Cracking a skill-specific interview, like one for Ultrasound Image Examination, requires understanding the nuances of the role. In this blog, we present the questions you’re most likely to encounter, along with insights into how to answer them effectively. Let’s ensure you’re ready to make a strong impression.
Questions Asked in Ultrasound Image Examination Interview
Q 1. Describe the principles of ultrasound image formation.
Ultrasound image formation relies on the principle of echolocation, similar to how bats navigate. A transducer sends high-frequency sound waves (ultrasound) into the body. These waves travel through tissues, reflecting at boundaries between tissues with differing acoustic impedance (the resistance to sound wave propagation). The reflected waves (echoes) are detected by the same transducer. The time it takes for the echoes to return and their intensity are used to create an image.
The machine calculates the distance to the reflecting interfaces based on the time of flight of the ultrasound wave. Stronger reflections appear brighter on the image, representing interfaces with significant impedance differences (like bone and soft tissue). Weaker reflections appear darker.
Think of it like shining a flashlight in a dark room: the light reflects off objects and the intensity and time it takes for the light to return determine how bright and how far away the objects are perceived. Ultrasound uses sound instead of light, and the resulting image is a representation of the sound wave reflections.
Q 2. Explain the difference between A-mode, B-mode, M-mode, and Doppler ultrasound.
Ultrasound imaging offers several display modes:
- A-mode (Amplitude mode): Displays the amplitude of returning echoes as a function of depth. It shows a series of spikes, each representing a reflection; primarily used for precise depth measurements, less common in modern practice.
- B-mode (Brightness mode): Displays the amplitude of returning echoes as brightness variations on a grayscale image. This is the most common mode and produces the familiar two-dimensional cross-sectional images we associate with ultrasound.
- M-mode (Motion mode): Displays the amplitude of returning echoes from a single line over time. Used to assess the movement of structures, like heart valves or fetal heartbeats. Think of it as a ‘moving A-mode’; the image shows a series of parallel lines showing movement over time.
- Doppler ultrasound: Measures the velocity and direction of blood flow or other moving tissues within the body. This is done by analyzing the frequency shift of the reflected ultrasound waves due to the Doppler effect (change in frequency due to relative motion between the source and receiver). Doppler ultrasound is invaluable in assessing blood flow in arteries and veins, identifying blockages, and assessing cardiac function.
In essence, they represent different ways of processing and displaying the same underlying echo data.
Q 3. What are the various types of ultrasound transducers and their applications?
Ultrasound transducers come in various forms, each suited for specific applications:
- Linear array transducers: Produce rectangular images with excellent resolution, commonly used for superficial structures (e.g., skin, muscles, breast, thyroid). They provide good detail in the near field and have a relatively narrow field of view.
- Curvilinear array transducers: Produce sector-shaped images, ideal for deeper structures (e.g., abdominal organs, pregnant uterus). They have a wider field of view than linear transducers.
- Phased array transducers: Also produce sector-shaped images, commonly used for cardiac imaging (echocardiography). They offer excellent temporal resolution, allowing for real-time visualization of moving structures.
- Endocavity transducers: Designed for insertion into body cavities (e.g., rectum, vagina), allowing for very close-range imaging of internal organs. They provide high-resolution images in a limited area.
- Transesophageal echocardiography (TEE) probes: A specialized type of phased array probe inserted into the esophagus to obtain images of the heart from a different perspective than standard echocardiography.
The choice of transducer depends on the specific application, depth of penetration needed, and desired image resolution.
Q 4. How do you adjust the gain, depth, and frequency settings on an ultrasound machine?
Adjusting the ultrasound machine settings is crucial for optimizing image quality. The controls vary slightly among different ultrasound machines, but the basic principles are universal:
- Gain: Controls the amplification of the received echoes. Increasing the gain increases the brightness of the entire image; however, excessive gain can lead to noise and make interpretation difficult. Think of it as adjusting the volume – too high and you get distortion, too low and you miss important signals.
- Depth: Determines the imaging depth. Increasing the depth allows visualization of deeper structures, but at the cost of reduced resolution. It’s like adjusting the zoom lens on a camera; increasing depth shows more, but it sacrifices the detail.
- Frequency: Higher frequencies provide better resolution but penetrate less deeply, while lower frequencies penetrate deeper but have lower resolution. A higher frequency is like using a finely detailed brush for painting a small area, while a lower frequency is like using a broader brush for covering a larger space. The selection of the frequency often depends on the part of the body examined.
