The thought of an interview can be nerve-wracking, but the right preparation can make all the difference. Explore this comprehensive guide to Case Management and Treatment Planning interview questions and gain the confidence you need to showcase your abilities and secure the role.
Questions Asked in Case Management and Treatment Planning Interview
Q 1. Describe your experience developing and implementing treatment plans.
Developing and implementing treatment plans is a cornerstone of effective case management. It involves a collaborative process, starting with a thorough assessment of the client’s needs and goals, followed by the creation of a personalized plan outlining specific interventions, timelines, and measurable outcomes.
My approach begins with active listening and building rapport. I then use evidence-based practices and models relevant to the client’s specific challenges. For example, with a client struggling with substance abuse, I might incorporate components of Cognitive Behavioral Therapy (CBT) and motivational interviewing. The plan is documented clearly, outlining the frequency and duration of sessions, specific goals (e.g., achieving sobriety, improving coping mechanisms), and methods for monitoring progress. Regular review and modification based on client progress are crucial to ensure the plan remains relevant and effective. I always strive for plans that are client-centered, empowering them to actively participate in the process.
For instance, I worked with a young woman experiencing anxiety and depression. Her initial treatment plan included weekly therapy sessions focusing on CBT techniques, relaxation exercises, and stress management strategies. As she progressed, we modified the plan to incorporate social skills training and gradually reduce the frequency of therapy sessions, ultimately supporting her independent self-management skills.
Q 2. Explain your process for assessing client needs and identifying appropriate resources.
Assessing client needs and identifying appropriate resources is a multi-faceted process requiring both strong clinical judgment and a comprehensive understanding of available community resources. I begin with a thorough biopsychosocial assessment, considering the client’s biological factors (e.g., medical conditions), psychological factors (e.g., mental health diagnoses, coping mechanisms), and social factors (e.g., family dynamics, support systems, housing). This assessment uses various tools, including standardized questionnaires, interviews, and observations.
Based on this assessment, I identify the client’s strengths and vulnerabilities, defining their specific needs. This then guides my search for appropriate resources which could include therapy, medication management, vocational rehabilitation, housing assistance, substance abuse treatment, or support groups. I maintain an updated directory of resources, including contact information and relevant eligibility criteria. Importantly, I involve the client in this process, ensuring that the chosen resources are culturally sensitive and align with their preferences and goals.
For example, a client experiencing homelessness might need housing assistance, along with mental health services and job training. I would connect them with a local shelter, a mental health clinic, and a vocational rehabilitation center, ensuring smooth referrals and collaborative care.
Q 3. How do you prioritize competing demands and manage multiple cases simultaneously?
Managing multiple cases simultaneously requires exceptional organizational skills and time management techniques. I utilize a case management system, often a combination of electronic health records (EHR) and personal organizational tools, to track client progress, appointments, and deadlines. Prioritization is crucial and I use a combination of urgency and importance, addressing immediate crises while ensuring long-term goals are not neglected.
My system relies on several strategies: I regularly review my caseload, prioritizing clients based on their immediate needs and risk levels. Time blocking helps schedule specific time slots for each client and administrative tasks. Regularly reviewing my calendar and to-do list allows me to stay organized and adapt to unexpected events. Effective delegation when appropriate is also valuable.
For instance, a client experiencing a severe mental health crisis would take precedence over other cases that may require less immediate attention. This does not mean neglecting the other cases, merely prioritizing my time and resources effectively. I always strive to maintain clear communication with clients, adjusting my schedule as needed to meet their urgent needs.
Q 4. What is your approach to working with clients who are resistant to treatment?
Working with resistant clients requires patience, empathy, and a collaborative approach. It’s essential to understand the reasons behind their resistance. This may stem from past negative experiences with the healthcare system, mistrust, fear of judgment, or lack of understanding of the benefits of treatment.
My approach is centered on building a strong therapeutic alliance. This begins with actively listening to their concerns and validating their feelings. I avoid judgmental language and focus on building rapport. I might ask open-ended questions to understand their perspective and collaboratively set realistic, achievable goals that align with their values and preferences. I may adjust the treatment plan to accommodate their preferences or pacing. If the resistance is significant, involving family members (with client consent) or referring to another provider might be considered.
