Unlock your full potential by mastering the most common Victimology and Trauma Assessment interview questions. This blog offers a deep dive into the critical topics, ensuring you’re not only prepared to answer but to excel. With these insights, you’ll approach your interview with clarity and confidence.
Questions Asked in Victimology and Trauma Assessment Interview
Q 1. Define victimology and its key principles.
Victimology is the scientific study of victims of crime and the processes involved in victimization. It explores the characteristics of victims, the impact of victimization, and the responses of society to victimization. Key principles include understanding that victimization is a complex event shaped by various factors, including the offender’s actions, the victim’s vulnerabilities, and societal responses. It emphasizes the importance of considering the victim’s perspective and experiences, acknowledging the diverse impacts of crime, and promoting victim empowerment and support. It also rejects victim-blaming and recognizes the role of social and systemic factors in creating vulnerability to crime. For example, victimology might study the prevalence of domestic violence within specific communities, considering factors like socioeconomic status and cultural norms, rather than focusing solely on individual victim behavior.
Q 2. Explain the various types of trauma and their impact on victims.
Trauma encompasses a wide range of experiences that overwhelm an individual’s ability to cope. Types include:
- Acute trauma: A single, overwhelming event like a car accident or a violent assault.
- Chronic trauma: Repeated or prolonged exposure to adversity, such as child abuse or domestic violence.
- Complex trauma: Exposure to multiple traumatic events, often within a relationship (e.g., childhood abuse and neglect). This type frequently involves betrayal and a disruption of attachment.
- Intergenerational trauma: The transmission of trauma across generations. For example, the effects of historical trauma like genocide can manifest in subsequent generations.
Impacts vary greatly depending on the type, severity, and individual’s resilience. Common impacts include Post-Traumatic Stress Disorder (PTSD), anxiety, depression, substance abuse, difficulty in relationships, physical health problems, and emotional dysregulation. For example, a survivor of a car accident (acute trauma) might experience flashbacks and nightmares, whereas a survivor of childhood abuse (chronic trauma) may struggle with trust issues and difficulty forming intimate relationships.
Q 3. Describe different trauma assessment methods and their limitations.
Trauma assessment employs various methods to understand the impact of trauma on an individual. These include:
- Clinical interviews: Structured or semi-structured interviews to gather information about traumatic experiences, symptoms, and coping mechanisms.
- Self-report questionnaires: Standardized measures like the PTSD Checklist (PCL) or the Trauma Symptom Checklist (TSC) to assess symptom severity.
- Observational assessments: Observing the individual’s behavior and emotional regulation during the assessment process.
Limitations exist in each method. Self-report measures rely on the individual’s self-awareness and honesty, which may be affected by trauma-related symptoms such as memory difficulties or denial. Clinical interviews can be subjective and influenced by the interviewer’s biases. Observational assessments provide limited information regarding the individual’s inner experience. Furthermore, cultural factors and language barriers can also affect the accuracy and reliability of assessment results.
Q 4. How do you conduct a trauma-informed interview?
A trauma-informed interview prioritizes the survivor’s safety, empowerment, and control. Key components include:
- Building rapport: Creating a safe and trustworthy environment through empathy and validation.
- Starting with the individual’s strengths and coping mechanisms: Shifting the focus from deficits to resources.
- Respecting the survivor’s pace and comfort level: Avoiding pressure and allowing the individual to set the pace of the interview.
- Collaborating with the survivor to define the focus and goals of the interview: Ensuring that the survivor feels heard and in control.
- Using trauma-sensitive language: Avoiding judgmental or triggering language.
- Providing clear and concise explanations of the process: Ensuring that the survivor fully understands the purpose and procedures of the interview.
- Making referrals as needed to appropriate resources: Connecting the survivor with support services.
For example, instead of directly asking about details of a traumatic event, the interviewer might start by asking about the individual’s current support system, positive coping skills, and what kind of help they are seeking.
Q 5. What are the ethical considerations in working with trauma survivors?
Ethical considerations are paramount when working with trauma survivors. These include:
- Confidentiality: Protecting the survivor’s privacy and ensuring that information is not disclosed without their consent.
- Informed consent: Obtaining the survivor’s voluntary agreement to participate in the assessment and treatment process.
- Avoiding retraumatization: Being mindful of language and actions that might trigger further trauma.
- Recognizing power dynamics: Acknowledging the inherent power imbalance between the professional and the survivor and working to mitigate this imbalance.
- Cultural sensitivity: Respecting the survivor’s cultural beliefs and practices.
- Self-care: Practitioners must engage in self-care practices to prevent vicarious trauma and burnout.
A breach of confidentiality, for instance, can severely damage trust and impede the healing process. Similarly, using insensitive language during an interview can cause retraumatization.
Q 6. Explain the concept of secondary trauma and how to mitigate it.
