Interviews are opportunities to demonstrate your expertise, and this guide is here to help you shine. Explore the essential Food Allergy Diagnosis and Management interview questions that employers frequently ask, paired with strategies for crafting responses that set you apart from the competition.
Questions Asked in Food Allergy Diagnosis and Management Interview
Q 1. Describe the process of skin prick testing for food allergies.
Skin prick testing is a quick and relatively inexpensive method to screen for IgE-mediated food allergies. It involves placing a tiny drop of a potential allergen extract onto the skin, usually on the forearm or back. A sterile lancet is then used to lightly prick the skin through the drop, allowing a small amount of allergen to enter. After 15-20 minutes, the area is examined for a wheal (a raised, itchy bump) and flare (redness surrounding the wheal). A larger wheal and flare indicate a positive reaction, suggesting an allergy to that specific food. A negative reaction means no significant IgE-mediated response was detected. A saline solution is used as a control to ensure the test is working correctly; a reaction to saline suggests a false positive.
For example, if a patient is suspected of having a peanut allergy, a drop of peanut extract will be pricked onto their skin. A positive reaction (a wheal of a certain size or larger) would suggest the presence of peanut-specific IgE antibodies. It’s crucial to remember that skin prick testing isn’t foolproof; it can produce false positives or negatives, and further testing might be required for confirmation.
Q 2. Explain the difference between IgE-mediated and non-IgE-mediated food allergies.
Food allergies are broadly classified into IgE-mediated and non-IgE-mediated types. IgE-mediated allergies are the classic, often severe, allergic reactions. They are triggered by the binding of allergen-specific IgE antibodies to mast cells and basophils, leading to the release of histamine and other inflammatory mediators. This causes rapid-onset symptoms. Examples include peanut allergy, milk allergy, and shellfish allergy.
Non-IgE-mediated allergies, on the other hand, don’t involve IgE antibodies. They typically have a slower onset and are often less severe. These reactions are mediated by other immune cells and pathways, such as T cells, and involve mechanisms like cell-mediated cytotoxicity or eosinophilic inflammation. Examples include reactions to food additives like sulfites or some forms of food protein-induced enterocolitis syndrome (FPIES).
Think of it like this: IgE-mediated reactions are like a rapid fire response – immediate and intense. Non-IgE mediated reactions are more like a slow burn – the symptoms develop gradually.
Q 3. How do you interpret a food allergy blood test (RAST/CAP)?
RAST (Radioallergosorbent test) and CAP (Component-resolved diagnostics) are blood tests that measure the levels of specific IgE antibodies against various food allergens. These tests are less prone to false positives compared to skin prick tests, especially in individuals with eczema or taking antihistamines which might interfere with skin prick tests. However, they might miss non-IgE mediated allergies. The results are reported as a quantitative value – usually a class or a specific number representing the concentration of IgE antibodies. A higher number indicates a stronger allergic response.
Interpreting the results involves comparing the patient’s IgE levels to established reference ranges. For instance, a high IgE level for peanut might indicate peanut allergy. However, the interpretation should also consider the patient’s clinical history (symptoms) and other diagnostic findings. A negative test doesn’t completely rule out allergy, especially if the clinical picture suggests it, hence further tests may be needed.
Component-resolved diagnostics provides a more detailed analysis by identifying specific allergen components within a food causing the allergy. This helps in tailoring better allergy management plans, such as immunotherapy targeting the specific allergens identified.
Q 4. What are the common symptoms of a food allergic reaction?
Symptoms of food allergic reactions vary greatly in severity and onset, ranging from mild to life-threatening. Mild reactions might include skin symptoms like hives, itching, or rash; gastrointestinal problems such as nausea, vomiting, diarrhea, or abdominal cramps; and respiratory symptoms like a runny nose or sneezing.
More severe reactions can involve angioedema (swelling, especially around the face, lips, and tongue), difficulty breathing (due to bronchospasm or swelling in the throat), hypotension (low blood pressure), dizziness, and loss of consciousness. The most severe reaction is anaphylaxis, a life-threatening condition requiring immediate medical attention.
For example, a mild reaction to milk might involve some mild stomach upset. In contrast, a severe reaction to peanuts might manifest as hives, throat swelling, difficulty breathing, and a drop in blood pressure—requiring immediate epinephrine administration and emergency medical care.
Q 5. What is the difference between food allergy and food intolerance?
Food allergy and food intolerance are often confused, but they are distinct conditions. Food allergy is an immune system response triggered by a specific food protein, leading to potentially severe reactions mediated by the immune system, commonly involving IgE. It can manifest in various symptoms, ranging from mild to life-threatening anaphylaxis.
