Preparation is the key to success in any interview. In this post, we’ll explore crucial Knowledge of current trends and best practices in mental health interview questions and equip you with strategies to craft impactful answers. Whether you’re a beginner or a pro, these tips will elevate your preparation.
Questions Asked in Knowledge of current trends and best practices in mental health Interview
Q 1. Describe the current trends in evidence-based practices for treating anxiety disorders.
Evidence-based treatments for anxiety disorders are constantly evolving, but several approaches consistently demonstrate effectiveness. Cognitive Behavioral Therapy (CBT) remains a cornerstone, focusing on identifying and modifying negative thought patterns and maladaptive behaviors contributing to anxiety. Exposure therapy, a key component of CBT, gradually exposes individuals to feared situations or objects to reduce avoidance and anxiety responses. Acceptance and Commitment Therapy (ACT) helps individuals accept difficult emotions and thoughts without judgment, focusing on values-based actions. Mindfulness-based interventions, like Mindfulness-Based Cognitive Therapy (MBCT), teach techniques to cultivate present moment awareness and manage anxious thoughts and feelings. Pharmacological interventions, such as selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs), are also frequently used, often in conjunction with psychotherapy.
Example: A patient with social anxiety might benefit from CBT targeting negative self-talk before social situations (e.g., ‘I’m going to embarrass myself’), combined with gradual exposure to social settings, starting with less anxiety-provoking situations and progressively increasing the challenge. An ACT approach would emphasize acceptance of anxiety feelings as part of the human experience and focus on pursuing valued activities despite anxiety.
Q 2. What are the ethical considerations surrounding the use of telehealth in mental health?
Telehealth offers significant access improvements to mental healthcare but raises several ethical concerns. Confidentiality is paramount; ensuring secure platforms and adherence to HIPAA regulations is crucial. Informed consent must be obtained, explicitly addressing technological limitations and potential risks. Competence in providing telehealth services must be maintained; therapists need training in adapting their therapeutic approach to the virtual environment. Jurisdictional boundaries need careful consideration, as licenses and regulations vary across states or countries. Technological equity is also a concern; ensuring access for those lacking reliable internet or devices is vital. Finally, emergency situations require protocols to ensure patients can access appropriate care when needed.
Example: A therapist using telehealth must ensure their platform uses end-to-end encryption and adheres to all relevant data privacy regulations. They must also have a clear plan for handling emergencies, such as a patient experiencing a severe panic attack.
Q 3. Explain the differences between CBT and DBT therapies and when each is most effective.
Both Cognitive Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT) are evidence-based treatments, but they differ in their focus. CBT primarily targets maladaptive thoughts and behaviors, helping individuals identify and modify negative thought patterns and develop more adaptive coping mechanisms. It’s highly structured and goal-oriented. DBT, on the other hand, is more comprehensive and emphasizes emotional regulation, distress tolerance, and interpersonal effectiveness skills, in addition to cognitive restructuring. It’s particularly useful for individuals with borderline personality disorder and other conditions characterized by intense emotions and unstable relationships.
When each is most effective: CBT is effective for various anxiety disorders, depression, and other conditions characterized by problematic thoughts and behaviors. DBT is more suited to individuals struggling with intense emotions, self-harm behaviors, and difficulties in relationships. A patient with generalized anxiety might benefit from CBT’s focus on managing anxious thoughts and developing coping skills, while a patient with borderline personality disorder could benefit from DBT’s emphasis on emotional regulation and interpersonal skills.
Q 4. How do you stay up-to-date on the latest research and best practices in mental health?
Staying current in mental health requires a multifaceted approach. I regularly read peer-reviewed journals such as the Journal of Consulting and Clinical Psychology and American Psychologist. I actively participate in professional organizations like the American Psychological Association (APA), attending conferences and webinars to learn about the latest research and best practices. I also engage in continuing education courses to maintain my licensure and enhance my expertise. Furthermore, I utilize online resources like PubMed and PsycINFO to search for relevant research articles. Maintaining a network of colleagues in the field and discussing current trends and clinical challenges provides valuable insights.
Q 5. Discuss the role of trauma-informed care in mental health treatment.
Trauma-informed care is a fundamental shift in how mental health services are delivered. It recognizes the pervasive impact of trauma—including abuse, neglect, violence, or significant loss—on individuals’ mental and physical health. A trauma-informed approach emphasizes safety, trustworthiness, choice, collaboration, and empowerment. It avoids triggering past trauma, fostering a supportive and understanding environment where individuals feel safe to share their experiences. Clinicians receive specialized training to understand the impact of trauma on the brain and behavior. Therapeutic techniques are adapted to address the unique needs of trauma survivors. This involves creating a safe therapeutic relationship built on trust and respect.
Example: A trauma-informed therapist might avoid using language that could be triggering for a survivor of domestic violence, ensure the client feels in control of the therapeutic process, and collaborate to create goals and treatment plans. They might utilize techniques like EMDR or somatic experiencing to help process traumatic memories.
Q 6. What are some common barriers to accessing mental healthcare, and how can they be addressed?
Access to mental healthcare faces several significant barriers. Financial constraints are a major obstacle; many lack insurance coverage or affordable options. Geographic limitations restrict access for those in rural areas or underserved communities lacking mental health providers. Stigma surrounding mental illness continues to prevent many from seeking help. Lack of awareness about available resources and treatment options also contributes to underutilization of services. Systemic issues like long wait times and complex referral processes can deter individuals from seeking help.