Adjusting these parameters requires experience and an understanding of the anatomy being imaged. Proper settings are crucial for obtaining high-quality images suitable for accurate diagnosis.
Q 5. Describe the artifacts commonly encountered in ultrasound imaging and their causes.
Ultrasound images are sometimes affected by artifacts, which are image features not representative of true anatomy. Understanding these artifacts is essential for correct interpretation:
- Acoustic shadowing: A dark area posterior to a highly reflective structure (e.g., bone, stones). This occurs because the sound wave is mostly reflected, leaving minimal energy to penetrate deeper. Think of a very strong reflection like a mirror; no light gets through behind it.
- Acoustic enhancement: A brighter area posterior to a fluid-filled structure (e.g., cyst, gallbladder). This happens because sound waves travel faster through fluids than through tissue, resulting in increased echo intensity. The opposite of shadowing.
- Reverberation: Multiple reflections between two strongly reflective interfaces, appearing as parallel lines. Think of the echo effect between two mirrors.
- Mirror image artifact: A duplicate image of a structure displayed symmetrically on the opposite side of a strong reflector (e.g., diaphragm).
- Side lobes: Reflective signals that appear slightly away from the main signal. They are caused by sound waves that are not transmitted in the central beam. These can be mistaken as actual structures.
Recognizing and understanding these artifacts is a crucial skill for any sonographer to avoid misinterpretation.
Q 6. Explain the acoustic window concept and its importance in ultrasound examinations.
The acoustic window refers to an area of the body where sound waves can effectively penetrate to reach the target organ. It is essential because the sound waves must travel through intervening structures before reaching the organ of interest. Obstructions or areas with high acoustic impedance can significantly impede sound transmission.
For example, when imaging the liver, the intercostal spaces (spaces between ribs) offer good acoustic windows, while the ribs themselves create significant acoustic shadowing. Similarly, a full bladder provides an excellent acoustic window for imaging the pelvic organs. Therefore, choosing an appropriate acoustic window is vital for acquiring high-quality images.
The proper positioning of the transducer is key to utilizing the acoustic window effectively, allowing optimal visualization of the targeted anatomy.
Q 7. How do you assess the quality of an ultrasound image?
Assessing ultrasound image quality involves several key factors:
- Image resolution: The ability to distinguish between closely spaced structures. High resolution is important for detail and accurate diagnosis.
- Penetration depth: The ability to visualize structures at various depths. This depends on factors like frequency and the properties of the tissues being imaged.
- Noise level: The presence of unwanted signals that can obscure the actual structures. Excessive noise is often linked to insufficient signal processing or incorrect setting adjustments.
- Artifact presence: The identification and understanding of artifacts are critical for differentiating them from actual structures to avoid errors in diagnosis.
- Anatomical correctness: The image must accurately represent the anatomy being examined. This necessitates a thorough knowledge of anatomy.
Overall image quality is judged based on the clarity of the image, the visualization of the relevant anatomy, and the absence of significant artifacts that could interfere with accurate interpretation. Experienced sonographers can quickly assess image quality and adjust parameters accordingly.
Q 8. Describe the safety precautions associated with ultrasound examinations.
Ultrasound is generally considered a safe imaging modality, but precautions are essential. The primary concern is the potential for bioeffects from the ultrasound energy, although these are generally considered minimal at diagnostic intensities. The ALARA principle (As Low As Reasonably Achievable) guides our practice. This means we use the lowest possible output power needed to obtain a diagnostic image.
- Time: We minimize examination time to reduce overall exposure.
- Power: We adjust the power output to the lowest setting that still provides a clear image. We avoid unnecessary high-intensity settings.
- Thermal and Mechanical Effects: While rare at diagnostic levels, we are aware of the potential for thermal (heating) and mechanical (cavitation) effects. These are minimized by using appropriate techniques and avoiding prolonged exposure to one area.
- Patient Comfort: Ensuring patient comfort is crucial. Unnecessary pressure from the transducer can cause discomfort and should be avoided. We use gel to ensure good acoustic coupling and reduce friction.
- Infection Control: Standard infection control practices are strictly adhered to, including hand hygiene and proper transducer disinfection between patients.
For example, during a fetal ultrasound, we prioritize short scan times to minimize the fetus’s exposure. We also carefully explain the procedure to reduce patient anxiety, ensuring a relaxed environment that allows for better image acquisition.
