Every successful interview starts with knowing what to expect. In this blog, we’ll take you through the top Substance Use Prevention and Control interview questions, breaking them down with expert tips to help you deliver impactful answers. Step into your next interview fully prepared and ready to succeed.
Questions Asked in Substance Use Prevention and Control Interview
Q 1. Describe your experience developing and implementing substance use prevention programs.
My experience in developing and implementing substance use prevention programs spans over 15 years, encompassing a range of settings from schools and community centers to correctional facilities and healthcare organizations. I’ve been involved in every stage, from needs assessment and program design to implementation, evaluation, and refinement. For example, in a rural community facing high rates of opioid misuse, I led the development of a multi-pronged program combining school-based education, community outreach events, and collaboration with local healthcare providers to increase access to treatment and harm reduction services. This involved securing funding, training facilitators, developing culturally relevant materials, and establishing strong partnerships with stakeholders. The program’s success was measured by reductions in opioid-related hospitalizations and emergency room visits, and increases in help-seeking behaviors among at-risk youth. Another significant project focused on creating a comprehensive prevention curriculum for middle schools, incorporating interactive workshops, peer mentoring, and parent education components. This project highlighted the importance of adapting prevention strategies to the specific needs and developmental stage of the target population.
Q 2. Explain different evidence-based prevention strategies for adolescents.
Evidence-based prevention strategies for adolescents target multiple levels of influence—individual, peer, family, school, and community. Some key approaches include:
- Information Dissemination: Educating adolescents about the risks associated with substance use, dispelling myths, and providing accurate information about the effects of different substances. This often involves interactive workshops, media campaigns, and educational materials.
- Social Influence Programs: These programs aim to change social norms around substance use, reducing the perceived social pressure to use drugs. Techniques like peer leadership and media counter-campaigns are commonly used.
- Life Skills Training: Equipping adolescents with the skills necessary to resist peer pressure, manage stress, make healthy choices, and cope with challenging situations. These skills include refusal skills, problem-solving, conflict resolution, and stress management techniques.
- Family-Based Interventions: Strengthening family bonds and communication patterns, addressing family conflict, and improving parenting skills can significantly reduce adolescents’ risk of substance use. Family therapy and parent training programs are examples.
- School-Based Programs: Implementing comprehensive school-wide prevention efforts that integrate substance use prevention into the overall school climate. This includes policies against substance use, teacher training, and school-based support services.
- Community-Based Programs: Creating supportive community environments that promote healthy behaviors and reduce the availability of substances. This can involve community-wide campaigns, public awareness initiatives, and partnerships with local organizations.
It’s crucial to remember that a multi-faceted approach, combining multiple evidence-based strategies, is usually most effective.
Q 3. How would you assess the needs of a community to develop a targeted prevention program?
Assessing community needs for a targeted prevention program requires a comprehensive approach involving several key steps:
- Data Collection: Gather data from various sources, including epidemiological studies, law enforcement reports, health surveys, and school records, to understand the prevalence and patterns of substance use in the community.
- Community Forums and Surveys: Organize community forums, focus groups, and surveys to gather input from residents, stakeholders, and community leaders about their perceptions of substance use, its impact on their lives, and potential solutions.
- Key Informant Interviews: Conduct interviews with key individuals in the community, such as healthcare professionals, educators, law enforcement officials, and faith leaders, to obtain their perspectives and insights on substance use issues.
- Risk and Protective Factor Assessment: Identify the specific risk and protective factors contributing to substance use within the community. Risk factors might include poverty, lack of access to resources, exposure to substance use, while protective factors could include strong family ties, positive peer influences, and access to healthy activities.
- Needs Assessment Report: Synthesize the information gathered to develop a comprehensive needs assessment report that identifies the community’s specific needs, priorities, and challenges related to substance use.
- Program Development and Implementation: Use the needs assessment findings to guide the development and implementation of a targeted prevention program that addresses the identified needs and risk factors.
For instance, a community might reveal high rates of youth alcohol use linked to easy access to alcohol and a lack of alternative recreational activities. The program would then prioritize addressing these specific issues through initiatives such as stricter enforcement of underage drinking laws and the establishment of youth-oriented recreational programs.
Q 4. What are the key risk factors associated with substance abuse?
Key risk factors for substance abuse are complex and interconnected, falling into several categories:
- Individual Risk Factors: These include genetic predisposition, early onset of substance use, mental health disorders (depression, anxiety, etc.), impulsivity, low self-esteem, and history of trauma.
- Family Risk Factors: Factors such as family history of substance abuse, parental substance use, dysfunctional family dynamics, lack of parental supervision, and family conflict increase the risk.