Addressing these barriers requires a multi-pronged approach involving expanded insurance coverage, increasing the number of mental health professionals, particularly in underserved areas, reducing stigma through public awareness campaigns, simplifying access to services, and implementing telehealth solutions to overcome geographic barriers. Investing in community-based programs and peer support groups can also improve access and reduce reliance on costly professional services.
Q 7. Describe your experience with different assessment tools used in mental health.
My experience encompasses a wide range of assessment tools, tailored to the individual’s presenting concerns. For example, I frequently use standardized questionnaires like the Beck Depression Inventory (BDI-II) and the Generalized Anxiety Disorder 7-item scale (GAD-7) to assess symptom severity. For a more comprehensive evaluation, I might utilize the Minnesota Multiphasic Personality Inventory (MMPI-2-RF) or other personality inventories to gain insight into personality traits and psychological functioning. Neuropsychological testing is sometimes warranted to assess cognitive abilities in individuals with suspected cognitive impairment. Clinical interviews are a crucial component, allowing for detailed exploration of symptoms, history, and functioning. Structured clinical interviews provide a standardized approach for diagnostic assessment.
Example: If a client presents with symptoms of depression, I would likely use the BDI-II to quantitatively assess the severity of their depression. A clinical interview would provide qualitative information about the context and nature of their depressive symptoms, their personal history, and other relevant factors. This combination provides a comprehensive understanding of their condition, guiding the selection of appropriate treatment strategies.
Q 8. Explain the importance of cultural competency in mental health practice.
Cultural competency in mental health is paramount because it ensures that we provide effective and ethical care that’s sensitive to the unique experiences, beliefs, and values of individuals from diverse backgrounds. Ignoring cultural factors can lead to misdiagnosis, ineffective treatment, and a breakdown in the therapeutic relationship. It’s not simply about being polite; it’s about understanding how culture shapes a person’s worldview, their expression of symptoms, and their preferred methods of healing.
- Understanding Cultural Variations in Symptom Presentation: For example, depression might manifest differently across cultures. While sadness and hopelessness are common in Western presentations, other cultures might emphasize somatic complaints like fatigue or digestive issues.
- Respecting Cultural Beliefs and Practices: Some cultures may have traditional healing practices that can complement or even integrate with Western therapies. Ignoring these practices can be dismissive and undermine trust.
- Addressing Systemic Barriers: Cultural competency also involves acknowledging and addressing systemic barriers to care, such as language barriers, lack of culturally relevant resources, and implicit bias within the healthcare system itself.
In practice, cultural competency means actively seeking out knowledge about different cultures, being mindful of potential biases, and engaging in ongoing self-reflection. It requires developing strong communication skills that allow you to build rapport with clients from diverse backgrounds and adapt your approach to meet their specific needs.
Q 9. How do you handle difficult or challenging patient interactions?
Difficult patient interactions are inevitable in mental health work. My approach centers on de-escalation, empathy, and clear communication. I start by actively listening to the patient’s concerns, even if they’re expressed in a challenging manner. I validate their feelings, even if I don’t agree with their behavior. This doesn’t mean condoning inappropriate behavior, but acknowledging their emotional state is crucial for de-escalation.
- Setting Boundaries: It’s important to establish and maintain professional boundaries. This may involve calmly explaining limits on behavior and ensuring the safety of both myself and the patient.
- Seeking Consultation: If I’m struggling to manage a situation, I’ll always consult with a supervisor or colleague. This ensures I have support and to help develop an effective strategy.
- Self-Reflection: After a challenging interaction, I take time to reflect on what happened, what triggered the difficulty, and what I could have done differently. This is essential for continuous professional growth.
For instance, a patient might be angry about a perceived delay in treatment. Instead of reacting defensively, I would actively listen to their frustration, acknowledge the validity of their feelings about the wait, and then clearly explain the process and any reasons for delays. Sometimes, a simple apology for any inconvenience can significantly improve the interaction.
Q 10. Describe your crisis intervention skills and experience.
Crisis intervention is a core skill in mental health practice. My training equips me to assess a situation quickly, intervene effectively, and connect individuals with necessary resources. This involves a structured approach that prioritizes safety and stabilization.
- Assessment: I begin by assessing the immediate risk of harm to the individual or others, paying close attention to their verbal and non-verbal cues. This includes assessing for suicidal or homicidal ideation, substance abuse, and other contributing factors.
- Stabilization: The next step is to help the individual stabilize their emotional state. This might involve techniques like grounding exercises, deep breathing, or simply providing a calm and reassuring presence.
- Referral & Resource Provision: Once the immediate crisis is addressed, I connect the individual with appropriate resources, such as emergency services, inpatient hospitalization, or community support programs. I ensure a smooth transition to these resources and provide follow-up as needed.
I have experience handling a range of crises, including suicidal ideation, acute psychotic episodes, and domestic violence situations. My experience includes working in both inpatient and outpatient settings, giving me a broad understanding of different crisis management strategies. I also have training in techniques such as motivational interviewing and cognitive behavioral therapy (CBT), which can be invaluable during crisis intervention.
Q 11. What are your strategies for managing your own stress and maintaining your well-being as a mental health professional?
Maintaining my own well-being is not just important; it’s essential for effective practice. Burnout is a significant risk in this field, so prioritizing self-care is a non-negotiable aspect of my professional life.
- Setting Boundaries: I strictly adhere to work-life balance, avoiding overcommitment and ensuring I have time for personal activities and relaxation. I also diligently utilize paid time off.