Q 9. Explain the process of performing a Doppler ultrasound examination, including spectral analysis.
Doppler ultrasound uses the Doppler effect to measure blood flow velocity. Sound waves bounce off moving red blood cells, and the change in frequency allows us to determine the speed and direction of blood flow. This is incredibly useful in diagnosing vascular disease and assessing cardiac function.
The process involves applying a Doppler transducer to the skin, using ultrasound gel for optimal acoustic coupling. The machine then processes the returning signals to create waveforms. These waveforms are visually represented in a spectral Doppler analysis, providing information about the velocity, direction, and character of blood flow.
Spectral Analysis: This analysis shows a graph plotting blood flow velocity (y-axis) against time (x-axis). We assess several key parameters:
- Peak systolic velocity (PSV): The highest velocity during systole (heart contraction).
- End diastolic velocity (EDV): The velocity at the end of diastole (heart relaxation).
- Resistive index (RI): (PSV-EDV)/PSV, an indicator of vascular resistance.
- Pulsatility index (PI): (PSV-EDV)/mean velocity.
These parameters can help identify blockages, stenosis (narrowing), or other abnormalities in blood vessels. For example, a high resistive index in a renal artery suggests potential stenosis.
Imagine it like listening to a train’s whistle: as the train approaches, the pitch increases, and as it moves away, the pitch decreases. Similarly, Doppler ultrasound detects the change in frequency of sound waves reflecting off moving blood cells to measure their velocity.
Q 10. How do you identify and differentiate various tissue types based on their ultrasound appearance?
Different tissues have distinct acoustic properties, affecting how they appear on ultrasound images. These properties include density, elasticity, and the speed of sound within the tissue. We identify tissues based on several characteristics:
- Echogenicity: The brightness of the tissue on the ultrasound image. Hyperechoic tissues appear bright (e.g., bone, stones), hypoechoic tissues appear relatively dark (e.g., fluid), and anechoic tissues are black (e.g., water).
- Texture: The overall pattern of echoes within the tissue (e.g., homogeneous, heterogeneous).
- Borders: The sharpness or irregularity of the tissue boundaries.
- Shape: The overall shape and size of the tissue structure.
For example, a liver cyst will appear anechoic (black) with smooth borders, while a liver tumor might appear hypoechoic or hyperechoic, with irregular borders and a heterogeneous texture. We use a combination of these characteristics to differentiate between various tissue types. Experience and a thorough understanding of normal anatomy are critical for accurate interpretation.
Q 11. Describe your experience with different ultrasound modalities (e.g., abdominal, cardiac, vascular).
My experience encompasses a wide range of ultrasound modalities. I’ve performed numerous abdominal ultrasounds, focusing on the liver, gallbladder, kidneys, spleen, and pancreas, identifying various pathologies including cysts, masses, and inflammatory changes. I am also proficient in cardiac ultrasound (echocardiography), evaluating heart structure and function, including ejection fraction, valvular function, and wall motion abnormalities. In vascular ultrasound, I have extensive experience with carotid, peripheral arterial, and venous studies, identifying blockages, stenosis, and thrombi. Each modality requires specific knowledge of anatomy, physiology, and pathology, as well as technical skill in image acquisition and optimization.
For instance, in a recent case, I used Doppler ultrasound to assess a patient’s carotid arteries, identifying significant stenosis requiring intervention. In another instance, I performed a transthoracic echocardiogram to evaluate a patient with suspected heart failure, revealing reduced ejection fraction.
Q 12. How do you handle challenging situations, such as difficult patient positioning or technical malfunctions?
Challenging situations require adaptability and problem-solving skills. Difficult patient positioning might involve adjusting the examination table, using pillows or wedges for support, and communicating clearly with the patient to ensure their comfort and cooperation. For example, for patients with back pain, careful positioning and use of supportive devices are crucial for optimal image acquisition.
Technical malfunctions necessitate a systematic approach. First, I’d try basic troubleshooting steps, such as checking cable connections and transducer settings. If the problem persists, I’d escalate the issue to the biomedical engineering team for repair. In cases where a particular image is compromised, I might adjust the machine settings, transducer position, or use alternative imaging techniques to obtain a diagnostically useful image. Patient safety and delivering the best possible care are paramount; I always ensure alternative solutions are in place if necessary.
