Feeling uncertain about what to expect in your upcoming interview? We’ve got you covered! This blog highlights the most important Interventional Spine Procedures interview questions and provides actionable advice to help you stand out as the ideal candidate. Let’s pave the way for your success.
Questions Asked in Interventional Spine Procedures Interview
Q 1. Describe your experience with kyphoplasty and vertebroplasty procedures.
Kyphoplasty and vertebroplasty are minimally invasive procedures used to treat vertebral compression fractures, often caused by osteoporosis. Both involve injecting bone cement (polymethylmethacrylate or PMMA) into a fractured vertebra to stabilize it and relieve pain. The key difference lies in the technique: Vertebroplasty involves injecting cement directly into the fractured bone, while kyphoplasty uses a balloon to create a cavity within the vertebra before cement injection. This cavity creation in kyphoplasty helps restore some vertebral height, potentially improving posture and reducing kyphosis (spinal curvature).
In my experience, I’ve performed numerous kyphoplasty and vertebroplasty procedures, carefully selecting the appropriate technique based on the patient’s specific fracture characteristics, including the degree of compression and bone quality. For example, a patient with significant vertebral collapse and kyphosis might be a better candidate for kyphoplasty, as the balloon helps to restore vertebral body height. Conversely, a patient with a smaller, less significantly compressed fracture might be a good candidate for the less invasive vertebroplasty. Post-operative pain management is crucial in both procedures, and I typically prescribe analgesics and closely monitor patients for potential complications like cement leakage.
Q 2. Explain the indications and contraindications for spinal cord stimulation.
Spinal cord stimulation (SCS) is a therapy that delivers electrical impulses to the spinal cord, thereby interrupting pain signals traveling to the brain. It’s primarily indicated for patients with chronic neuropathic pain that hasn’t responded to other treatments, such as failed back surgery syndrome (FBSS), complex regional pain syndrome (CRPS), and peripheral neuropathy.
- Indications: Chronic neuropathic pain, failed back surgery syndrome (FBSS), complex regional pain syndrome (CRPS), peripheral neuropathy, angina pectoris.
- Contraindications: Active infection, bleeding disorders, severe obesity hindering lead placement, significant psychological issues that might interfere with therapy compliance, and certain implanted electronic devices that could be affected by the stimulation.
The decision to use SCS involves a thorough evaluation of the patient’s pain history, neurological examination, and imaging studies. A trial period with temporary SCS leads is often conducted to assess the effectiveness of the therapy before permanent implantation. It is essential to manage patient expectations, as SCS isn’t a cure for pain but rather a management tool for reducing pain intensity and improving quality of life.
Q 3. Discuss the different types of spinal injections and their applications.
Several types of spinal injections are used to diagnose and treat various spinal conditions. These include:
- Epidural steroid injections (ESIs): Injected into the epidural space to reduce inflammation and pain around nerve roots. They are often used for radiculopathy (nerve root pain) caused by conditions such as spinal stenosis or disc herniation.
- Facet joint injections: Targeted at the facet joints, which are small joints in the spine that can become inflamed and painful. These injections help diagnose and treat facet joint pain.
- Selective nerve root blocks: Used to identify the specific nerve root causing pain. A local anesthetic is injected around a nerve root to temporarily block its function. If pain relief occurs, it confirms the nerve root’s involvement in the pain generation.
- Medial branch blocks: These injections target the medial branches of the spinal nerves that innervate the facet joints. They are helpful in diagnosing and treating facet joint pain.
The choice of injection type depends on the patient’s specific diagnosis, pain location, and response to prior treatments. For instance, a patient with radicular pain radiating down the leg might benefit from an ESI, whereas a patient with localized back pain stemming from a facet joint might benefit from a facet joint injection.
Q 4. How do you select the appropriate needle size and approach for a given procedure?
Needle size and approach selection for spinal procedures are critical for safety and effectiveness. The ideal needle size and approach are determined by several factors:
- Target anatomy: The size and depth of the target structure dictate the needle length and gauge (diameter). For instance, a smaller gauge needle might be used for a facet joint injection, while a larger gauge needle might be needed for a more challenging procedure such as a kyphoplasty.
- Patient factors: Body habitus (size and build), skin condition, and presence of pre-existing conditions influence needle selection and approach. A patient with a deep target area might require a longer needle.