- Mindfulness and Self-Reflection: I incorporate mindfulness practices, such as meditation or yoga, into my routine to reduce stress and improve self-awareness.
- Support Network: I maintain a strong support network of colleagues, friends, and family who understand the demands of this profession. Regular supervision provides a safe space to process challenging experiences.
- Seeking Professional Help: I understand the importance of seeking professional support myself when needed. This isn’t a sign of weakness but a testament to self-awareness and commitment to professional wellness.
I recognize that the emotional toll of working with individuals experiencing mental health challenges is substantial. Therefore, actively engaging in self-care practices allows me to maintain emotional resilience and continue providing compassionate, effective care.
Q 12. Discuss the role of technology in mental health treatment and its potential benefits and risks.
Technology plays an increasingly significant role in mental health treatment, offering both exciting opportunities and potential pitfalls. Telehealth, for instance, expands access to care for individuals in remote areas or those with mobility limitations.
- Benefits: Increased access to care, convenience for clients, cost-effectiveness in some cases, use of data analytics to improve treatment outcomes, and utilization of apps for self-monitoring and symptom tracking. Examples include virtual therapy sessions via video conferencing and mental health apps offering cognitive behavioral therapy (CBT) exercises.
- Risks: Privacy concerns regarding electronic health records, the digital divide excluding those without reliable internet access or technological literacy, potential for misdiagnosis through solely relying on virtual assessments, and a lack of the nuance possible in face-to-face interaction.
Ethical considerations are critical when using technology in mental healthcare. Data security, client confidentiality, and ensuring appropriate levels of clinical supervision for virtual practitioners are vital. It’s also essential to consider the potential for bias in algorithms used in mental health apps and to be mindful of the limitations of technology in assessing non-verbal cues.
Q 13. Explain your understanding of the DSM-5 and its implications for diagnosis and treatment.
The DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, 5th Edition) provides a standardized classification system for mental disorders. It’s a crucial tool for clinicians, aiding in diagnosis, communication, and treatment planning. However, it’s important to recognize its limitations.
- Diagnosis and Treatment: The DSM-5 provides criteria for various mental health conditions, allowing for a common language among professionals. Diagnosing a condition allows for targeted treatment, such as medication or specific therapeutic interventions. However, it’s not a rigid formula; clinical judgment is essential.
- Limitations: The DSM-5 is descriptive, not explanatory. It details symptoms but doesn’t necessarily explain the underlying causes of disorders. There’s also the possibility of over-diagnosis or misdiagnosis due to the complexity of mental illness. Comorbidity (co-occurrence of multiple disorders) is common, adding layers of complexity to diagnosis and treatment planning.
My approach is to use the DSM-5 as a guide, not a rigid rulebook. I carefully consider the individual’s complete clinical picture, including their history, presenting symptoms, and cultural context. The diagnostic label is only one aspect of a comprehensive assessment, informing but not defining the course of treatment.
Q 14. What is your approach to working with clients who have comorbid conditions?
Comorbidity, the co-occurrence of two or more mental health disorders, is incredibly common. My approach to working with clients who have comorbid conditions is holistic and integrated.
- Comprehensive Assessment: I begin with a thorough assessment to identify all relevant diagnoses and contributing factors. This goes beyond simply checking boxes; it includes a deep understanding of how the different conditions interact and impact the individual’s life.
- Integrated Treatment Plan: I develop an integrated treatment plan that addresses all the client’s conditions simultaneously, rather than treating them in isolation. This might involve a combination of medication, psychotherapy, and other supportive interventions.
- Collaboration: Collaboration is key. If appropriate, I work in consultation with other professionals, such as psychiatrists, to coordinate care and ensure the client receives the most comprehensive and effective treatment. This often involves regular communication and shared decision-making.
- Patient-Centered Approach: I prioritize a patient-centered approach, ensuring that the treatment plan is tailored to the individual’s unique needs, preferences, and goals. This includes open communication and shared decision-making throughout the process.
For example, a client might present with both depression and anxiety. Instead of treating the depression and anxiety separately, the treatment plan might address the underlying mechanisms linking the conditions. This integrated approach could involve therapies like CBT or mindfulness-based therapies that target both symptoms simultaneously.
Q 15. How do you ensure client confidentiality and maintain ethical boundaries?
Client confidentiality is paramount in mental health. It’s the cornerstone of the therapeutic relationship, built on trust and the understanding that shared information will remain private. Maintaining ethical boundaries is equally crucial, ensuring professional objectivity and avoiding any conflict of interest.
I adhere to strict confidentiality protocols, outlined in HIPAA (Health Insurance Portability and Accountability Act) and relevant state laws. This includes secure storage of client records, both physical and electronic; using encrypted communication methods; and only disclosing information with explicit client consent or when legally mandated (e.g., reporting child abuse or imminent harm to self or others).
Example: If a client discloses a past crime, I wouldn’t report it unless they were expressing a current intention to commit a similar act. My role focuses on supporting their well-being, not acting as a law enforcement agent. I’d maintain strict confidentiality while offering therapeutic support.
Ethical boundaries are maintained by avoiding dual relationships (e.g., becoming friends with a client), managing personal feelings appropriately (e.g., seeking supervision if I develop strong emotional reactions), and setting clear professional limits on the therapeutic relationship. Regular supervision and continuing education help me to maintain awareness and uphold these standards.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Describe your experience with different therapeutic modalities.