Food intolerance, on the other hand, is not an immune response but rather a problem with digesting a certain food. Symptoms tend to be less severe and are often gastrointestinal in nature, such as bloating, gas, abdominal pain, or diarrhea. These symptoms are usually not life threatening and can be avoided by dietary restrictions.
For instance, someone with a milk allergy might experience hives and breathing difficulties upon consuming dairy products. In contrast, someone with lactose intolerance might experience bloating and diarrhea after drinking milk due to the inability to digest lactose.
Q 6. Explain the management of anaphylaxis.
Anaphylaxis is a life-threatening, rapidly progressing allergic reaction that requires immediate intervention. The cornerstone of anaphylaxis management is the administration of epinephrine (adrenaline). This should be given as soon as anaphylaxis is suspected.
Steps involved in managing anaphylaxis:
- Immediate Epinephrine Injection: Administer epinephrine via intramuscular injection (thigh) using an auto-injector (EpiPen, Auvi-Q). Follow the instructions on the auto-injector carefully.
- Call Emergency Services: Dial emergency services immediately, even after administering epinephrine. Anaphylaxis can recur.
- Monitoring and Support: Closely monitor the patient’s vital signs (breathing, heart rate, blood pressure). Ensure airway patency, provide oxygen, and place the patient in a supine position with their legs elevated.
- Further Medical Care: Patients who have experienced anaphylaxis need to be taken to the hospital for ongoing observation and potential treatment, which may include intravenous fluids, antihistamines, corticosteroids, and bronchodilators.
It’s critical to remember that epinephrine is the most important treatment for anaphylaxis and should be given promptly. Delaying treatment can be life-threatening. Patients should always carry an auto-injector and be trained on its proper use. Post-anaphylaxis, a comprehensive assessment and management plan should be created by an allergist.
Q 7. Discuss the role of an elimination diet in food allergy diagnosis.
An elimination diet involves temporarily removing suspected allergenic foods from a patient’s diet to see if symptoms improve. It’s a valuable tool in diagnosing food allergies, especially in cases where other diagnostic tests are inconclusive or suggest a non-IgE mediated allergy. The process usually involves a strict elimination phase, followed by a gradual reintroduction phase under medical supervision.
The elimination phase typically lasts for several weeks, during which the patient avoids all suspected allergens. If symptoms improve, it suggests a possible link between those foods and the patient’s condition. The reintroduction phase involves gradually adding back the eliminated foods one at a time, while closely monitoring for any return of symptoms. This helps to identify the specific trigger food(s) and confirm the diagnosis.
For example, if a patient suspects they are allergic to dairy, gluten, and eggs, an elimination diet would involve removing these foods from their diet for several weeks. If their symptoms (e.g., bloating, eczema, etc.) improve, the foods are reintroduced one by one. If a reintroduction of dairy causes a return of symptoms, this confirms the diagnosis of a dairy allergy. It’s important to note that elimination diets should be done under the guidance of a registered dietitian or allergist to ensure nutritional adequacy and avoid potential deficiencies.
Q 8. Describe the process of oral food challenges.
Oral food challenges (OFCs) are a crucial diagnostic tool in food allergy management. They involve gradually increasing the dose of an allergenic food under strict medical supervision to determine the threshold at which a reaction occurs. It’s the gold standard for confirming or refuting a suspected food allergy, especially after a positive skin prick test or blood test.
The process typically begins with a very small dose of the food, administered in a controlled setting like a hospital or allergist’s office, with continuous monitoring for reactions. The dose is incrementally increased over several hours or even days, depending on the severity of the suspected allergy and the patient’s response. Vital signs, such as heart rate and blood pressure, are closely monitored throughout. The patient is observed for any signs or symptoms of a reaction, from mild skin rashes to life-threatening anaphylaxis. If no reaction occurs at the final dose, the patient is deemed to have outgrown the allergy or has a low risk of reaction with that food.
For example, a child suspected of having a peanut allergy might start with a minuscule amount of peanut protein and gradually increase the dose while being carefully observed by medical professionals. If any allergic symptoms occur at any stage, the challenge is stopped immediately. Successful completion means they likely tolerate peanut products, although continued caution is always advised.
Q 9. How do you counsel patients with food allergies on dietary management?
Counseling patients with food allergies on dietary management requires a holistic approach, encompassing education, planning, and emotional support. It’s not just about avoiding the allergen; it’s about developing safe eating habits and strategies to manage the allergy effectively in daily life.
This involves:
- Detailed education about the allergen: Understanding the specific foods containing the allergen and hidden sources is crucial. This includes cross-contamination risks.