- Peer Risk Factors: Peer pressure, association with substance-using peers, and lack of prosocial peer networks are significant risk factors.
- School Risk Factors: Academic difficulties, poor school performance, lack of school engagement, and negative school climate can increase the likelihood of substance use.
- Community Risk Factors: Easy access to drugs, lack of community resources, high rates of crime and poverty, and weak community bonds contribute significantly to substance abuse.
- Societal Risk Factors: Societal norms that normalize or condone substance use, media portrayals that glamorize substance use, and lack of public awareness about the risks of substance abuse also play a role.
It’s essential to understand that the presence of multiple risk factors significantly increases an individual’s vulnerability to substance abuse. Conversely, the presence of protective factors can buffer against these risks.
Q 5. How do you incorporate cultural sensitivity into substance use prevention interventions?
Incorporating cultural sensitivity into substance use prevention interventions is paramount for their effectiveness. Ignoring cultural factors can lead to programs that are irrelevant, ineffective, and even harmful. Here’s how to ensure cultural sensitivity:
- Needs Assessment: Conduct a thorough needs assessment that specifically addresses the cultural context of the target community. Understand the community’s values, beliefs, traditions, and communication styles.
- Culturally Relevant Materials: Develop educational materials and programs that are culturally appropriate and relatable to the target audience. Use language, images, and examples that resonate with their cultural background.
- Cultural Brokers: Employ cultural brokers or community members to help build trust, facilitate communication, and ensure the program is culturally sensitive and relevant.
- Respect for Cultural Practices: Be respectful of cultural practices and beliefs that may affect substance use patterns or treatment adherence. For example, certain cultures may have traditional healing practices that can be integrated into prevention or treatment programs.
- Language Access: Ensure access to services in the preferred language of the target community.
- Collaboration with Community Leaders: Engage with community leaders and organizations to gain their support and ensure the program aligns with community values.
For example, a program targeting Native American communities should incorporate traditional healing practices and address historical trauma, which can significantly impact substance use patterns. Similarly, a program targeting Latino communities should consider the role of family and religious beliefs in shaping attitudes towards substance use.
Q 6. Explain your understanding of the stages of change in addiction treatment.
The Stages of Change model (Transtheoretical Model) provides a framework for understanding and addressing an individual’s readiness for change in the context of addiction treatment. These stages are:
- Precontemplation: The individual is not considering changing their substance use behavior. They may be unaware of the problem or unwilling to acknowledge it.
- Contemplation: The individual is beginning to think about changing their behavior. They are weighing the pros and cons of change, often experiencing ambivalence.
- Preparation: The individual is making plans to change their behavior. They may be taking small steps towards change, such as seeking information or talking to a counselor.
- Action: The individual is actively making changes to their behavior. This stage requires significant effort and commitment.
- Maintenance: The individual is working to maintain their changed behavior over time. Relapse prevention strategies are crucial during this stage.
- Relapse: A return to previous substance use patterns. Relapse is considered a normal part of the recovery process, and it’s an opportunity to learn and adjust strategies for future success.
Understanding these stages allows for tailored interventions that match the individual’s readiness for change. For example, someone in the precontemplation stage might benefit from motivational interviewing to raise awareness of the problem, while someone in the action stage might need support in developing coping mechanisms and relapse prevention strategies.
Q 7. Describe your experience working with individuals struggling with substance use disorders.
My experience working with individuals struggling with substance use disorders involves both direct clinical work and program development. I’ve worked with diverse populations in various settings, utilizing different therapeutic approaches tailored to individual needs. I’ve used evidence-based practices such as Motivational Interviewing (MI) to help individuals explore their ambivalence about change and build intrinsic motivation. Cognitive Behavioral Therapy (CBT) has been instrumental in helping individuals identify and modify negative thought patterns and behaviors that contribute to substance use. I’ve also worked with clients facing co-occurring disorders (mental health and substance use), utilizing integrated treatment approaches to address both conditions simultaneously. One particularly memorable case involved working with a young adult struggling with opioid addiction and severe anxiety. Through a combination of MI, CBT, and medication management, we were able to help them achieve sustained recovery, highlighting the importance of individualized and holistic care. Furthermore, I have experience coordinating care with other professionals including medical doctors, psychiatrists, and social workers, which is crucial for providing comprehensive and effective support.
Q 8. What are some effective strategies for engaging individuals in treatment?
Engaging individuals in treatment for substance use requires a multifaceted approach that prioritizes building rapport and understanding their individual needs and motivations. It’s not a one-size-fits-all solution; we need to meet people where they are.
