Feeling uncertain about what to expect in your upcoming interview? We’ve got you covered! This blog highlights the most important Pediatric Neurometabolic Disorders interview questions and provides actionable advice to help you stand out as the ideal candidate. Let’s pave the way for your success.
Questions Asked in Pediatric Neurometabolic Disorders Interview
Q 1. Describe the diagnostic approach to suspected organic acidemias.
Suspecting an organic acidemia requires a multi-pronged diagnostic approach, starting with a thorough clinical evaluation. The hallmark is often a metabolic crisis presenting with lethargy, vomiting, poor feeding, and potentially respiratory distress. This is usually triggered by an illness or even fasting.
Laboratory investigations are crucial:
Newborn screening: Many organic acidemias are detectable through newborn screening programs, often identifying affected infants before they become symptomatic.
Urine organic acid analysis: This is a cornerstone of diagnosis, identifying abnormal elevations of specific organic acids excreted in the urine. For example, a high level of methylmalonic acid points towards methylmalonic acidemia.
Blood gas analysis: This helps assess acidosis, a common feature of organic acidemias.
Plasma amino acid analysis: Can reveal abnormalities in amino acid profiles related to specific defects in metabolic pathways.
Acylcarnitine profile: Measured in dried blood spots or plasma, this profiles specific acylcarnitine esters, revealing defects in fatty acid oxidation. Certain patterns can indicate specific organic acidemias.
Enzyme assays: While sometimes challenging to obtain due to tissue availability and variability, direct enzyme assays on a liver biopsy, fibroblast culture or leukocytes can offer definitive confirmation.
Genetic testing: Once a suspected diagnosis is formed based on the above, genetic testing can be done to confirm the diagnosis by identifying the underlying genetic defect.
Example: A newborn presents with lethargy, vomiting, and poor feeding following a viral infection. Urine organic acid analysis reveals elevated propionic acid. This strongly suggests propionic acidemia, which is then confirmed with genetic testing.
Q 2. Explain the role of newborn screening in detecting neurometabolic disorders.
Newborn screening is a critical public health intervention for detecting neurometabolic disorders. It involves analyzing a blood sample collected from a newborn infant shortly after birth, typically from the heel prick. This screening tests for a panel of conditions, including many organic acidemias, aminoacidopathies, and fatty acid oxidation disorders. Early detection is essential because these disorders often manifest in the first weeks or months of life, and prompt intervention can significantly mitigate the severity of long-term complications.
Impact of Early Detection: Early diagnosis allows for timely initiation of treatment, preventing or minimizing irreversible neurological damage. Imagine a scenario where a child with PKU remains undiagnosed: Their brain would be affected by the buildup of phenylalanine. Newborn screening catches this early allowing for dietary restriction to start immediately.
Limitations: While newborn screening is incredibly valuable, it’s not perfect. It has a limited panel of testable disorders, and false-positive and false-negative results can occur. Therefore, clinical suspicion remains crucial, especially if a child presents with symptoms suggestive of a neurometabolic disorder even after a normal newborn screen.
Q 3. Discuss the management of acute metabolic decompensation.
Acute metabolic decompensation is a life-threatening emergency requiring immediate and intensive medical management. It’s characterized by a rapid deterioration in a child’s clinical condition, often marked by neurological symptoms (lethargy, seizures, coma), respiratory distress, and metabolic acidosis. The cause is usually the buildup of toxic metabolites, such as organic acids or ammonia.
Management Principles:
Stabilization of vital signs: This includes managing airway, breathing, and circulation, often requiring intensive care support such as mechanical ventilation.
Correction of acidosis: Administering intravenous fluids and bicarbonate to correct the metabolic acidosis is essential.
Removal of toxic metabolites: Specific treatments depend on the underlying disorder. For instance, hemodialysis or hemoperfusion may be needed to remove toxic substances from the blood. Specific therapies might include medications that enhance detoxification pathways.
Nutritional support: Providing adequate calories and restricting specific metabolites through dietary modifications or specific formulations are essential.
Supportive care: This includes managing seizures with anticonvulsant medications, maintaining proper fluid and electrolyte balance, and addressing any infections.
Example: A child with maple syrup urine disease (MSUD) develops lethargy, vomiting, and seizures. Immediate management involves intensive care support, intravenous fluids, bicarbonate, and dietary restriction of branched-chain amino acids.