- Label reading: We thoroughly explain the importance of scrutinizing food labels for allergen declarations, including those for potential hidden sources like cross-contamination.
- Safe food preparation and handling: We provide instructions on safe food preparation techniques, emphasizing avoiding cross-contamination. This includes using separate cutting boards, utensils, and cooking surfaces.
- Developing strategies for social situations: Navigating eating out, parties, and school lunches requires specific planning. We help them develop strategies, like bringing their own safe food and communicating with others about their allergies.
- Emergency preparedness: We teach patients about recognizing symptoms of allergic reactions and how to use their epinephrine auto-injectors if needed. We also stress the importance of having a written action plan.
- Addressing emotional aspects: Food allergies can impact social life and emotional well-being. We provide support and strategies for coping with stress and social anxieties related to food allergies.
For instance, I’d counsel a teenager with a severe milk allergy on how to navigate social gatherings by bringing a safe snack or alternative milk, and I would empower them to confidently communicate their allergy to friends and peers. It’s a collaborative process of empowerment, not just restriction.
Q 10. What are the current guidelines for food allergy labeling?
Food allergy labeling guidelines vary across countries but generally aim to ensure consumer safety and transparency. Many jurisdictions, such as the United States and the European Union, mandate the declaration of major allergens on food labels. These typically include milk, eggs, fish, shellfish, tree nuts, peanuts, wheat, and soybeans. However, the precise regulations regarding what constitutes a major allergen and how it should be labeled differ.
Key aspects of food allergy labeling usually include:
- Clear allergen declaration: Allergens must be clearly identified in the ingredient list, often using plain language and bold type.
- Statement of potential cross-contamination: Manufacturers might include statements indicating the potential for cross-contamination during processing, handling, or packaging.
- Precaution statements: Warnings might be included to highlight the presence of allergens in ingredients that aren’t explicitly mentioned (e.g., ‘May contain traces of nuts’).
- Standardized terminology: Many countries use standardized terms to improve consistency and understanding. For example, ‘peanuts’ and not ‘groundnuts.’
It is essential to note that regulations continually evolve, and keeping abreast of the most current guidelines is critical for both clinicians and consumers. There are also variations based on the level of processing of a product; a manufactured item will have more stringent regulations than a fresh product.
Q 11. Discuss the role of epinephrine in managing food allergic reactions.
Epinephrine is a life-saving medication for managing severe allergic reactions (anaphylaxis). It’s a potent vasoconstrictor and bronchodilator that reverses the effects of histamine and other mediators involved in anaphylaxis. It addresses both the respiratory and circulatory components.
In a food allergy reaction, epinephrine works by:
- Constricting blood vessels: This helps raise blood pressure, which can be dangerously low during anaphylaxis.
- Relaxing airway muscles: This opens up the airways and makes breathing easier. This counters the bronchoconstriction caused by allergic mediators.
- Slowing down the release of histamine and other inflammatory mediators: This prevents further escalation of the allergic reaction.
Epinephrine is administered via auto-injectors, such as EpiPen or Auvi-Q, designed for easy self-administration or administration by bystanders. It’s essential for patients at risk of anaphylaxis to carry an auto-injector at all times and to be trained on its use. Even if symptoms improve after epinephrine, immediate medical attention is crucial as a second phase of anaphylaxis can occur.
In a practical setting, I teach my patients how to correctly use their auto-injectors and the importance of seeking immediate medical attention even after administration.
Q 12. How do you advise patients on avoiding cross-contamination?
Avoiding cross-contamination is paramount in managing food allergies, as even tiny amounts of allergen can trigger a reaction. This requires a multi-pronged approach, emphasizing awareness, careful food handling, and communication.
Advice on avoiding cross-contamination includes:
- Dedicated food preparation areas: Use separate cutting boards, utensils, and cooking surfaces for allergen-free foods. Thoroughly wash and clean everything between uses.
- Careful storage: Store allergen-free foods separately from allergenic foods, ideally in airtight containers. This prevents airborne particles from contaminating other items.
- Proper cleaning of surfaces: Always wash hands thoroughly before and after handling food, and sanitize surfaces after contact with allergens.
- Restaurant awareness: When eating out, clearly communicate allergies to staff, and check how food is prepared. Many restaurants lack comprehensive procedures; it is better to be too cautious.
- Communication and education: Inform family, friends, caregivers, teachers, and other relevant individuals about the allergy and how to avoid cross-contamination.
For example, a parent of a child with a milk allergy would be advised to use separate milk-free butter and utensils for the child’s food. In restaurants, they should ensure clear communication with staff about the child’s allergy. This requires proactive communication and careful planning to ensure the child’s safety.
