Interviews are opportunities to demonstrate your expertise, and this guide is here to help you shine. Explore the essential Allergic Disease Management interview questions that employers frequently ask, paired with strategies for crafting responses that set you apart from the competition.
Questions Asked in Allergic Disease Management Interview
Q 1. Explain the difference between Type I, Type II, Type III, and Type IV hypersensitivity reactions.
Hypersensitivity reactions are classified into four types based on their underlying mechanisms. Think of them as different ways your immune system can overreact to a harmless substance.
- Type I (Immediate): This is the classic allergic reaction, mediated by IgE antibodies. When you’re exposed to an allergen (like pollen or peanuts), IgE antibodies bind to mast cells. Subsequent exposure triggers mast cell degranulation, releasing histamine and other inflammatory mediators. This leads to rapid symptoms like hives, swelling, and difficulty breathing. Imagine it like a pre-set trap – the first exposure sets the trap (IgE binding), and the second exposure springs it (histamine release).
- Type II (Cytotoxic): This involves IgG or IgM antibodies binding to antigens on cell surfaces, leading to cell destruction. An example is autoimmune hemolytic anemia, where antibodies attack red blood cells. Think of it like the immune system mistakenly targeting its own cells.
- Type III (Immune Complex-mediated): This occurs when antigen-antibody complexes deposit in tissues, triggering inflammation. Serum sickness is a classic example. It’s like having a build-up of immune debris causing tissue damage.
- Type IV (Delayed): This is a cell-mediated reaction, involving T cells rather than antibodies. The reaction takes several days to develop, unlike the immediate reactions of Types I-III. Contact dermatitis (e.g., poison ivy) is a good example. Imagine it as a slower, more targeted attack by immune cells.
Q 2. Describe the pathogenesis of allergic rhinitis.
Allergic rhinitis, or hay fever, begins with allergen exposure (like pollen or pet dander). This allergen is inhaled and comes into contact with the nasal mucosa. Mast cells residing in the nasal mucosa are sensitized by IgE antibodies specific to that allergen. Upon subsequent exposure, the allergen cross-links the IgE on the mast cells, triggering their degranulation and the release of inflammatory mediators such as histamine, leukotrienes, and prostaglandins. This causes vasodilation, increased vascular permeability (leading to nasal congestion), mucus secretion, and inflammation of the nasal lining, resulting in the characteristic symptoms like sneezing, runny nose, and itchy eyes. Essentially, it’s an inflammatory cascade triggered by the immune system’s overreaction to harmless substances.
Q 3. What are the common diagnostic tests used in allergic disease management?
Diagnosing allergic diseases often involves a combination of approaches:
- Skin prick tests: A small amount of allergen is pricked onto the skin. A wheal and flare reaction indicates an allergy. It’s a quick, relatively inexpensive, and widely used method.
- Specific IgE blood tests (RAST): These measure the level of IgE antibodies specific to certain allergens in the blood. They’re useful for patients with eczema or other skin conditions that might interfere with skin prick tests.
- Nasal provocation testing: This involves exposing the nasal mucosa to specific allergens to directly assess the response. It’s more specific but less commonly used than skin prick testing.
- Complete blood count (CBC) and other blood tests: May reveal eosinophilia (increased eosinophils), a sign of allergic inflammation.
The choice of test depends on the patient’s clinical presentation and the suspected allergens. Often, a combination of these tests is employed for accurate diagnosis.
Q 4. Discuss the management of anaphylaxis.
Anaphylaxis is a life-threatening allergic reaction requiring immediate intervention. Management follows a clear protocol:
- Establish an airway: This is the priority. If the patient is struggling to breathe, provide supplemental oxygen and potentially intubation.
- Administer epinephrine: This is the cornerstone of anaphylaxis treatment. Epinephrine reverses the effects of histamine, relaxes airway smooth muscles, and improves blood pressure. Intramuscular injection is preferred over intravenous administration in most cases.
- Fluid resuscitation: Intravenous fluids may be needed to treat hypotension.
- Monitor vital signs and provide supportive care: Continuous monitoring of heart rate, blood pressure, and oxygen saturation is crucial. Further treatment may include antihistamines, corticosteroids, and bronchodilators.
- Transfer to a hospital: Even after initial stabilization, patients need to be transferred to a hospital for observation and further management.
