Are you ready to stand out in your next interview? Understanding and preparing for Development and Implementation of Treatment Plans interview questions is a game-changer. In this blog, we’ve compiled key questions and expert advice to help you showcase your skills with confidence and precision. Let’s get started on your journey to acing the interview.
Questions Asked in Development and Implementation of Treatment Plans Interview
Q 1. Describe your experience in developing individualized treatment plans.
Developing individualized treatment plans requires a deep understanding of the patient’s unique needs, goals, and circumstances. It’s not a one-size-fits-all approach. My process begins with a thorough assessment, gathering information from various sources – the patient themselves, family members, medical records, and relevant psychological tests. This assessment informs the identification of the problem(s), the setting of realistic and measurable goals, and the selection of appropriate interventions. For example, if working with a patient struggling with anxiety, the assessment would explore the triggers, the severity of symptoms, the patient’s coping mechanisms, and their personal preferences. Based on this, the plan might include cognitive behavioral therapy (CBT), relaxation techniques, medication management (if appropriate), and a support network. Each plan is a dynamic document, regularly reviewed and adapted as needed.
I also consider the patient’s strengths and resources. This is crucial because incorporating their strengths into the treatment process increases engagement and promotes a sense of empowerment. The final plan outlines specific, measurable, achievable, relevant, and time-bound (SMART) goals, ensuring clarity and facilitating progress tracking.
Q 2. Explain the process you follow when implementing a treatment plan.
Implementing a treatment plan involves a structured and collaborative process. First, I ensure the patient fully understands the plan, their role, and the expected outcomes. This involves clear communication, using simple language and avoiding jargon. Then, we work together to schedule sessions and tasks, considering the patient’s availability and preferences. Regular check-ins are crucial to monitor progress, address any challenges, and provide support and encouragement. I use various methods depending on the patient and plan – individual therapy sessions, group therapy, homework assignments, phone calls, and online platforms for communication and resource sharing. For instance, if the plan involves exposure therapy for a phobia, we would gradually introduce the feared stimulus, starting with less anxiety-provoking situations and building up to more challenging ones. Throughout the implementation, I regularly document the patient’s progress, noting successes, challenges, and adjustments made to the plan.
Q 3. How do you ensure treatment plans align with evidence-based practices?
Aligning treatment plans with evidence-based practices is paramount. This involves staying updated with the latest research and clinical guidelines. I regularly consult peer-reviewed journals, professional organizations’ recommendations (e.g., APA, NIMH), and reputable online databases like PubMed to ensure that the interventions I select are supported by robust scientific evidence. For example, when treating depression, I would prioritize evidence-based approaches like CBT or interpersonal therapy over less researched or unproven methods. Additionally, I always consider the specific evidence base relevant to the individual patient’s diagnosis and unique circumstances. The best treatment is not just scientifically supported but also suitable for the individual.
Q 4. What strategies do you use to monitor and evaluate treatment plan effectiveness?
Monitoring and evaluating treatment plan effectiveness is an ongoing process, not a one-time event. I use a variety of methods, including regular assessments, progress tracking using standardized measures (e.g., symptom rating scales), and ongoing feedback from the patient. For instance, if treating PTSD, I might use the PCL-5 (PTSD Checklist for DSM-5) to quantitatively track symptom reduction. Qualitative data, such as patient self-reports and observations during therapy sessions, are also critical. Regular sessions provide opportunities to discuss progress, identify obstacles, and make necessary adjustments. Furthermore, I utilize data visualization techniques to graphically represent progress over time, providing a clear picture of the treatment’s effectiveness and allowing for timely adjustments. If the treatment isn’t producing the desired outcomes, I actively explore alternative approaches or refer the patient to a specialist.
Q 5. How do you adapt treatment plans based on patient progress and feedback?