Q 4. What are the common clinical presentations of mitochondrial disorders in children?
Mitochondrial disorders are a heterogeneous group of diseases affecting the mitochondria, the powerhouses of the cells. They exhibit incredibly diverse clinical presentations, making diagnosis challenging. Common clinical features in children include:
Neurological symptoms: These are prevalent, ranging from developmental delay and hypotonia (low muscle tone) to seizures, stroke-like episodes, and encephalopathy (brain dysfunction).
Myopathy: Weakness and hypotonia, often affecting skeletal muscles, leading to exercise intolerance.
Cardiomyopathy: Heart muscle weakness leading to heart failure.
Gastrointestinal issues: Feeding difficulties, vomiting, diarrhea, hepatopathy (liver disease).
Respiratory problems: Shortness of breath and respiratory failure.
Lactate acidosis: An accumulation of lactate, a byproduct of energy metabolism, indicates that mitochondria are not functioning properly.
Clinical Presentation Variability: The severity and combination of symptoms vary greatly depending on the specific gene involved, the extent of mitochondrial dysfunction, and the tissues affected. Some children may exhibit severe symptoms from birth, whereas others may have milder, later-onset manifestations.
Example: One child might present with primarily myopathy (muscle weakness), while another might have severe neurological problems with developmental delay and seizures. A third might exhibit cardiac problems.
Q 5. Outline the principles of dietary management in phenylketonuria (PKU).
Phenylketonuria (PKU) is an inherited metabolic disorder where the body cannot break down phenylalanine, an essential amino acid. Dietary management is the cornerstone of PKU treatment, aimed at maintaining blood phenylalanine levels within the therapeutic range to prevent neurological damage.
Principles of Dietary Management:
Phenylalanine Restriction: The diet strictly limits dietary phenylalanine intake through carefully controlled intake of protein-containing foods (meat, dairy, eggs, nuts, legumes). Low-protein foods are utilized.
Tyrosine Supplementation: Tyrosine is synthesized from phenylalanine; when phenylalanine is restricted, tyrosine becomes essential, needing supplementation to ensure adequate levels.
Monitoring Blood Phenylalanine Levels: Regular blood tests monitor phenylalanine levels, guiding adjustments to dietary intake to maintain the therapeutic range.
Nutritional Completeness: The diet needs to be nutritionally complete, meeting the child’s energy and micronutrient requirements.
Specialized Formulas: Commercially available low-phenylalanine formulas often supplement the diet, providing essential amino acids and nutrients.
Individualized Approach: Dietitians and medical professionals customize dietary plans based on the child’s age, growth rate, and individual needs.
Practical Example: A child with PKU will follow a diet significantly lower in protein than typically recommended for their age. They will rely on special phenylalanine-restricted formulas and carefully measured portions of allowed foods. Regular blood tests ensure that their phenylalanine levels stay within the safe range, preventing neurological damage.
Q 6. Explain the genetic basis of several common lysosomal storage disorders.
Lysosomal storage disorders (LSDs) are a group of inherited metabolic disorders resulting from deficiencies of lysosomal enzymes. These enzymes break down complex molecules within lysosomes (cellular compartments). The deficiencies lead to the accumulation of undigested substrates, causing progressive damage to various organs and systems.
Genetic Basis: Each LSD is caused by a mutation in a different gene encoding a specific lysosomal enzyme. Examples:
Gaucher disease: Deficiency of glucocerebrosidase, leading to the accumulation of glucocerebroside in macrophages (immune cells).
Tay-Sachs disease: Deficiency of hexosaminidase A, leading to the accumulation of GM2 ganglioside in neurons.
Hunter syndrome: Deficiency of iduronate-2-sulfatase, leading to the accumulation of glycosaminoglycans (GAGs).
Hurler syndrome: Deficiency of α-L-iduronidase, leading to accumulation of GAGs.
Pompe disease: Deficiency of acid α-glucosidase, leading to accumulation of glycogen in various tissues.
Genetic Inheritance: Most LSDs are inherited in an autosomal recessive pattern, meaning that both parents must carry a mutated gene for the child to inherit the disorder. Some, like Hunter syndrome, are X-linked recessive, impacting mostly males.
Q 7. Describe the challenges in managing severe combined immunodeficiency (SCID).
Severe combined immunodeficiency (SCID) is a group of rare genetic disorders characterized by a profound deficiency in both B cells and T cells, leaving the affected infants with no functional adaptive immune system. This renders them extremely vulnerable to life-threatening infections.