Motivational Interviewing: This collaborative, person-centered approach helps individuals explore and resolve ambivalence about change. I use open-ended questions, reflective listening, and affirmations to empower them to make their own decisions.
Harm Reduction Strategies: Offering harm reduction services, like needle exchange programs or naloxone training, can build trust and demonstrate a non-judgmental approach. This shows clients that we’re focused on their well-being, regardless of their current substance use.
Addressing Barriers: Practical obstacles like childcare, transportation, or lack of insurance can prevent someone from seeking help. We actively work to remove these barriers, connecting clients with resources and support systems.
Building a Therapeutic Alliance: Establishing a strong, trusting relationship based on empathy and respect is crucial. I strive to create a safe and comfortable environment where clients feel heard and understood.
Peer Support: Connecting individuals with peer recovery support specialists who’ve successfully navigated recovery can be incredibly powerful. Hearing from someone who understands their struggles firsthand can be incredibly motivating.
For example, I recently worked with a young woman struggling with opioid addiction. She was hesitant to enter treatment due to childcare concerns. By connecting her with a local daycare offering subsidized care, we removed that barrier, allowing her to focus on her recovery.
Q 9. How do you handle resistance to treatment among clients?
Resistance to treatment is common and often stems from a complex interplay of factors, including fear, denial, shame, and a lack of perceived benefit. Addressing this resistance requires patience, understanding, and a willingness to adapt our approach.
Validate Feelings: Acknowledge and validate the client’s feelings without judgment. Saying something like, “It makes sense that you’re hesitant; change is difficult,” can help build rapport.
Explore Ambivalence: Use motivational interviewing techniques to gently explore the client’s ambivalence about change. Help them weigh the pros and cons of treatment in their own words.
Collaborative Goal Setting: Instead of imposing a treatment plan, work collaboratively with the client to set realistic and achievable goals. This fosters a sense of ownership and control.
Adjust Treatment Strategies: If one approach isn’t working, be prepared to adjust your strategy. Perhaps a different therapeutic modality or a different level of care is needed.
Involve Support Systems: Engaging family or friends in the treatment process, with the client’s consent, can provide additional support and encouragement.
For instance, I had a client who initially resisted attending group therapy. By understanding his social anxiety, we started with individual sessions and gradually introduced him to group settings, offering him a supportive and comfortable environment to adjust.
Q 10. What are the ethical considerations in providing substance use prevention and treatment services?
Ethical considerations are paramount in substance use prevention and treatment. Maintaining client confidentiality, ensuring informed consent, and upholding professional boundaries are vital.
Confidentiality (HIPAA): Strict adherence to HIPAA regulations is essential. All client information must be protected and disclosed only with appropriate authorization.
Informed Consent: Clients must be fully informed about the treatment process, including potential risks and benefits, before consenting to services. This includes understanding their rights and options.
Dual Relationships: Avoiding dual relationships, such as social or personal relationships with clients, is critical to maintain professional boundaries and prevent conflicts of interest.
Cultural Competence: Providing culturally sensitive and appropriate care is vital. This includes understanding and respecting the client’s cultural beliefs and practices.
Mandatory Reporting: Understanding and following mandatory reporting laws regarding child abuse, elder abuse, or threats of harm to self or others is crucial.
For example, a client may share sensitive information about a past trauma. Ethical practice mandates maintaining strict confidentiality while providing appropriate support and referrals if needed.
Q 11. How do you measure the effectiveness of your prevention programs?
Measuring the effectiveness of prevention programs involves utilizing a variety of methods to assess both process and outcomes. A multi-pronged approach is best to capture a holistic view of program impact.
Quantitative Data: This includes using surveys, questionnaires, and statistical analysis to measure changes in substance use behaviors, knowledge, attitudes, and risk factors among participants. For example, we might track changes in alcohol consumption rates or the prevalence of drug use among a target population.
Qualitative Data: This involves using focus groups, interviews, and observations to gather in-depth information on participants’ experiences, perspectives, and feedback. This helps us understand the impact of the program beyond numbers.
Process Evaluation: Assessing the implementation process itself – fidelity to the program model, participant engagement, staff training, and resource allocation – helps identify areas for improvement.
Longitudinal Studies: Following participants over time allows us to assess the long-term impact of the prevention program on substance use patterns and other relevant outcomes. This provides valuable insights into the sustainability of the program’s effects.
For example, a school-based prevention program might track students’ substance use prevalence before, during, and after the program’s implementation, and conduct follow-up surveys years later to evaluate long-term impact.
Q 12. What are the common relapse prevention strategies you use?
Relapse prevention is a crucial aspect of substance use treatment. It involves equipping individuals with the skills and strategies to manage cravings, triggers, and high-risk situations.