It’s crucial to emphasize that early recognition and rapid treatment are critical for survival. Patients with a history of anaphylaxis should always carry an epinephrine auto-injector and have a detailed emergency action plan.
Q 5. Explain the principles of immunotherapy (allergy shots).
Immunotherapy, or allergy shots, involves the gradual introduction of increasing doses of allergens to desensitize the immune system. The goal is to shift the immune response away from IgE-mediated responses towards a more tolerant, IgG-mediated response. This process involves:
- Initial build-up phase: Allergen doses are gradually increased over several months to achieve a maintenance dose.
- Maintenance phase: Regular injections of the maintenance dose are given for several years.
The mechanism is complex but generally involves altering the balance of T helper cell subsets (Th1/Th2), inducing regulatory T cells, and promoting the production of IgG blocking antibodies. Think of it as retraining the immune system to recognize allergens as less of a threat. It’s effective for many allergies, including seasonal allergies and insect venom allergies but requires a commitment to a long-term treatment plan and careful monitoring for side effects.
Q 6. What are the common triggers for food allergies in children?
Common food allergy triggers in children include:
- Milk: Cow’s milk protein is a major allergen.
- Eggs: Both egg white and yolk contain allergens.
- Peanuts: A very common and potentially severe allergen.
- Tree nuts (e.g., almonds, walnuts): Another group of potent allergens.
- Soy: Allergens found in soy products.
- Wheat: Although less common than the others, wheat allergy can occur.
- Fish and shellfish: These are often responsible for severe allergic reactions.
It’s important to note that food allergies can develop at any age, although many are diagnosed during childhood. Early identification and management are crucial to prevent serious reactions.
Q 7. How do you differentiate between allergic and non-allergic rhinitis?
Differentiating between allergic and non-allergic rhinitis requires careful consideration of symptoms, history, and diagnostic testing.
- Allergic rhinitis: Typically involves symptoms like sneezing, itchy eyes and nose, clear rhinorrhea (runny nose), and nasal congestion. It’s strongly linked to specific allergens, shown through positive skin prick tests or IgE blood tests. There’s often a family history of allergic disease.
- Non-allergic rhinitis: This encompasses a range of conditions with similar symptoms but without the underlying allergic mechanism. Triggers can include irritants (like smoke, dust), hormonal changes, or medications. Diagnostic tests for allergies will typically be negative. Vasomotor rhinitis (due to fluctuating blood vessel reactivity) and drug-induced rhinitis are common types of non-allergic rhinitis.
A detailed history, physical examination, and appropriate diagnostic tests are crucial to determine the underlying cause and guide treatment effectively. Often, symptoms overlap, making a precise diagnosis challenging. A specialist may be necessary for complex cases.
Q 8. Describe the management of atopic dermatitis (eczema).
Managing atopic dermatitis (eczema) focuses on controlling the inflammation and itching, improving skin barrier function, and preventing flare-ups. It’s a holistic approach involving several strategies, tailored to the individual’s severity and response.
- Topical Treatments: These are the cornerstone of eczema management. This includes corticosteroids (to reduce inflammation), topical calcineurin inhibitors (like tacrolimus or pimecrolimus, for long-term maintenance in milder cases and when corticosteroids are unsuitable), and moisturizers (to hydrate and support the skin barrier). Choosing the right strength and type of corticosteroid is crucial, and overuse should be avoided.
- Emollients/Moisturizers: Regular application of emollients is essential, ideally multiple times a day, to prevent dryness and itching. Think of it like daily hydration for your skin. This is often the first line of defense in mild cases and is vital alongside other treatments.
- Wet Wraps: For severe flare-ups, wet wraps (applying moisturizer and then wrapping the affected area in wet bandages) can provide significant relief by increasing hydration and reducing inflammation.
- Systemic Treatments: In severe cases unresponsive to topical therapies, oral or injectable medications, like systemic corticosteroids (for short-term, intense flare-ups), or biologics (like dupilumab or lebrikizumab), might be necessary. These options should be used cautiously due to potential side effects.
- Lifestyle Modifications: Identifying and avoiding triggers, such as certain fabrics, soaps, and allergens, is crucial. Managing stress and maintaining good skin hygiene are also important components.
- Phototherapy: In some cases, controlled exposure to ultraviolet (UV) light can help reduce inflammation. This must be done under the strict supervision of a dermatologist.