- Procedural type: Different procedures require different needles. For example, a small-gauge needle is preferred for diagnostic injections, while a larger gauge needle might be used for cement injection in kyphoplasty.
- Fluoroscopic guidance: Real-time fluoroscopic imaging allows for precise needle placement, enabling the use of smaller-gauge needles to minimize trauma and complications.
Choosing the appropriate approach (e.g., anterior, posterior, transforaminal) also depends on the target anatomy and patient factors. A detailed anatomical understanding and careful planning, often aided by preoperative imaging studies, are crucial. An example of this planning would be using a lateral approach to access the facet joint, or a posterior approach for epidural injection. Every step is carefully considered to optimize the procedure’s outcome and minimize risks.
Q 5. What are the potential complications of epidural steroid injections?
Epidural steroid injections (ESIs), while generally safe and effective, carry potential complications:
- Infection: Though rare, infection at the injection site or a more serious epidural abscess is possible.
- Bleeding: Patients with bleeding disorders or those on anticoagulants are at higher risk of bleeding at the injection site or into the epidural space.
- Nerve damage: Accidental damage to a nerve root during the injection can lead to temporary or permanent neurological deficits.
- Headache: Dural puncture (accidental puncture of the dura mater) during an ESI can cause a post-dural puncture headache.
- Increased pain: Though uncommon, some patients may experience increased pain after the injection.
Minimizing these risks involves careful patient selection, strict sterile technique, use of image guidance (fluoroscopy), and a thorough understanding of anatomy. Pre-procedural discussions with the patient covering potential complications, alternative treatments, and informed consent are crucial.
Q 6. How do you manage post-procedural pain and complications?
Post-procedural pain and complication management is critical for a successful outcome. My approach involves a multimodal approach that includes:
- Pain medication: Analgesics, such as NSAIDs or opioids, are prescribed based on the patient’s pain level and tolerance.
- Ice and compression: Applied to the injection site to reduce swelling and inflammation.
- Rest and activity modification: Patients are advised to rest appropriately and gradually resume activities as tolerated.
- Physical therapy: Rehabilitation programs can help improve strength, range of motion, and overall function.
- Monitoring for complications: Close follow-up appointments are scheduled to monitor for any signs or symptoms of complications, such as infection or neurological deficits.
Early recognition and management of potential complications are key to preventing serious adverse events. For example, if a patient develops signs of infection, such as fever or increased pain and redness at the injection site, prompt treatment with antibiotics is initiated.
Q 7. Describe your experience with fluoroscopy guidance in interventional spine procedures.
Fluoroscopy guidance is essential in virtually all interventional spine procedures. It provides real-time X-ray imaging, allowing for precise needle placement and visualization of anatomical structures. This significantly reduces the risk of complications by enabling the practitioner to see exactly where the needle is going and to avoid critical structures like nerves and blood vessels.
My experience with fluoroscopy guidance is extensive. I utilize fluoroscopy routinely to guide needle placement in procedures such as ESIs, facet joint injections, medial branch blocks, and vertebroplasty/kyphoplasty. The ability to obtain multiple views (AP, lateral, oblique) enhances accuracy. For instance, in performing a transforaminal ESI, fluoroscopy is essential to confirm needle placement within the appropriate foramen and avoid inadvertent intrathecal or intravascular injection. In kyphoplasty, fluoroscopy is critical in guiding the precise placement of the balloon and cement to ensure optimal vertebral body reconstruction and minimize the risk of cement leakage. Fluoroscopy use is a cornerstone of safe and effective interventional spine procedures, and proficiency in its use is paramount for practitioners in this field.
Q 8. How do you assess patient candidacy for interventional spine procedures?
Assessing candidacy for interventional spine procedures is a multi-step process requiring a thorough evaluation of the patient’s medical history, physical examination findings, and imaging studies. We begin by carefully reviewing the patient’s symptoms, including the location, nature, duration, and intensity of their pain. We also explore the impact of the pain on their daily activities and quality of life. A comprehensive physical exam helps pinpoint the source of pain and assess neurological function, range of motion, and muscle strength. This is crucial in differentiating between various pain generators (e.g., nerve root, facet joint, disc). Imaging, such as X-rays, MRI, and CT scans, are essential in visualizing the spine’s anatomy and identifying any structural abnormalities like disc herniations, spinal stenosis, or fractures that might be contributing to the pain.