Identifying Triggers: We work with clients to identify personal triggers – people, places, things, emotions – that increase the risk of relapse. This involves self-monitoring and reflection.
Developing Coping Mechanisms: Clients learn healthy coping strategies to manage stress, cravings, and difficult emotions without resorting to substance use. Examples include relaxation techniques, mindfulness practices, and healthy distraction activities.
Relapse Prevention Planning: We collaboratively develop a personalized relapse prevention plan that outlines strategies for managing high-risk situations, identifying warning signs of relapse, and seeking support when needed.
Social Support: Building a strong support network through family, friends, support groups (like AA or NA), or peer support specialists is vital. This network can provide crucial encouragement and accountability.
Contingency Management: This involves establishing clear rewards and consequences for adherence to the treatment plan. This can help maintain motivation and prevent backsliding.
For instance, a client might identify that feeling lonely triggers their substance use. We’d then work together to develop coping mechanisms like connecting with support groups or engaging in hobbies that foster connection and reduce loneliness.
Q 13. Describe your experience with motivational interviewing techniques.
Motivational Interviewing (MI) is a cornerstone of my approach. It’s a person-centered, directive counseling method that helps individuals resolve ambivalence about change.
Principles of MI: MI is guided by four core principles: expressing empathy, developing discrepancy, rolling with resistance, and supporting self-efficacy. These principles guide my interactions with clients.
Open-Ended Questions: I use open-ended questions to encourage clients to explore their thoughts and feelings about substance use and their desire for change. Examples include: “Tell me about your experience with…” or “How do you feel about…”
Reflective Listening: I actively listen to clients, reflecting back what I hear to ensure understanding and to help them clarify their own thoughts. This shows that I’m paying attention and validating their feelings.
Affirmations: I offer affirmations to acknowledge clients’ strengths and efforts, fostering a sense of hope and self-belief. This can be especially important when dealing with low self-esteem.
Summarizing: I regularly summarize key points of our conversations to reinforce understanding and help clients identify their own progress toward change.
For example, with a client struggling with alcohol use, I might use reflective listening to understand their ambivalence and then gently guide them towards identifying their reasons for wanting to change.
Q 14. How do you address co-occurring disorders (e.g., mental health and substance use) in your work?
Co-occurring disorders (CODs), also known as dual diagnoses, are common among individuals with substance use disorders. Addressing these requires an integrated approach that acknowledges the interconnectedness of mental health and substance use.
Integrated Treatment: I advocate for integrated treatment models that simultaneously address both the substance use disorder and the co-occurring mental health condition. This may involve working collaboratively with a psychiatrist or other mental health professionals.
Comprehensive Assessment: A thorough assessment is crucial to accurately diagnose both disorders and tailor treatment accordingly. This might involve psychological testing and interviews.
Medication Management: Medication can play a crucial role in stabilizing mental health symptoms and reducing cravings. This is typically managed in collaboration with a psychiatrist.
Therapy for Both Disorders: Therapeutic approaches, such as Cognitive Behavioral Therapy (CBT) or Dialectical Behavior Therapy (DBT), can address underlying mental health issues and develop coping skills for both substance use and mental health challenges.
For example, a client with depression and alcohol dependence might receive medication to manage depression alongside therapy to address both the depression and the substance use. An integrated approach ensures that both conditions are treated holistically.
Q 15. What are some effective methods for harm reduction in substance use?
Harm reduction strategies aim to minimize the negative consequences of substance use without necessarily requiring abstinence. They acknowledge that complete cessation isn’t always feasible or desirable for everyone, especially in the initial stages of recovery. These methods focus on reducing risks associated with drug use, improving health and well-being, and promoting engagement in treatment.
Needle exchange programs: Provide clean needles and syringes to prevent the spread of infectious diseases like HIV and Hepatitis C. Imagine a scenario where a person who injects drugs can exchange used needles for clean ones, significantly reducing their risk of contracting a life-threatening illness.
Naloxone distribution: Provides naloxone, a medication that can reverse opioid overdoses. Training individuals on how to administer naloxone can be life-saving, allowing them to quickly respond to an overdose and potentially prevent a fatality. This empowers communities to take direct action in saving lives.
Supervised consumption sites: Offer a safe and hygienic environment for individuals to use drugs under medical supervision. These sites can reduce overdose deaths, provide access to healthcare, and link individuals to treatment and support services. Think of them as a controlled setting where immediate medical attention is available, mitigating risks associated with unsupervised substance use.
Methadone and buprenorphine treatment: Medication-assisted treatment (MAT) uses medications to manage withdrawal symptoms, cravings, and reduce the risk of relapse. These medications are used under medical supervision and can drastically increase the chances of successful recovery.
