Cracking a skill-specific interview, like one for Insect Allergy Testing, requires understanding the nuances of the role. In this blog, we present the questions you’re most likely to encounter, along with insights into how to answer them effectively. Let’s ensure you’re ready to make a strong impression.
Questions Asked in Insect Allergy Testing Interview
Q 1. Explain the process of skin prick testing for insect allergies.
Skin prick testing is a quick, relatively inexpensive, and widely used method for diagnosing insect allergies. It involves placing a small amount of diluted insect venom or allergen extract onto the skin, usually on the forearm. A tiny prick is then made through the drop with a sterile lancet, allowing the allergen to penetrate the skin. We observe the area for a wheal (a raised, itchy bump) and flare (redness) after 15-20 minutes. The size of the wheal and flare is compared to a negative control (saline solution) and a positive control (histamine), helping determine the severity of the allergic reaction.
For example, a large wheal and flare reaction to yellow jacket venom would indicate a significant allergy, whereas a small or absent reaction suggests little or no allergy. The test is interpreted by comparing the patient’s reaction to the controls and established guidelines. It’s important to note that skin prick testing is generally not used to diagnose allergies to whole insect bodies (e.g., cockroaches), but rather to specific venoms.
Q 2. Describe the interpretation of IgE specific immunoassays for insect venom.
Specific IgE immunoassays, often called blood tests, measure the levels of Immunoglobulin E (IgE) antibodies specific to various insect venoms in a patient’s blood. These tests are highly sensitive and can detect even small amounts of IgE antibodies. A high IgE level for a particular venom indicates sensitization, meaning the body has mounted an immune response to that venom and is at risk of an allergic reaction upon subsequent exposure. A low or undetectable IgE level usually indicates a low risk of allergy.
The results are usually reported as a quantitative value (e.g., kU/L or IU/ml) or qualitatively as negative, positive, or borderline. For example, a high IgE level to honeybee venom would suggest a greater chance of experiencing a reaction to a honeybee sting than a low level. It’s crucial to interpret these results in context with the patient’s history, clinical presentation, and other diagnostic tests. Results might need to be confirmed with skin prick testing or other confirmatory tests.
Q 3. What are the common cross-reactivities among insect venom allergens?
Cross-reactivity in insect venom allergies refers to the possibility of having an allergic reaction to one insect venom after sensitization to a different insect venom. This occurs because some venoms share similar protein structures. The most common cross-reactivities are seen within the same insect family.
For example, someone allergic to honeybee venom may also react to yellow jacket or hornet venom. This is because these venoms contain similar allergens, such as phospholipase A2. However, the degree of cross-reactivity varies. While some individuals with a honeybee allergy may experience only a mild reaction to a yellow jacket sting, others may experience a severe reaction. Therefore, careful assessment of both sensitization and clinical reactivity to various venoms is essential.
Understanding cross-reactivity is important for determining appropriate management strategies, including venom immunotherapy and avoidance measures.
Q 4. Discuss the management of anaphylaxis following an insect sting.
Anaphylaxis is a severe, life-threatening allergic reaction that requires immediate medical attention. Management involves prompt administration of epinephrine (adrenaline) using an auto-injector (EpiPen or similar), followed by supportive care. This includes maintaining airway patency, administering oxygen, and providing intravenous fluids.
The steps involved are:
- Immediate Epinephrine Injection: This is the cornerstone of anaphylaxis treatment. The dose should be adjusted based on age and weight.
- Airway Management: Ensure the patient can breathe properly; this may involve intubation in severe cases.
- Oxygen Supplementation: Administer oxygen to improve oxygen levels.
- Fluid Resuscitation: Administer intravenous fluids to maintain blood pressure.
- Monitoring: Continuously monitor vital signs (heart rate, blood pressure, oxygen saturation).
- Transfer to Hospital: Even after initial stabilization, transfer to a hospital for ongoing monitoring and management is essential.