For example, a child with mild eczema might benefit from regular moisturizer application and avoidance of harsh detergents. Conversely, an adult with severe eczema might require a combination of topical corticosteroids, wet wraps, and possibly systemic therapy, under the guidance of a dermatologist.
Q 9. What are the potential side effects of antihistamines?
Antihistamines are commonly used to treat allergic reactions, but they can have side effects, varying in severity and frequency depending on the type (first-generation or second-generation) and the individual’s sensitivity.
- First-generation antihistamines (like diphenhydramine and chlorpheniramine) are more likely to cause drowsiness, dry mouth, blurred vision, and urinary retention. These effects are due to their ability to cross the blood-brain barrier.
- Second-generation antihistamines (like cetirizine, fexofenadine, and loratadine) are less sedating because they don’t cross the blood-brain barrier as readily. However, they can still cause less frequent side effects such as headache, fatigue, and nausea.
It’s crucial to discuss any potential side effects with your doctor or pharmacist. If drowsiness is a concern, taking the medication at bedtime can mitigate this. It’s important to note that individual responses vary, and what works well for one person might cause more pronounced side effects in another.
Q 10. How do you counsel a patient about the use of epinephrine auto-injectors?
Counseling a patient about epinephrine auto-injectors (like EpiPens) involves a multi-step process, emphasizing the importance of proper use during a life-threatening allergic reaction (anaphylaxis).
- Understanding Anaphylaxis: Explain anaphylaxis in simple terms, emphasizing the severity and potential for rapid deterioration, including respiratory distress and circulatory collapse.
- Proper Technique: Demonstrate the correct injection technique – holding the auto-injector firmly against the outer thigh at a 90-degree angle, pushing firmly until a click is heard, and holding it in place for several seconds. Practical demonstration and hands-on practice are crucial.
- When to Use: Clearly explain the circumstances necessitating epinephrine use – symptoms like difficulty breathing, swelling of the face or throat, dizziness, or a rapid drop in blood pressure.
- After Injection: Instruct the patient to call emergency medical services immediately after administering epinephrine, even if symptoms improve. Epinephrine buys time, but it’s not a cure.
- Carrying the Auto-Injector: Stress the importance of always carrying the auto-injector and having a spare. Discuss strategies for carrying it in a readily accessible location.
- Follow-up Care: Explain the need for immediate medical attention following injection and the necessity of follow-up care with an allergist to determine triggers and develop a long-term management plan.
Using real-life scenarios and role-playing can make this education more impactful. For example, I would simulate a scenario where the patient experiences symptoms and then guide them step-by-step on how to use the auto-injector.
Q 11. What are the risk factors for developing asthma?
Asthma risk factors are complex and multifactorial, involving genetic predispositions and environmental exposures. Identifying these factors can help in prevention and management.
- Genetic Predisposition: Family history of asthma, allergies, or eczema significantly increases the risk. This highlights a genetic component that affects airway inflammation and reactivity.
- Environmental Exposures: Exposure to allergens (like dust mites, pet dander, pollen), air pollutants (like vehicle exhaust and industrial emissions), and respiratory infections in early childhood can trigger asthma development.
- Other Factors: Obesity, smoking during pregnancy (maternal smoking), and low birth weight are also associated with an increased risk of developing asthma.
For instance, a child with a family history of allergies and who lives in a home with pets and dust mites has a substantially higher risk of developing asthma compared to a child without these risk factors. Understanding these factors is key to implementing preventive measures, such as allergen control in the home.
Q 12. Discuss the management of asthma exacerbations.
Managing asthma exacerbations requires a prompt and aggressive approach, aiming to rapidly improve lung function and prevent life-threatening complications.
- Short-Acting Beta-Agonists (SABAs): These (like albuterol) provide quick relief by relaxing the airway muscles. They are the cornerstone of acute treatment. The patient should use their inhaler as prescribed, or more frequently as needed during an exacerbation.
- Oral Corticosteroids: These (like prednisone or methylprednisolone) are potent anti-inflammatory medications used to reduce airway inflammation. They are usually given for a short course (5-10 days).
- Systemic Therapies: For severe exacerbations requiring hospitalization, intravenous corticosteroids and other supportive treatments like oxygen therapy may be necessary.
- Monitoring: Frequent monitoring of respiratory rate, pulse oximetry (to measure oxygen saturation), and peak expiratory flow (PEF) is essential to assess the severity and response to treatment.