Secondary trauma, also known as vicarious trauma, refers to the emotional distress that helpers experience when they are exposed to the trauma of others. It can manifest as anxiety, depression, intrusive thoughts, sleep disturbances, and feelings of hopelessness. Mitigating secondary trauma requires a proactive approach focusing on self-care strategies such as:
- Supervision: Regular consultation with a supervisor or mentor to discuss cases and process emotional responses.
- Peer support: Connecting with colleagues who understand the challenges of working with trauma survivors.
- Self-reflection: Regularly reflecting on one’s emotional state and identifying signs of vicarious trauma.
- Maintaining healthy boundaries: Establishing clear boundaries between professional and personal life.
- Engaging in self-care activities: Participating in activities that promote well-being, such as exercise, mindfulness practices, or spending time in nature.
For example, a therapist regularly working with child abuse survivors might experience feelings of anger, sadness, and helplessness. Regular supervision and peer support would allow for processing these emotions in a safe and constructive manner.
Q 7. How do you identify and address the needs of diverse trauma survivors?
Trauma impacts diverse populations differently. Identifying and addressing the needs of diverse survivors necessitates understanding the intersection of trauma with other aspects of their identities such as race, ethnicity, gender, sexual orientation, socioeconomic status, and immigration status. This involves:
- Culturally competent care: Understanding the cultural context of trauma and adapting assessment and intervention methods accordingly. This includes utilizing interpreters when necessary and considering the cultural nuances of disclosure and help-seeking behaviours.
- Addressing systemic inequalities: Acknowledging the ways in which systemic oppression can increase vulnerability to trauma and perpetuate its effects. For example, a survivor from a marginalized community may have experienced additional trauma from systemic discrimination.
- Providing trauma-informed services that are accessible and equitable: Ensuring that services are accessible to all survivors, regardless of their background or resources. This includes considering accessibility issues such as language, location, and financial constraints.
- Building trust and rapport with diverse communities: Establishing relationships with community leaders and organizations to build trust and facilitate access to services.
For instance, working with a refugee survivor might require a deep understanding of their experience with war, displacement, and resettlement, and the particular challenges these pose to their healing journey.
Q 8. What are the signs and symptoms of PTSD and other trauma-related disorders?
Post-traumatic stress disorder (PTSD) and other trauma-related disorders manifest in a wide range of signs and symptoms, both psychologically and physically. These can vary greatly depending on the individual, the nature of the trauma, and other factors like pre-existing mental health conditions.
Psychological Symptoms: These often include intrusive memories (flashbacks), nightmares, avoidance of trauma-related stimuli (people, places, things), negative alterations in mood and cognition (e.g., persistent fear, guilt, detachment), and alterations in arousal and reactivity (e.g., hypervigilance, irritability, difficulty sleeping). For example, a veteran with PTSD might experience flashbacks to combat, have nightmares about the experience, avoid watching war movies, and be easily startled.
Physical Symptoms: Physical manifestations can include chronic pain, headaches, gastrointestinal issues, fatigue, and sleep disturbances. These physical symptoms often accompany the psychological ones and can significantly impact daily life. For instance, someone who experienced a serious car accident might suffer from persistent headaches, stomach problems, and insomnia alongside the psychological trauma response.
Other Trauma-Related Disorders: Beyond PTSD, other disorders like acute stress disorder (ASD) – a shorter-term reaction to trauma – and adjustment disorders can also appear. These share overlapping symptoms but differ in duration and intensity. Accurate diagnosis requires a thorough assessment by a mental health professional.
Q 9. Describe the stages of grief and trauma recovery.
The stages of grief and trauma recovery aren’t always linear, and individuals may experience them differently and at varying paces. There isn’t one universally accepted model, but several frameworks help us understand the process. One common model uses these stages:
- Shock and Denial: An initial period of numbness and disbelief. It’s the brain’s attempt to cope with overwhelming information.
- Anger and Bargaining: As reality sets in, anger, resentment, and frustration may emerge, along with attempts to bargain with fate (e.g., “If only I had…” ).
- Depression and Despair: A profound sense of sadness, loss, and hopelessness may follow. This stage involves processing the full impact of the trauma.
- Acceptance and Integration: Gradually, a sense of acceptance emerges, along with the capacity to integrate the experience into one’s life narrative. This doesn’t mean forgetting, but rather finding a way to live with the trauma’s impact.
Important Note: These are simply stages, not rigid boxes. Individuals may cycle through them, skip stages entirely, or experience them in a different order. The recovery journey is unique to each person, and professional support plays a vital role in navigating it.
Q 10. How do you collaborate with other professionals (e.g., law enforcement, medical personnel) in trauma cases?
Collaboration is crucial in trauma cases. My role as a victimologist and trauma assessor involves coordinating with various professionals to ensure holistic support for survivors.
With Law Enforcement: I offer expertise on victim behaviors, trauma responses, and the impact of the crime on the victim. This collaboration can help in gathering accurate information, conducting sensitive interviews, and tailoring investigative approaches. I might, for example, explain why a victim’s delayed reporting of a sexual assault isn’t uncommon due to the trauma’s impact.