Furthermore, we consider the patient’s overall health, including any comorbidities like diabetes, heart disease, or bleeding disorders that could increase the risk of complications during the procedure. Finally, we discuss the patient’s expectations and preferences, ensuring they understand the risks, benefits, and alternatives to interventional procedures. Only after a thorough evaluation and informed consent do we determine if a patient is a suitable candidate for a specific interventional spine procedure.
Q 9. What are the imaging techniques used to guide interventional spine procedures?
Imaging plays a vital role in guiding interventional spine procedures, ensuring accuracy and safety. Fluoroscopy is the most commonly used technique. It provides real-time X-ray images, allowing the physician to visualize the needle’s trajectory as it’s advanced towards the target area within the spine. This dynamic imaging is crucial for navigating through complex anatomy and avoiding damage to vital structures such as nerves and blood vessels.
Computed tomography (CT) scans offer high-resolution anatomical detail and can be integrated with fluoroscopy (CT-fluoroscopy) for more precise targeting, particularly in complex cases. Magnetic resonance imaging (MRI) provides excellent soft tissue contrast and is valuable in pre-procedural planning to identify the precise location of pathology, such as a disc herniation or nerve compression. Sometimes, a combination of these imaging modalities is utilized to achieve optimal procedural planning and execution.
Q 10. Explain your understanding of the anatomy relevant to interventional spine procedures.
A deep understanding of spinal anatomy is paramount for successful interventional spine procedures. This includes a detailed knowledge of the vertebral column, its various segments (cervical, thoracic, lumbar, sacral), and the intricate relationships between bones, ligaments, muscles, nerves, and blood vessels. We must know the precise location and course of nerve roots, their branches, and the spinal cord itself to avoid inadvertent injury during procedures. Furthermore, a thorough understanding of the intervertebral discs, facet joints, and other structures within the spine is crucial for targeting specific areas for treatment.
For instance, in performing an epidural steroid injection, we need to precisely locate the epidural space, which lies outside the dura mater, to deliver medication effectively and safely to alleviate nerve root inflammation. Similarly, in procedures targeting facet joints, a precise knowledge of their anatomy is paramount to accurately deliver medication or perform radiofrequency ablation. A strong grasp of this complex anatomy is fundamental to minimizing risks and maximizing the effectiveness of these interventions.
Q 11. Describe your experience with discography and its interpretation.
Discography is a diagnostic procedure involving the injection of contrast material into the nucleus pulposus of an intervertebral disc. It’s primarily used to assess the internal structure and integrity of the disc and to identify if disc pathology is a source of the patient’s pain. During the procedure, fluoroscopy is used to guide the needle precisely into the disc. The contrast material allows visualization of the disc’s internal architecture, identifying any tears, fissures, or internal disruption.
Interpretation of discography involves careful assessment of the contrast spread within the disc. A normal disc typically shows uniform contrast filling. Abnormal findings, such as irregular contrast spread, extravasation (leakage) of contrast outside the disc, or pain reproduction during the injection, suggest disc pathology. However, interpretation needs careful consideration of the patient’s clinical presentation and other imaging findings. Discography results should be interpreted in conjunction with the patient’s history, physical exam, and other imaging studies (MRI, CT) to avoid false positives or negatives. It’s important to remember that discography can be painful and is therefore used selectively.
Q 12. How do you differentiate between different types of spinal pain?
Differentiating between various types of spinal pain requires a systematic approach. We start by obtaining a detailed patient history, paying close attention to the location, character (sharp, dull, aching), radiation (does the pain spread), and aggravating and relieving factors. The physical examination is crucial in identifying neurological deficits, such as muscle weakness, sensory changes, or reflex abnormalities, which can help pinpoint the source of the pain.
For example, radicular pain, caused by nerve root compression, typically radiates down the limb along the dermatomal distribution of the affected nerve root. Facet joint pain, often characterized by localized back pain, might be aggravated by specific movements or postures. Spinal stenosis, which involves narrowing of the spinal canal, can cause pain, numbness, and weakness in the legs, especially with prolonged standing or walking. Imaging studies like X-rays, MRI, and CT scans are indispensable in visualizing spinal structures and identifying the underlying cause of the pain. By integrating the patient’s history, physical exam, and imaging findings, we can effectively differentiate between various types of spinal pain and guide treatment strategies.