Harm reduction counseling and education: Providing education about safer drug use practices, including reducing dosage, avoiding mixing drugs, and recognizing signs of overdose. This empowers individuals with knowledge to make informed decisions about their health.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Explain your knowledge of different types of substance use disorders.
Substance Use Disorders (SUDs) are a broad category encompassing a range of conditions characterized by problematic patterns of substance use that lead to clinically significant impairment or distress. The severity of the disorder varies greatly.
Alcohol Use Disorder (AUD): This encompasses a spectrum of problems, from mild alcohol misuse to severe alcohol dependence, marked by a strong craving for alcohol, loss of control over drinking, and continued use despite negative consequences.
Opioid Use Disorder (OUD): Involves problematic use of opioid medications or illicit opioids like heroin, characterized by intense cravings, tolerance (needing higher doses for the same effect), and withdrawal symptoms.
Stimulant Use Disorder (SUD): Encompasses the problematic use of stimulants such as cocaine, methamphetamine, and ADHD medications. This can lead to increased energy, decreased need for sleep, and potential for significant psychological and physiological harm.
Cannabis Use Disorder (CUD): Involves problematic use of cannabis, leading to impairment in daily functioning and significant distress. While less severe than other SUDs in many cases, the long-term effects of cannabis use should not be dismissed.
Other SUDs: This includes problematic use of sedatives, hypnotics, anxiolytics (e.g., benzodiazepines), hallucinogens (e.g., LSD), inhalants, and tobacco.
The diagnosis of a SUD considers factors like the severity of substance use, the impact on daily life, and the presence of withdrawal symptoms and tolerance. Each type of SUD requires a tailored treatment approach.
Q 17. How do you maintain confidentiality and adhere to HIPAA regulations?
Maintaining confidentiality and adhering to HIPAA regulations is paramount in my work. HIPAA (Health Insurance Portability and Accountability Act) is a US law protecting the privacy and security of Protected Health Information (PHI). I ensure compliance through several key practices:
Strict adherence to HIPAA guidelines: I understand and apply all relevant HIPAA rules and regulations related to the handling, storage, and disclosure of PHI. This includes using secure electronic systems and following protocols for paper-based records.
Limited access to client information: Only authorized personnel involved directly in a client’s care have access to their PHI. Access is granted on a need-to-know basis, and all access is logged and monitored.
Secure data storage: Client records are stored in secure, password-protected electronic systems, following best practices for data encryption and backup.
Confidential communication: I use secure communication methods when discussing clients’ information with other professionals, avoiding public or unsecured communication channels.
Client consent: I always obtain informed consent before disclosing any PHI, ensuring clients understand how their information will be used and with whom it will be shared.
Continuing education: I stay updated on HIPAA regulations and best practices through continuing education courses and professional development.
Breaches of confidentiality can have serious legal and ethical consequences. My commitment to protecting client privacy is unwavering.
Q 18. What are some community resources you frequently utilize?
I frequently utilize a variety of community resources to provide comprehensive support to my clients. These resources form a vital network that extends beyond individual therapy.
Local hospitals and emergency rooms: For immediate medical attention in cases of overdose or other medical emergencies.
Mental health clinics: To address co-occurring mental health disorders, which are often present in individuals with SUDs.
Substance abuse treatment centers: For detoxification, residential treatment, and outpatient programs tailored to specific needs.
Support groups (e.g., AA, NA): These peer-support groups provide valuable social support and a sense of community for individuals in recovery.
Housing assistance programs: Stable housing is crucial for recovery, and I often work with organizations that provide housing support to individuals experiencing homelessness.
Vocational rehabilitation services: These programs help clients develop job skills and find employment, an important step toward independent living.
Collaborating with these organizations ensures a holistic approach to care, enhancing the effectiveness of treatment and improving client outcomes.
Q 19. How do you build rapport with clients from diverse backgrounds?
Building rapport with clients from diverse backgrounds requires cultural sensitivity, empathy, and a genuine commitment to understanding individual experiences. I use a person-centered approach, adapting my communication style to meet each client’s unique needs.
Active listening: Paying close attention to both verbal and nonverbal cues, demonstrating that I value their perspective.
Cultural humility: Acknowledging my own biases and limitations, and continuously seeking to learn more about different cultures and perspectives. I might ask questions about their cultural background, but always respectfully.
Language access: Ensuring access to interpreters or culturally appropriate materials, as needed. This is vital for effective communication and building trust.
Understanding unique challenges: Recognizing that individuals from marginalized communities may face additional barriers to accessing care, such as systemic discrimination or lack of resources. Addressing these barriers is vital.