With Medical Personnel: I help bridge the gap between physical and psychological trauma, ensuring that the victim’s medical needs are addressed alongside their emotional and psychological well-being. For example, I might communicate with a doctor regarding the impact of chronic pain on a survivor’s mental state.
With other professionals: This includes social workers, therapists, legal advocates and other relevant parties. I work to create a coordinated, supportive environment which addresses the victim’s immediate and long-term needs. This might involve attending case conferences, facilitating referrals, or providing information about available resources.
Q 11. Explain the difference between acute stress disorder and PTSD.
Both acute stress disorder (ASD) and post-traumatic stress disorder (PTSD) are trauma-related disorders, but they differ mainly in duration and timing of symptoms.
Acute Stress Disorder (ASD): ASD develops within one month of a traumatic event and lasts for at least three days but less than one month. Symptoms are similar to PTSD, including intrusive memories, avoidance, negative alterations in mood, and alterations in arousal and reactivity. However, in ASD, the intensity and duration of these symptoms are more limited compared to PTSD.
Post-Traumatic Stress Disorder (PTSD): PTSD develops after experiencing or witnessing a traumatic event (e.g., war, abuse, natural disasters), and it’s characterized by persistent symptoms lasting longer than one month. The symptoms are more enduring and potentially debilitating than those in ASD.
Essentially, ASD is considered a short-term response to trauma, and if symptoms persist beyond one month, a diagnosis of PTSD is generally considered.
Q 12. How do you assess the risk of re-victimization?
Assessing the risk of re-victimization involves a comprehensive approach that considers various factors.
Risk Factors: These include the nature of the initial trauma (e.g., intimate partner violence carries a high risk of recurrence), the victim’s current living situation (e.g., unstable housing or lack of social support), and pre-existing vulnerabilities (e.g., history of abuse, substance use). Certain personality traits might also contribute to vulnerability.
Assessment Tools: While no single tool perfectly predicts re-victimization, several structured assessments exist that can help evaluate a victim’s risk level. These might involve questionnaires, interviews, and reviews of available information.
Practical Application: In my work, I use these assessments to inform recommendations for safety planning and support services. This may include advice about securing housing, developing crisis plans, obtaining legal protection orders, and connecting the victim with relevant support networks. The goal is to empower the victim and create a safer environment.
Q 13. What are evidence-based trauma treatment approaches?
Several evidence-based trauma treatment approaches have proven effective in helping individuals heal from trauma. These are often tailored to the individual’s specific needs and experiences.
- Trauma-Focused Cognitive Behavioral Therapy (TF-CBT): This approach addresses trauma-related thoughts, feelings, and behaviors through a combination of cognitive restructuring, exposure therapy, and relaxation techniques. It’s particularly effective for children and adolescents who have experienced abuse or trauma.
- Prolonged Exposure (PE): This involves repeatedly confronting trauma-related memories and situations in a safe and controlled environment, gradually reducing avoidance and fear responses. It’s highly effective for PTSD.
- Eye Movement Desensitization and Reprocessing (EMDR): This therapy utilizes bilateral stimulation (e.g., eye movements) while processing traumatic memories, helping to reduce the intensity of emotional responses.
- Narrative Exposure Therapy (NET): This approach focuses on helping individuals reconstruct their traumatic experiences into a coherent narrative, reducing the intrusive and disruptive nature of the memories. It’s often used in cases involving torture or political violence.
The selection of the most appropriate approach depends on the individual’s specific needs, trauma history, and preferences.
Q 14. Describe your experience with crisis intervention strategies.
Crisis intervention strategies are crucial in providing immediate support to individuals experiencing acute distress following a traumatic event. My approach emphasizes a collaborative and empathetic framework.
Key Principles: I focus on ensuring safety, providing immediate emotional support, stabilizing the individual, and connecting them with necessary resources. This often involves active listening, validation of their feelings, and helping them develop coping mechanisms for the immediate crisis.
Techniques: I utilize techniques like grounding exercises (focusing on the present moment), breathing exercises to manage anxiety, and collaborative problem-solving to help them identify immediate needs and resources. I might help a victim who just experienced a robbery locate a safe place to stay, or connect them with immediate support services.
Long-term Perspective: While crisis intervention focuses on immediate stabilization, it also lays the foundation for longer-term support. I ensure that individuals are linked to appropriate therapists, support groups, or other resources to address their ongoing needs and prevent future crises.
Q 15. Explain your understanding of the impact of trauma on various developmental stages.
Trauma’s impact varies significantly across developmental stages. Young children (0-6 years) may exhibit developmental regression, attachment difficulties, and difficulties with emotional regulation. Their trauma responses might manifest as nightmares, separation anxiety, or changes in eating and sleeping patterns. Middle childhood (6-12 years) often sees trauma expressed through aggressive behavior, social withdrawal, or academic difficulties. Adolescents (13-18 years) might grapple with identity issues, risky behaviors, self-harm, and substance abuse. Adults might experience PTSD, depression, anxiety, relationship problems, and difficulties with work or daily functioning. The specific manifestation depends on the type and severity of trauma, the child’s resilience, and the support system available.