Q 13. Explain the importance of reading food labels.
Reading food labels is a fundamental skill for anyone with food allergies, and it’s a skill that should be taught to all ages. Labels provide essential information about ingredients, potential allergens, and manufacturing processes, which can significantly impact the safety of a food product for someone with allergies.
The importance of reading food labels stems from several factors:
- Allergen identification: Labels clearly list all ingredients, including those containing major allergens. This allows individuals to quickly determine if a food is safe for consumption.
- Hidden allergens: Many processed foods contain hidden allergens, such as traces of nuts in manufactured chocolate. Reading labels helps identify these hidden allergens.
- Cross-contamination warnings: Labels may include warnings about potential cross-contamination during processing or packaging, alerting the consumer to a risk.
- Ingredient variations: Product formulations can change, and updated labeling helps manage this dynamic landscape. Regular checks are essential.
I teach my patients to carefully scrutinize the ingredients list, paying close attention to any precautionary statements regarding possible cross-contamination. The skill of reading food labels is crucial for maintaining safety.
Q 14. What are the different types of food allergy reactions?
Food allergy reactions vary greatly in their severity and presentation, ranging from mild to life-threatening. They’re classified based on the systems of the body that are affected.
Types of food allergy reactions include:
- Mild reactions: These may involve mild skin reactions (hives, itching, redness), mild gastrointestinal symptoms (nausea, vomiting, diarrhea), or mild respiratory symptoms (runny nose, sneezing).
- Moderate reactions: These include more severe skin reactions (extensive hives, swelling), more intense gastrointestinal symptoms, or more significant respiratory symptoms (wheezing, coughing).
- Severe reactions (anaphylaxis): This is a life-threatening systemic reaction involving multiple organ systems. It can present with difficulty breathing, swelling of the throat or tongue, dizziness, loss of consciousness, rapid pulse, and a drop in blood pressure. It requires immediate medical attention and administration of epinephrine.
It is important to note that the same food can cause different reactions in different individuals and even in the same individual on different occasions, with the severity ranging from mild symptoms to potentially fatal anaphylaxis. This underscores the importance of accurate diagnosis and consistent emergency preparedness.
Q 15. What are the potential long-term complications of untreated food allergies?
Untreated food allergies can lead to a range of serious long-term complications. The most immediate danger is anaphylaxis, a life-threatening reaction that can cause airway constriction, circulatory collapse, and even death. Even without anaphylaxis, repeated exposure to allergens can cause chronic inflammation in the gastrointestinal tract, leading to conditions like eosinophilic esophagitis (EoE), characterized by esophageal inflammation and difficulty swallowing. Other potential long-term consequences include chronic urticaria (hives), eczema, and asthma. The chronic inflammation associated with untreated food allergies can also impact overall health and potentially increase the risk of other autoimmune diseases. Imagine a scenario where a child repeatedly experiences mild reactions to peanuts, ignoring the warnings. Over time, these seemingly minor reactions could build up, leading to a more severe reaction later, possibly even anaphylaxis. The cumulative effect of these allergic reactions can have a significant impact on the child’s quality of life, affecting their diet, social interactions, and overall well-being.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you approach the diagnosis of food allergies in infants and children?
Diagnosing food allergies in infants and children requires a multi-step approach. It begins with a thorough history taking, including detailed information about the child’s symptoms, their timing relative to food intake, and family history of allergies. A physical exam is crucial, looking for signs of eczema, asthma, or other allergic manifestations. We then proceed with allergy testing. Skin prick tests are often the first line of defense; they are relatively quick and non-invasive. However, blood tests (like IgE specific antibody tests) are sometimes necessary, particularly for infants too young for skin prick testing or when skin prick tests are inconclusive. A controlled food challenge, where the suspected allergen is introduced gradually under medical supervision, is often the gold standard for confirming a diagnosis, but it should only be conducted in a setting where immediate medical intervention is available. For example, if a child exhibits symptoms consistent with a milk allergy—such as vomiting, diarrhea, and rashes—after consuming milk, we would begin with a thorough history, look for other allergy signs, and then perform skin prick testing or a blood test to detect IgE antibodies against milk proteins. If the results are positive, a controlled milk challenge under careful medical observation might be needed to definitively confirm the diagnosis and assess the severity of the reaction.
Q 17. Discuss the role of collaboration with other healthcare professionals in managing food allergies.