It’s critical to emphasize that early administration of epinephrine is crucial to prevent life-threatening complications. Individuals at risk of anaphylaxis should always carry an auto-injector and be trained on its proper use.
Q 5. How do you differentiate between insect allergy and other similar conditions?
Differentiating insect allergy from other conditions mimicking allergic reactions, like exercise-induced anaphylaxis or food allergies, relies on a thorough history, physical examination, and appropriate diagnostic tests.
A detailed history focusing on the timing and circumstances of reactions is crucial. An insect sting or bite is a key feature of insect allergy. Physical examination may reveal characteristic features like urticaria (hives), angioedema (swelling), or signs of respiratory distress. Diagnostic tests such as skin prick testing and specific IgE immunoassays help confirm the presence of IgE antibodies specific to insect venoms, thereby distinguishing insect allergy from other conditions.
For instance, exercise-induced anaphylaxis symptoms can be similar to an insect sting reaction, but the absence of a sting history and the relationship to exercise point toward a different diagnosis. Similarly, food allergies might be considered if symptoms appear after ingesting a particular food, although cross-reactivity can complicate this. Thorough allergy testing and a careful clinical evaluation allow for a precise diagnosis.
Q 6. What are the limitations of current insect allergy diagnostic tests?
Current insect allergy diagnostic tests have some limitations. Skin prick tests can be affected by factors like skin conditions, medications, or previous reactions. False-negative results are possible, even in sensitized individuals. Specific IgE immunoassays, while very sensitive, may not always correlate directly with clinical reactivity. In other words, a positive test doesn’t always mean severe reactions will occur; similarly, a negative result doesn’t entirely rule out clinical allergy.
Another limitation is the lack of standardized testing and interpretation across different laboratories. This can lead to inconsistencies in diagnosis. Furthermore, testing for all potential insect allergens can be expensive and time-consuming. Lastly, neither test predicts the severity of potential future reactions. Clinicians must combine test results with clinical history and patient-specific risk factors for accurate assessment and management.
Q 7. Explain the role of immunotherapy in insect allergy treatment.
Venom immunotherapy (VIT) is a form of allergen-specific immunotherapy (AIT) used to treat insect venom allergies. It involves administering gradually increasing doses of venom extract subcutaneously over several months or years. The goal is to desensitize the patient to the venom, reducing their allergic response to subsequent stings. This is achieved by modifying the immune system’s response to the venom, shifting it from an IgE-mediated response to a more tolerant IgG-mediated response.
VIT is most effective for individuals who have experienced systemic reactions (anaphylaxis or near-anaphylaxis) to an insect sting. While it’s not a cure, it significantly reduces the risk of future severe reactions. Patients undergoing VIT should be closely monitored for potential adverse effects. This is a carefully managed process, requiring specialized expertise and meticulous adherence to protocols. The decision to use VIT depends on numerous factors including the patient’s risk profile and the availability of resources. It’s a valuable tool for managing severe insect venom allergies but not a first-line treatment for all individuals.
Q 8. Describe different types of insect venom immunotherapy regimens.
Insect venom immunotherapy (IVIT) aims to desensitize individuals allergic to insect venom, reducing the severity of future reactions. Regimens vary, but generally involve subcutaneous injections of increasing doses of venom extract over several months.
- Rush Immunotherapy: This involves rapidly increasing venom doses over a short period (e.g., a few days) in a controlled hospital setting. It’s typically reserved for high-risk patients with a history of severe reactions. Think of it as a fast track to desensitization.
- Maintenance Immunotherapy: After the build-up phase, patients receive regular maintenance doses (e.g., weekly or monthly) to maintain their desensitization. This ongoing treatment is like regular upkeep to prevent the allergy from returning.
- Preseasonal Immunotherapy: For seasonal insect stings, such as yellow jackets, this approach involves starting immunotherapy before the peak stinging season to proactively manage allergy symptoms.