For example, a client initially hesitant to engage in therapy might be more receptive when offered a flexible schedule or a different therapeutic approach. Celebrating small victories and consistently highlighting progress reinforces their motivation and engagement.
Q 5. How do you ensure continuity of care during transitions between treatment settings?
Ensuring continuity of care during transitions between treatment settings is vital to prevent disruptions in treatment and to support client progress. This requires strong communication and collaboration with all involved professionals and facilities. Before the transition, I facilitate a comprehensive handover meeting to share relevant information about the client’s background, treatment history, progress, and future treatment needs.
This might involve completing standardized transfer forms, providing detailed written summaries of the client’s care, and participating in multidisciplinary meetings. I often maintain direct contact with the new care providers to ensure a smooth transition and address any arising questions. I also ensure the client is involved in this process, providing them with opportunities to ask questions and express their concerns.
For example, when transferring a client from an inpatient facility to an outpatient program, I ensure their medication regimen is clearly communicated, appointments are scheduled with their new therapist, and the client has access to necessary support systems.
Q 6. Describe a situation where you had to advocate for a client.
I once advocated for a client who was facing eviction due to a lack of affordable housing. She was struggling with mental illness and lacked the resources to secure alternative housing. I contacted several agencies and organizations, including the local housing authority and mental health advocacy groups. I provided them with comprehensive documentation outlining her clinical needs and the potential risks of homelessness.
I attended meetings, communicated regularly with the housing authority, and collaborated with her psychiatrist to document her medical needs and vulnerability. Through these combined efforts, we successfully secured subsidized housing for the client. This experience highlighted the importance of advocacy in providing holistic support and helping vulnerable clients overcome systemic barriers to accessing essential services.
Q 7. Explain your understanding of the different models of case management.
Several models of case management exist, each with its own approach and focus.
- Brokerage Model: This model focuses primarily on connecting clients with available resources. The case manager acts as a facilitator, linking clients to appropriate services and ensuring they navigate the system effectively.
- Case Management Model: This is a more comprehensive approach, involving a deeper assessment of client needs, development of a personalized care plan, and ongoing monitoring of progress. It often involves advocacy and coordination of services from multiple providers.
- Strength-Based Case Management: This model emphasizes client empowerment and focuses on identifying their strengths and resources. The case manager works collaboratively with the client to build on these strengths and develop strategies for achieving their goals.
- Assertive Community Treatment (ACT): This intensive model is designed for clients with severe mental illness who require high levels of support. It typically involves a multidisciplinary team providing services directly in the community.
The choice of model depends on the client’s specific needs and the resources available. In my practice, I often integrate elements from multiple models to create a personalized approach that best meets the client’s unique circumstances.
Q 8. How do you measure the effectiveness of your interventions?
Measuring the effectiveness of interventions in case management requires a multifaceted approach. We can’t simply rely on one metric; instead, we need a combination of quantitative and qualitative data to paint a complete picture.
Quantitative measures often involve tracking changes in pre-defined outcomes. For example, if we’re working with a client struggling with substance abuse, we might track the number of days abstinent, frequency of relapses, or improvements in lab results. For a client with mental health challenges, we might track symptom severity scores using standardized scales like the PHQ-9 for depression or the GAD-7 for anxiety. These objective measures provide concrete evidence of progress.
Qualitative measures are equally important. They provide context and depth to the quantitative data. This could involve regular client feedback sessions, charting observations of the client’s behaviour and mood, and noting changes in their engagement with treatment or daily life. For example, we might observe increased social interaction, improved self-esteem, or a greater sense of self-efficacy. These qualitative insights help understand the ‘why’ behind the numbers.
Finally, it’s vital to regularly review the effectiveness of our interventions. Are the goals still relevant? Are we using the most effective strategies? Regular evaluation allows for adjustments and ensures that we’re providing the best possible care. For instance, if a particular therapy isn’t yielding results, we might need to explore alternative approaches or collaborate with other professionals to develop a more comprehensive strategy.
Q 9. What are some common challenges in case management, and how do you overcome them?
Case management presents unique challenges. One common hurdle is resource scarcity. Finding appropriate housing, securing financial assistance, or accessing specialized services can be difficult, especially for clients with multiple needs. To overcome this, I build strong relationships with community organizations and agencies to create a support network for my clients. This includes proactively seeking out new resources and collaborating with other professionals to ensure my clients receive comprehensive care.