Adapting treatment plans based on patient progress and feedback is crucial for optimal outcomes. Regular monitoring allows for the identification of areas where the plan needs adjustment. For example, if a patient is struggling with a specific aspect of the plan, we collaboratively explore alternative approaches. If the initial goals are not being met, we might re-evaluate the goals, adjust the interventions, or introduce new strategies. Patient feedback is invaluable. I encourage open communication, actively listening to their concerns, suggestions, and perspectives. This collaborative approach increases patient engagement and commitment to the treatment process. For instance, if a patient finds a particular exercise too challenging, we explore modifications or alternative methods to achieve similar results.
Q 6. Explain your approach to collaborating with interdisciplinary teams on treatment plans.
Collaboration with interdisciplinary teams is vital, especially for patients with complex needs. I believe in a team-based approach, fostering open communication and shared decision-making. This involves regular meetings with other professionals (e.g., psychiatrists, physicians, social workers, case managers), sharing information, coordinating interventions, and ensuring a holistic approach to patient care. Effective communication is achieved through regular meetings, shared electronic medical records, and transparent communication channels. For example, when working with a patient with both a mental health and a physical health challenge, I would coordinate with the patient’s physician to ensure the treatment plans are complementary and avoid potential drug interactions. The ultimate goal is to create a unified treatment strategy that maximizes the patient’s well-being.
Q 7. Describe a situation where you had to modify a treatment plan due to unforeseen circumstances.
In one case, I was working with a patient undergoing CBT for social anxiety. The treatment plan involved gradual exposure to social situations. However, the patient experienced a sudden and unexpected family emergency that significantly impacted their ability to engage in these activities. We needed to modify the plan immediately. Instead of focusing on structured exposures, we prioritized emotional support and coping skills to address the immediate stress. We also incorporated techniques to manage the trauma resulting from the family crisis. Once the acute phase had passed, we gradually re-introduced the exposure exercises, adapting the plan to accommodate the patient’s emotional state and capacity. The situation highlighted the importance of flexibility and adaptability in treatment planning and the need to maintain close contact with patients to respond effectively to unforeseen circumstances.
Q 8. How do you handle challenges in treatment plan adherence?
Addressing treatment plan adherence challenges requires a multifaceted approach. It’s not simply about providing instructions; it’s about building a collaborative relationship with the patient and understanding their unique circumstances. I begin by ensuring the patient fully understands the plan, using clear, non-medical language where possible, and tailoring it to their lifestyle. For instance, if a patient struggles with medication adherence, I’ll explore the reasons behind it – are there side effects? Cost issues? Forgetfulness?
Then, I implement strategies to address these issues. This might include using pill organizers, setting medication reminders on their phone, connecting them with support groups, or adjusting the treatment plan itself to minimize side effects. Regular follow-up appointments, where we review progress and address any concerns, are crucial. Furthermore, I actively involve family or caregivers when appropriate, ensuring they understand their role in supporting adherence. Finally, I utilize motivational interviewing techniques to empower patients to take ownership of their treatment. I believe success hinges on open communication and a collaborative spirit.
Q 9. What methods do you use to track patient progress and outcomes related to the treatment plan?
Tracking patient progress and outcomes is paramount. I employ a combination of methods, beginning with regular assessments using standardized questionnaires and clinical evaluations relevant to the specific condition being treated. For example, in managing depression, I might use the PHQ-9 to monitor symptom severity. The data is meticulously documented in the EHR. I also actively seek patient feedback on their perceived progress and any challenges they are facing. Beyond self-reported data, I integrate objective measures when available, such as physiological data (e.g., blood pressure for hypertension) or performance-based assessments (e.g., cognitive tests for cognitive rehabilitation). This ensures a holistic view of progress. The data is analyzed regularly to gauge effectiveness and make necessary adjustments to the treatment plan. This iterative process ensures we’re constantly optimizing treatment based on real-time outcomes.
Q 10. How do you ensure patient understanding and engagement in the treatment plan?