The specific regimen is tailored to the patient’s individual history, sensitivity, and tolerance. Close monitoring is essential throughout the process.
Q 9. What are the potential side effects of immunotherapy for insect stings?
While IVIT is highly effective, potential side effects exist. These can range from mild to severe, and prompt medical attention is crucial if a severe reaction occurs.
- Local Reactions: These are common and usually mild, including redness, swelling, itching, and pain at the injection site. Think of it as a small, localized bump like a mosquito bite.
- Systemic Reactions: These are more serious and can involve hives, itching, swelling in the throat or face (angioedema), difficulty breathing, and dizziness. These mimic the symptoms of an insect sting but are less severe than a true anaphylactic reaction. These require immediate medical attention.
- Anaphylaxis: A rare but life-threatening reaction characterized by severe respiratory distress, circulatory collapse, and potential loss of consciousness. This is a medical emergency requiring immediate epinephrine injection and emergency medical services.
Careful patient selection and close monitoring during immunotherapy are crucial to minimizing risks.
Q 10. How do you counsel patients regarding self-injection of epinephrine?
Counseling patients on epinephrine auto-injectors (like EpiPens) is paramount. It’s crucial to explain its vital role in managing a severe allergic reaction, especially anaphylaxis.
- Demonstration and Practice: I always demonstrate the correct injection technique using a trainer device and have the patient practice several times.
- Timing: Emphasize administering the injection immediately upon recognizing symptoms of a severe allergic reaction, not waiting to see if symptoms worsen.
- Call 911: Reinforce the absolute necessity of calling emergency medical services after self-administering epinephrine. It’s crucial to get professional medical assistance immediately.
- Storage and Expiration: Explain proper storage and check the expiration date regularly. An expired injector is useless in an emergency.
- Follow-up Care: After the injection, even if symptoms improve, they should still seek immediate medical attention at the emergency room.
Patients should carry their auto-injector at all times and inform family members, friends, and teachers/co-workers about its use. I provide written instructions and encourage follow-up questions.
Q 11. What are the indications for referral to a specialist for insect allergy?
Referral to a specialist, such as an allergist/immunologist, is indicated in several scenarios:
- Severe Sting Reactions: A history of anaphylaxis or near-anaphylaxis mandates referral for comprehensive assessment and management.
- Multiple Sting Reactions: Repeated episodes of severe systemic symptoms warrant specialist evaluation for immunotherapy consideration.
- Uncertain Diagnosis: When the diagnosis of insect allergy is unclear, a specialist can conduct thorough testing to determine the specific allergen(s).
- Intolerance to Immunotherapy: If a patient experiences intolerable side effects during immunotherapy, specialist intervention is required to adjust the regimen or explore alternative options.
- Comorbidities: Patients with other medical conditions that could complicate allergy management may require specialized care.
Early referral ensures appropriate care and reduces the risk of serious complications.
Q 12. Discuss the role of component-resolved diagnostics in insect allergy.
Component-resolved diagnostics (CRD) represent a significant advancement in insect allergy testing. Unlike traditional skin or blood tests that only identify the presence of an allergy to a whole venom, CRD identifies the specific components within the venom that cause the allergic reaction.
For example, a patient might test positive for yellow jacket venom allergy using a traditional test. However, CRD could reveal that they are only allergic to specific proteins within the venom, such as hyaluronidase or phospholipase A2. This precise information improves diagnosis and management. It may allow us to tailor immunotherapy to include only the relevant allergens, reducing the risk of side effects and improving treatment efficacy.
CRD helps us better understand the patient’s specific allergy profile and allows for more personalized immunotherapy. This approach moves away from a ‘one-size-fits-all’ approach to more targeted therapy.
Q 13. How do you manage a patient with a history of severe insect sting reaction?
Managing a patient with a history of severe insect sting reactions involves a multi-pronged approach:
- Epinephrine Auto-injector: Immediate access to and proper training on the use of an epinephrine auto-injector is essential.