Q 13. What are the risks and benefits of different interventional spine procedures?
Interventional spine procedures, while offering significant benefits in pain relief, also carry potential risks. The specific risks and benefits vary depending on the procedure. For instance, epidural steroid injections, commonly used to treat radiculopathy, carry a low risk of infection, bleeding, nerve damage, or allergic reaction. However, the benefits can include significant reduction in pain and improved function.
Procedures like facet joint injections or radiofrequency ablation carry similar risks albeit at varying rates, with the potential for temporary or rarely permanent nerve damage. Benefits include reduced pain in specific areas. More invasive procedures, such as vertebroplasty or kyphoplasty used for vertebral compression fractures, carry a higher risk of complications, including cement leakage, nerve injury, or infection. Benefits include pain relief and improved stability. Each procedure’s risks and benefits are carefully weighed against the patient’s clinical presentation, expectations, and overall health before proceeding. A detailed discussion with the patient ensures they are fully informed and can make an informed decision.
Q 14. How do you assess the success of an interventional spine procedure?
Assessing the success of an interventional spine procedure involves a multi-faceted approach combining objective and subjective measures. Subjectively, we rely heavily on the patient’s self-reported pain levels using validated pain scales (e.g., visual analog scale, numerical rating scale). We also assess improvements in their functional status, such as their ability to perform daily activities, return to work, or participate in recreational activities.
Objectively, we might use measures such as range of motion, muscle strength, and neurological examinations to monitor improvements. Imaging studies, though not always necessary, can be used in some cases to assess changes in spinal structures or inflammation. A successful procedure is one that leads to a clinically significant reduction in pain, improvement in function, and an enhanced quality of life for the patient. Follow-up appointments are crucial in monitoring the long-term outcomes and addressing any potential complications. The success of a procedure is not solely determined by immediate post-procedural pain relief but also by the sustained improvement in the patient’s overall condition over time.
Q 15. Explain your understanding of different types of spinal implants and their application.
Spinal implants are crucial in interventional spine procedures, providing structural support and stability to the spine. The choice of implant depends heavily on the specific pathology and the patient’s individual anatomy. They range from simple to complex designs.
- Interbody fusion cages: These are placed between vertebrae to promote bone fusion, often used in cases of disc degeneration or spondylolisthesis. Think of them as scaffolding that encourages the bones to grow together. Different materials exist, including titanium, PEEK (polyetheretherketone), and carbon fiber, each with unique properties regarding biocompatibility and strength.
- Pedicle screws: These screws are inserted into the pedicles (strong bony projections on the vertebrae) to provide fixation for spinal instrumentation. They are often used in conjunction with rods to create a stable construct, correcting deformities like scoliosis or stabilizing fracture sites. Precise placement is crucial to avoid nerve root injury.
- Vertebral body tethers: These minimally invasive implants are designed to provide support and reduce motion in damaged vertebral bodies, often used in osteoporotic vertebral compression fractures. They are smaller and less invasive than traditional instrumentation.
- Facet joint screws and plates: These are used to stabilize the facet joints, which are the joints between the vertebrae. They are particularly useful in cases of facet joint arthritis or instability.
- Bone graft substitutes: These materials are used to fill bone voids and promote fusion. They can be composed of various materials including bone morphogenetic proteins (BMPs) or synthetic bone graft substitutes.
Selecting the appropriate implant requires careful consideration of the patient’s age, bone quality, the level and type of spinal pathology, and surgical approach. For example, a younger patient with strong bones might be a good candidate for pedicle screws and rods, while an older patient with osteoporosis may benefit from vertebral body tethers or minimally invasive approaches.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Describe your experience with nerve root blocks.
Nerve root blocks are a cornerstone of interventional pain management. They involve the injection of an anesthetic and/or steroid medication directly near a compressed or inflamed nerve root to reduce pain and inflammation. I have extensive experience performing various types of nerve root blocks, including selective nerve root blocks, transforaminal epidural steroid injections (TFESI), and caudal epidural injections.