Ensuring patient understanding and engagement is the cornerstone of successful treatment. I start by using plain language, avoiding medical jargon, and explaining the rationale behind each component of the plan. I actively listen to their concerns and questions, making sure they feel comfortable asking anything. Visual aids, such as diagrams or infographics, can be extremely helpful, particularly for explaining complex medical concepts. Involving patients in the decision-making process empowers them and increases their buy-in. For example, I might present different treatment options and discuss the pros and cons of each with them, allowing them to choose the approach that best fits their preferences and lifestyle. Finally, celebrating small victories and acknowledging challenges helps maintain motivation and build a strong therapeutic alliance.
Q 11. How familiar are you with different treatment modalities and their applications?
I am familiar with a wide range of treatment modalities, including but not limited to cognitive-behavioral therapy (CBT), dialectical behavior therapy (DBT), psychodynamic therapy, mindfulness-based stress reduction (MBSR), medication management, and various rehabilitative techniques depending on the patient’s specific needs. My understanding extends to the appropriate application of each modality, considering factors such as the patient’s diagnosis, severity of symptoms, personal preferences, and comorbid conditions. For example, CBT is highly effective for anxiety disorders, while DBT is often used for borderline personality disorder. I understand the limitations of each approach and would not hesitate to consult with other specialists or recommend alternative treatments if necessary. I constantly update my knowledge by participating in professional development activities and staying current with the latest research.
Q 12. Describe your experience using electronic health records (EHRs) for treatment planning and documentation.
I am proficient in using electronic health records (EHRs) for treatment planning and documentation. I utilize the EHR to create comprehensive treatment plans, including patient demographics, diagnostic information, treatment goals, interventions, and progress notes. The EHR allows for efficient documentation, ensuring a clear and concise record of patient care. I use the EHR’s features for scheduling appointments, managing medication lists, generating reports, and tracking key metrics to monitor treatment outcomes. Furthermore, I leverage the EHR’s capabilities for secure communication with patients and other healthcare professionals involved in their care, promoting collaboration and continuity of care. My experience includes using various EHR systems, adapting quickly to different platforms and maximizing their functionalities.
Q 13. How do you prioritize tasks and manage time effectively when implementing multiple treatment plans?
Managing multiple treatment plans requires effective prioritization and time management. I employ several strategies, including utilizing time-blocking techniques to allocate specific time slots for individual patients and tasks. I prioritize patients based on urgency and clinical need, giving priority to those with the most immediate and severe needs. Delegation, when appropriate, helps optimize workflow. Regularly reviewing my schedule and adjusting it as needed is essential. I utilize technology like appointment scheduling software and EHR reminders to enhance efficiency and reduce the risk of missed appointments or overlooked tasks. Finally, consistent self-reflection on time management helps identify areas for improvement and refine my strategies over time. This is similar to project management, breaking down large tasks into smaller, manageable pieces.
Q 14. How do you handle situations where a treatment plan is not yielding desired results?
When a treatment plan isn’t yielding desired results, a systematic approach is crucial. I begin by carefully reviewing the treatment plan, considering whether the goals are realistic and appropriately tailored to the patient’s needs. I re-evaluate the diagnosis and assess whether additional testing or consultation is necessary. I analyze the data gathered through progress monitoring to pinpoint areas where the plan is falling short. Is the patient adhering to the plan? Are there unforeseen obstacles? Are there alternative interventions or modifications to the plan that might be more effective? Open communication with the patient is vital; I discuss my findings and collaborate with them to identify the reasons for the lack of progress and to develop a revised plan. Sometimes, referring the patient to another specialist or seeking a second opinion is necessary. The goal is to remain flexible and adapt to the patient’s changing needs, continuously optimizing the treatment strategy to achieve the best possible outcomes.
Q 15. What is your understanding of patient confidentiality and HIPAA regulations?
Patient confidentiality is paramount in healthcare. It’s the ethical and legal obligation to protect sensitive patient information. HIPAA (Health Insurance Portability and Accountability Act) is the US law that sets the standards for protecting the privacy and security of Protected Health Information (PHI). PHI includes any individually identifiable health information, such as medical records, diagnoses, treatment plans, and billing information.