My therapeutic approach is eclectic, meaning I draw from various modalities to tailor treatment to each individual’s needs. I’m proficient in Cognitive Behavioral Therapy (CBT), which focuses on identifying and modifying negative thought patterns and behaviors. I also utilize Dialectical Behavior Therapy (DBT), particularly helpful for managing intense emotions and improving interpersonal skills, often employed with clients experiencing borderline personality disorder. Furthermore, I’m trained in Acceptance and Commitment Therapy (ACT), which emphasizes acceptance of difficult thoughts and feelings while focusing on valued actions.
Example: With a client struggling with anxiety, I might use CBT techniques to challenge their catastrophic thinking, DBT skills to manage emotional distress, and ACT to help them focus on their values and goals despite anxiety symptoms. The integration of these methods allows for a comprehensive and personalized therapeutic approach.
I also integrate mindfulness-based techniques, such as meditation and breathwork, into my practice, recognizing their effectiveness in stress reduction and self-awareness. The choice of modality is always guided by the client’s specific needs and preferences, in collaboration with them.
Q 17. Explain your understanding of the recovery model in mental health.
The recovery model emphasizes empowerment and person-centered care in mental health. It shifts the focus from illness management to promoting individual strengths, resilience, and self-determination. It recognizes that recovery is a unique and personal journey, not a linear process.
Instead of viewing mental illness as a life sentence, the recovery model acknowledges that individuals can live fulfilling lives despite their challenges. It emphasizes hope, self-efficacy, and the importance of peer support. Recovery is defined by the individual themselves, not by the absence of symptoms.
Practical Application: In practice, this means collaborating with clients to set their own goals and treatment plans. It involves actively listening to their experiences, honoring their values, and supporting them in developing coping mechanisms and pursuing their aspirations. This includes connecting them with community resources, support groups, and peer support specialists, recognizing the importance of social support in the recovery journey. It’s about moving from a medical model of ‘fixing’ someone to a holistic model of supporting personal growth and well-being.
Q 18. What are some common challenges faced by mental health professionals, and how do you address them?
Mental health professionals face many challenges. Burnout is a significant concern, stemming from high caseloads, emotional demands, and the inherent difficulties of working with individuals experiencing mental distress. Secondary Trauma, resulting from exposure to clients’ traumatic experiences, is another critical issue. Ethical Dilemmas, such as navigating confidentiality concerns or managing conflicting client needs, can be emotionally and professionally taxing.
Addressing these challenges involves:
- Self-Care: Prioritizing my own mental and physical well-being through exercise, mindfulness, and healthy boundaries is non-negotiable.
- Supervision and Peer Support: Regularly engaging in clinical supervision provides a safe space to process challenging cases and receive guidance.
- Continuing Education: Staying current with research and best practices helps me to effectively address diverse challenges.
- Utilizing Resources: Accessing organizational support services and employee assistance programs to address burnout and secondary trauma.
- Ethical Reflection and Consultation: Engaging in ethical decision-making models and seeking consultation when faced with complex ethical dilemmas.
Q 19. How do you incorporate patient preferences and values into treatment planning?
Incorporating patient preferences and values into treatment planning is central to person-centered care. This is not just about asking what the client wants but truly understanding their perspectives, goals, and beliefs.
Process:
- Active Listening and Empathy: Carefully listening to the client’s story, understanding their lived experience, and acknowledging their feelings.
- Collaborative Goal Setting: Working together to define specific, measurable, achievable, relevant, and time-bound (SMART) goals that align with the client’s values and priorities.
- Treatment Options Exploration: Presenting different treatment options, explaining their potential benefits and limitations, and allowing the client to make informed choices.
- Regular Feedback and Evaluation: Continuously monitoring the effectiveness of the treatment plan and making adjustments based on the client’s progress, preferences, and feedback.
Example: A client might prioritize improving their relationships over addressing specific symptoms. The treatment plan would then focus on building social skills and communication strategies, even if it means addressing other symptoms indirectly.
Q 20. Describe your experience with medication management in collaboration with a psychiatrist.
My experience with medication management is collaborative. I don’t prescribe medication; that’s the role of a psychiatrist. However, I work closely with psychiatrists to coordinate care and optimize outcomes for clients who are on medication.
My role involves:
- Assessment and Referral: Identifying clients who may benefit from medication and referring them to psychiatrists for evaluation.
- Monitoring and Communication: Regularly monitoring clients’ response to medication, including side effects and efficacy, and communicating this information to the psychiatrist.
- Psychotherapy Integration: Integrating psychotherapy with medication management to address underlying psychological factors and improve overall well-being.
- Education and Support: Educating clients about their medications, side effects, and how to manage them effectively.
Example: I might work with a client and their psychiatrist to adjust medication dosages based on the client’s reported symptoms and progress in therapy. Open communication between myself and the psychiatrist ensures a holistic approach to treatment.
Q 21. What are your strategies for building rapport and trust with clients?
Building rapport and trust is foundational to effective therapy. It’s about creating a safe and empathetic space where clients feel comfortable sharing their vulnerabilities.
My strategies include:
- Empathetic Listening: Actively listening to the client’s concerns without judgment, reflecting their feelings, and demonstrating genuine understanding.
- Building a Therapeutic Alliance: Collaboratively establishing the goals and direction of therapy, ensuring the client feels heard and involved in the process.
- Respectful Communication: Using clear and straightforward language, respecting the client’s privacy, and maintaining confidentiality.
- Cultural Sensitivity: Being mindful of cultural differences and adapting my approach to meet the client’s unique cultural needs and perspectives.