For example, if a patient experiences increased wheezing, coughing, and shortness of breath, they should immediately use their SABA inhaler. If symptoms don’t improve or worsen, they should seek medical attention and might require oral corticosteroids or hospitalization.
Q 13. Explain the role of pulmonary function tests in asthma diagnosis.
Pulmonary function tests (PFTs), particularly spirometry, play a vital role in diagnosing and monitoring asthma. They objectively assess lung function, providing quantitative data to support the clinical diagnosis.
- Spirometry: Measures how much air a person can breathe in and out and how quickly they can exhale. Reduced airflow (obstruction) is a key characteristic of asthma. A spirometry test showing reversible airflow obstruction after bronchodilator administration strongly supports an asthma diagnosis.
- Peak Expiratory Flow (PEF): This measures the maximum speed of exhalation and is helpful in monitoring asthma control and detecting early signs of exacerbation. Patients are often taught to use a peak flow meter at home to track their lung function.
Spirometry results showing a significant improvement in FEV1 (forced expiratory volume in one second) after using a bronchodilator indicates reversible airflow limitation, a hallmark of asthma. This, combined with a patient’s clinical symptoms and history, helps confirm the diagnosis.
Q 14. What are the common challenges in managing food allergies?
Managing food allergies presents several significant challenges, requiring careful attention to avoidance, emergency preparedness, and patient education.
- Accidental Exposures: Accidental ingestion of allergens remains a major challenge, particularly in children, due to hidden ingredients in food or cross-contamination during food preparation. Reading food labels carefully and understanding ingredient lists is crucial.
- Labeling Inconsistencies: The labeling of food products varies across countries and regions, making it challenging for individuals with food allergies to always accurately identify potential allergens. This emphasizes the need for thorough label reading and an awareness of potential hidden allergens.
- Anaphylaxis Risk: The potential for life-threatening anaphylaxis necessitates proper emergency preparedness, including carrying epinephrine auto-injectors, knowing how to use them, and having a clear plan for seeking immediate medical attention. This is crucial in preventing life-threatening complications.
- Psychological Impact: Living with food allergies can significantly impact a person’s quality of life, leading to anxiety, social limitations, and dietary restrictions. Providing appropriate support and counseling is an essential aspect of management.
For example, a child with a peanut allergy faces significant challenges in school settings, requiring careful monitoring and communication with school staff and other parents. Educating the child, their parents, and school staff about allergen avoidance and emergency procedures is paramount.
Q 15. Describe the process of skin prick testing.
Skin prick testing is a simple, quick, and relatively inexpensive method used to identify allergens that trigger allergic reactions. It involves pricking the skin with a small amount of a suspected allergen. If you’re allergic to that substance, your skin will react.
The Process:
- The skin on the forearm or back is cleaned with alcohol.
- Small drops of different allergen extracts are placed on the skin.
- A lancet (a small, sterile needle) is used to lightly prick through each drop, allowing a tiny amount of allergen to penetrate the skin.
- The test is left for 15-20 minutes, during which time the area is observed for a wheal (a raised, itchy bump) and flare (redness) reaction.
- A negative control (saline solution) and a positive control (histamine) are also used to ensure the test is working correctly. A positive control should always give a positive reaction, while a negative control should not.
Example: Imagine testing for a peanut allergy. A small drop of peanut extract is pricked into the skin. A positive reaction (a wheal larger than 3mm in diameter) indicates a peanut allergy.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you interpret a positive skin prick test?
A positive skin prick test is interpreted by the presence of a wheal (a raised, pale, itchy bump) and flare (surrounding redness) at the prick site. The size of the wheal is compared to the negative and positive controls. A wheal greater than 3mm in diameter larger than the negative control is typically considered a positive result, indicating allergy. The larger the wheal, the more significant the allergic reaction is likely to be. It’s important to note that the interpretation of a skin prick test should always be done by a qualified healthcare professional who takes the entire clinical picture into account.
Important Considerations: The results should be interpreted in the context of a patient’s medical history and symptoms. A positive test doesn’t automatically mean severe allergy, and a negative test doesn’t rule out allergy completely. False positives and false negatives can occur.
Q 17. Discuss the role of IgE in allergic reactions.
Immunoglobulin E (IgE) is a type of antibody that plays a central role in allergic reactions. It’s produced by plasma cells in response to exposure to an allergen (a substance that causes an allergic reaction).
Mechanism:
- Sensitization: Upon first exposure to an allergen, the immune system produces IgE antibodies specific to that allergen.