For instance, a preschooler witnessing domestic violence might regress to thumb-sucking or bedwetting, while a teenager experiencing sexual assault might exhibit self-destructive behaviors or develop an eating disorder. Understanding these developmental variations is crucial for tailoring appropriate interventions.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you build rapport and trust with trauma survivors?
Building rapport and trust with trauma survivors requires patience, empathy, and a non-judgmental approach. It’s essential to create a safe and comfortable environment where the survivor feels empowered to share their experiences without fear of criticism or blame. This involves actively listening, validating their feelings, and respecting their pace and boundaries. I start by introducing myself clearly, explaining my role, and outlining the process. I use simple, straightforward language, avoiding jargon and technical terms. I ensure the survivor feels in control, offering choices whenever possible, such as where they’d like to sit or what they’d like to drink. It’s critical to consistently demonstrate respect for their autonomy and decision-making power.
For example, I might start a session by asking something like, ‘What’s important for you to feel safe and comfortable during this session?’ or ‘How would you like to proceed today?’ This shows that I value their input and agency.
Q 17. How do you handle disclosures of sensitive information?
Handling sensitive disclosures requires a calm, empathetic, and professional approach. First, I validate the survivor’s experience and acknowledge the courage it took to share their story. I assure them that I’m there to listen without judgment. I avoid interrupting or pressuring them to provide more information than they’re comfortable with. My focus is on creating a supportive space where they feel heard and understood. I document the disclosure accurately and objectively, paying close attention to detail but avoiding leading questions. Confidentiality is paramount, and I always explain the limits of confidentiality upfront, such as mandated reporting requirements.
If a disclosure involves child abuse or elder abuse, mandated reporting protocols require immediate intervention. I carefully balance the survivor’s wishes with my legal obligations. It is important to carefully document the entire process, including all conversations and actions taken.
Q 18. What are your strategies for managing your own stress when working with trauma survivors?
Working with trauma survivors can be emotionally taxing. To manage my own stress, I prioritize self-care and utilize various coping mechanisms. This includes regular supervision with a qualified professional to process my experiences and discuss challenging cases. I engage in activities that promote relaxation and well-being, such as exercise, spending time in nature, or practicing mindfulness. Maintaining clear boundaries between my professional and personal life is essential. I also participate in continuing education to enhance my skills and knowledge, ensuring that I’m equipped to handle the emotional demands of the work. Regular reflection on my practice helps me to identify areas where I might need additional support.
Recognizing the signs of burnout and seeking support when needed is crucial. It is not a sign of weakness, but rather a sign of self-awareness and professional responsibility.
Q 19. Describe your experience with conducting forensic interviews.
My experience with forensic interviews involves utilizing a structured, developmentally appropriate approach. The goal is to obtain factual information from children and vulnerable adults who have experienced trauma, in a way that minimizes stress and ensures accurate and reliable testimony. I use techniques such as open-ended questions, avoiding leading questions that could influence their responses. I validate the child’s experience while maintaining objectivity. The interview is carefully planned and conducted in a neutral, child-friendly environment. I use techniques to build rapport, making sure the child feels safe and comfortable. Detailed notes and recordings are maintained throughout the process, documenting every aspect of the interview.
For example, instead of asking ‘Did the man touch you inappropriately?’, I might ask ‘Can you tell me what happened?’ This allows the child to describe the events in their own words.
Q 20. How do you differentiate between fact and opinion in victim statements?
Differentiating between fact and opinion in victim statements is crucial for accurate assessment and legal proceedings. Facts are objective statements that can be verified or proven. Opinions are subjective beliefs or interpretations. I accomplish this by carefully analyzing the language used in statements, distinguishing between descriptive statements that recount events and inferential statements which offer explanations or interpretations. I look for evidence of bias, emotional language, or speculation. I corroborate information whenever possible with other sources of evidence. The context of the statement, the victim’s mental state, and any potential biases are carefully considered.
For example, a statement like ‘He hit me’ is a fact, while ‘He was angry at me’ is an opinion, although it might be based on observed behavior. My training focuses on identifying such nuances to ensure accuracy.
Q 21. What are the legal and ethical considerations surrounding informed consent in trauma assessments?
Informed consent in trauma assessments is governed by ethical and legal principles, emphasizing the victim’s autonomy and right to self-determination. It’s imperative to provide clear and understandable information about the assessment process, its purpose, potential benefits and risks, and the limits of confidentiality. This includes explaining the potential uses of the information gathered, who will have access to it, and how it will be protected. The victim must be fully capable of understanding and voluntarily agreeing to participate. Documentation of the informed consent process is crucial, and it should be age- and competency-appropriate.
If a victim is a minor or has diminished capacity, consent must be obtained from their legal guardian, and their best interests should always be paramount. Failure to obtain proper informed consent can have significant legal and ethical ramifications, potentially invalidating the assessment and leading to legal challenges.