- Self-Disclosure (judiciously): Sharing relevant personal experiences when appropriate can humanize the therapeutic process and foster a deeper connection. However, this is done with great caution and only when it serves the client’s needs.
Example: Starting a session by asking how the client is doing, showing interest in their life outside therapy, and acknowledging their effort to attend therapy, are all simple ways to show respect and build a positive rapport.
Q 22. How do you handle situations where clients are resistant to treatment?
Resistance to treatment is common and often stems from a variety of factors, including fear, mistrust, lack of understanding, or a feeling of being overwhelmed. My approach focuses on building a strong therapeutic alliance based on empathy and collaboration. I start by actively listening to the client’s concerns and validating their feelings. I avoid pressuring them into anything and instead work collaboratively to identify their goals and collaboratively create a treatment plan tailored to their needs and preferences. This might involve exploring alternative approaches, adjusting the treatment frequency or intensity, or focusing on small, achievable steps rather than overwhelming changes. For example, if a client is resistant to medication, we might explore non-pharmacological interventions like mindfulness or CBT alongside psychoeducation about medication.
If resistance persists despite these efforts, I might utilize motivational interviewing techniques to help the client identify their own reasons for change and overcome ambivalence. Ultimately, the client’s autonomy is paramount. If a client remains firmly resistant and it’s clear treatment is not a good fit at this time, I will explore options for referral to other professionals or support services who may better meet their needs.
Q 23. Describe your understanding of the impact of social determinants of health on mental wellbeing.
Social determinants of health (SDOH) are the conditions in the environments where people are born, live, learn, work, play, worship, and age that affect a wide range of health, functioning, and quality-of-life outcomes and risks. These factors significantly impact mental wellbeing. For instance, poverty, lack of access to healthcare and education, food insecurity, unstable housing, discrimination, and exposure to violence are all strongly correlated with increased rates of mental health disorders and poorer treatment outcomes. A person living in poverty might experience chronic stress and lack the resources for adequate self-care, increasing their vulnerability to depression or anxiety. Similarly, systemic racism can lead to trauma and mental health challenges, and access to mental healthcare may be limited due to cost or geographical barriers in underserved communities.
Understanding SDOH is crucial for effective mental health practice. It necessitates a holistic approach that goes beyond addressing symptoms and considers the broader context of a client’s life. This may involve advocating for policy changes to address systemic inequalities, connecting clients with community resources like food banks or housing assistance, and collaborating with other professionals, such as social workers, to support client needs in a comprehensive way. Integrating this understanding into treatment planning is paramount for ensuring equitable and effective mental health care.
Q 24. What is your experience with working with diverse populations?
I have extensive experience working with diverse populations, including individuals from various cultural backgrounds, ethnicities, sexual orientations, gender identities, religious beliefs, and socioeconomic statuses. I’ve learned the importance of cultural humility—a lifelong commitment to self-reflection and learning, acknowledging power imbalances, and working in partnership with clients to understand their unique perspectives. This includes actively seeking out and understanding their cultural beliefs about mental health, their preferred communication styles, and their potential experiences with discrimination.
For example, working with a client from a collectivist culture might necessitate a different approach than working with a client from an individualistic culture. In collectivist cultures, family involvement may be vital to effective treatment, whereas respecting client privacy and autonomy is crucial in individualistic cultures. Understanding these cultural nuances allows me to tailor my approach to resonate with each individual while ensuring a safe, empathetic, and effective therapeutic relationship. I actively engage in ongoing professional development to expand my cultural competence and sensitivity, recognizing that this is a continuous process of learning and adaptation.
Q 25. How do you document client progress and outcomes effectively?
Effective documentation of client progress and outcomes is crucial for ethical practice, continuity of care, and ensuring accountability. My documentation adheres to HIPAA and other relevant legal and ethical standards and focuses on being clear, concise, and objective. I utilize a combination of methods to capture client information, including progress notes that describe sessions and interventions; assessment tools that measure symptoms and functioning; and outcome measures that track changes over time. Progress notes usually include the date, the client’s presenting issues, the therapeutic interventions used, the client’s response to these interventions, and any plans for future sessions.
For example, when using a standardized outcome measure like the PHQ-9 (Patient Health Questionnaire-9) for depression, I record the client’s score at each session and document any changes. I might also use a qualitative approach to describe behavioral changes, changes in the client’s mood and affect, and changes in their ability to cope with stressful events. I regularly review my documentation to ensure it is accurate, complete, and reflects the client’s progress comprehensively. This organized approach ensures all involved parties including the client, other clinicians, or insurance companies can understand the client’s journey and evaluate the effectiveness of the treatment.
Q 26. Explain your understanding of the role of supervision and continuing education in maintaining professional competence.
Supervision and continuing education are essential for maintaining professional competence and providing high-quality care. Supervision provides a valuable opportunity for feedback, reflection, and consultation on complex cases. A supervisor acts as a mentor, guiding me in ethical decision-making and providing support for challenges I encounter in my practice. This ensures the ongoing development of my skills and assists in mitigating risks and potential burnout.
Continuing education is equally crucial for staying abreast of the latest research, treatment modalities, and best practices in the field. This might involve attending workshops, conferences, taking online courses, or engaging in self-directed learning. For example, I regularly update my knowledge on evidence-based practices for specific disorders, and I make sure to remain knowledgeable about new diagnostic criteria, medications, and ethical guidelines. By proactively seeking supervision and continuing education, I maintain a high level of professional competence and client safety.
Q 27. Describe your experience with utilizing electronic health records (EHRs) in mental health practice.