- Binding: These IgE antibodies attach to the surface of mast cells and basophils, which are immune cells found in tissues and blood.
- Re-exposure: When the same allergen is encountered again, it binds to the IgE antibodies already attached to the mast cells and basophils.
- Degranulation: This binding triggers the release of various inflammatory mediators from mast cells and basophils, such as histamine, leukotrienes, and prostaglandins. These mediators are responsible for the symptoms of allergic reactions.
Examples of Allergic Reactions mediated by IgE: Hay fever (seasonal allergies), asthma, urticaria (hives), anaphylaxis.
Q 18. What are the different types of inhalers used in asthma management?
Several types of inhalers are used in asthma management, broadly categorized as ‘reliever’ inhalers (for quick relief of symptoms) and ‘preventer’ inhalers (for long-term control).
- Metered-dose inhalers (MDIs): Deliver a precise dose of medication with each puff. Often require a spacer device to improve delivery to the lungs. Some MDIs contain a propellant (hydrofluoroalkane).
- Dry powder inhalers (DPIs): Deliver medication as a dry powder. Often preferred by patients who find MDIs difficult to use. These don’t require coordination of breathing and actuation as precisely as MDIs.
- Soft mist inhalers (SMIs): Deliver medication as a fine mist and are considered easier to use than MDIs. They also generally produce a lower oropharyngeal deposition than MDIs, reducing side effects like thrush.
- Nebulizers: Deliver medication as a mist via a compressor and mask or mouthpiece. Often used for severe asthma exacerbations or for patients who struggle to use inhalers correctly.
Each inhaler type contains different medications, such as beta-agonists (like albuterol – a reliever), corticosteroids (like fluticasone – a preventer), or a combination. The choice of inhaler depends on individual patient needs and preferences, as determined by their physician.
Q 19. Explain the mechanism of action of leukotriene inhibitors.
Leukotriene inhibitors, also known as leukotriene receptor antagonists or LTRA, block the action of leukotrienes, inflammatory chemicals involved in asthma and allergies. Leukotrienes contribute to airway inflammation, bronchoconstriction (narrowing of the airways), and mucus production.
Mechanism of Action: LTRA medications, such as montelukast and zafirlukast, competitively inhibit the binding of leukotrienes to their receptors on cells in the airways and other tissues. By blocking the leukotriene receptors, they prevent the inflammatory effects of leukotrienes, thereby reducing airway inflammation and improving lung function.
Clinical Significance: LTRAs are effective in preventing and treating asthma symptoms, particularly in patients with mild to moderate persistent asthma. They are often used as add-on therapy with inhaled corticosteroids or as an alternative to low-dose inhaled corticosteroids in patients who cannot tolerate them or who have mild asthma. They’re also used in the treatment of allergic rhinitis (hay fever).
Q 20. What are the indications for using monoclonal antibodies in allergic diseases?
Monoclonal antibodies are targeted therapies increasingly used in the management of severe allergic diseases, particularly those that do not respond well to conventional treatments. They work by specifically targeting key players in the allergic response.
Indications:
- Severe allergic asthma: Omalizumab, mepolizumab, reslizumab, dupilumab, and benralizumab are examples of monoclonal antibodies used to target specific components of the allergic inflammatory cascade in severe, uncontrolled asthma.
- Chronic urticaria (hives): Omalizumab and dupilumab are used for chronic spontaneous urticaria that is unresponsive to other treatments.
- Eosinophilic esophagitis (EoE): Dupilumab is an effective treatment for this condition involving eosinophilic inflammation of the esophagus.
- Atopic dermatitis (eczema): Dupilumab and tralokinumab are effective biologics in treating severe atopic dermatitis.
Mechanism: These antibodies target specific molecules like IgE, interleukin-5 (IL-5), or IL-4/IL-13, crucial for the development and progression of allergic inflammation. By neutralizing these molecules, they reduce the inflammatory response and alleviate symptoms.
Q 21. Describe the management of urticaria.
Urticaria, commonly known as hives, is characterized by itchy, raised welts on the skin. Management focuses on symptom relief and identifying and avoiding triggers.
Management Strategies:
- Antihistamines: First-line treatment for most cases of urticaria. Both first-generation (e.g., diphenhydramine) and second-generation (e.g., cetirizine, loratadine) antihistamines are effective, with second-generation agents preferred for their reduced sedative effects.