Managing food allergies effectively relies heavily on collaboration. I work closely with pediatricians, allergists, gastroenterologists, and registered dietitians. Pediatricians provide overall health care and assess the child’s general well-being. Allergists specialize in diagnosing and managing allergic diseases and provide expertise in allergy testing and treatment plans. Gastroenterologists play a crucial role in cases with gastrointestinal involvement. Registered dietitians help patients develop safe and nutritionally balanced diets, addressing potential nutrient deficiencies caused by avoiding specific foods. For instance, if a child has a severe peanut allergy, the allergist might guide allergy testing, develop an emergency action plan, and provide recommendations for avoidance. The dietitian then helps the family create a peanut-free diet rich in protein and other essential nutrients. Collaboration is not limited to medical professionals; we also emphasize collaboration with patients and their families to ensure compliance with the treatment plan and empower them to manage the allergy effectively.
Q 18. Explain the different types of food allergy testing available.
Several food allergy testing methods exist. Skin prick tests involve pricking the skin with a small amount of the suspected allergen and observing for a wheal (a raised, itchy bump). This is a quick, relatively inexpensive, and widely used method. Blood tests measure the level of specific IgE antibodies in the blood against various allergens. This method is useful for infants and those who cannot tolerate skin prick testing. Food challenges, as mentioned, involve controlled introduction of the allergen under medical supervision. This is the gold standard for confirmation but carries inherent risks and needs to be done in a monitored setting. Component-resolved diagnostics (CRD) are newer tests that identify specific allergen molecules within a food that cause reactions, potentially offering more personalized risk assessments. For example, a patient might have a strong IgE response to a specific protein component of milk, but not others, allowing for a more tailored approach to management.
Q 19. What are the limitations of different food allergy testing methods?
Each testing method has limitations. Skin prick tests can produce false negatives (a negative result when the patient actually has an allergy) or false positives (a positive result when there isn’t an allergy). They might also not be reliable for certain allergens. Blood tests, while useful, can also show false positives or negatives, especially for low-level allergies. While accurate for many, they don’t always reflect the clinical reality, meaning a positive blood test doesn’t always mean a clinical reaction will occur. Food challenges, though the gold standard, are time-consuming, expensive, and carry a risk of severe reactions. Furthermore, CRD tests are still relatively new and might not be widely available or comprehensive. It’s vital to consider the limitations of each test and integrate clinical presentation with the test results to reach a comprehensive diagnosis.
Q 20. How do you manage a patient experiencing a severe allergic reaction in a clinical setting?
Managing a severe allergic reaction requires immediate action. The first step involves recognizing the signs and symptoms of anaphylaxis (e.g., difficulty breathing, swelling of the face and throat, dizziness, and a sudden drop in blood pressure). Immediate administration of epinephrine via an auto-injector (like an EpiPen) is crucial. This is followed by maintaining the airway, providing supplemental oxygen, and monitoring vital signs closely. The patient must be transported to the nearest hospital immediately for further treatment, which may include intravenous fluids, medications to counteract the allergic reaction, and continuous monitoring. It’s essential to remember that every second counts during an anaphylactic reaction. Timely administration of epinephrine is paramount to preventing life-threatening consequences. Post-reaction care includes assessing the severity, providing patient education on avoidance strategies and carrying an epinephrine auto-injector, and potentially adjusting their allergy management plan.
Q 21. What is your experience with managing food allergies in special populations (e.g., athletes, pregnant women)?
Managing food allergies in special populations requires careful consideration. Athletes with food allergies face the challenge of maintaining optimal nutritional intake without risking an allergic reaction. Close collaboration with sports nutritionists is essential to develop performance-enhancing diets that are also allergen-free. Pregnant women with food allergies need careful monitoring to ensure both maternal and fetal well-being. While there’s no evidence that avoiding allergens during pregnancy reduces the risk of infant allergy, it’s crucial to manage maternal allergies effectively to prevent severe maternal reactions. The management strategy should always prioritize the safety and well-being of the mother and child. For example, an athlete with a dairy allergy might need careful planning to ensure sufficient calcium intake through alternative sources, and a pregnant woman with a severe peanut allergy must develop a detailed avoidance plan with a close collaboration with her physician and dietitian. A proactive approach, close monitoring, and tailored strategies are crucial for optimizing outcomes in these special populations.
Q 22. Describe your approach to educating patients about food allergy self-management.
Educating patients about food allergy self-management is crucial for their safety and well-being. My approach is multifaceted and tailored to each patient’s age, understanding, and specific needs. I begin by clearly explaining the nature of their allergy, emphasizing the severity and potential consequences of accidental exposure. This includes a detailed discussion of symptoms, ranging from mild hives to life-threatening anaphylaxis.