My understanding of HIPAA encompasses its key provisions, including the Privacy Rule, Security Rule, and Breach Notification Rule. The Privacy Rule dictates how PHI can be used, disclosed, and protected. The Security Rule outlines administrative, physical, and technical safeguards to ensure the confidentiality, integrity, and availability of electronic PHI. The Breach Notification Rule mandates reporting of any unauthorized disclosures of PHI.
In practice, this means I adhere strictly to HIPAA regulations by obtaining proper authorizations before disclosing information, using secure methods for communication and storage of patient data, and maintaining a strict code of conduct regarding the handling of sensitive patient information. For example, I would never discuss a patient’s case with anyone not directly involved in their care, and I would ensure all electronic records are password-protected and accessed only through secure networks.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Explain your experience in developing treatment plans for specific populations (e.g., geriatric, pediatric).
I have extensive experience developing treatment plans for diverse populations, including geriatric and pediatric patients. Working with geriatric patients requires a keen understanding of age-related physiological changes and potential comorbidities. For example, a treatment plan for a geriatric patient with osteoarthritis would focus on pain management, physical therapy tailored to their mobility limitations, and potentially medication adjustments considering potential drug interactions with other medications they might be taking.
With pediatric patients, the treatment plans are adapted to their developmental stage and cognitive abilities. For instance, a treatment plan for a child with ADHD might incorporate behavioral therapy techniques alongside medication, with careful consideration of the child’s age and understanding. The communication strategies would drastically differ from those used for an adult. Parent/guardian involvement is also crucial in the pediatric population.
In both cases, I collaborate closely with the interdisciplinary team, including physicians, nurses, therapists, and social workers to create comprehensive and individualized plans. Each plan includes clearly defined goals, measurable objectives, and a timeline for achieving those objectives. Regular reviews and adjustments are essential to ensure the effectiveness of the treatment.
Q 17. How do you measure the success of a treatment plan?
Measuring the success of a treatment plan is a multifaceted process. It’s not solely about achieving a specific outcome but also about the overall impact on the patient’s well-being. I use a combination of quantitative and qualitative measures.
Quantitative measures might include tracking changes in vital signs, lab results, functional abilities (using standardized scales), or symptom scores. For example, monitoring a patient’s blood pressure after implementing a hypertension treatment plan, or tracking a child’s attention span following ADHD treatment. Qualitative measures involve gathering data through patient interviews, observations of behavior, and feedback from caregivers or family members. This provides a holistic view of the patient’s progress beyond just numbers.
Ultimately, successful treatment plans lead to improved patient outcomes, a higher quality of life, and enhanced patient satisfaction. The success is evaluated by comparing the patient’s initial status with their status after the implementation of the treatment plan. Regular monitoring allows for adjustments to ensure the plan remains effective and aligned with the patient’s needs.
Q 18. What are some common challenges encountered in implementing treatment plans, and how do you address them?
Implementing treatment plans often presents challenges. Patient non-adherence is a common issue, particularly with long-term plans or those requiring significant lifestyle changes. Lack of resources, such as financial constraints or limited access to healthcare services, can also impede implementation.
Other challenges include the complexity of co-morbidities, unexpected adverse effects of medications, and changes in the patient’s condition. To address these, I employ several strategies. I prioritize patient education and shared decision-making to foster adherence. Collaboration with social workers and other support systems helps address resource limitations. Regular monitoring and adjustments to the treatment plan, based on the patient’s response, are crucial. I also engage in open communication to discuss challenges and find solutions collaboratively with the patient and their support system.
For instance, if a patient isn’t adhering to their medication regimen, I might explore the reasons behind this, such as side effects, cost, or forgetfulness. I’ll then adapt the plan – perhaps suggesting a different medication, exploring financial assistance programs, or creating a medication reminder system. Flexibility and a proactive approach are essential to navigate these challenges.
Q 19. Describe your experience using data to inform treatment plan development and adjustments.