- Medical Identification: Patients should wear medical identification jewelry or carry a card alerting medical personnel to their allergy and the need for prompt epinephrine administration.
- Immunotherapy: IVIT is usually recommended to reduce the risk of future reactions. The type of immunotherapy is highly individualized based on the severity and nature of previous reactions.
- Emergency Plan: Develop a comprehensive emergency plan that includes procedures to follow in case of a sting, including calling emergency services and seeking immediate medical attention.
- Sting Avoidance: Educate the patient on strategies to avoid insect stings, such as wearing protective clothing, avoiding scented products, and being cautious near potential stinging insects.
Regular follow-up appointments with an allergist/immunologist are critical to monitor the patient’s response to treatment and adjust strategies as needed. The goal is to minimize the risk of life-threatening reactions.
Q 14. Explain the different types of insect allergy diagnostic tests available.
Several diagnostic tests help identify insect allergies:
- Skin Prick Test: This involves placing a small amount of diluted venom extract on the skin and pricking it. A positive reaction (wheal and flare) indicates an allergy. This is a quick, relatively inexpensive method, and the result is generally visible within 15-20 minutes. It’s a common first-line approach.
- Intradermal Test: A more sensitive test than skin prick, involving injecting a smaller amount of diluted venom intradermally. This is used if skin prick tests are negative, but there is still a high clinical suspicion of allergy.
- Serum-Specific IgE (sIgE) Test: This blood test measures the level of IgE antibodies specific to certain insect venoms. A high IgE level suggests allergy. This is a useful tool particularly in patients with skin conditions that interfere with skin testing.
- Component-Resolved Diagnostics (CRD): As discussed earlier, this blood test identifies the specific venom components causing the allergy.
The choice of test depends on several factors, including the patient’s history, clinical presentation, and the available resources. Often, a combination of tests is used for a comprehensive evaluation.
Q 15. What are the advantages and disadvantages of each diagnostic method?
Insect allergy diagnosis relies on several methods, each with its own strengths and weaknesses. Let’s compare two primary techniques: skin prick testing (SPT) and radioallergosorbent test (RAST).
Skin Prick Test (SPT):
- Advantages: SPT is quick, inexpensive, relatively easy to perform, and provides immediate results. It’s highly sensitive for detecting IgE-mediated allergies.
- Disadvantages: SPT can be affected by skin conditions (e.g., eczema), medications (e.g., antihistamines), and prior infections, leading to false negatives or positives. It can also cause a local reaction, although usually mild. It doesn’t quantify the level of allergy.
Radioallergosorbent Test (RAST):
- Advantages: RAST is useful for patients who cannot undergo SPT due to medication use, skin conditions, or severe reactions. It’s a quantitative test, meaning it measures the level of IgE antibodies.
- Disadvantages: RAST is more expensive and time-consuming than SPT, with results taking days to weeks. It’s less sensitive than SPT in some cases and can produce false negatives, especially at low IgE levels. It also requires a blood sample.
Choosing the right method depends on the patient’s clinical presentation, medical history, and resource availability. Often, both tests are used complementarily for a comprehensive diagnosis.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you interpret a positive and negative skin prick test result?
Interpreting skin prick test results is straightforward. A positive result shows a wheal (a raised, itchy bump) at the test site, typically larger than 3 mm in diameter compared to the negative control. This indicates a likely allergic reaction to the specific insect allergen tested. The size of the wheal can sometimes correlate with the severity of the reaction, but this is not always reliable.
A negative result means there’s no significant wheal formation, suggesting that the patient likely does not have an IgE-mediated allergy to that insect allergen. It is important to note that negative results do not completely rule out allergy as other mechanisms might still be involved. A negative result in the setting of a strong clinical history should prompt further investigation.
Example: A patient with a history of bee sting reactions undergoes SPT. A large wheal appears at the bee venom site, but not at the saline control site. This is interpreted as a positive result, consistent with a bee venom allergy.