The procedure typically involves fluoroscopic guidance to ensure accurate needle placement, minimizing the risk of complications. Patient selection is critical; a thorough history and physical examination, along with imaging studies (MRI, CT), are essential to identify the specific nerve root involved and to rule out other potential causes of pain. For example, in a case of lumbar radiculopathy, a selective nerve root block can confirm the diagnosis and provide diagnostic and therapeutic relief. Post-procedure, patients are monitored for any adverse effects and provided with appropriate instructions regarding activity levels and potential side effects.
Success rates vary depending on the underlying pathology and patient factors, but nerve root blocks often provide significant pain relief in the short-term, allowing patients to regain functionality and pursue physical therapy. Long term effects are usually monitored through follow up appointments.
Q 17. How do you manage patients with failed back surgery syndrome?
Failed back surgery syndrome (FBSS) presents a complex challenge, requiring a multidisciplinary approach. Patients experiencing FBSS have persistent pain despite previous spinal surgery. Managing these patients necessitates a thorough evaluation to determine the cause of their ongoing symptoms. This evaluation typically involves reviewing the patient’s previous surgical reports, imaging studies (MRI, CT scans), and performing a detailed physical examination.
My approach typically involves a combination of diagnostic and therapeutic interventional techniques. These might include repeat epidural steroid injections, nerve root blocks, or diagnostic injections to pinpoint the source of pain. In some cases, additional surgery might be considered, but this is carefully evaluated considering the patient’s overall health and previous surgical history. If the cause of pain is a non-surgical issue, such as scar tissue adhesion, then procedures such as adhesiolysis may be considered.
Non-interventional management, including physical therapy, medication management (pain medications, antidepressants, anticonvulsants), psychological support, and alternative therapies, plays a significant role in managing FBSS. The goal is to improve the patient’s functional capacity, reduce pain, and improve their quality of life. Each patient requires an individualized plan tailored to their specific circumstances. Open communication and realistic expectations are crucial to success.
Q 18. What is your experience with minimally invasive spine surgery techniques?
Minimally invasive spine surgery (MISS) techniques have revolutionized the field, offering patients reduced trauma, smaller incisions, less blood loss, shorter hospital stays, and faster recovery times compared to open surgery. My experience with MISS techniques is extensive. I routinely utilize various approaches, including:
- Percutaneous procedures: These involve accessing the spine through small incisions under fluoroscopic or image-guided navigation. This includes procedures such as vertebroplasty, kyphoplasty, and minimally invasive discectomies.
- Minimally invasive fusion techniques: These procedures use smaller incisions and specialized instruments to perform spinal fusion, reducing the muscle trauma associated with traditional open surgery. These procedures may involve techniques like tubular retractors or less dissection.
- Lateral lumbar interbody fusion (LLIF): This technique accesses the disc space from the side, preserving the paraspinal muscles.
- Transforaminal lumbar interbody fusion (TLIF): This technique approaches the disc space through the foramen (the opening where the nerve roots exit the spinal canal).
The selection of a specific MISS technique depends heavily on the patient’s anatomy, the specific pathology, and the surgeon’s expertise. Careful preoperative planning, including detailed imaging studies and meticulous surgical technique, are essential to ensure successful outcomes with MISS. I always strive to utilize the least invasive technique that achieves the desired therapeutic goal.
Q 19. How do you counsel patients about the risks and benefits of interventional spine procedures?
Counseling patients about the risks and benefits of interventional spine procedures is a critical aspect of my practice. I believe in fostering open and honest communication. I begin by explaining the patient’s condition in clear, non-technical terms, outlining the diagnosis and the rationale for considering an interventional procedure.
I then thoroughly discuss the potential benefits, such as pain reduction, improved mobility, and improved quality of life. Crucially, I also explain the potential risks, including infection, bleeding, nerve damage, and the possibility that the procedure may not provide the desired relief. I present the information in a balanced way, avoiding undue alarm but ensuring that patients have a complete understanding of what to expect.
I involve patients in shared decision-making, actively listening to their concerns and answering their questions. I often use analogies and visual aids to help them grasp complex medical concepts. For example, I might compare the injection of a steroid to targeted medication delivery for inflammation. I encourage them to ask questions and to express any hesitations they may have. The goal is to ensure that they make an informed decision that aligns with their personal values and expectations.
Q 20. Describe your experience with the use of intraoperative neuromonitoring.