Data plays a critical role in informing treatment plan development and adjustments. I utilize data from various sources, including electronic health records (EHRs), patient-reported outcome measures (PROMs), and clinical assessments. This data helps me understand the patient’s baseline condition, track their progress over time, and identify areas requiring modification.
For example, if I’m developing a treatment plan for diabetes, I would analyze the patient’s blood glucose levels, HbA1c levels, weight, and other relevant data to establish their baseline and tailor the plan accordingly. Ongoing monitoring allows me to assess the effectiveness of the interventions and adjust the plan as needed based on the collected data. Data analytics tools can help identify patterns and trends, potentially leading to improved outcomes for a larger patient population. This data-driven approach enhances the precision and effectiveness of treatment.
I am proficient in using various software and databases to collect, analyze, and interpret this data. This allows me to continuously evaluate the plan’s effectiveness and make evidence-based adjustments to optimize outcomes.
Q 20. How do you communicate treatment plan details effectively to patients and their families?
Effective communication is crucial. I employ a patient-centered approach, ensuring information is presented in a clear, concise, and easily understandable manner, tailoring my language and approach to the patient’s educational level and cultural background. I use plain language, avoiding medical jargon unless absolutely necessary, and I encourage patients to ask questions.
When communicating with families, I involve them as active participants in the process, respecting their input and concerns. I provide opportunities for questions and discussion, fostering a collaborative environment. Visual aids, such as diagrams or flowcharts, can also significantly enhance understanding. Written summaries of treatment plans, in addition to verbal explanations, ensure everyone has access to the information and can refer to it later.
I ensure that all communication, whether verbal or written, is documented appropriately in the patient’s medical record to maintain a clear and comprehensive history of the treatment process.
Q 21. What are your preferred methods for documenting treatment progress and outcomes?
I utilize a combination of methods for documenting treatment progress and outcomes. Electronic health records (EHRs) are the primary means, ensuring timely, secure, and readily accessible documentation. Within the EHR, I meticulously record initial assessments, treatment goals, interventions implemented, patient responses, and any modifications to the plan.
In addition to EHRs, I may use standardized assessment tools, such as questionnaires or scales, to quantify specific aspects of the patient’s progress. These provide objective data to complement the narrative notes in the EHR. Progress notes are written regularly, reflecting the patient’s response to treatment, any challenges encountered, and adjustments made to the plan. The final documentation includes a summary of the treatment process, the achieved outcomes, and any recommendations for ongoing care.
Maintaining accurate and comprehensive documentation is essential for continuity of care, communication with other healthcare providers, and legal compliance.
Q 22. How do you stay current with best practices and new developments in treatment planning?
Staying current in the dynamic field of treatment planning requires a multifaceted approach. It’s not enough to simply rely on initial training; continuous learning is crucial. I actively engage in several strategies to ensure I’m utilizing best practices and incorporating the latest advancements.
Professional Development: I regularly attend conferences, workshops, and webinars focusing on evidence-based practices in my area of expertise. These events provide opportunities to network with peers and learn about innovative techniques from leading experts. For example, recently I attended a conference on trauma-informed care, which significantly impacted my approach to working with clients who have experienced trauma.
Professional Journals and Publications: I subscribe to and regularly review reputable journals like the Journal of Consulting and Clinical Psychology and the American Journal of Psychiatry. These publications keep me abreast of the latest research findings and emerging treatment modalities.
Continuing Education Units (CEUs): I actively pursue CEUs to maintain my professional licensure and expand my knowledge base. This ensures I am compliant with regulations and consistently updating my skills.
Mentorship and Peer Consultation: I actively seek out mentorship opportunities from experienced professionals and participate in peer consultation groups. These interactions offer invaluable insights and allow for the sharing of best practices and challenges faced in clinical settings.
This combination of formal and informal learning allows me to adapt my treatment planning approaches to reflect the most current and effective methods.
Q 23. Describe your experience in developing and implementing crisis intervention plans.