Collaboration with community leaders: Working with community leaders and organizations to build bridges and better understand the needs of diverse populations.
Building trust is a fundamental aspect of effective treatment. By demonstrating respect and understanding, I can create a safe and supportive environment where clients feel comfortable sharing their experiences.
Q 20. How do you collaborate with other professionals in the field?
Collaboration with other professionals is essential for effective substance use prevention and control. I regularly work with a multidisciplinary team to provide comprehensive care.
Physicians: For medical evaluations, medication management, and monitoring of physical health.
Psychiatrists: To address co-occurring mental health disorders.
Social workers: For case management, connecting clients to resources, and addressing social determinants of health.
Case managers: Coordinate services and help navigate the healthcare system.
Peer support specialists: Individuals with lived experience who provide valuable support and understanding.
Family therapists: When appropriate, to involve family members in the treatment process and address family dynamics.
Effective communication and regular meetings with team members are crucial for coordinating care, sharing information, and ensuring a consistent approach. We use a shared electronic health record system (where permitted) to enhance communication and prevent information silos. This collaborative approach enhances the quality of care and improves client outcomes.
Q 21. Describe your experience with crisis intervention related to substance abuse.
Crisis intervention in substance abuse can involve a range of situations, from overdose to acute withdrawal symptoms or suicidal ideation. My approach emphasizes immediate safety and stabilization, followed by connection to ongoing care.
Assessment: Rapidly assessing the client’s immediate needs, identifying the nature of the crisis, and ensuring their safety. This may involve checking vital signs, assessing risk factors for suicide or violence, and stabilizing any medical conditions.
Stabilization: Addressing immediate needs, such as medical care, managing withdrawal symptoms, or providing emotional support. This might include administering naloxone in an overdose situation, or providing supportive counseling during an acute anxiety episode.
Referral and connection to resources: Connecting the client to appropriate resources, such as a hospital, detoxification facility, mental health services, or community support groups. This might include helping them schedule appointments or arrange transportation.
Safety planning: Developing a safety plan to help prevent future crises. This could involve identifying warning signs, creating coping mechanisms, and establishing support systems.
Follow-up: Following up with the client to ensure they have accessed necessary services and are doing well. This ensures continuous support beyond the immediate crisis.
Effective crisis intervention requires quick thinking, strong decision-making skills, and a deep understanding of substance use disorders. It’s crucial to maintain a calm and reassuring demeanor to build trust and help the individual feel safe.
Q 22. How do you address substance abuse among different age groups?
Addressing substance abuse requires a tailored approach, varying significantly across age groups due to developmental differences, social contexts, and exposure to risk factors.
Children and Adolescents: Prevention is paramount. We focus on education programs in schools, targeting risk factors like peer pressure and early experimentation. We also work with families, providing support and guidance to create protective environments. Interventions involve evidence-based strategies like motivational interviewing and family-based therapy. For instance, a school program might teach refusal skills and the long-term consequences of substance use.
Young Adults (18-25): This group often faces transitions like college or entering the workforce, increasing vulnerability. Interventions focus on harm reduction strategies, such as responsible alcohol consumption, and addressing underlying mental health issues that can contribute to substance abuse. Peer support groups and targeted social media campaigns are often effective. For example, a university might offer workshops on stress management and healthy coping mechanisms.
Adults (26+): Treatment strategies for adults may involve individual or group therapy, medication-assisted treatment (MAT), and relapse prevention planning. Addressing co-occurring disorders (mental health issues and substance abuse) is crucial. For instance, a treatment program might combine cognitive behavioral therapy (CBT) with medication to address both depression and opioid addiction.
Older Adults: This population faces unique challenges, including chronic health problems and social isolation. Interventions often need to adapt to physical limitations and incorporate strategies that address age-related concerns. For instance, a treatment program might incorporate support for managing chronic pain alongside addressing substance dependence.
Q 23. What is your experience with specific therapeutic modalities for addiction treatment?
My experience encompasses a range of therapeutic modalities, each with its strengths in addressing specific aspects of addiction.
Cognitive Behavioral Therapy (CBT): CBT helps individuals identify and change negative thought patterns and behaviors that contribute to substance use. I’ve used CBT extensively to help clients develop coping mechanisms for cravings and triggers. For example, I’ve helped clients identify situations that lead to substance use and then collaboratively develop alternative responses.
Motivational Interviewing (MI): MI is a client-centered approach that empowers individuals to recognize their own reasons for change. It’s particularly effective in the early stages of treatment, fostering intrinsic motivation. For example, I use MI to explore a client’s ambivalence towards recovery and guide them toward identifying their own goals.