Q 17. Discuss the role of RAST (Radioallergosorbent test) in insect allergy diagnosis.
RAST (Radioallergosorbent test) plays a crucial role in insect allergy diagnosis by measuring the level of specific IgE antibodies in the blood against insect venom or body extracts. This provides a quantitative measure of sensitization, offering more precise information than the qualitative SPT. It helps determine the severity and type of allergic response a patient might have to a particular insect. It is particularly useful in cases where SPT is not feasible.
Clinical Application: If a patient has a history of insect sting reactions but SPT is contraindicated due to medication or skin conditions, a RAST can help determine the allergen(s) causing their reaction. The RAST result informs the decision to proceed with immunotherapy and helps determine appropriate starting doses of venom for immunotherapy.
Q 18. How do you determine the appropriate dose of immunotherapy for a patient?
Determining the appropriate dose of venom immunotherapy requires careful consideration of several factors. It’s not a one-size-fits-all approach.
- Severity of past reactions: Patients with severe systemic reactions (anaphylaxis) usually require a more cautious up-dosing schedule compared to those with only local reactions.
- Skin test results: While SPT provides qualitative information, the degree of reaction can help guide initial dose selection. More pronounced wheal and flare reactions would suggest a lower starting dose.
- RAST results: RAST results provide a quantitative measure of IgE antibodies, providing another measure to inform dosing. High IgE levels often necessitate a more gradual approach.
- Patient history: Co-morbidities like asthma or cardiovascular disease might necessitate a more conservative up-dosing regimen.
Typically, immunotherapy starts with a very low dose of venom and gradually increases the dose over many months until a maintenance dose is achieved. This process is closely monitored, and dose adjustments are made according to the patient’s response. A skilled allergist is essential for carefully managing this process to minimize the risks of adverse reactions.
Q 19. What are the contraindications for insect venom immunotherapy?
Several contraindications exist for insect venom immunotherapy (VIT). It is crucial to exclude these before initiating treatment:
- Uncontrolled asthma or other significant medical conditions: Poorly managed asthma or severe cardiovascular conditions can significantly increase the risk of severe reactions during immunotherapy.
- Recent severe allergic reaction: Patients who have experienced severe systemic reactions within the past few months are generally not candidates.
- History of anaphylaxis to other allergens: Individuals demonstrating severe reactions to various allergens might exhibit heightened sensitivity to venom immunotherapy.
- Autoimmune disease: Immunotherapy can potentially worsen autoimmune disease.
- Pregnancy or breastfeeding: Immunotherapy is generally deferred during pregnancy and breastfeeding.
- Active infection: Immunotherapy is deferred until infection resolves.
- Use of beta-blockers: Beta-blockers can impair the body’s response to epinephrine and therefore must be carefully managed in individuals initiating immunotherapy.
A thorough evaluation of the patient’s medical history and current health is crucial before initiating VIT. Each case must be assessed individually to determine suitability.
Q 20. How do you monitor patients undergoing insect venom immunotherapy?
Monitoring patients undergoing VIT is crucial for ensuring safety and efficacy. This involves regular visits to the allergist’s office during the initial up-dosing phase and at intervals during the maintenance phase. Monitoring includes:
- Observation for local and systemic reactions after each injection: Close observation for at least 30 minutes post-injection is standard practice. This can involve monitoring vital signs, skin reactions, respiratory status, etc.
- Documentation of reactions: Detailed record keeping of the dose, route of administration, and reaction severity is essential for tracking the patient’s progress.
- Regular allergy testing (SPT/RAST): Testing can be performed periodically to monitor IgE levels and to confirm continued desensitization.
- Patient education: It is vital to educate patients about recognizing and managing potential side effects.
- Emergency preparedness: Patients should carry an epinephrine auto-injector and understand how to use it.
The frequency and type of monitoring may be adjusted based on the patient’s response and any adverse events experienced.