Q 13. Describe your proficiency in using different ultrasound machines and software.
I’m proficient in using various ultrasound machines from leading manufacturers, including GE, Philips, and Siemens. My experience extends to different software platforms used for image acquisition, post-processing, and image archiving. I’m adept at navigating various user interfaces and customizing settings for optimal image quality, depending on the specific clinical question and patient anatomy.
My proficiency includes using advanced tools like elastography (measuring tissue stiffness) and 3D/4D ultrasound for enhanced visualization and diagnostic accuracy. Regular training and continuing medical education keep my skills up-to-date with technological advancements in ultrasound technology.
Q 14. Explain your understanding of image optimization techniques.
Image optimization is critical for accurate diagnosis. It involves adjusting various parameters to achieve the best possible image quality. These include:
- Gain: Amplifies the received echoes, improving image brightness. Too much gain can introduce noise; too little obscures detail.
- Depth: Adjusting the depth of penetration to focus on the area of interest.
- Frequency: Higher frequencies provide better resolution but less penetration; lower frequencies offer deeper penetration but less resolution. The selection depends on the clinical need and the target tissue.
- Focus: Fine-tuning the focus to optimize image clarity in the area of interest.
- TGC (Time Gain Compensation): Compensates for the attenuation of sound waves as they travel through tissues, ensuring even brightness across the image depth.
Imagine taking a photograph – you adjust the focus, aperture, and lighting to achieve the optimal image. Similarly, in ultrasound, optimizing these parameters is essential to improve visualization and accurately assess tissue characteristics. Experience and careful assessment of the image are key to mastering these techniques.
Q 15. How do you ensure patient safety and comfort during an ultrasound exam?
Patient safety and comfort are paramount in ultrasound examinations. My approach is multifaceted, starting with a thorough explanation of the procedure. I explain the process in simple, non-medical terms, answering any questions the patient may have to alleviate anxiety. This builds trust and ensures informed consent.
During the exam, I maintain a calm and reassuring demeanor, ensuring the patient is comfortable with the positioning and the gel. I pay close attention to their verbal and nonverbal cues, adjusting the exam as needed to minimize discomfort. For example, if a patient expresses discomfort during a certain position, I will explore alternative approaches to achieve the same imaging goals. I also provide breaks as needed, allowing the patient to rest and reposition themselves. Finally, I always maintain strict infection control protocols, using sterile gel and ensuring appropriate cleaning of the equipment between patients.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Describe your experience with image documentation and reporting.
Image documentation and reporting are critical for accurate medical record-keeping and effective communication among healthcare professionals. I meticulously document each ultrasound examination, including patient demographics, the reason for the exam, the imaging protocol used, and detailed descriptions of the findings. This involves annotating images with measurements, key landmarks, and descriptions of any abnormalities detected. My reports are clear, concise, and structured using standardized terminology, ensuring easy interpretation by referring physicians.
I utilize PACS (Picture Archiving and Communication System) for efficient image storage, retrieval, and distribution. This allows for easy access to images by other healthcare providers involved in the patient’s care. I also maintain detailed quality control logs of the equipment utilized to demonstrate its proper functioning.
Q 17. Explain your understanding of the ethical considerations in ultrasound practice.
Ethical considerations are at the forefront of my ultrasound practice. Patient confidentiality is paramount; I strictly adhere to HIPAA regulations and maintain the privacy of all patient information. Informed consent is crucial; I ensure patients understand the procedure, its benefits, risks, and alternatives before proceeding with the exam. I avoid making diagnostic interpretations beyond my scope of practice and always refer findings to the appropriate specialists when necessary.
Furthermore, I maintain professional boundaries, treating all patients with respect and dignity, regardless of their background or condition. I am committed to continuing education to stay abreast of the latest advancements in ultrasound technology and ethical guidelines to ensure best practices. For example, I recently completed a course on ethical dilemmas in medical imaging.
Q 18. How do you maintain the accuracy and reliability of ultrasound equipment?
Maintaining the accuracy and reliability of ultrasound equipment is critical for accurate diagnoses. This involves a multi-pronged approach that includes regular quality assurance (QA) and quality control (QC) procedures. We perform daily QC checks, which typically include evaluating the machine’s performance parameters, image quality, and transducer functionality. This might involve using test phantoms—objects with known acoustic properties—to assess the system’s performance against established standards.