- High-dose antihistamines: For severe or persistent urticaria, higher doses of second-generation antihistamines may be necessary. Sometimes this requires a prescription from a physician.
- H2-blockers: These medications, such as ranitidine or famotidine, can be added to antihistamines for improved symptom control.
- Leukotriene inhibitors: In cases unresponsive to antihistamines, leukotriene inhibitors can provide additional benefit.
- Corticosteroids: These are generally used for short-term control of severe flares, often orally or as injections, but prolonged use should be avoided due to side effects.
- Omalizumab: For patients with chronic urticaria unresponsive to other treatments.
- Identifying and avoiding triggers: This is crucial for long-term management. Common triggers include foods, medications, stress, infections, and physical stimuli (e.g., heat, cold, pressure).
Example: A patient with chronic urticaria might start with a second-generation antihistamine. If symptoms persist despite increasing the dose, a leukotriene inhibitor or omalizumab might be considered. Identifying and avoiding food triggers is also imperative for management success.
Q 22. What are the common symptoms of angioedema?
Angioedema is a swelling of the deeper layers of the skin, often involving the face, lips, tongue, and throat. It’s distinct from hives (urticaria), which affects the upper skin layers. Think of it like this: hives are a superficial rash; angioedema is a deeper, more significant swelling.
Common symptoms include:
- Swelling of the face, especially around the eyes, lips, and cheeks
- Swelling of the tongue and throat, potentially causing difficulty breathing or swallowing (this is a medical emergency)
- Swelling of the hands and feet
- Itching or burning sensation in the affected area
- Sometimes, abdominal pain if the swelling affects the intestines.
The severity of angioedema varies greatly. Mild cases may involve only facial swelling, while severe cases can be life-threatening due to airway compromise.
Q 23. Discuss the management of allergic conjunctivitis.
Managing allergic conjunctivitis, or allergic eye inflammation, involves identifying and avoiding triggers and using appropriate medications. It’s crucial to tailor treatment to the severity of the symptoms.
Management strategies include:
- Identifying and avoiding allergens: This is the cornerstone of treatment. Keep detailed diaries to identify pollen, pet dander, dust mites, or cosmetics causing symptoms.
- Cold compresses: Simple yet effective for soothing itchy eyes.
- Artificial tears: These help wash away allergens and provide lubrication.
- Antihistamine eye drops: These effectively block histamine, a key inflammatory mediator in allergic reactions. Examples include ketotifen and olopatadine.
- Mast cell stabilizers: Such as cromolyn sodium, prevent the release of histamine from mast cells. These are particularly useful for preventing future reactions.
- Corticosteroid eye drops: These are potent anti-inflammatory agents reserved for more severe cases, and typically only used for a short period due to potential side effects.
For example, a patient with significant seasonal allergic conjunctivitis might benefit from a combination of antihistamine eye drops, artificial tears, and avoidance of peak pollen times. A patient with mild symptoms might manage successfully with cold compresses and artificial tears alone.
Q 24. How do you assess the severity of allergic reactions?
Assessing the severity of allergic reactions requires a systematic approach, considering both the symptoms and the patient’s overall condition. We use a grading system to categorize reactions, ranging from mild to life-threatening.
Severity assessment considers:
- Skin involvement: Urticaria (hives), angioedema (swelling).
- Respiratory symptoms: Wheezing, shortness of breath, cough, difficulty speaking.
- Cardiovascular symptoms: Hypotension (low blood pressure), tachycardia (rapid heart rate).
- Gastrointestinal symptoms: Nausea, vomiting, abdominal cramps.
- Neurological symptoms: Dizziness, confusion, syncope (fainting).
A mild reaction might involve mild hives and itching. A moderate reaction could include widespread hives, some swelling, and mild respiratory distress. A severe reaction, or anaphylaxis, is life-threatening and involves difficulty breathing, low blood pressure, and potential loss of consciousness. This necessitates immediate medical intervention including epinephrine administration.
Q 25. Explain the importance of patient education in managing allergic diseases.
Patient education is paramount in managing allergic diseases. Empowered patients are better able to control their symptoms and prevent future reactions. It’s not just about dispensing medication; it’s about fostering a partnership where the patient actively participates in their care.
Key aspects of patient education include:
- Allergen identification: Helping patients recognize and avoid their triggers.
- Medication education: Explaining how and when to use medications, including potential side effects and interactions.