Next, I provide comprehensive instruction on allergen avoidance strategies. This involves meticulous label reading, understanding cross-contamination risks (e.g., shared cooking utensils, airborne allergens), and safe food preparation techniques. I emphasize the importance of carrying emergency epinephrine auto-injectors (like EpiPens) at all times and knowing how to administer them, providing hands-on training whenever possible. We then discuss action plans for accidental exposures, including immediate steps to take and when to seek emergency medical attention.
Furthermore, I empower patients with tools for managing their allergy in various settings, such as school, work, or social events. This may involve creating personalized emergency action plans, educating caregivers or teachers about the allergy, and developing strategies for handling social situations involving food. Regular follow-up appointments allow me to reinforce learning, address any concerns, and adjust management strategies as needed. For example, I recently worked with a young boy with a severe peanut allergy; we not only taught him how to use his EpiPen but also developed a plan for his school, including staff training and a designated safe space for him during lunch.
Q 23. How do you determine the severity of a food allergy?
Determining the severity of a food allergy involves a comprehensive assessment that goes beyond simple skin prick tests or blood tests. It’s crucial to understand the patient’s reaction history. A mild reaction might present as hives or mild gastrointestinal upset, while a severe reaction would involve symptoms such as breathing difficulties, swelling of the throat or tongue (angioedema), and a significant drop in blood pressure (anaphylaxis).
I meticulously gather information on the timing, location, intensity, and duration of previous reactions. The presence of anaphylaxis is a key indicator of severity. I review the patient’s medical history for any previous allergic reactions, including those not necessarily food-related, as this can provide valuable insight into their overall allergic tendency. The use of an objective scoring system, like the Systemic Anaphylaxis Score, helps quantify the severity of anaphylactic episodes for better management and risk stratification.
For instance, a patient who consistently experiences mild hives after consuming traces of milk may have a less severe allergy compared to a patient who has previously experienced life-threatening anaphylaxis after accidental peanut exposure. In some cases, I recommend oral food challenges under carefully controlled medical supervision to determine the threshold for triggering a reaction, allowing for a more precise assessment of allergy severity.
Q 24. What are the ethical considerations in food allergy diagnosis and management?
Ethical considerations in food allergy diagnosis and management are paramount. Firstly, informed consent is critical. Patients must fully understand the risks and benefits of diagnostic tests and treatment options before proceeding. This includes potential side effects of medications, the limitations of diagnostic testing, and the possibility of false positives or negatives.
Secondly, maintaining patient confidentiality is crucial. All information obtained during consultations and testing should be kept private and only shared with authorized individuals involved in the patient’s care. Thirdly, equitable access to care is essential; regardless of socioeconomic status, all patients should have access to appropriate diagnostic testing and treatment options. This might involve advocating for insurance coverage for necessary medications and tests.
Furthermore, there is an ethical obligation to provide evidence-based care, following established guidelines and recommendations from reputable organizations. This means staying current with research and ensuring that treatments are safe and effective. Finally, there is the ethical dilemma of balancing risk reduction with quality of life. While strict avoidance is often necessary, we need to support patients in navigating social situations and avoiding excessive restrictions which may negatively impact their mental and social well-being.
Q 25. How do you stay up-to-date on the latest research and guidelines in food allergy?
Keeping up-to-date in the field of food allergy requires a multi-pronged approach. I regularly review publications from leading journals such as the Journal of Allergy and Clinical Immunology and Annals of Allergy, Asthma & Immunology. I actively participate in continuing medical education courses and conferences focusing on advances in allergy diagnosis and management. These events often feature presentations by leading researchers, providing opportunities to learn about the latest findings and best practices.
I am a member of professional organizations, such as the American Academy of Allergy, Asthma & Immunology (AAAAI), which provides access to updated guidelines, position statements, and educational materials. I utilize online resources and databases, including the AAAAI website and PubMed, to search for relevant research articles and guidelines. I regularly engage with colleagues through professional networks and discussions to share knowledge and learn from their experiences. This network enables me to receive up-to-date information on new diagnostic tools and treatment approaches, ensuring that my practice remains at the forefront of the field.
Q 26. Discuss your experience with different allergen immunotherapy approaches.
Allergen immunotherapy, including sublingual immunotherapy (SLIT) and oral immunotherapy (OIT), offers a promising approach for desensitizing patients to specific allergens. My experience with SLIT involves administering drops of allergen extract under the tongue, gradually increasing the dose over time to build tolerance. This treatment is generally well-tolerated but can cause mild side effects such as itching or mild oral reactions. OIT involves gradually increasing doses of the allergen via oral ingestion, usually under close medical supervision, often in a clinic setting or hospital. It’s a more intensive approach and carries a higher risk of systemic reactions, requiring careful monitoring.