Q 21. Describe the management of adverse reactions during immunotherapy.
Managing adverse reactions during VIT is paramount. The severity of the reaction determines the management approach. Mild reactions (local swelling, itching, redness) can usually be managed with observation and supportive measures like antihistamines.
Severe reactions (anaphylaxis) require immediate intervention: This involves the prompt administration of epinephrine (adrenaline), oxygen, and supportive care. Patients experiencing anaphylaxis should immediately be transported to the nearest emergency department for monitoring and further treatment. A multidisciplinary team approach, including emergency medicine physicians, critical care specialists, and allergists, may be needed for severe reactions.
After an adverse reaction: The dose of immunotherapy may need to be adjusted or the treatment might be temporarily interrupted. A careful reassessment is needed to determine if and when VIT can be safely resumed. A thorough investigation of the event is conducted to identify contributing factors and to modify the management plan.
Q 22. What are the challenges in diagnosing insect allergies in children?
Diagnosing insect allergies in children presents unique challenges compared to adults. One major hurdle is the difficulty in obtaining a reliable history. Young children may not be able to articulate their symptoms clearly, and parents might misinterpret reactions or attribute them to other causes. Additionally, children’s immune systems are still developing, making their reactions sometimes unpredictable and less consistent than those seen in adults. For example, a child might have a mild reaction to a bee sting one time and a severe anaphylactic reaction the next. Another challenge lies in the fact that symptoms can mimic other conditions, such as viral infections or other allergies, potentially leading to misdiagnosis. Finally, skin prick tests, a common diagnostic tool, can be less reliable in young children due to factors like skin sensitivity and the difficulty in obtaining a good test sample. Accurate diagnosis often requires a combination of careful history-taking, physical examination, allergy testing, and sometimes observation of reactions following controlled exposure.
Q 23. Discuss the role of genetic factors in the development of insect allergies.
Genetic factors play a significant role in the predisposition to insect allergies. While a single gene doesn’t directly cause insect allergy, research points to a strong inherited component. Individuals with a family history of allergies, particularly asthma, eczema, or other insect sting allergies, are at a much higher risk. This suggests the involvement of multiple genes influencing immune system development and responsiveness. Specific genes related to immunoglobulin E (IgE) production and immune cell function are being investigated, but the exact mechanisms are still under exploration. Think of it like this: you might inherit a tendency towards a stronger allergic response, making you more susceptible to developing an allergy if exposed to insect venom. It’s not a guaranteed outcome, environmental factors are crucial, but it significantly increases the likelihood.
Q 24. Explain the pathophysiology of insect allergy.
The pathophysiology of insect allergy involves a complex interplay between the immune system and insect venom proteins. Upon the first exposure (sensitization), the immune system identifies certain proteins in the venom as foreign substances (allergens). This triggers the production of IgE antibodies specific to these allergens. These IgE antibodies attach to mast cells and basophils, which are immune cells found in tissues. Subsequent exposure to the same insect venom leads to the cross-linking of these IgE antibodies by the venom allergens, causing the mast cells and basophils to release a cascade of inflammatory mediators such as histamine, leukotrienes, and prostaglandins. These mediators trigger the characteristic symptoms of an allergic reaction—ranging from mild hives and itching to life-threatening anaphylaxis involving airway swelling, hypotension, and circulatory collapse. The severity of the reaction depends on the amount of venom injected, the individual’s level of sensitization, and the release of these mediators.
Q 25. Describe the different types of insect allergens.
Insect allergens are diverse and vary depending on the insect species. Hymenoptera venom (bees, wasps, hornets, ants) contains a complex mixture of proteins, the most common of which include phospholipase A2, hyaluronidase, and various other enzymes. These proteins have different allergenic potentials, meaning some provoke stronger allergic reactions than others. For example, phospholipase A2 is a major allergen in bee venom, frequently responsible for severe reactions. Other insects, like cockroaches, moths, and dust mites, also produce allergens that can trigger allergic responses. These allergens are often found in their feces, shed body parts, and saliva. Identifying the specific allergens causing a reaction is crucial for targeted diagnosis and treatment, which is often achieved through allergy testing using specific extracts.