Q 22. How do you ensure cultural sensitivity in your assessment and treatment practices?
Cultural sensitivity is paramount in trauma assessment and treatment. It’s not simply about being polite; it’s about recognizing that trauma manifests differently across cultures and that individuals’ experiences are shaped by their unique cultural backgrounds, beliefs, and values. I ensure cultural sensitivity by:
- Prioritizing self-reflection: Regularly examining my own biases and assumptions to avoid imposing my worldview on clients.
- Utilizing culturally appropriate assessment tools: Selecting and adapting assessment measures that are valid and reliable within the client’s cultural context. This may involve using interpreters, modifying questions, or selecting instruments specifically designed for particular cultural groups.
- Building rapport through culturally sensitive communication: I actively listen and try to understand the client’s perspective, respecting their communication styles and non-verbal cues. This includes being mindful of eye contact, personal space, and touch, as these vary across cultures.
- Collaborating with cultural experts: Consulting with community leaders, cultural consultants, or other professionals familiar with the client’s cultural background when needed.
- Considering the impact of cultural factors on trauma responses: Understanding how cultural norms and beliefs may influence the expression and experience of trauma. For example, some cultures may encourage emotional restraint, leading to underreporting of symptoms.
For example, working with a client from a collectivist culture might require a different approach than working with someone from an individualistic culture. In a collectivist culture, family involvement may be essential in the treatment process, whereas in an individualistic culture, the focus might be solely on the individual’s needs.
Q 23. What are the limitations of self-report measures in trauma assessment?
Self-report measures, while convenient and widely used in trauma assessment, have inherent limitations. These measures rely on the individual’s ability and willingness to accurately report their experiences, which can be affected by various factors. Some key limitations include:
- Memory biases: Traumatic events can distort memory, leading to incomplete or inaccurate recall. The emotional intensity of the event can affect memory consolidation and retrieval.
- Response bias: Individuals may underreport or exaggerate symptoms due to social desirability, shame, or fear of judgment. They might also struggle to articulate their experiences accurately, particularly complex or emotionally charged ones.
- Cultural influences: The way individuals perceive and express trauma is shaped by their cultural background, which can impact the validity of standardized self-report measures designed for a different cultural context.
- Symptom overlap: Symptoms of PTSD and other trauma-related disorders can overlap with other mental health conditions, making it difficult to accurately attribute symptoms solely to trauma using self-report alone.
- Lack of contextual information: Self-report measures often fail to capture the complexity of the individual’s experience, including pre-trauma functioning, social support systems, and ongoing stressors.
For example, a client might underreport their symptoms due to stigma associated with mental health issues or a lack of understanding of the symptoms themselves. Therefore, relying solely on self-report can lead to an incomplete or inaccurate picture of the individual’s trauma experience.
Q 24. Explain the role of collateral information in trauma assessment.
Collateral information plays a crucial role in supplementing self-report data and enhancing the accuracy of trauma assessment. It involves gathering information from sources other than the individual, such as family members, friends, medical records, or school records. This can provide valuable context and corroborate or challenge the individual’s self-report.
- Validation of self-reported information: Collateral information can confirm the occurrence of a traumatic event and its impact on the individual’s life.
- Identifying discrepancies: Discrepancies between self-report and collateral information can highlight areas requiring further exploration, such as potential memory distortions or intentional misrepresentation.
- Providing a broader perspective: Collateral sources offer insights into the individual’s pre-trauma functioning, coping mechanisms, and social support systems, which are critical for understanding the impact of trauma.
- Observing behavioral changes: Collateral informants can report changes in the individual’s behavior, mood, or functioning that might not be apparent during a clinical interview.
- Understanding the context of the trauma: Collateral information can provide a richer understanding of the circumstances surrounding the trauma, the individual’s response to the event, and the ongoing impact on their life.
For instance, information from a spouse or parent about a client’s changes in sleep, appetite, or social interaction can greatly complement the client’s self-report and paint a more comprehensive clinical picture.
Q 25. How do you assess the reliability and validity of trauma-related information?
Assessing the reliability and validity of trauma-related information is a critical aspect of trauma assessment. Reliability refers to the consistency of the information, while validity refers to its accuracy. I employ several strategies:
- Multiple sources of information: Triangulating information from different sources (self-report, collateral interviews, medical records) increases the reliability and validity of the findings.
- Consistent reporting across interviews: Comparing information from multiple interviews with the individual helps to determine the consistency of their accounts.
- Considering the informant’s reliability: Evaluating the credibility and potential biases of informants is essential. Are they objective, or might their own experiences or relationships with the individual influence their reporting?
- Using validated assessment tools: Employing standardized, psychometrically sound assessment measures increases the validity of the assessment.
- Clinical judgment: Integrating the gathered information within a clinical framework, considering the individual’s overall presentation, developmental history, and other relevant factors. This relies on experience and professional expertise.