My experience with electronic health records (EHRs) in mental health practice has been extensive and positive. I am proficient in using EHR systems to document client information securely, manage appointments, generate reports, and communicate with other healthcare professionals. EHRs streamline administrative tasks, enhance data security, and facilitate better coordination of care. For example, I can easily access a client’s complete history, including previous diagnoses, treatment plans, and medication records, ensuring seamless continuity of care. I also utilize EHR’s capabilities to securely exchange information with other providers involved in the client’s treatment.
However, I also acknowledge that EHRs present challenges. The time required for accurate documentation can be substantial, impacting the time available for direct client interaction. Also, the potential for technological glitches and the need for training can be significant factors. It’s crucial to select and use EHR systems efficiently and effectively to maximize benefits while minimizing drawbacks. I am committed to using technology in a way that enhances, not detracts from, the therapeutic relationship and the provision of quality care.
Q 28. How do you utilize data and outcomes to inform your practice and improve client care?
Data and outcomes are essential for informing my practice and improving client care. I regularly review client data, including assessment scores, progress notes, and outcome measures, to evaluate the effectiveness of my interventions. This process involves both quantitative and qualitative analysis. For example, I might track changes in a client’s depression scores on the PHQ-9 over time to determine if the treatment is working. I also consider qualitative data like the client’s self-reported experiences and feedback to understand the broader impact of the treatment.