Developing and implementing crisis intervention plans requires a structured and proactive approach. My experience involves collaborating with clients, families, and other professionals to create personalized plans that address individual needs and potential triggers.
I begin by conducting a thorough assessment of the client’s history, identifying potential risk factors and triggers that might precipitate a crisis. This involves exploring past crisis episodes, current stressors, and coping mechanisms. For example, a client with a history of substance abuse might have a crisis plan that includes contact information for support groups and detoxification facilities.
The plan itself outlines specific steps to be taken during a crisis. This typically includes:
- Warning signs: Identifying early indicators of escalating distress.
- De-escalation techniques: Strategies to calm the individual, such as deep breathing exercises or grounding techniques.
- Emergency contacts: A list of individuals (family, friends, therapists, crisis hotlines) who can provide immediate support.
- Safe place: Identifying a safe and calming environment where the individual can retreat during a crisis.
- Professional intervention: Procedures for contacting emergency services or mental health professionals if the situation escalates beyond self-management capabilities.
After creating the plan, I work with the client to practice implementing it. This ensures they feel comfortable and confident using the plan during an actual crisis. Regular review and updating of the crisis plan are essential to adapt to the client’s changing needs and circumstances.
Q 24. How do you integrate family and caregiver involvement into treatment plans?
Family and caregiver involvement is paramount for successful treatment outcomes. Their insights, support, and collaboration are invaluable in creating and implementing effective treatment plans. I actively incorporate their participation through several strategies.
Initial Assessment: I conduct a thorough assessment involving family members or caregivers, gathering their perspective on the client’s challenges, strengths, and history. This helps build a holistic understanding of the situation.
Shared Decision-Making: I actively involve them in the development of the treatment plan, ensuring they feel heard and understood. This includes discussing goals, interventions, and expectations. For example, family therapy sessions may be included to address relational dynamics impacting the client’s progress.
Collaboration and Communication: I maintain open communication with family and caregivers, providing regular updates on the client’s progress, challenges, and any adjustments to the treatment plan. This collaborative approach fosters trust and builds a stronger therapeutic alliance.
Education and Support: I provide education on the client’s condition, treatment modalities, and coping strategies. This equips family members with the knowledge and skills they need to support their loved one effectively. I may also connect them with support groups or other resources.
By valuing and integrating their perspectives, I create a supportive network around the client, significantly increasing the chances of successful treatment implementation and long-term well-being.
Q 25. What ethical considerations are involved in treatment plan development and implementation?
Ethical considerations are central to treatment planning and implementation. Maintaining client confidentiality, respecting autonomy, and ensuring beneficence are fundamental principles.
Confidentiality: I adhere strictly to HIPAA regulations and other relevant privacy laws, safeguarding client information from unauthorized access. Discussions regarding treatment plans are held in confidential settings.
Informed Consent: I ensure clients are fully informed about the treatment plan, including potential benefits, risks, and alternatives. This includes obtaining their informed consent before proceeding with any intervention. This process is particularly crucial when dealing with vulnerable populations or those with diminished capacity.
Beneficence and Non-maleficence: My primary goal is to benefit the client and avoid causing harm. Treatment plans are carefully tailored to the individual’s specific needs and circumstances, while considering potential risks and side effects. I prioritize interventions that are evidence-based and safe.
Justice and Fairness: I strive to provide equitable and unbiased care to all clients, regardless of their background, race, gender, or socioeconomic status. I am aware of potential biases and actively work to mitigate their influence on my treatment decisions.
Autonomy: I empower clients to make informed decisions about their treatment. While I offer guidance and recommendations, the final decision rests with the client.
Addressing these ethical considerations ensures that treatment is provided in a responsible, compassionate, and legally compliant manner.
Q 26. How do you ensure cultural sensitivity in treatment planning?