Regular preventative maintenance is also crucial. This involves scheduled servicing by qualified biomedical engineers, who conduct thorough inspections, calibrations, and repairs as needed. We meticulously maintain detailed logs of all QC and maintenance activities, ensuring compliance with regulatory guidelines and maintaining a record for traceability. Any equipment malfunction or deviations from established quality standards are immediately reported and addressed to ensure patient safety and the reliability of the imaging results.
Q 19. Describe your knowledge of relevant anatomy and physiology related to ultrasound imaging.
A strong understanding of anatomy and physiology is fundamental to performing effective ultrasound examinations. My knowledge encompasses detailed anatomical structures relevant to various ultrasound applications, such as abdominal, obstetric, and vascular imaging. For abdominal scans, I have a thorough grasp of the liver, gallbladder, kidneys, spleen, and pancreas, including their normal sonographic appearance and common variations.
In obstetrics, I am proficient in identifying fetal structures, assessing fetal growth, and diagnosing potential abnormalities. In vascular imaging, I am experienced in visualizing blood vessels, assessing blood flow, and identifying potential pathologies. My understanding of physiology allows me to interpret the ultrasound images in the context of the patient’s clinical presentation and to recognize subtle variations that might indicate underlying conditions. For example, understanding the physiological changes during pregnancy allows me to accurately assess fetal well-being. This in-depth knowledge ensures I can accurately identify anatomical structures, interpret image findings, and provide accurate and reliable reports.
Q 20. Explain your experience with quality assurance and quality control in ultrasound.
Quality assurance (QA) and quality control (QC) are integral parts of my ultrasound practice. QA encompasses the systematic monitoring of the entire ultrasound process to ensure consistent high quality, including equipment performance, image acquisition protocols, image interpretation, and report generation. QC involves the specific testing and calibration of the equipment itself.
I participate in regular QA/QC meetings, and actively contribute to the implementation of standardized protocols to ensure uniformity in image acquisition and interpretation within our department. We use various tools, such as quality control phantoms, to regularly assess equipment performance and ensure it meets established standards. We also participate in proficiency testing programs to objectively evaluate our skills and maintain competence. All of these activities help us to maintain the high quality of ultrasound services we provide and to continuously improve our practices.
Q 21. How would you explain a complex ultrasound finding to a patient?
Explaining complex ultrasound findings to patients requires careful communication skills and a patient-centered approach. I start by acknowledging that medical terminology can be confusing and adjust my language accordingly. I use clear, simple language and avoid medical jargon, relying instead on analogies and visual aids whenever possible.
For example, if a patient has a complex cardiac finding, I might use a diagram of the heart to illustrate the affected area and explain its function. I explain the finding in terms of its potential impact on the patient’s health and address any concerns they may have. I also involve family members if the patient agrees. Crucially, I avoid providing a diagnosis; instead, I relay the findings to the referring physician who will discuss the next steps with the patient. My role is to provide the information clearly and supportively, ensuring the patient feels understood and supported.
Q 22. What are your strengths and weaknesses as an ultrasound technologist?
My greatest strength as an ultrasound technologist is my ability to quickly adapt to various clinical situations and patient needs. I’m skilled at performing a wide range of ultrasound examinations, from basic abdominal scans to more complex cardiac studies, and I’m comfortable working with diverse patient populations, adjusting my approach as necessary to ensure their comfort and understanding. I am also proficient in troubleshooting equipment malfunctions and maintaining a calm demeanor under pressure. For example, during a recent exam, a patient experienced unexpected anxiety. I calmly reassured them, explaining the procedure step by step, ultimately completing the scan successfully. A weakness I’m actively working on is delegation. While I’m highly efficient, I sometimes take on too much responsibility. I’m actively working on better time management and prioritizing tasks to improve this area.
Q 23. Describe your experience working with electronic medical records (EMR) systems.
I have extensive experience with various EMR systems, including Epic and Cerner. My experience spans data entry, image management, report generation, and patient information retrieval. I understand the importance of accurate and timely documentation within the EMR system. For example, I’m skilled in using these systems to accurately record scan findings and ensuring that all relevant images are attached to the patient’s record. My attention to detail is crucial here as it ensures that all the relevant clinical information is available to the physicians when they review the study. I’m also familiar with EMR-integrated reporting systems, speeding up the process and improving efficiency.
Q 24. How do you stay up-to-date with advances in ultrasound technology and techniques?