Another challenge is client resistance or lack of engagement. Clients may be hesitant to participate in services or struggle with adherence to treatment plans due to various factors like mistrust, fear of failure, or underlying mental health issues. To address this, I employ a collaborative, person-centered approach. This involves building rapport, active listening, setting realistic goals, and empowering clients to take ownership of their recovery.
Finally, managing the complexities of multiple cases can be overwhelming. Effective time management, prioritization, and organizational skills are crucial. Utilizing case management software and developing clear, well-structured treatment plans are essential in effectively juggling multiple cases while ensuring each client receives the individualized attention they need.
Q 10. Describe your experience utilizing electronic health records (EHRs) in case management.
My experience with EHRs (Electronic Health Records) in case management has been largely positive. EHRs streamline the documentation process, making it easier to maintain accurate and up-to-date records. They also enhance collaboration among team members, as everyone can access the same information in real time.
For example, I use EHRs to securely store client information, track progress towards treatment goals, schedule appointments, and generate reports. The ability to quickly access a client’s history and treatment plan helps me tailor my interventions to their specific needs, providing efficient and personalized care.
However, it’s important to acknowledge the challenges. Maintaining data integrity, ensuring privacy and security, and navigating the complexities of different EHR systems can be time-consuming. Despite these challenges, the advantages of improved efficiency, enhanced collaboration, and data-driven decision-making outweigh the drawbacks.
Q 11. How familiar are you with HIPAA regulations and maintaining client confidentiality?
I am thoroughly familiar with HIPAA regulations (Health Insurance Portability and Accountability Act) and understand the importance of maintaining client confidentiality. This is fundamental to building trust and ensuring ethical practice. HIPAA regulations govern the use and disclosure of protected health information (PHI).
I consistently follow HIPAA guidelines by using secure methods for storing and transmitting client information, only accessing information relevant to my role, and obtaining informed consent before sharing PHI with others. I am also trained on appropriate disposal of sensitive materials and participate in regular compliance training to stay updated on the latest regulations.
Client confidentiality is not just a regulatory requirement; it’s a cornerstone of the therapeutic relationship. Without trust, it’s difficult for clients to feel comfortable sharing the information necessary for effective treatment. Protecting their privacy is paramount to providing quality care.
Q 12. What are your strategies for managing difficult or complex cases?
Managing difficult or complex cases requires a flexible and adaptable approach. It’s often necessary to step back and assess the situation from various perspectives. First, I conduct a thorough assessment, examining the client’s history, current challenges, and support systems.
Then, I develop a comprehensive treatment plan in collaboration with the client, identifying specific, measurable, achievable, relevant, and time-bound (SMART) goals. This includes incorporating evidence-based practices and tailoring interventions to meet the client’s unique needs. If a client is demonstrating significant resistance, I might explore underlying issues contributing to this behaviour, such as trauma or mistrust.
For instance, if a client is struggling with severe substance abuse and co-occurring mental health issues, I might collaborate with psychiatrists, substance abuse counselors, and other relevant professionals to create a comprehensive team. Regular team meetings are crucial for sharing information, coordinating efforts, and adjusting the treatment plan as needed. This approach ensures that the client receives holistic support and increases the likelihood of positive outcomes.
Q 13. How do you collaborate effectively with interdisciplinary teams?
Effective collaboration with interdisciplinary teams is essential for providing comprehensive care. I believe in open communication, active listening, and mutual respect.
To facilitate collaboration, I regularly attend team meetings, actively participate in discussions, and share relevant client information in a timely manner. I utilize electronic communication tools like secure messaging to facilitate rapid exchange of information and coordination of care.
In addition, I proactively seek input from other professionals, valuing their expertise and perspectives. I believe that through collaborative efforts, we can provide comprehensive care that addresses all aspects of the client’s needs. For example, if a client has physical health issues impacting their mental well-being, I would consult with their physician to ensure their treatment plans are coordinated.
Q 14. Explain your understanding of discharge planning and its importance.
Discharge planning is a crucial aspect of case management. It’s the process of preparing a client for a safe and successful transition from one level of care to another, such as from inpatient treatment to outpatient services, or from a hospital to their home.