Cultural sensitivity is crucial in treatment planning. Ignoring cultural differences can lead to ineffective interventions and even cause harm. I ensure cultural sensitivity by:
Cultural Assessment: I conduct a thorough cultural assessment at the beginning of treatment, exploring the client’s cultural background, beliefs, values, and practices. This includes their understanding of mental health, their preferred communication styles, and their social support networks.
Culturally Adapted Interventions: I tailor treatment approaches to align with the client’s cultural context. This may involve incorporating traditional healing practices, adapting therapeutic techniques, or modifying communication styles. For example, incorporating family members into the treatment process might be crucial in some cultures while counterproductive in others.
Language Access: I ensure that clients have access to interpreters or other language support services if needed. Effective communication is crucial for building a therapeutic alliance and achieving positive outcomes.
Cultural Humility: I approach treatment with a spirit of humility, acknowledging that my understanding of culture is limited and continuously learning. I actively seek feedback from clients about their experiences and adjust my approach accordingly.
Collaboration with Cultural Experts: When necessary, I consult with cultural experts or community leaders to gain a deeper understanding of specific cultural contexts and best practices.
By prioritizing cultural sensitivity, I create a safe and comfortable therapeutic environment where clients feel understood, respected, and empowered to engage in treatment.
Q 27. How do you utilize technology to enhance treatment plan effectiveness?
Technology offers numerous opportunities to enhance treatment plan effectiveness. I utilize various technological tools to improve accessibility, engagement, and monitoring of progress.
Telehealth: I utilize telehealth platforms to provide convenient and accessible treatment options, especially beneficial for clients in remote areas or with mobility challenges. This allows for consistent sessions and reduces barriers to care.
Electronic Health Records (EHRs): EHRs streamline documentation, improve information sharing among healthcare providers, and enhance the overall organization of client data, reducing administrative burden and ensuring timely access to information.
Mobile Apps: I may recommend or utilize mobile applications for tracking mood, sleep patterns, medication adherence, or engaging in therapeutic exercises. These apps provide valuable data that informs treatment decisions and enhances client self-monitoring.
Online Resources and Educational Materials: I share relevant online resources and educational materials with clients to supplement treatment sessions. This empowers them to actively participate in their own care and supports self-management.
Data Analytics: EHR systems and mobile apps provide data that can be analyzed to track progress, identify patterns, and adjust treatment strategies as needed. This data-driven approach ensures treatment remains effective and targeted.
However, it’s crucial to maintain ethical considerations surrounding data privacy and security when employing technology in treatment planning. Informed consent regarding data collection and usage is always obtained.
Key Topics to Learn for Development and Implementation of Treatment Plans Interview
- Assessment and Diagnosis: Understanding the process of gathering comprehensive client information, conducting thorough assessments, and formulating accurate diagnoses based on established criteria. This includes familiarity with various assessment tools and their limitations.
- Treatment Planning Principles: Mastering the theoretical frameworks underpinning effective treatment planning, such as the biopsychosocial model and evidence-based practices. This involves understanding how to establish measurable goals, select appropriate interventions, and develop a plan that is culturally sensitive and client-centered.
- Intervention Selection and Rationale: Justifying the choice of specific therapeutic interventions based on the client’s needs, diagnosis, and research-supported efficacy. This includes understanding the strengths and limitations of various therapeutic modalities and how to tailor them to individual situations.
- Implementation and Monitoring: Knowing how to effectively implement the treatment plan, including session structure, techniques, and documentation. This also emphasizes the crucial role of ongoing monitoring, progress evaluation, and plan modification as needed based on client response and feedback.
- Collaboration and Ethical Considerations: Understanding the importance of teamwork and collaboration with other professionals involved in the client’s care. This includes adhering to ethical guidelines, maintaining client confidentiality, and navigating potential conflicts of interest.
- Documentation and Record Keeping: Mastering the skills of accurate, concise, and legally compliant documentation of all aspects of the treatment process. This ensures continuity of care and accountability.
- Case Conceptualization: Developing a comprehensive understanding of the client’s presenting problem, integrating various factors contributing to their difficulties, and formulating a coherent explanation to guide treatment.