Dialectical Behavior Therapy (DBT): DBT is particularly useful for clients with co-occurring disorders, such as borderline personality disorder and substance abuse. It focuses on emotional regulation and distress tolerance skills. For instance, I’ve used DBT to teach a client mindfulness techniques to manage intense emotions and reduce impulsive behaviors related to substance use.
Medication-Assisted Treatment (MAT): I work collaboratively with physicians to incorporate MAT where appropriate. MAT uses medications like methadone or buprenorphine to reduce withdrawal symptoms and cravings, making it easier for clients to engage in therapy and achieve sustained recovery.
Q 24. Explain your understanding of the impact of trauma on substance abuse.
Trauma significantly impacts substance abuse. Many individuals use substances as a maladaptive coping mechanism to manage the psychological pain and distress resulting from traumatic experiences. This is often referred to as self-medication.
The connection between trauma and substance abuse is complex. Trauma can lead to mental health conditions like PTSD, depression, and anxiety, which increase the risk of substance use. Moreover, trauma can alter brain function, impacting impulse control and decision-making, making individuals more vulnerable to addiction. For instance, someone who experienced childhood abuse might use drugs or alcohol to numb emotional pain or avoid painful memories. It’s critical to address the underlying trauma through trauma-informed care, which involves creating a safe and supportive therapeutic environment and utilizing trauma-specific therapies, such as EMDR or trauma-focused CBT, alongside substance use treatment. Ignoring the trauma will likely hinder recovery efforts.
Q 25. How do you stay updated on current best practices in substance use prevention and treatment?
Staying current in this rapidly evolving field is crucial. I utilize several strategies to maintain my expertise:
Professional Organizations: Active membership in organizations like the Substance Abuse and Mental Health Services Administration (SAMHSA) provides access to the latest research, guidelines, and best practices.
Conferences and Workshops: Attending conferences and workshops allows me to network with colleagues and learn about innovative treatment approaches.
Peer-Reviewed Journals: Regularly reviewing peer-reviewed journals like the Journal of Substance Abuse Treatment keeps me updated on current research findings.
Continuing Education: I dedicate time to completing continuing education courses to maintain my certification and enhance my knowledge of emerging treatment methods.
Q 26. Describe a time you had to adapt your approach to meet a client’s specific needs.
I once worked with a client who was resistant to traditional group therapy due to severe social anxiety. My initial approach, which involved encouraging participation in group sessions, proved ineffective. Recognizing this, I adapted my strategy. I began with individual sessions focusing on building trust and addressing her anxiety. Gradually, I introduced her to the group setting, starting with brief introductory sessions and offering her choices and control throughout the process. Eventually, she felt comfortable participating fully, and we observed significant improvement in both her social skills and her substance use.
Q 27. What are your strengths and weaknesses in working with individuals struggling with addiction?
Strengths: I possess strong interpersonal skills, allowing me to build rapport and trust with clients. My experience with a variety of therapeutic modalities allows me to tailor treatment plans to individual needs. I am also adept at crisis management and de-escalation techniques. I am empathetic, patient, and persistent in helping clients achieve their recovery goals.
Weaknesses: Like any professional, I am continually working on enhancing my skills. Sometimes, maintaining professional boundaries while empathizing deeply with clients can be challenging. I actively participate in supervision to manage this aspect and ensure the best outcomes for clients.
Q 28. How do you handle challenging situations or difficult clients?
Handling challenging situations and difficult clients requires a multifaceted approach.
De-escalation Techniques: I use active listening and calm, reassuring language to de-escalate tense situations. Maintaining a non-judgmental stance is critical. I focus on understanding the client’s perspective and addressing their immediate concerns.
Boundary Setting: Clear and consistent boundaries are essential. I communicate expectations calmly but firmly. For instance, if a client is verbally abusive, I will state clearly that such behavior is unacceptable and may result in the termination of the session.
Collaboration and Consultation: If I am struggling to manage a client’s behavior or needs, I don’t hesitate to seek consultation from colleagues or supervisors. Collaboration with other professionals, including psychiatrists and social workers, is often crucial in complex cases.
Self-Care: Working with individuals struggling with addiction can be emotionally demanding. Prioritizing self-care through stress management techniques and regular supervision helps me maintain professional boundaries and avoid burnout.
Key Topics to Learn for Substance Use Prevention and Control Interview
- Understanding Substance Use Disorders: Develop a strong grasp of the diagnostic criteria, different types of substance use disorders, and their impact on individuals and communities. Consider the biological, psychological, and social factors contributing to addiction.
- Prevention Strategies: Explore evidence-based prevention programs targeting various age groups and populations. Understand the principles of universal, selective, and indicated prevention and their practical application in diverse settings.