Intraoperative neuromonitoring (IONM) is a crucial adjunct in many spine procedures, providing real-time assessment of nerve function during surgery. My experience with IONM is extensive, and I consider it an indispensable tool for improving patient safety and surgical precision. IONM involves the use of electrodes to monitor the electrical activity of nerves during the procedure. This allows me to identify and mitigate any potential injury to the nerves in real-time.
Different modalities of IONM exist, including somatosensory evoked potentials (SSEPs), motor evoked potentials (MEPs), and electromyography (EMG). The specific modalities used depend on the type of surgery being performed. For example, SSEPs might be used during spinal fusion to monitor the function of the sensory pathways. The data are constantly monitored by a trained IONM technician, and any changes in the signals can alert me to potential nerve injury, allowing for immediate corrective action.
IONM enhances precision by providing feedback during critical steps of the surgery. This reduces the risk of neurological complications and improves the safety profile of spine procedures. While not eliminating all risks, it significantly improves the chances of a successful and complication-free outcome.
Q 21. Explain your experience with managing bleeding complications during procedures.
Bleeding complications, while relatively uncommon in interventional spine procedures, can be serious. My experience in managing these complications includes both proactive measures to prevent bleeding and reactive strategies to manage it effectively when it occurs.
Proactive measures include careful patient selection (excluding patients with severe bleeding disorders), meticulous surgical technique to minimize tissue trauma, the judicious use of electrocautery, and the use of appropriate hemostatic agents. I also ensure that the patient’s blood clotting profile is optimized prior to the procedure.
Reactive strategies include the use of surgical techniques to control bleeding, such as pressure, direct coagulation, and the placement of surgical sponges or drains. In rare instances, blood transfusions might be necessary. Knowing the anatomy, promptly identifying bleeding sources, and skillful implementation of haemostatic strategies is crucial. In cases of significant bleeding, the procedure may be interrupted to address the issue before continuing; open communication with the anesthesiologist is critical in such scenarios. Postoperatively, patients are closely monitored for any signs of bleeding or hematoma formation.
Q 22. How do you address patient anxiety and manage pain before, during and after the procedure?
Addressing patient anxiety and managing pain is paramount in interventional spine procedures. We employ a multi-pronged approach starting well before the procedure. This includes a thorough pre-operative consultation where I explain the procedure in detail, answer all questions honestly and patiently, and address any concerns. I often use analogies to simplify complex medical terms, making the process less daunting. For example, explaining vertebroplasty as ‘filling a crack in a bone with special cement’ can be far more reassuring than using technical jargon.
Pain management begins with optimizing medications before the procedure. This might involve adjusting existing pain medications or introducing new ones, always considering the patient’s overall health and potential interactions. During the procedure, we use local anesthetic and sedation techniques tailored to the individual’s needs and tolerance. We monitor vital signs closely and adjust medications as needed to ensure comfort and safety. Post-procedure, a carefully planned pain management regimen is implemented, often combining oral analgesics, nerve blocks, and physical therapy to minimize discomfort and promote healing. Regular follow-up visits allow for adjustments to the pain management plan based on the patient’s progress and feedback.
Q 23. Discuss your experience with different types of spinal stents and their application.
Spinal stents have become increasingly important in managing spinal stenosis and other conditions causing compression of the neural elements. I have extensive experience with various types, including self-expanding metallic stents, balloon-expandable stents, and bioabsorbable stents. The choice depends on factors like the specific anatomy, the severity of stenosis, and patient-specific considerations.
For example, self-expanding metallic stents are excellent for providing immediate and durable expansion in challenging anatomical locations. However, they are permanent implants. Balloon-expandable stents offer precise placement and expansion but may require a slightly longer procedure. Bioabsorbable stents, while offering the advantage of eventual resorption, may not provide the same level of immediate expansion and long-term support as metallic stents. My approach involves carefully assessing each case and selecting the stent type that best addresses the patient’s unique needs and anatomy, ensuring the best possible clinical outcome and minimizing the risk of complications.
Q 24. What are your preferred techniques for managing infections related to spinal procedures?
Infection prevention and management are critical in interventional spine procedures. Our protocol prioritizes meticulous sterile technique throughout the entire process – from pre-operative skin preparation to post-operative wound care. This includes using appropriate antibiotic prophylaxis, adhering to strict aseptic guidelines during the procedure, and maintaining a clean and organized operating room environment.