If the data indicates that a treatment isn’t effective, I collaborate with the client to adjust the treatment plan, explore alternative strategies, or potentially refer the client to another provider. This data-driven approach helps to optimize treatment outcomes and ensures that clients receive the most effective and appropriate care. Additionally, I utilize aggregate data to identify trends and patterns in client presentations, which in turn informs my professional development, and helps me advocate for improved services and resources for those in need.
Key Topics to Learn for Knowledge of current trends and best practices in mental health Interview
- Integrated Care Models: Understanding the collaborative approach between mental health and primary care, and the benefits of integrating physical and mental healthcare.
- Trauma-Informed Care: Applying principles of trauma-informed care in assessment, treatment planning, and intervention strategies. This includes recognizing the impact of trauma on behavior and mental health.
- Evidence-Based Practices (EBPs): Familiarity with current research supporting various therapeutic modalities (e.g., CBT, DBT, ACT) and their application in different populations.
- Technology in Mental Healthcare: Exploring the role of telehealth, mobile apps, and digital tools in delivering mental health services and their impact on access and outcomes.
- Cultural Competence and Diversity: Understanding the importance of culturally sensitive and appropriate assessment and treatment strategies for diverse populations.
- Ethical Considerations in Mental Health: Knowledge of ethical dilemmas, professional boundaries, confidentiality, and informed consent in mental health practice.