I carefully select patients for immunotherapy, considering factors like the severity of their allergy, their age, and the potential benefits and risks of each approach. Careful patient selection is crucial to minimize the risk of severe reactions. The decision to initiate immunotherapy should be made on a case-by-case basis, weighing the potential benefits against the potential risks and after thorough discussion with the patient and their family. For instance, I’ve successfully used SLIT for patients with mild-to-moderate pollen allergies, while OIT has been more appropriate for certain carefully selected patients with peanut allergies who have shown a consistent response to controlled challenge.
The process requires rigorous monitoring for adverse reactions, with regular follow-up appointments to adjust dosing and assess the patient’s progress. It is a collaborative process involving careful monitoring, ongoing assessment, and close communication between patient, family, and healthcare providers.
Q 27. Explain your experience in managing patients with multiple food allergies.
Managing patients with multiple food allergies requires a highly individualized approach, as the complexity increases significantly with each additional allergen. My strategy centers on meticulous allergen identification and avoidance plans. This involves a thorough history taking, skin prick testing, and specific IgE blood tests to confirm each allergy and establish its severity. This is crucial to avoid accidental exposure. Detailed discussions with the patient and their family are important to understand their dietary habits and potential risk factors.
Developing comprehensive avoidance strategies is critical. This necessitates careful label reading for all food products, awareness of hidden allergens in processed foods, and a detailed understanding of cross-contamination risks in various settings. We work together to create a detailed meal plan and practical strategies to reduce the risk of accidental exposure. I also frequently collaborate with registered dieticians to help patients develop well-balanced, safe diets that meet their nutritional needs.
For instance, a patient with multiple allergies to peanuts, tree nuts, and dairy requires extremely careful attention to all aspects of food handling and preparation, including the avoidance of restaurants with high risk of cross-contamination, and strict adherence to food labeling laws. Regular follow-up is essential to adjust the management plan and address any concerns that may arise.
Q 28. How would you handle a situation where a patient’s symptoms don’t align with the diagnosis?
When a patient’s symptoms don’t align with their diagnosis, a thorough reevaluation is necessary. This situation warrants a systematic investigation to identify potential contributing factors. First, I review the patient’s symptom history, meticulously documenting the timing, severity, and associated factors. I consider the possibility of misdiagnosis, exploring whether previous testing was adequately performed and interpreted. Re-testing, with more specific or sensitive allergy tests, may be warranted. Furthermore, I carefully review the medication list for potential drug interactions or side effects that might mimic allergic reactions.
It’s also important to consider other underlying conditions that may cause similar symptoms, such as gastrointestinal issues, infections, or other allergic conditions. This might necessitate consultation with specialists in other fields, like gastroenterology or immunology. A food diary might be helpful to identify potential food triggers. I’ll carefully discuss the possibility of new onset or evolving allergies, or even co-morbidities presenting similarly to a food allergy.
A patient with a diagnosed peanut allergy who experiences similar symptoms after consuming soy might have a previously undiagnosed soy allergy, or possibly a reaction to a different food. A thorough reevaluation, including detailed history-taking, potential re-testing and consultation with other specialists, is essential to accurately identify the underlying cause of the patient’s symptoms and adjust their management plan accordingly.
Key Topics to Learn for Food Allergy Diagnosis and Management Interview
- Patient History and Physical Examination: Understanding techniques for eliciting a thorough and accurate patient history, including dietary habits and symptom presentation. Practical application: Differentiating between food intolerance and true allergy based on clinical presentation.
- Skin Prick Testing and In Vitro Diagnostics: Mastering the principles and limitations of common allergy tests such as skin prick tests, serum-specific IgE, and component-resolved diagnostics. Practical application: Interpreting test results in the context of patient history and clinical findings; understanding the implications of false positives and negatives.
- Oral Food Challenges: Understanding the procedures, safety protocols, and interpretation of results for double-blind placebo-controlled food challenges (DBPCFCs) and open food challenges. Practical application: Managing potential adverse reactions during and after oral food challenges.
- Allergen Avoidance Strategies: Developing comprehensive strategies for allergen avoidance, including label reading, cross-contamination prevention in various settings (home, school, restaurants), and emergency preparedness. Practical application: Counseling patients on effective avoidance techniques and addressing their concerns.
- Pharmacological Management: Understanding the use of antihistamines, epinephrine, and other medications in the management of allergic reactions. Practical application: Choosing the appropriate medication based on the severity and type of reaction, and educating patients on medication use.