- Self-management strategies: Teaching patients how to monitor their symptoms and adjust treatment accordingly.
- Emergency preparedness: Educating patients about the signs and symptoms of severe reactions and how to use emergency medications like epinephrine auto-injectors.
- Lifestyle modifications: Advising on environmental control measures and other lifestyle changes that can reduce exposure to allergens.
For example, a patient with asthma triggered by pet dander needs to understand how to manage their inhalers and how to minimize exposure to pets. Similarly, a patient with food allergies needs to carefully read food labels and be prepared for accidental exposure.
Q 26. Discuss the role of environmental control in preventing allergic reactions.
Environmental control plays a crucial role in preventing allergic reactions by reducing exposure to allergens. This is particularly important for indoor allergens like dust mites, pet dander, and mold.
Strategies for environmental control include:
- Dust mite control: Encase mattresses and pillows in allergen-impermeable covers, regularly wash bedding in hot water, and use dust mite-proof mattress covers. Maintain low humidity.
- Pet dander control: Restrict pets to certain areas of the house, regularly vacuum and clean surfaces, and consider using air purifiers with HEPA filters.
- Mold control: Fix leaks promptly, use dehumidifiers in damp areas, clean moldy areas thoroughly, and consider using anti-fungal sprays.
- Pollen control: Keep windows closed during peak pollen seasons, use air conditioning, and shower and change clothes after spending time outdoors.
For instance, a child with severe dust mite allergy may benefit significantly from implementing all the above dust mite control strategies. A person with pollen allergy might find symptom relief by taking antihistamines and using an air purifier, while avoiding strenuous outdoor activities during peak pollen counts.
Q 27. What are the ethical considerations in managing patients with allergic diseases?
Ethical considerations in managing patients with allergic diseases center around patient autonomy, beneficence, non-maleficence, and justice.
Key ethical issues include:
- Informed consent: Ensuring patients fully understand their diagnosis, treatment options, risks, and benefits before making decisions about their care.
- Balancing risks and benefits: Weighing the potential benefits of treatment against potential side effects, particularly when considering medications with significant side effect profiles.
- Resource allocation: Fairly distributing limited resources, such as specialized allergy testing and treatments.
- Patient confidentiality: Protecting sensitive patient information, including allergy history and treatment plans.
- Truthfulness and transparency: Honestly communicating with patients about their condition and treatment options, even if the information is difficult to hear.
For example, a physician needs to fully inform a patient about the potential side effects of immunotherapy before initiating treatment. Similarly, a physician must be sensitive to a patient’s concerns about the cost of allergy testing or treatment and explore available options to ensure equitable access.
Q 28. How do you stay updated on the latest advances in allergic disease management?
Staying updated on the latest advances in allergic disease management is crucial for providing optimal patient care. I utilize several strategies to maintain my knowledge base:
- Reading peer-reviewed journals: I regularly read publications such as the Journal of Allergy and Clinical Immunology and the Annals of Allergy, Asthma & Immunology.
- Attending professional conferences and meetings: These offer opportunities to learn about the latest research findings and best practices from leading experts.
- Participating in continuing medical education (CME) activities: I regularly engage in CME courses and webinars to update my knowledge and skills.
- Networking with colleagues: Discussions and collaboration with other allergists and immunologists are invaluable.
- Monitoring reputable online resources: Staying informed through trusted websites and online medical databases.
A commitment to lifelong learning is essential in the field of allergy and immunology due to the ever-evolving understanding of these complex diseases and the development of new diagnostic and therapeutic modalities.
Key Topics to Learn for Allergic Disease Management Interview
- Immunology Fundamentals: Understanding the basic mechanisms of allergic reactions, including IgE-mediated responses, mast cell activation, and the role of various immune cells.
- Common Allergic Diseases: In-depth knowledge of conditions like allergic rhinitis, asthma, atopic dermatitis, food allergies, and anaphylaxis; including their clinical presentation, diagnosis, and management.
- Diagnostic Techniques: Proficiency in interpreting skin prick tests, allergy blood tests (RAST, ImmunoCAP), and other relevant diagnostic tools.
- Treatment Modalities: Comprehensive understanding of pharmacological therapies (e.g., antihistamines, corticosteroids, leukotriene inhibitors, immunotherapy) and non-pharmacological approaches (e.g., allergen avoidance, environmental control).