The goal is to ensure the client has the resources and support they need to maintain their progress and avoid relapse. Discharge planning begins well before the actual discharge date. I work closely with the client, their family (if appropriate), and other members of the treatment team to identify their needs, resources, and potential challenges after leaving a facility or program.
A comprehensive discharge plan might include arranging for housing, securing ongoing mental health or substance abuse treatment, providing transportation assistance, and connecting them with community support services. Effective discharge planning reduces hospital readmissions, improves client outcomes, and contributes to a smooth transition into community life.
Q 15. How do you identify and address potential safety concerns for clients?
Identifying and addressing client safety concerns is paramount in case management. It requires a proactive and holistic approach, beginning with a thorough initial assessment. This assessment should explore various risk factors, including the client’s history of violence, substance use, mental health status, and current living situation.
For example, if a client expresses suicidal ideation, a detailed suicide risk assessment is crucial. This includes evaluating the client’s access to lethal means, the presence of a support system, and the intensity of their suicidal thoughts. Based on this assessment, appropriate interventions can be implemented, such as hospitalization, crisis intervention, or increased monitoring. Similarly, if a client exhibits signs of aggression towards others, a safety plan needs to be developed collaboratively with the client and relevant stakeholders, outlining strategies to de-escalate conflict and prevent harm.
Ongoing monitoring is vital. Regular check-ins, utilizing tools such as risk assessment scales, and communication with collateral contacts (family, friends, or other professionals) enable timely identification of escalating risks. If safety concerns arise, immediate action is necessary, which may involve notifying relevant authorities, adjusting the treatment plan, or providing more intensive support. Transparency and collaboration with the client are key throughout the process.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What is your experience with crisis intervention?
My experience with crisis intervention is extensive. I’ve worked with clients experiencing a wide range of acute crises, including suicidal ideation, psychotic breaks, acute anxiety attacks, and severe substance withdrawal. My approach is grounded in evidence-based practices, emphasizing rapid assessment, de-escalation techniques, and stabilization.
For example, during a client’s acute psychotic episode, my primary focus would be on ensuring their safety and the safety of others. This may involve creating a calm and secure environment, using active listening and validation to reduce anxiety, and coordinating with emergency services if necessary. Once stabilized, the focus shifts to identifying the triggers for the crisis and developing strategies to prevent future episodes. This often involves medication management, therapeutic interventions like Cognitive Behavioral Therapy (CBT), and the development of a comprehensive relapse prevention plan.
I am proficient in various de-escalation techniques, including verbal intervention strategies, mindfulness practices, and crisis communication protocols. My approach is always client-centered, empowering individuals to regain control and develop coping mechanisms. Regular training and supervision help me stay updated on the latest best practices in crisis intervention.
Q 17. Describe your approach to building rapport and trust with clients.
Building rapport and trust is foundational to effective case management. It’s not just about professionalism; it’s about genuine human connection. I begin by actively listening to the client’s story, showing empathy and understanding without judgment. I create a safe and comfortable space where they feel heard and valued.
For instance, I might start a session by asking about their week, their hobbies, or anything that helps me understand their personality and preferences beyond their presenting issue. This approach helps to humanize the interaction and establish a collaborative relationship. I am mindful of my verbal and nonverbal communication, ensuring that my tone, body language, and facial expressions convey respect and genuine care. Honesty and transparency are essential; I always clearly explain the treatment process, my role, and the client’s rights.
Consistency and reliability are also key. Keeping appointments, following up on commitments, and demonstrating accountability build trust over time. I actively seek feedback from clients to ensure I am meeting their needs and adjusting my approach as necessary. This collaborative approach fosters mutual respect and strengthens the therapeutic alliance, creating a foundation for positive change.
Q 18. How do you utilize data and metrics to improve case management services?
Data and metrics are indispensable for enhancing case management services. I regularly track key indicators, such as client engagement rates, treatment outcomes, service utilization, and client satisfaction. This data helps to identify trends, pinpoint areas of strength and weakness, and measure the effectiveness of various interventions.
For example, if I notice a low engagement rate with a specific program, I can investigate the reasons behind this, such as accessibility issues, client preferences, or the program’s content. This analysis guides the development of targeted improvements to increase program participation. Similarly, tracking treatment outcomes helps to determine which interventions are most effective for specific populations or presenting problems, allowing for data-driven decisions about resource allocation and program development.