For example, if a client reports a specific traumatic event, and this is corroborated by medical records and statements from family members, the reliability and validity of the information are strengthened. However, if the client’s account changes significantly across multiple interviews, or if collateral information contradicts the self-report, further investigation is needed.
Q 26. Describe your experience working with specific trauma populations (e.g., children, veterans).
My experience encompasses working with diverse trauma populations, including children and veterans. Each population presents unique challenges and requires tailored assessment and treatment approaches.
- Children: Assessing trauma in children requires specialized techniques, as their cognitive and expressive abilities may limit their capacity for self-reporting. I rely heavily on play therapy, observation, and collateral information from parents, teachers, and caregivers. The use of age-appropriate assessment tools and adapting interview techniques to the child’s developmental level is crucial. For example, drawings or dolls can be utilized to help children express their experiences.
- Veterans: Working with veterans often involves understanding the specific types of trauma they’ve experienced (combat exposure, deployment-related stress, etc.) and how those experiences impact their lives. The assessment must consider the impact of military culture, potential co-occurring conditions like substance use disorders, and the challenges of reintegrating into civilian life. Collaboration with other professionals familiar with military culture and veterans’ specific needs is often essential.
Understanding the unique developmental considerations of children and the specific contexts of veteran trauma allows for a more nuanced and effective assessment and treatment approach. Each client’s individual needs are carefully considered and tailored to provide the best possible support.
Q 27. How do you utilize different theoretical frameworks to guide your assessment and treatment plans?
I integrate several theoretical frameworks to guide my assessment and treatment planning. This is not a matter of choosing one ‘best’ theory, but rather of using a flexible and integrative approach that suits each client’s needs and the complexities of their experience.
- Attachment theory: This informs my understanding of the client’s relationships and attachment patterns, particularly how past relational experiences may impact their response to trauma.
- Trauma-focused cognitive behavioral therapy (TF-CBT): This is a key treatment modality for many trauma-related disorders, emphasizing cognitive restructuring, exposure therapy, and coping skills training.
- Trauma-informed care: This overarching framework guides all aspects of my work, focusing on safety, trustworthiness, choice, collaboration, and empowerment.
- Psychodynamic theory: This perspective helps to understand the unconscious processes and defense mechanisms that may be involved in the client’s response to trauma.
- Narrative therapy: This approach allows clients to actively reconstruct their narratives, empowering them to gain a sense of agency and self-determination.
For instance, with a client struggling with PTSD after a car accident, I might integrate TF-CBT to help them process the trauma and develop coping skills, while using aspects of attachment theory to understand the impact of the event on their relationships. The choice of framework is always determined by the unique aspects of the client’s needs and clinical presentation.
Q 28. Explain your understanding of the biopsychosocial model in trauma recovery.
The biopsychosocial model recognizes that trauma and its recovery are not solely psychological phenomena. It emphasizes the interconnectedness of biological, psychological, and social factors in shaping an individual’s experience of trauma and their path towards healing.
- Biological factors: These include genetics, neurobiology (the impact of trauma on the brain), and physiological responses to stress (e.g., hormonal changes). For instance, genetic predispositions to anxiety can influence an individual’s response to trauma.
- Psychological factors: This encompasses thoughts, feelings, beliefs, and coping mechanisms. The individual’s personality, pre-existing mental health conditions, and their cognitive appraisal of the traumatic event all play a significant role.
- Social factors: These include social support networks, cultural context, and environmental stressors. A strong social support system can significantly enhance recovery, while social isolation or ongoing adversity can hinder it.
Understanding these interconnected factors is essential for effective trauma recovery. For example, a treatment plan for a client might involve addressing biological factors through medication management, psychological factors through trauma-focused therapy, and social factors by connecting them with support groups or community resources. A holistic approach that considers all these factors increases the chances of successful recovery.
Key Topics to Learn for Your Victimology and Trauma Assessment Interview
Preparing for an interview in Victimology and Trauma Assessment requires a comprehensive understanding of both the theoretical frameworks and practical applications. This section highlights key areas to focus your studies.
- Understanding Trauma: Explore different types of trauma (acute, chronic, complex), their impact on individuals, and the various theoretical models used to explain trauma’s effects (e.g., attachment theory, social learning theory).
- Victimology Principles: Develop a strong grasp of victimology theories, including risk factors, vulnerability, and the impact of victimization on individuals and communities. Consider the role of social support and resilience.
- Assessment Methods: Familiarize yourself with various assessment tools and techniques used in evaluating trauma and its impact. This includes understanding the ethical considerations and limitations of different methodologies.
- Clinical Interventions: Gain insight into evidence-based interventions and therapeutic approaches used in working with trauma survivors. Focus on the practical application of these methods and their effectiveness.
- Cultural Competence: Understand the influence of cultural background and social context on trauma experiences and responses. Develop awareness of culturally sensitive assessment and intervention strategies.
- Ethical Considerations: Master the ethical principles and guidelines related to working with trauma survivors, including confidentiality, informed consent, and appropriate boundaries.