Q 26. How do you assess the severity of an insect allergy?
Assessing the severity of an insect allergy involves considering both the reaction’s symptoms and their potential impact on the individual. Mild reactions might include localized swelling, itching, and hives at the sting site. Moderate reactions could involve more widespread hives, nausea, vomiting, or difficulty breathing. Severe reactions are defined as anaphylaxis, characterized by widespread swelling (angioedema), difficulty breathing (bronchospasm), hypotension (low blood pressure), and loss of consciousness. The severity is often graded based on the specific symptoms experienced and the level of medical intervention required. A detailed history of past reactions and the patient’s overall health status are also important considerations. For instance, a person with a history of anaphylaxis following an insect sting is at significantly greater risk of a severe reaction upon future stings compared to someone with only mild symptoms.
Q 27. What are the latest advancements in insect allergy diagnosis and treatment?
Advancements in insect allergy diagnosis are focusing on improved allergy testing methodologies, such as component-resolved diagnostics (CRD). CRD allows for the identification of specific allergens within the insect venom, giving a more precise diagnosis and tailoring treatment. In treatment, advancements include the development of more effective immunotherapy approaches, including sublingual immunotherapy (SLIT), which involves placing allergen extracts under the tongue. SLIT is proving to be a viable alternative to traditional injections. There’s also ongoing research in developing new drugs and therapies targeting specific inflammatory pathways in allergic reactions, such as monoclonal antibodies to inhibit IgE activity. Another area of investigation is using innovative technologies to improve the delivery of venom immunotherapy, and development of novel venom allergen vaccines.
Q 28. Describe the importance of patient education in insect allergy management.
Patient education is paramount in insect allergy management. It empowers individuals to understand their condition, avoid triggers, and manage potential reactions effectively. Education should cover the identification of allergenic insects, ways to prevent stings (e.g., wearing protective clothing outdoors, avoiding perfumes and bright colors), the recognition of early allergy symptoms, and the proper use of emergency medications like epinephrine auto-injectors (e.g., EpiPen). Patients should know when and how to seek medical attention, the importance of carrying their medication at all times, and the need for regular follow-up with their allergist. Providing clear, concise, and accessible information through various means – printed materials, interactive websites, and individual consultations – is key to ensuring patients are well-equipped to handle their allergies and avoid potentially life-threatening situations.
Key Topics to Learn for Your Insect Allergy Testing Interview
- Immunology of Insect Allergies: Understand the mechanisms behind insect sting and bite allergies, including IgE-mediated reactions, mast cell degranulation, and the role of various inflammatory mediators.
- Skin Prick Testing (SPT) and Intradermal Testing: Master the procedures, interpretation of results, and limitations of these common diagnostic tests. Be prepared to discuss potential false positives and negatives.
- Component-Resolved Diagnostics (CRD): Learn about the benefits of CRD in identifying specific allergens within insect venoms or saliva and how this impacts patient management and treatment strategies.
- Serum-Specific IgE Testing: Understand the role and limitations of measuring specific IgE antibodies against insect allergens. Discuss the interpretation of quantitative results and their clinical significance.
- Allergen-Specific Immunotherapy (SIT): Be familiar with the principles, procedures, and risks associated with venom immunotherapy for insect sting allergy. Discuss patient selection criteria and monitoring strategies.
- Interpreting Patient History and Clinical Presentation: Develop your skills in recognizing relevant symptoms and correlating them with diagnostic test results to create an accurate diagnosis.
- Emergency Management of Anaphylaxis: Understand the recognition, treatment, and prevention of severe allergic reactions to insect stings and bites. Be prepared to discuss the use of epinephrine and other supportive measures.