- Intervention and Treatment Approaches: Familiarize yourself with various treatment modalities, including behavioral therapies (CBT, motivational interviewing), medication-assisted treatment, and harm reduction strategies. Understand the importance of evidence-based practices and culturally sensitive approaches.
- Community-Based Programs and Collaboration: Learn about the role of community partnerships, collaboration with stakeholders (healthcare providers, law enforcement, social services), and the importance of community-level interventions in addressing substance use issues.
- Data Analysis and Program Evaluation: Understand how to collect, analyze, and interpret data related to substance use prevention and control efforts. Familiarity with epidemiological data and program evaluation methods is crucial.
- Policy and Advocacy: Develop an understanding of relevant policies, legislation, and advocacy strategies related to substance use prevention and control at local, state, and national levels.
- Ethical Considerations: Explore the ethical challenges and considerations related to providing services to individuals with substance use disorders, including confidentiality, informed consent, and cultural competency.
Next Steps
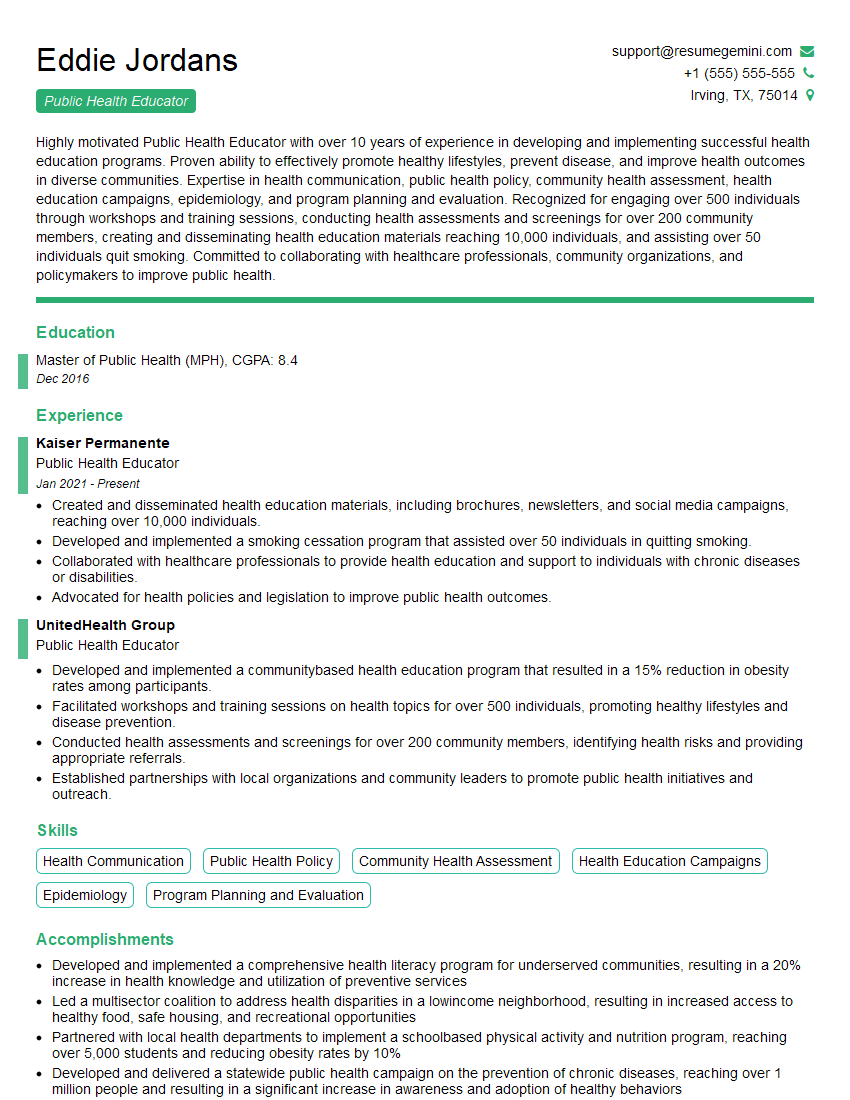
Mastering Substance Use Prevention and Control opens doors to rewarding careers with significant societal impact. To stand out, a well-crafted resume is essential. An ATS-friendly resume ensures your qualifications are effectively communicated to hiring managers. ResumeGemini is a trusted resource to help you build a compelling and professional resume that highlights your skills and experience. ResumeGemini provides examples of resumes tailored to Substance Use Prevention and Control, giving you a head start in crafting your application materials. Invest the time to build a strong resume – it’s your key to unlocking career success in this vital field.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.