- Anaphylaxis Recognition and Management: Recognizing the signs and symptoms of anaphylaxis and implementing appropriate emergency treatment protocols. Practical application: Describing the steps involved in managing anaphylaxis, including epinephrine administration and emergency medical services call.
- Dietary Management and Nutritional Considerations: Developing appropriate dietary plans for individuals with food allergies, considering nutritional needs and potential deficiencies. Practical application: Collaborating with dietitians and other healthcare professionals to ensure optimal patient care.
- Ethical Considerations and Patient Communication: Addressing the emotional and psychological impact of food allergies on patients and their families, and maintaining open and empathetic communication. Practical application: Building rapport with patients and families, providing support, and addressing concerns effectively.
Next Steps
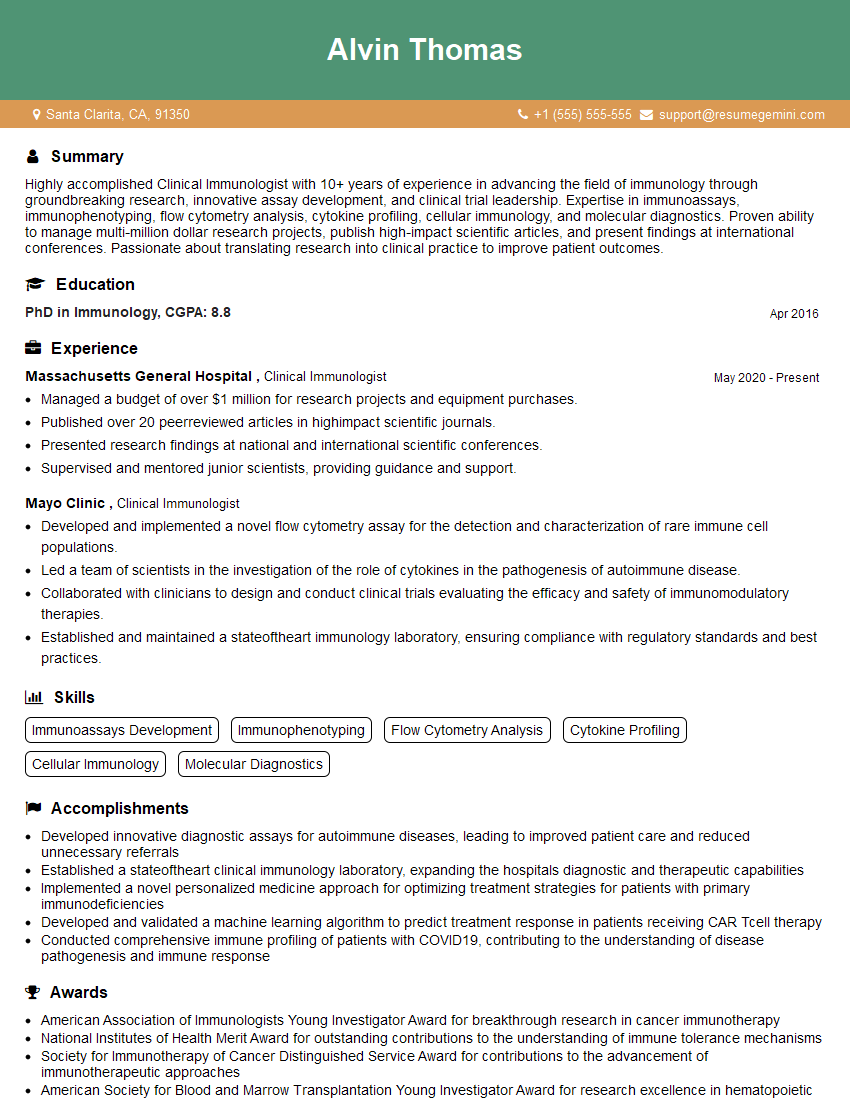
Mastering Food Allergy Diagnosis and Management is crucial for a successful and rewarding career in healthcare. A strong understanding of these concepts will significantly enhance your interview performance and open doors to exciting opportunities. To maximize your job prospects, creating an ATS-friendly resume is essential. ResumeGemini is a trusted resource that can help you build a professional and impactful resume. ResumeGemini provides examples of resumes tailored to Food Allergy Diagnosis and Management, giving you a head start in crafting a document that showcases your skills and experience effectively.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hi, I have something for you and recorded a quick Loom video to show the kind of value I can bring to you.
Even if we don’t work together, I’m confident you’ll take away something valuable and learn a few new ideas.
Here’s the link: https://bit.ly/loom-video-daniel
Would love your thoughts after watching!
– Daniel
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.