- Ethical Considerations and Patient Counseling: Discuss the importance of informed consent, managing patient expectations, and providing clear and empathetic communication regarding test results and treatment options.
- Quality Control and Assurance in Allergy Testing: Understand the importance of maintaining accurate and reliable testing procedures, including proper handling of reagents and adherence to standardized protocols.
Next Steps
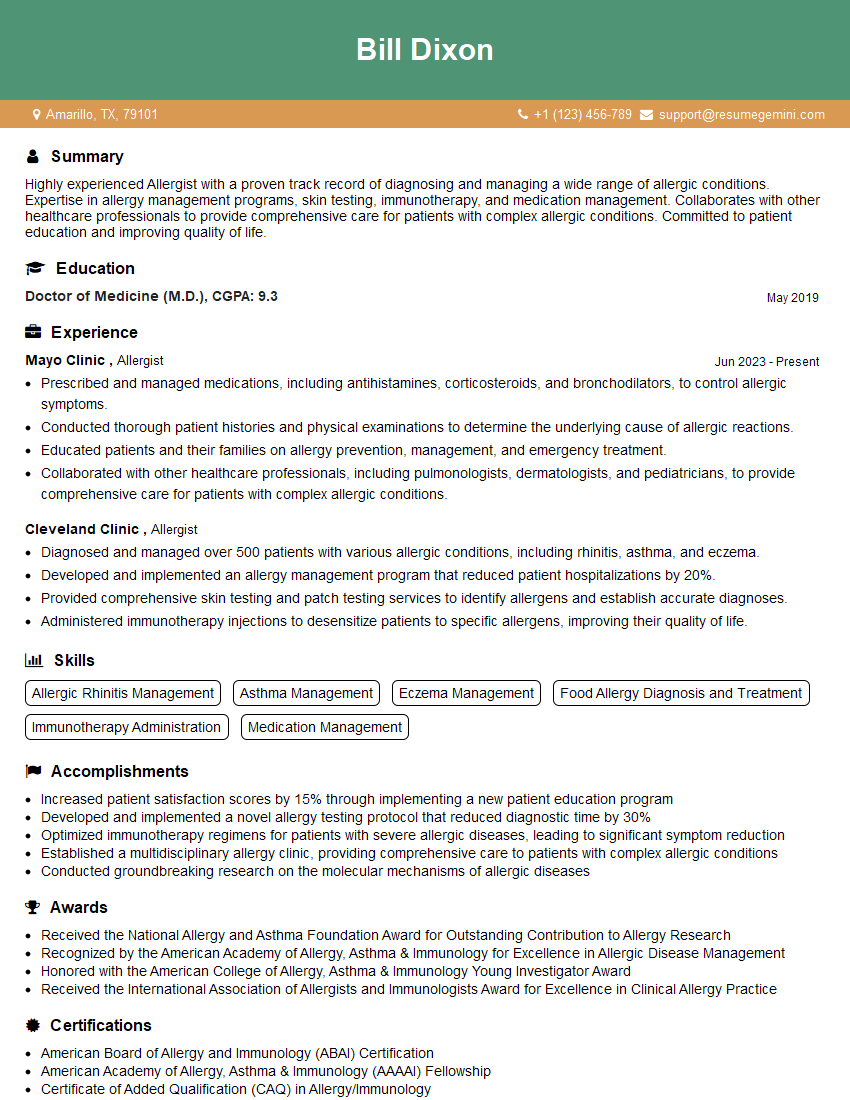
Mastering Insect Allergy Testing opens doors to a rewarding career in a field with high demand. Demonstrating expertise in this area significantly strengthens your candidacy for specialized roles. To enhance your job prospects, create a strong, ATS-friendly resume that showcases your skills and experience effectively. ResumeGemini is a valuable resource for building a professional and impactful resume. We offer examples of resumes specifically tailored to the Insect Allergy Testing field to help you present your qualifications in the best possible light.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.