I utilize data visualization tools to represent complex data in a clear and concise manner, facilitating the identification of patterns and insights. Regular reporting on key performance indicators (KPIs) allows for ongoing evaluation and quality improvement initiatives. This continuous feedback loop ensures the services provided remain relevant, effective, and responsive to the needs of the clients.
Q 19. How do you adapt your treatment planning approach to accommodate diverse client needs and preferences?
Adaptability is crucial in treatment planning. I recognize that every individual is unique, with diverse needs, preferences, cultural backgrounds, and coping mechanisms. A one-size-fits-all approach is ineffective. My treatment plans are individualized, acknowledging these differences.
For example, when working with a client from a specific cultural background, I make sure to consider their cultural values and beliefs in the treatment planning process. I might involve family members in the process if appropriate and culturally acceptable. I might also adjust the language used to better align with their cultural understanding. Similarly, clients’ personal preferences are carefully considered— whether they prefer individual therapy or group therapy, online or in-person sessions, and the pace at which they wish to progress.
The process of creating an individualized treatment plan is a collaborative one, involving open communication and shared decision-making between the client and myself. Regular review and adjustment of the plan ensure it remains relevant and supportive of the client’s evolving needs and progress. I also involve other professionals, such as psychiatrists, social workers, and occupational therapists, to ensure a comprehensive and holistic approach that fully addresses the diverse needs of each client.
Q 20. Explain your understanding of evidence-based practices in case management.
Evidence-based practices (EBPs) are the cornerstone of my case management approach. EBPs are interventions and strategies that have been proven effective through rigorous scientific research. Integrating EBPs ensures that the services provided are not only ethical but also demonstrably beneficial.
Examples of EBPs I frequently utilize include Cognitive Behavioral Therapy (CBT) for managing anxiety and depression, Dialectical Behavior Therapy (DBT) for borderline personality disorder, and motivational interviewing for addressing substance abuse. I stay updated on the latest research and clinical guidelines to maintain proficiency in these and other evidence-based methods.
The integration of EBPs is not merely about applying pre-determined techniques; it is about critically evaluating research findings and adapting them to individual client needs. This necessitates ongoing professional development, regular consultation with colleagues, and a commitment to continuous learning and improvement. By basing my practice on sound evidence, I can ensure that clients receive the most effective and appropriate care possible.
Q 21. How do you manage your own stress and maintain a healthy work-life balance in a demanding role?
Case management can be emotionally and mentally demanding. Self-care is not a luxury; it’s a necessity for maintaining well-being and professional effectiveness. I prioritize self-care strategies that enhance both my physical and mental health.
This includes regular exercise, maintaining a healthy diet, getting adequate sleep, and practicing mindfulness techniques like meditation or deep breathing exercises. I also engage in activities that promote relaxation and stress reduction, such as spending time in nature, listening to music, or pursuing hobbies. Creating boundaries between work and personal life is crucial; I maintain a strict separation of work hours and personal time as much as possible.
Furthermore, I actively participate in supervision and peer support groups, providing opportunities to discuss challenging cases, process emotions, and receive guidance from experienced colleagues. This collegial support network is invaluable for managing stress and preventing burnout. Regular self-reflection on my emotional and mental state helps me identify any warning signs of stress or burnout and proactively implement strategies to address them. By prioritizing self-care, I maintain a healthy work-life balance, ensuring my capacity to provide high-quality care to my clients.
Q 22. What are your goals for professional development in case management?
My professional development goals in case management center around enhancing my expertise in three key areas: technology integration, data-driven decision making, and advanced care coordination techniques. I aim to become proficient in utilizing advanced case management software to streamline workflows and improve data analysis. This includes learning to extract meaningful insights from client data to personalize treatment plans and measure outcomes more effectively. Furthermore, I’m committed to developing my skills in coordinating care across diverse and complex healthcare systems, particularly focusing on improving communication and collaboration among providers to ensure seamless transitions of care.
For example, I’m currently pursuing a certification in a specific case management software that is increasingly used in our area, and I plan to attend workshops on advanced analytics and care coordination strategies. This continual learning will allow me to provide more efficient and effective services to my clients and contribute more meaningfully to our team.