Staying current in the rapidly evolving field of ultrasound is crucial. I accomplish this through multiple avenues. I actively participate in continuing medical education (CME) courses and workshops, focusing on emerging technologies and advancements in specific ultrasound applications. I also subscribe to leading ultrasound journals like the Journal of Ultrasound in Medicine and regularly review peer-reviewed articles to keep my knowledge sharp. Furthermore, I engage in professional organizations like the Society of Diagnostic Medical Sonography (SDMS), participating in webinars and conferences to learn from experts and network with colleagues. This multi-faceted approach keeps me abreast of the latest advancements in the field.
Q 25. What is your understanding of HIPAA and patient confidentiality?
HIPAA (Health Insurance Portability and Accountability Act) and patient confidentiality are paramount. I understand the importance of protecting patients’ Protected Health Information (PHI). This includes adhering to strict protocols for accessing, storing, and transmitting patient data. I’m meticulous in ensuring that patient information is only accessed on a need-to-know basis and that all electronic and paper records are securely stored and handled according to HIPAA guidelines. For instance, I always verify patient identity before accessing their records and I immediately report any suspected breaches of confidentiality. Patient privacy is not just a policy; it’s a core principle guiding my practice.
Q 26. Describe your experience with different types of contrast agents used in ultrasound imaging.
I have experience with various contrast agents used in ultrasound, including both microbubble-based agents (like SonoVue and Definity) and newer agents under development. My understanding encompasses their mechanism of action, indications, contraindications, and potential adverse effects. I’m aware that microbubble contrast agents enhance visualization of blood flow and improve the detection of certain pathologies. For example, SonoVue is often used in liver imaging to better identify lesions or in cardiac studies to assess wall motion. I meticulously follow the manufacturer’s instructions for preparation and administration, ensuring patient safety throughout the procedure. I’m also well-versed in documenting the type and amount of contrast agent used in the patient’s record.
Q 27. How do you troubleshoot common technical issues encountered during an ultrasound examination?
Troubleshooting technical issues is a routine part of my work. My approach is systematic. I first assess the nature of the problem; is it related to the machine itself, the transducer, or the image settings? For example, if I’m getting a poor image quality, I would first check transducer connection, then machine settings (gain, TGC), and finally, look for any artifacts suggestive of a problem with the machine itself. If the problem persists, I follow the established protocol within my facility, which may involve contacting a biomedical engineer for assistance. My goal is to minimize downtime and ensure that the patient’s examination is completed efficiently and effectively. Accurate documentation of the issue and any troubleshooting steps taken is also critical.
Q 28. Explain your understanding of the limitations of ultrasound imaging.
Ultrasound, while a powerful imaging modality, has limitations. It’s crucial to understand these to interpret the images accurately. One major limitation is its dependence on acoustic impedance differences between tissues. This can lead to difficulty in visualizing structures with similar acoustic properties, for example, distinguishing between certain types of soft tissue masses. Another limitation is the inability of ultrasound to penetrate bone or air effectively, leading to shadowing artifacts and potentially missed pathology in those areas. Lastly, operator-dependence is a significant factor. The quality of the ultrasound image and the diagnostic accuracy are significantly impacted by the skill and experience of the sonographer. Thus, accurate interpretation requires awareness of these inherent limitations and correlation with clinical information.
Key Topics to Learn for Ultrasound Image Examination Interview
- Image Acquisition Techniques: Understand the principles behind different transducer types (linear, convex, phased array), their applications, and limitations. Master optimizing image settings for various anatomical structures.
- Image Optimization and Artifacts: Learn to identify and interpret common artifacts (e.g., shadowing, enhancement, reverberation) and how they affect diagnosis. Practice adjusting gain, TGC, and other parameters to improve image quality.
- Anatomical Knowledge: Develop a strong understanding of normal anatomy relevant to ultrasound examinations (e.g., abdominal, cardiac, vascular). Be prepared to describe the typical appearance of various organs and structures on ultrasound.
- Pathology Recognition: Familiarize yourself with common pathologies and their characteristic ultrasound appearances. Practice differentiating normal from abnormal findings and explaining your reasoning.
- Measurements and Calculations: Master the techniques for performing accurate measurements (e.g., organ size, fetal biometry) and relevant calculations (e.g., ejection fraction). Understand the clinical significance of these measurements.