- Crisis Intervention and Risk Assessment: Understanding methods for identifying and managing individuals in mental health crisis, including suicide risk assessment and intervention.
- Recovery-Oriented Care: Focusing on the client’s strengths and empowering them to achieve their goals and live fulfilling lives, rather than solely focusing on symptom reduction.
- Data-Driven Decision Making: Understanding the importance of utilizing data and outcomes to evaluate the effectiveness of interventions and adjust treatment plans accordingly.
- Current Legislation and Policy: Being aware of relevant mental health legislation, policies, and their impact on service delivery and access to care.
Next Steps
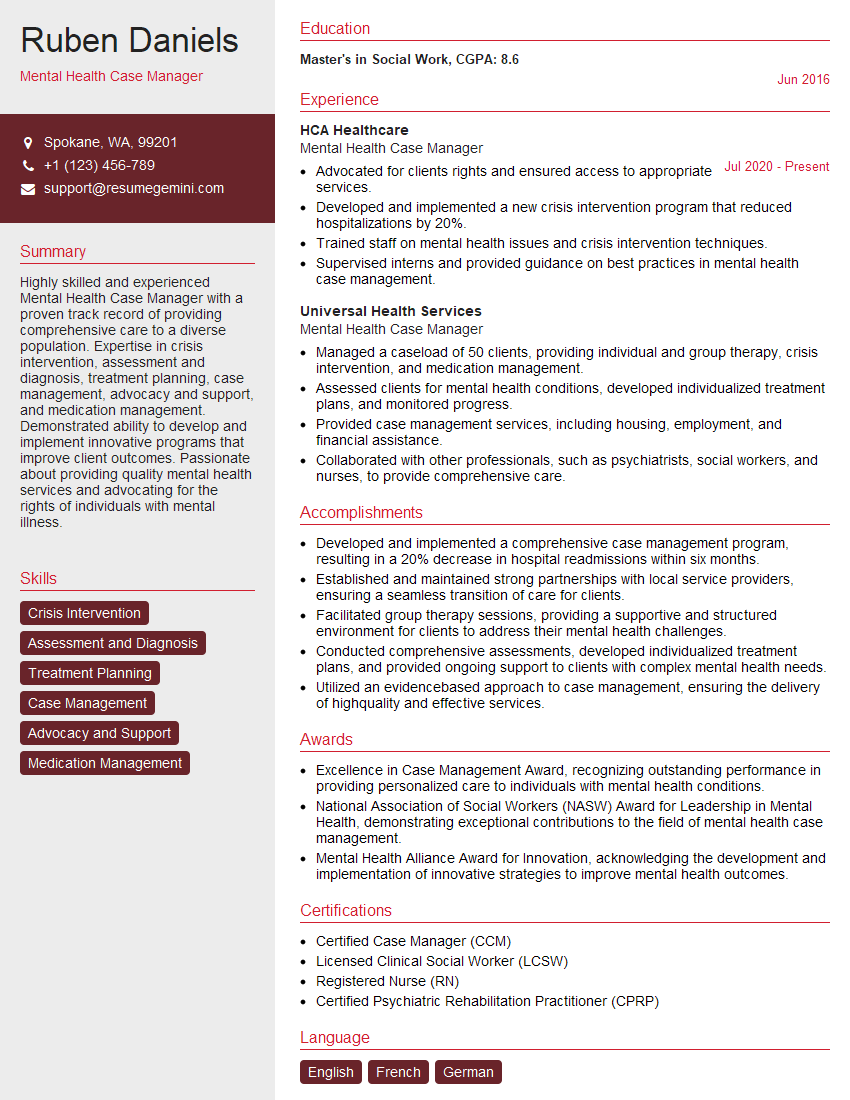
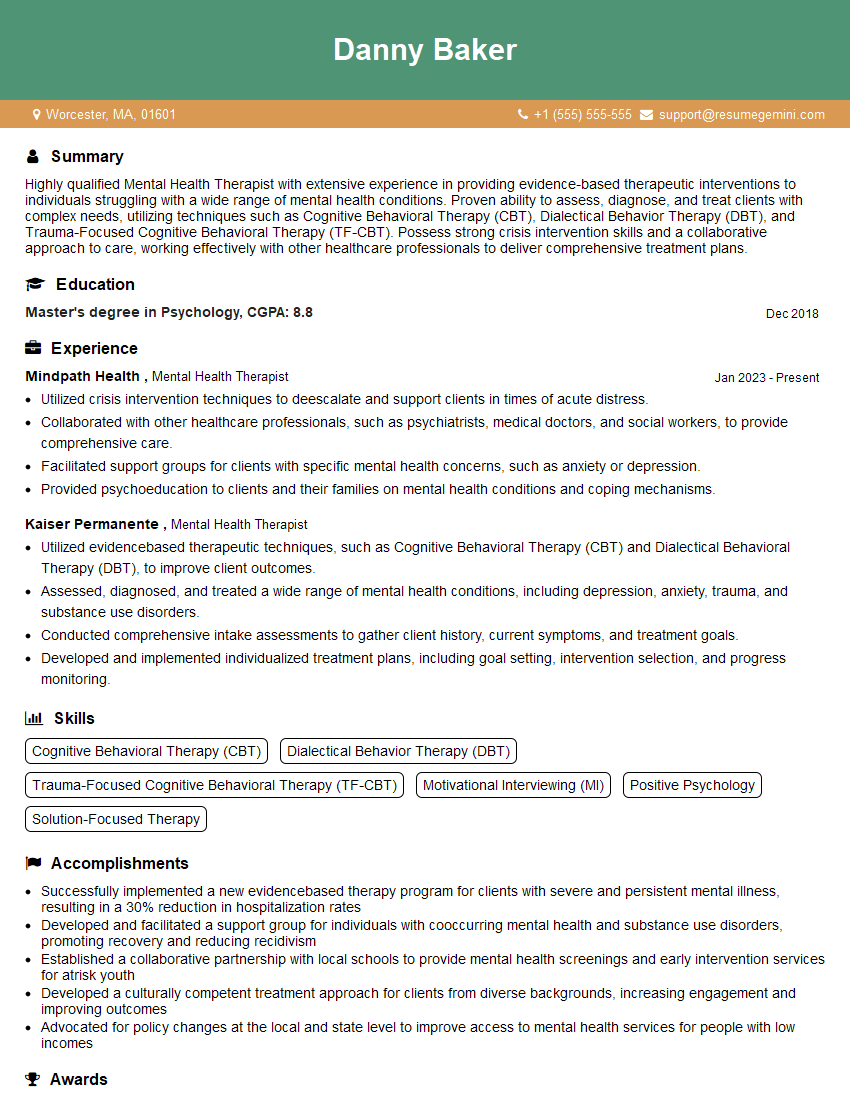
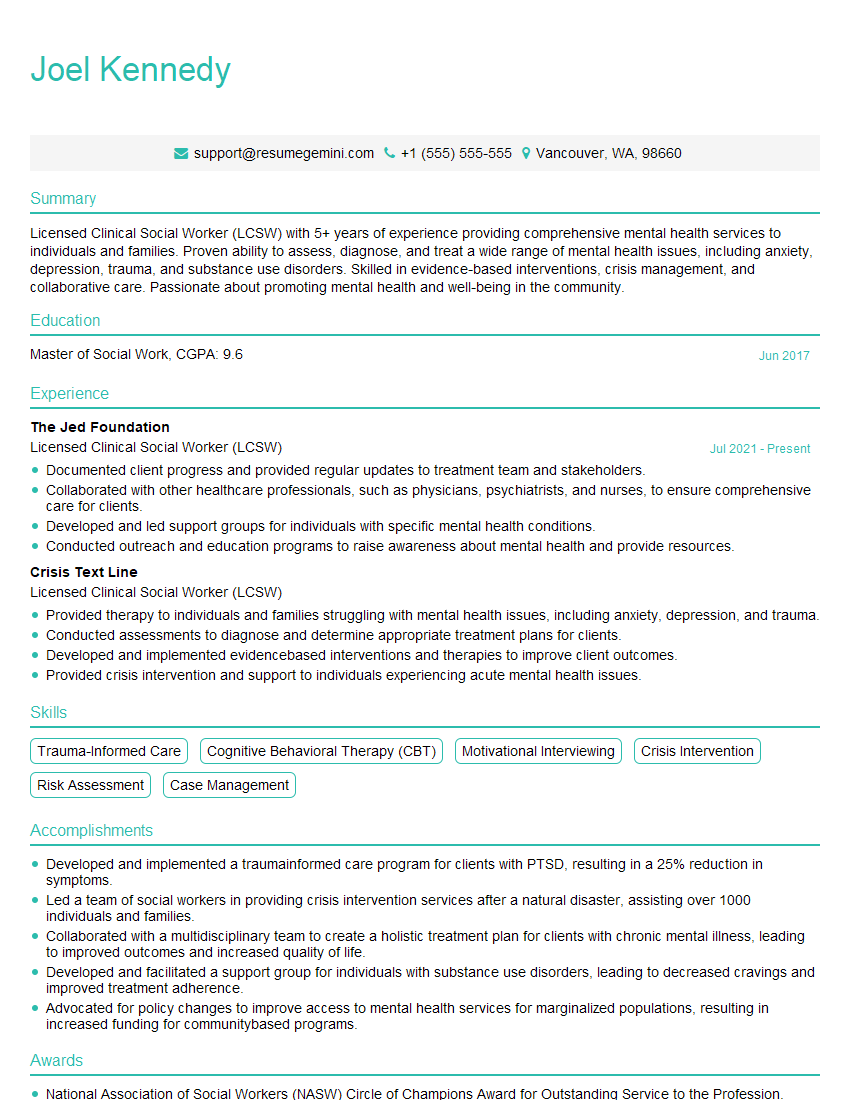
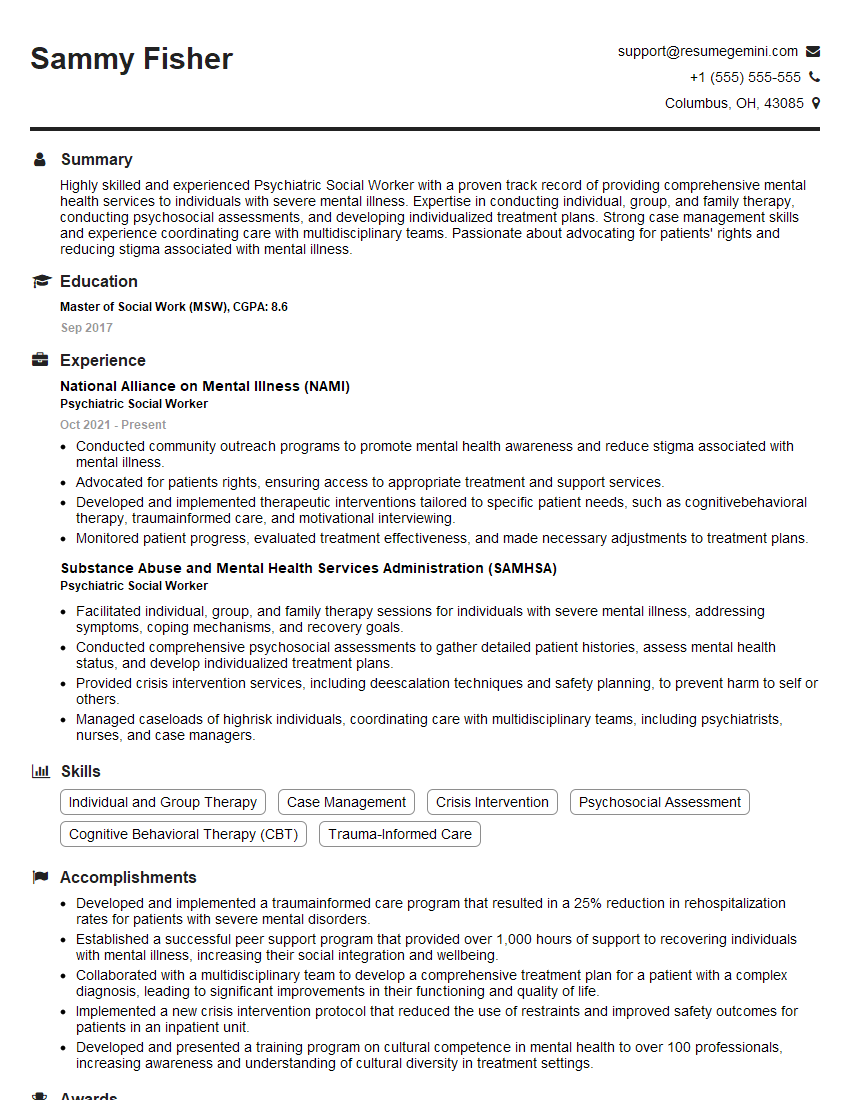
Mastering knowledge of current trends and best practices in mental health is crucial for career advancement in this dynamic field. Demonstrating this expertise through a strong resume is key to securing your dream role. To significantly enhance your job prospects, create an ATS-friendly resume that highlights your skills and experience effectively. We highly recommend using ResumeGemini, a trusted resource for building professional resumes. ResumeGemini provides examples of resumes tailored to showcasing expertise in current trends and best practices in mental health, helping you present yourself as a highly qualified candidate.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hi, I have something for you and recorded a quick Loom video to show the kind of value I can bring to you.
Even if we don’t work together, I’m confident you’ll take away something valuable and learn a few new ideas.
Here’s the link: https://bit.ly/loom-video-daniel
Would love your thoughts after watching!
– Daniel
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.