- Outcome Measurement and Evaluation: Understanding the importance of measuring treatment outcomes, employing appropriate evaluation methods, and using data to inform ongoing treatment decisions and demonstrate effectiveness.
Next Steps
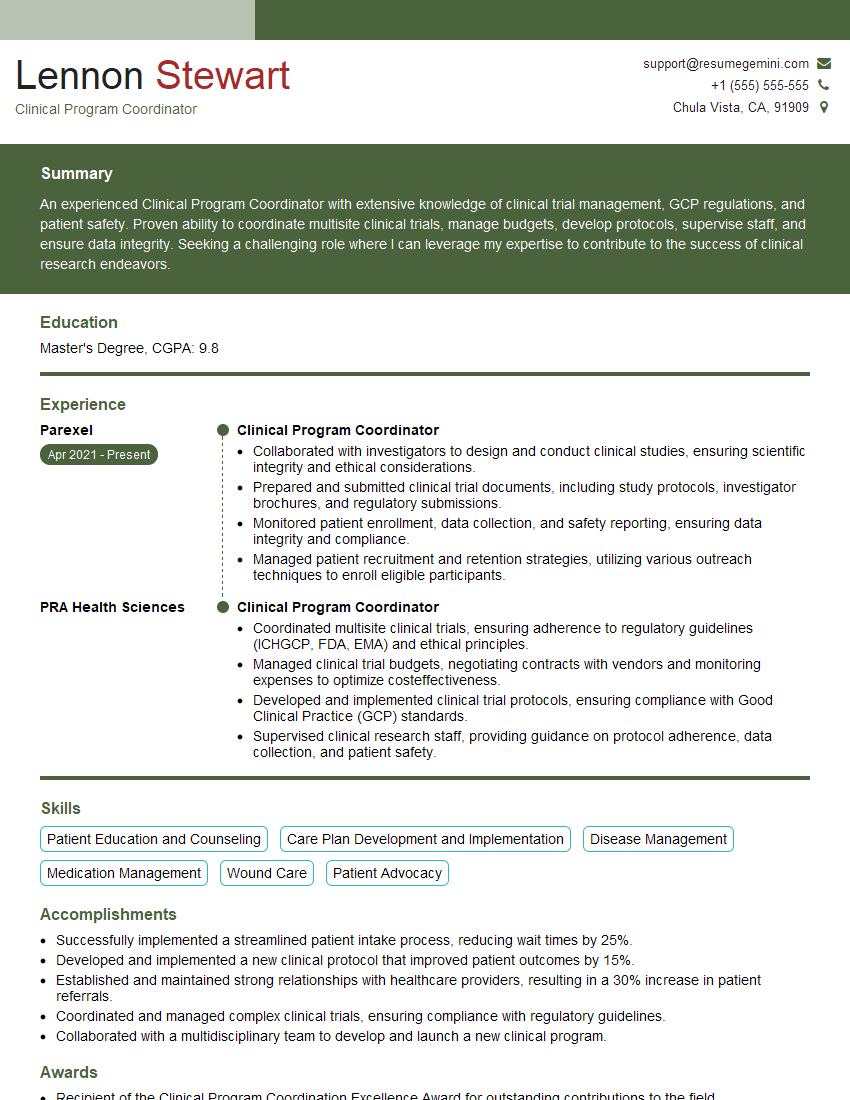
Mastering the development and implementation of treatment plans is crucial for career advancement in this field. It demonstrates a deep understanding of clinical practice and enhances your ability to provide effective and ethical care. To increase your job prospects, creating a strong, ATS-friendly resume is essential. ResumeGemini is a trusted resource that can help you build a professional resume that highlights your skills and experience effectively. Examples of resumes tailored to Development and Implementation of Treatment Plans are available to help you get started.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
To the interviewgemini.com Webmaster.
Very helpful and content specific questions to help prepare me for my interview!
Thank you
To the interviewgemini.com Webmaster.
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.