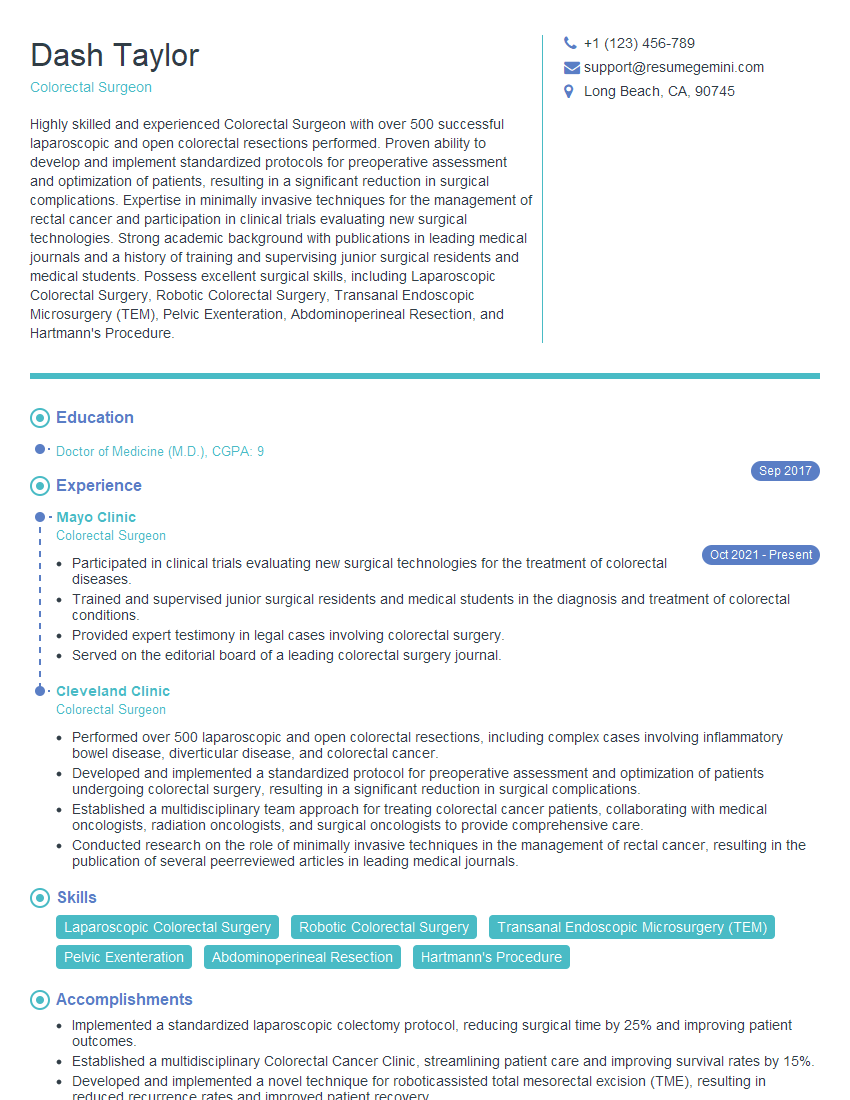
Mastering Colonoscopy with Polypectomy demonstrates advanced procedural skills and clinical judgment, significantly enhancing your career prospects in gastroenterology and related fields. To maximize your job search success, creating a strong, ATS-friendly resume is crucial. ResumeGemini is a trusted resource to help you build a professional resume that highlights your skills and experience effectively. Examples of resumes tailored to Colonoscopy with Polypectomy are available to guide you in showcasing your expertise.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
To the interviewgemini.com Webmaster.
Very helpful and content specific questions to help prepare me for my interview!
Thank you
To the interviewgemini.com Webmaster.
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.