- Safety Protocols and Patient Care: Review safety guidelines for ultrasound use, including ALARA principles and patient positioning. Be prepared to discuss patient communication and ethical considerations.
- Report Writing and Documentation: Understand the importance of clear and concise documentation. Practice describing findings and conclusions in a professional and medically accurate manner.
- Troubleshooting and Problem-Solving: Develop your ability to troubleshoot technical issues with ultrasound equipment and adapt your technique to overcome challenges during examinations.
Next Steps
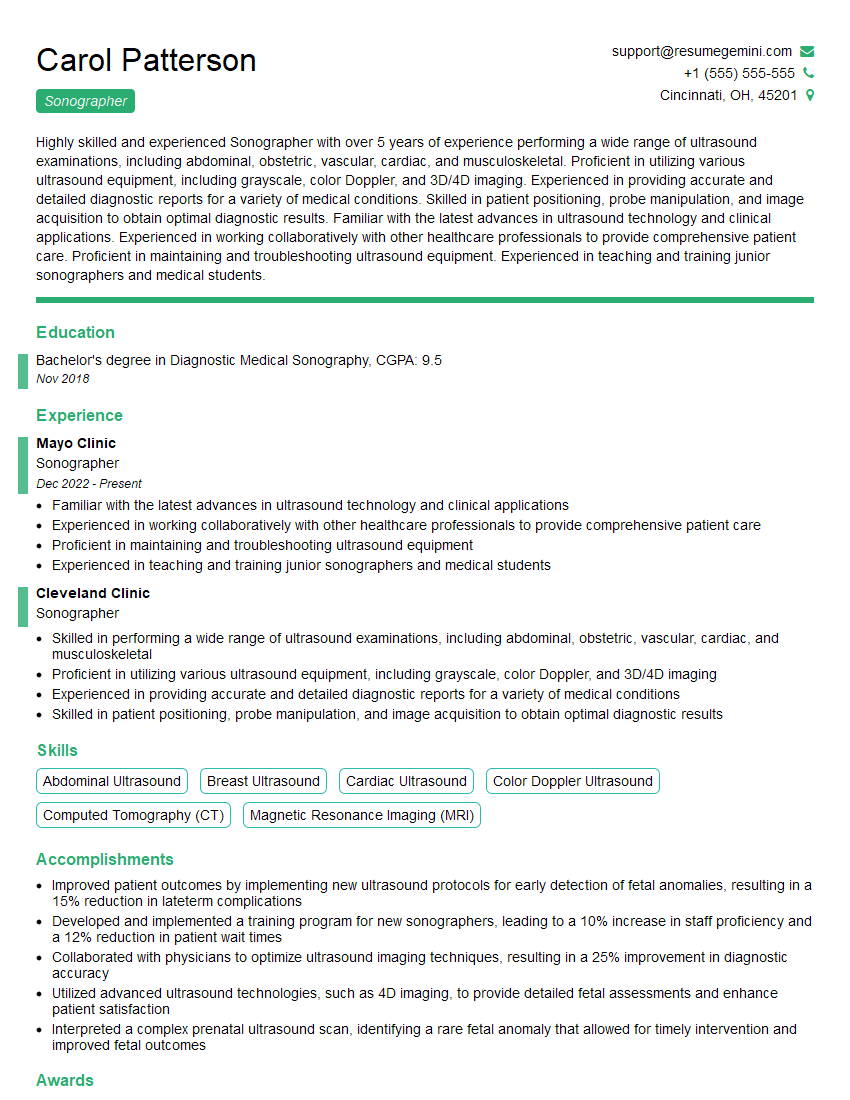
Mastering Ultrasound Image Examination opens doors to exciting career opportunities and advancement within the medical field. A strong foundation in this area demonstrates expertise and professionalism, making you a highly desirable candidate. To further enhance your job prospects, invest time in crafting an ATS-friendly resume that highlights your skills and experience effectively. ResumeGemini is a trusted resource that can help you build a professional and impactful resume tailored to the demands of the Ultrasound Image Examination field. Examples of resumes tailored to this specialization are available to help guide you. Take the next step towards your dream career today!
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hi, I have something for you and recorded a quick Loom video to show the kind of value I can bring to you.
Even if we don’t work together, I’m confident you’ll take away something valuable and learn a few new ideas.
Here’s the link: https://bit.ly/loom-video-daniel
Would love your thoughts after watching!
– Daniel
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.