Should an infection occur despite these precautions, we implement a comprehensive management strategy involving prompt diagnosis (often using imaging and cultures), aggressive antibiotic therapy guided by culture results, and potentially surgical debridement (removal of infected tissue) if necessary. Close monitoring of the patient’s clinical status and laboratory values is crucial to assess the effectiveness of treatment and to adjust the approach as needed. Multidisciplinary collaboration with infectious disease specialists is essential for optimal management of complex cases.
Q 25. How do you use advanced imaging techniques (CT, MRI) to plan and guide procedures?
Advanced imaging plays a pivotal role in planning and guiding interventional spine procedures. Pre-operative CT and MRI scans provide detailed anatomical information, including the precise location and extent of the pathology. We meticulously review these images to identify the target area, assess the surrounding structures, and plan the optimal approach and trajectory for the procedure.
During the procedure, fluoroscopy (real-time X-ray imaging) provides continuous visualization of the instruments and their relationship to the spinal anatomy. This allows for precise placement of devices, minimizing the risk of complications. In complex cases, we may also use intraoperative CT scans to further refine our approach and ensure accurate placement of implants. The integration of these advanced imaging modalities enhances procedural accuracy, reduces complications, and improves patient outcomes.
Q 26. Describe your experience with working in a multidisciplinary team setting.
I believe strongly in the power of a multidisciplinary approach to patient care. In interventional spine, effective teamwork is crucial. I routinely collaborate with neurologists, neurosurgeons, physiatrists, pain management specialists, radiologists, and physical therapists. This collaborative approach ensures that each patient receives a holistic assessment and a personalized treatment plan that addresses all aspects of their condition – not just the spinal pathology.
For instance, in a case of chronic back pain, I might collaborate with a physiatrist to develop a comprehensive rehabilitation program, and a pain management specialist to manage the patient’s pain medication. Regular team meetings ensure open communication and coordinated care, leading to better patient outcomes and a smoother patient experience.
Q 27. How do you stay current with the latest advancements in interventional spine techniques?
Staying current in interventional spine requires a multifaceted approach. I actively participate in professional organizations such as the North American Spine Society (NASS) and the Society for Interventional Radiology (SIR), attending conferences, and participating in continuing medical education courses. I also regularly review peer-reviewed journals and relevant medical literature to stay updated on the latest research findings and advancements in techniques and technologies.
Moreover, I engage in collaborative discussions with colleagues, both locally and nationally, sharing experiences and best practices. This exchange of knowledge and ideas keeps me at the forefront of this rapidly evolving field, allowing me to offer my patients the most effective and up-to-date treatment options.
Q 28. How do you handle difficult or challenging cases in interventional spine?
Handling difficult cases in interventional spine requires a combination of technical expertise, problem-solving skills, and a calm, decisive approach. Challenges might include unusual anatomical variations, pre-existing conditions, or unexpected intraoperative complications.
My strategy involves careful pre-operative planning, which includes thoroughly reviewing imaging studies and considering potential challenges. During the procedure, I remain flexible and adapt my approach based on the actual findings. If an unexpected complication arises, I prioritize patient safety, address the issue systematically, and don’t hesitate to consult with colleagues or modify the procedure as needed. Documentation of the entire process is meticulous, including any challenges encountered and the solutions implemented. This rigorous approach minimizes risks and optimizes outcomes even in the most challenging cases.
Key Topics to Learn for Interventional Spine Procedures Interview
- Anatomy and Physiology of the Spine: Thorough understanding of spinal structures, including vertebrae, discs, ligaments, nerves, and blood vessels. Consider the impact of aging and disease processes.
- Imaging Techniques: Fluoroscopy, CT, MRI – interpretation and application in guiding procedures. Be prepared to discuss the strengths and limitations of each modality.
- Minimally Invasive Spine Surgery Techniques: Detailed knowledge of various procedures, including vertebroplasty, kyphoplasty, discectomy, and nerve root blocks. Focus on indications, contraindications, and potential complications.
- Pain Management Strategies: Understanding of different pain pathways and how interventional procedures alleviate pain. Discuss pharmacological and non-pharmacological adjuncts to pain management.