Q 23. Describe your experience with care coordination across multiple healthcare settings.
I have extensive experience coordinating care across various healthcare settings, including hospitals, outpatient clinics, skilled nursing facilities, and home healthcare agencies. My work has involved coordinating care for individuals with complex medical and social needs, often requiring collaboration with multiple specialists, social workers, and family members. Think of it like orchestrating a complex symphony – each musician (healthcare provider) needs to play their part at the right time and in harmony to achieve the desired outcome (optimal patient care).
For instance, I recently worked with a patient transitioning from acute hospital care to home healthcare. I coordinated with the hospital discharge planner, home health nurse, physical therapist, and social worker to ensure a smooth and safe transition. This involved securing necessary medical equipment, arranging home modifications, and ensuring the patient had access to medication and transportation. Successful care coordination in such a scenario hinges on clear communication, proactive planning, and a deep understanding of each provider’s role and responsibilities.
Q 24. How familiar are you with different reimbursement models and their impact on treatment planning?
I am very familiar with various reimbursement models, including fee-for-service, capitation, and value-based care. Understanding these models is crucial because they directly influence treatment planning and resource allocation. For example, under a fee-for-service model, the focus might be on providing a high volume of individual services, whereas a value-based care model emphasizes cost-effective, outcome-driven interventions.
In my experience, a thorough understanding of the reimbursement model guides the development of the treatment plan. In a capitated model, for instance, I would focus on preventative measures and early interventions to avoid costly hospitalizations. In a value-based care model, I would concentrate on measurable outcomes like improved functional capacity and reduced hospital readmissions, documenting these improvements rigorously to demonstrate value.
Q 25. How do you handle ethical dilemmas in case management?
Ethical dilemmas in case management are inevitable. My approach involves a systematic process: identify the conflict, gather all relevant information, consider the perspectives of all involved parties, including the client, family, and healthcare providers, explore potential solutions, and consult with supervisors or ethics committees when necessary. The core principle guiding my decisions is always the client’s best interests, while adhering to relevant laws and professional standards.
For example, I once faced a situation where a client’s family disagreed with the client’s treatment plan. I carefully listened to both sides, ensuring the client’s wishes were respected to the greatest extent possible while ensuring safety and well-being. By facilitating open communication and mediation, we reached a compromise that satisfied both the client and the family, demonstrating the importance of ethical consideration and effective communication in resolving conflict.
Q 26. What are your strategies for ensuring client satisfaction and engagement?
Ensuring client satisfaction and engagement is paramount. My strategies include: active listening, shared decision-making, and consistent communication. I actively involve clients in the planning and implementation of their treatment, making them feel empowered and in control of their care. Regular check-ins, clear explanations, and prompt responses to their questions or concerns are essential. I also leverage motivational interviewing techniques to help clients identify and overcome barriers to their recovery and treatment adherence.
For example, I might start by understanding a client’s personal goals and priorities. Then, I integrate those goals into the treatment plan. Instead of simply dictating a plan, we collaborate on developing a roadmap that aligns with their values. This participatory approach fosters trust and builds a strong therapeutic relationship, leading to greater engagement and improved outcomes.
Q 27. Describe a time you had to make a difficult decision regarding a client’s treatment.
I once had to make a difficult decision regarding a client who was struggling with substance abuse and lacked consistent housing. The client wanted to focus solely on addressing their substance abuse, while I felt that securing stable housing was crucial for long-term success. After careful consideration of the client’s situation, including their history and the potential risks associated with each approach, I decided to prioritize securing stable housing before intensifying substance abuse treatment. This decision was based on the understanding that stable housing provided a foundation for addressing other needs effectively and reducing the risk of relapse.
The decision wasn’t easy, and it required ongoing communication and collaboration with the client. However, it ultimately proved beneficial as having a stable environment allowed the client to focus more effectively on substance abuse treatment and maintain progress over time.
Q 28. How do you stay up-to-date with the latest trends and best practices in case management?
Staying current is crucial in this rapidly evolving field. I utilize various strategies to stay abreast of the latest trends and best practices. This includes: actively participating in professional organizations like the Case Management Society of America (CMSA), attending continuing education workshops and conferences, reading peer-reviewed journals and professional publications, and actively engaging in online communities and forums dedicated to case management.