- Allergen Immunotherapy: Detailed knowledge of the principles, procedures, and management of subcutaneous and sublingual immunotherapy, including patient selection and monitoring.
- Emergency Management: Understanding the recognition and treatment of severe allergic reactions, including anaphylaxis, and the proper use of epinephrine.
- Patient Education and Counseling: Ability to effectively communicate complex medical information to patients and their families, empowering them to manage their allergies.
- Ethical Considerations: Awareness of ethical dilemmas related to diagnosis, treatment, and patient care in allergic disease management.
- Research and Emerging Trends: Familiarity with current research and advancements in the field, including novel therapies and diagnostic techniques.
- Problem-Solving and Case Studies: Ability to apply theoretical knowledge to real-world scenarios, diagnose allergic conditions based on clinical presentation, and develop effective treatment plans.
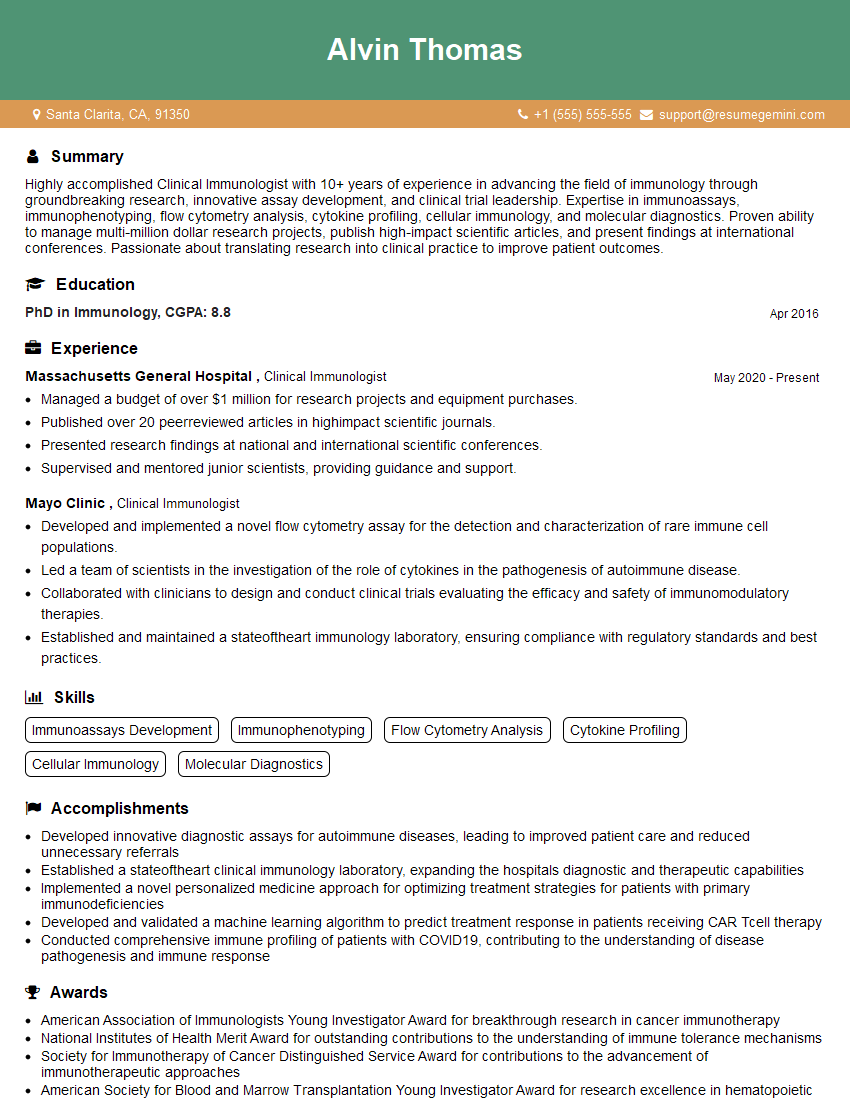
Next Steps
Mastering Allergic Disease Management is crucial for career advancement in this rapidly evolving field. A strong understanding of these key concepts demonstrates your expertise and readiness for challenging roles. To maximize your job prospects, creating a well-structured, ATS-friendly resume is essential. ResumeGemini is a trusted resource that can help you build a professional and impactful resume that highlights your skills and experience. Examples of resumes tailored specifically to Allergic Disease Management are available to guide you. Invest in your future; craft a compelling resume that secures your dream position.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.