- Complications and Management: Be prepared to discuss potential complications of each procedure and your approach to recognizing, managing, and preventing them. This includes post-operative care and patient education.
- Patient Selection and Assessment: Discuss criteria for selecting appropriate candidates for various interventional spine procedures. How do you determine if a patient is a suitable candidate? What are your assessment protocols?
- Advanced Techniques and Emerging Technologies: Familiarity with newer technologies and evolving techniques in interventional spine procedures. Demonstrate a commitment to continuous learning and professional development.
- Ethical Considerations and Informed Consent: Understanding of the ethical implications of interventional spine procedures and the importance of obtaining informed consent from patients.
Next Steps
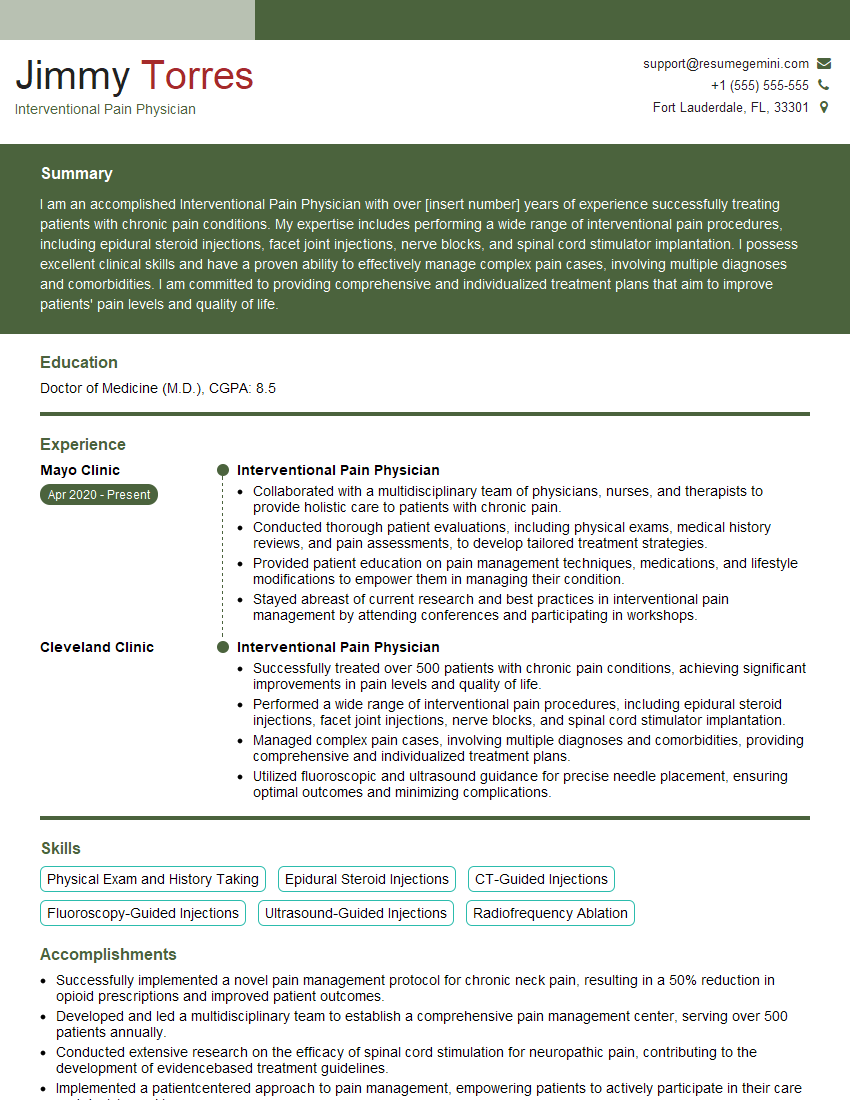
Mastering Interventional Spine Procedures is crucial for career advancement in this rapidly evolving field. A strong understanding of these techniques will significantly enhance your opportunities and allow you to contribute meaningfully to patient care. To maximize your job prospects, it’s essential to create a compelling and ATS-friendly resume that highlights your skills and experience effectively. ResumeGemini is a trusted resource that can help you build a professional resume tailored to the specific requirements of interventional spine procedure positions. Examples of resumes tailored to Interventional Spine Procedures are available to guide you through this process.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.