Additionally, I regularly review and update my knowledge of relevant laws and regulations, ensuring my practice aligns with the highest ethical and professional standards. I believe that continuous learning is essential to provide the best possible care to my clients and contribute to improving the overall quality of case management services.
Key Topics to Learn for Case Management and Treatment Planning Interview
- Assessment and Needs Identification: Understanding the process of conducting thorough client assessments, identifying their needs, and utilizing various assessment tools effectively.
- Treatment Planning Development: Mastering the creation of individualized treatment plans, including goal setting, intervention strategies, and measurable outcomes. Understand the importance of collaboration with clients and other professionals.
- Care Coordination and Collaboration: Demonstrate knowledge of effective communication and coordination strategies with clients, families, healthcare providers, and other stakeholders involved in the care process.
- Resource Management and Advocacy: Discuss the skills needed to identify and access appropriate community resources, advocate for clients’ needs, and navigate complex systems.
- Ethical Considerations and Legal Frameworks: Understanding the ethical principles and legal guidelines governing case management and treatment planning practices.
- Documentation and Reporting: Proficiency in accurate and timely documentation of client interactions, progress notes, and treatment plan updates. Be prepared to discuss different documentation systems and their requirements.
- Crisis Intervention and Risk Management: Understanding strategies for managing crises, assessing risk, and implementing safety plans.
- Case Closure and Evaluation: Demonstrate your knowledge of the process for closing cases, evaluating outcomes, and ensuring continuity of care.
- Cultural Competence and Diversity: Highlight your understanding of diverse populations and cultural considerations in treatment planning.
- Technology in Case Management: Discuss your familiarity with Electronic Health Records (EHRs) and other relevant technology used in case management.
Next Steps
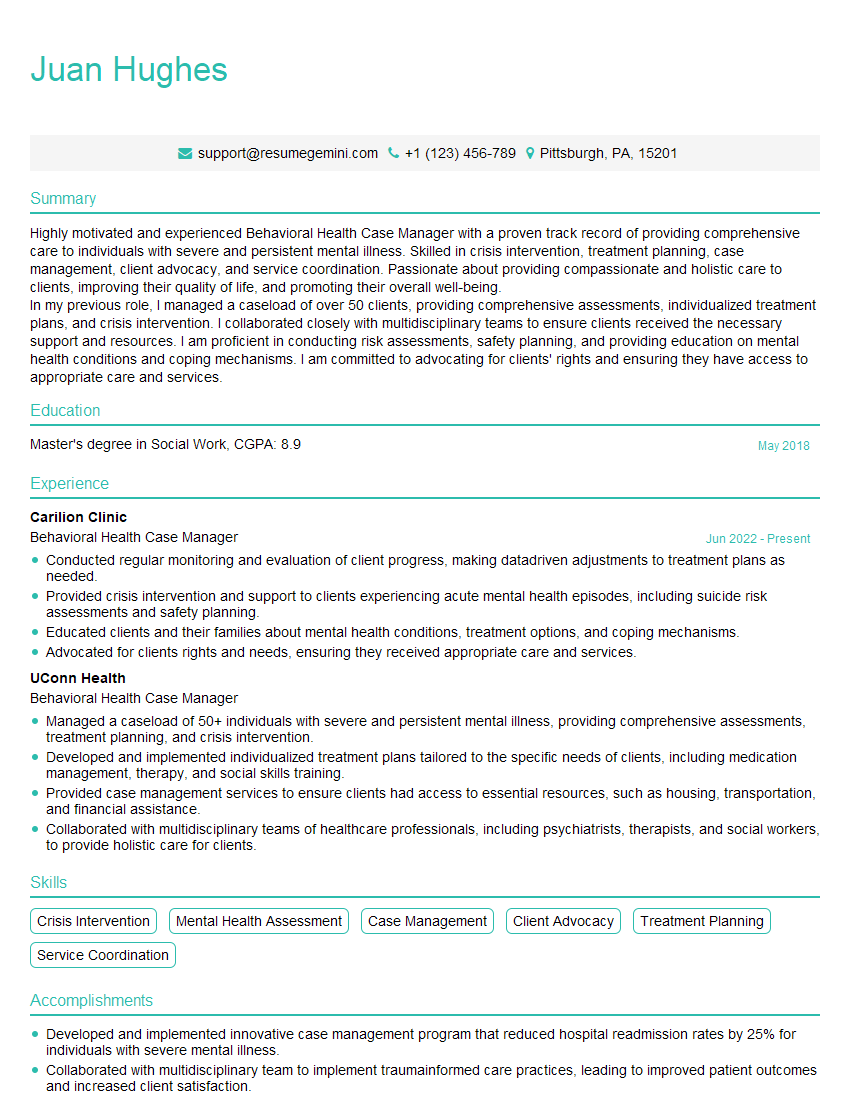
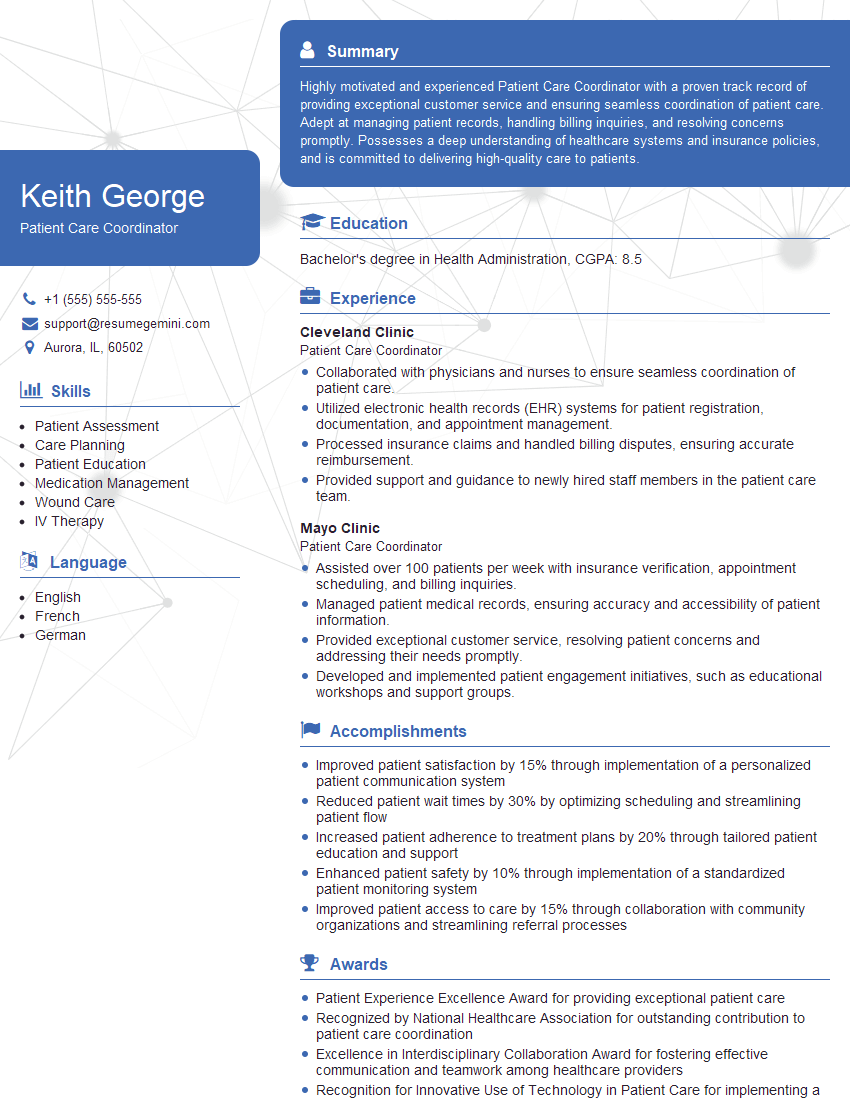
Mastering Case Management and Treatment Planning is crucial for career advancement in the human services field. It demonstrates your ability to provide comprehensive and effective client care, leading to greater responsibility and career growth opportunities. To stand out to potential employers, create an ATS-friendly resume that highlights your key skills and experience. ResumeGemini is a trusted resource that can help you build a professional and impactful resume tailored to the specific demands of this competitive field. Examples of resumes tailored to Case Management and Treatment Planning are available to provide you with inspiration and guidance.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.