- Case Study Analysis: Practice analyzing case studies involving trauma and victimization. Focus on identifying key issues, developing effective assessment plans, and outlining appropriate interventions.
Next Steps: Maximize Your Job Prospects
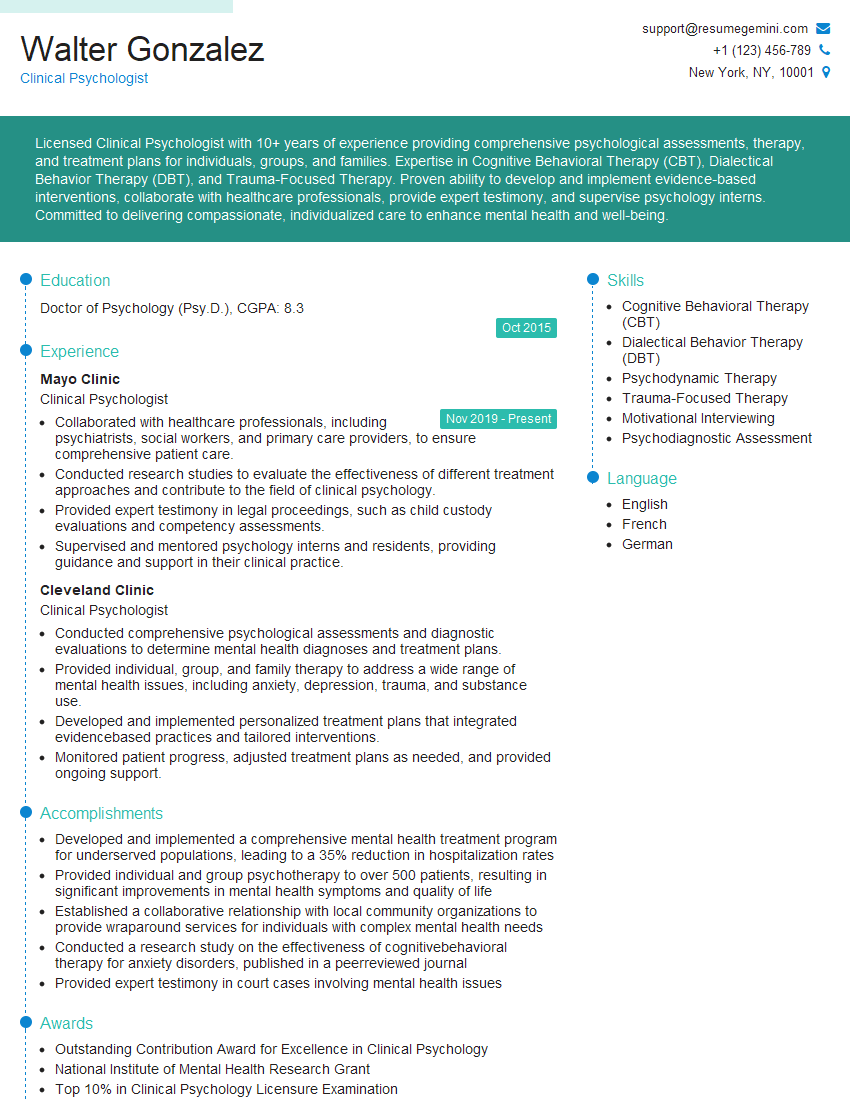
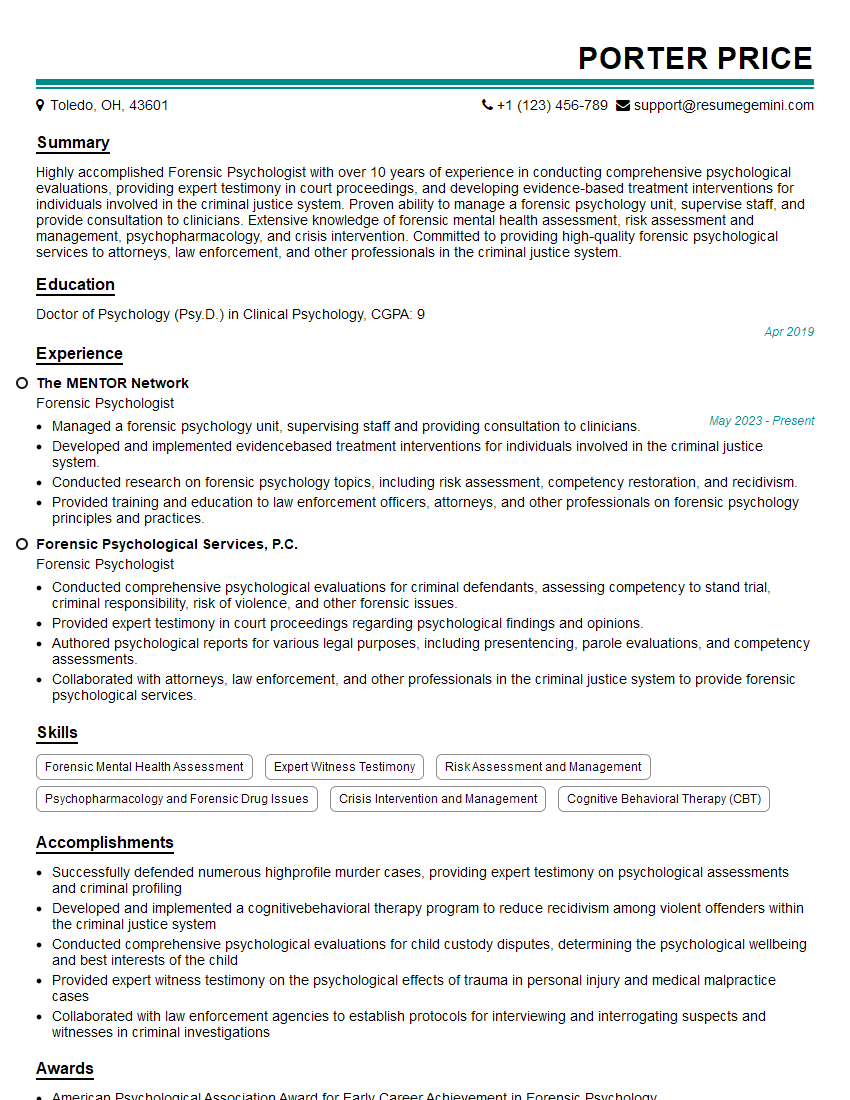
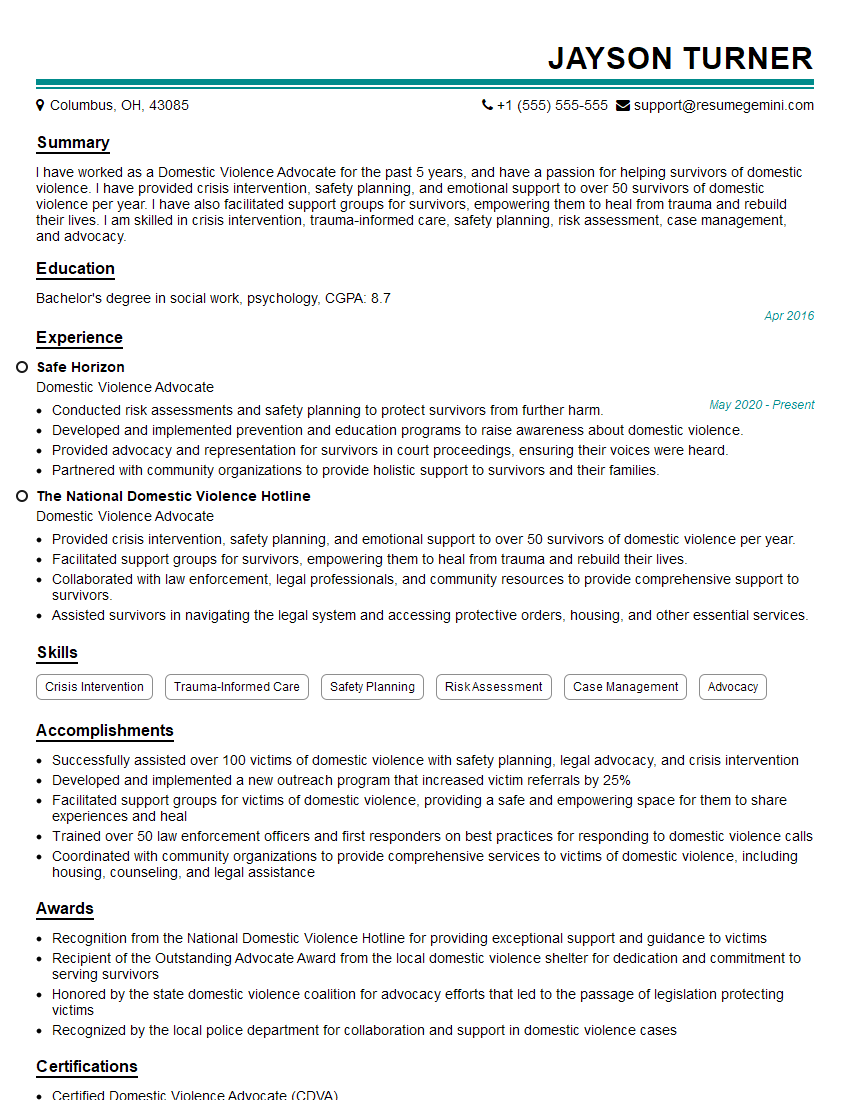
Mastering Victimology and Trauma Assessment opens doors to rewarding careers with significant impact. To stand out, a strong, ATS-friendly resume is crucial. It showcases your skills and experience effectively to potential employers. ResumeGemini is a trusted resource to help you build a professional and impactful resume tailored to this field. We provide examples of resumes specifically crafted for Victimology and Trauma Assessment roles to help guide you. Invest the time in crafting a compelling resume—it’s a key step in advancing your career.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.