Challenges in Management:
High risk of infection: The complete lack of adaptive immunity makes SCID children susceptible to opportunistic infections, including those that are usually harmless to other individuals. These infections can be life-threatening.
Sterile environment: Early management involves isolation in a sterile environment (often a bubble) until definitive treatment can be provided.
Treatment options: While hematopoietic stem cell transplantation (HSCT) is the curative treatment, it’s not always successful, and finding a suitable donor can be difficult. Gene therapy offers a promising alternative for some types of SCID, but it is not universally available or suitable for all SCID subtypes.
Long-term complications: Even with successful treatment, SCID children may face long-term complications such as growth retardation, chronic lung disease and other organ-specific issues. They also require lifelong monitoring.
Emotional and psychological impact: Managing SCID significantly impacts families and poses emotional and psychological challenges, demanding extensive education, support, and commitment.
Overall: SCID management is complex, multidisciplinary, and requires advanced medical care in specialized centers. Early diagnosis through newborn screening or other clinical suspicion, coupled with prompt intervention, is critical in improving outcomes.
Q 8. Discuss the role of enzyme replacement therapy in lysosomal storage disorders.
Enzyme replacement therapy (ERT) is a cornerstone treatment for many lysosomal storage disorders (LSDs). LSDs are a group of inherited metabolic diseases where a deficiency in a specific lysosomal enzyme leads to the accumulation of undigested substrates within cells, causing progressive damage. ERT aims to alleviate this by supplying the missing enzyme through intravenous infusions. The infused enzyme is designed to enter the cells and break down the accumulated substrates, reducing the severity of symptoms and slowing disease progression.
For example, in Pompe disease, a deficiency in acid alpha-glucosidase leads to glycogen accumulation in lysosomes. ERT with alglucosidase alfa helps to reduce glycogen buildup and improve muscle function. However, ERT is not a cure and has limitations. It may not reach all affected cells equally, and long-term efficacy can vary. Furthermore, not all LSDs are amenable to ERT, and the treatment can be expensive and require lifelong administration. Success is heavily dependent on early diagnosis and initiation of therapy.
Q 9. What are the long-term complications of untreated galactosemia?
Untreated galactosemia, a genetic disorder affecting galactose metabolism, can lead to a range of devastating long-term complications. The inability to properly metabolize galactose, a simple sugar, leads to its accumulation in various tissues and organs. This accumulation causes damage, particularly to the liver, brain, and eyes.
- Liver damage: Cirrhosis, jaundice, and liver failure can occur.
- Brain damage: Intellectual disability, speech delays, ataxia (lack of muscle coordination), and tremors are common.
- Eye problems: Cataracts, which can cause vision impairment or blindness, are frequently observed.
- Kidney problems: Renal dysfunction can develop.
- Ovarian failure: In females, premature ovarian failure can lead to infertility.
The severity of these complications varies depending on the specific type of galactosemia and the individual’s response to dietary management. Early diagnosis and prompt dietary restriction of galactose are crucial to minimizing these long-term effects. Even with early treatment, however, some residual effects are possible.
Q 10. Explain the pathophysiology of Leigh syndrome.
Leigh syndrome is a devastating neurometabolic disorder characterized by progressive degeneration of the central nervous system. It’s primarily caused by defects in mitochondrial function, the cellular powerhouses responsible for energy production. This results in impaired energy production within the brain and other tissues.
The pathophysiology is complex but involves mutations in genes that encode for proteins essential for mitochondrial respiratory chain complexes. These mutations impair the efficiency of oxidative phosphorylation (the process of generating ATP, the cell’s energy currency). The resulting energy deficiency affects multiple organs but manifests most severely in the developing brain, leading to neuronal damage and cell death. The specific clinical presentation varies depending on the affected gene and the severity of the mitochondrial dysfunction. Accumulation of toxic metabolites, such as lactic acid, can further contribute to neuronal damage. Imaging often reveals characteristic necrotic lesions in the basal ganglia and brainstem.
Q 11. Describe the differential diagnosis of hypotonia in a newborn.
Hypotonia, or decreased muscle tone, in a newborn is a non-specific finding that requires a thorough differential diagnosis. Many conditions can present with this symptom, ranging from benign to life-threatening. The approach requires a detailed history, physical examination, and often extensive investigations.
- Neuromuscular disorders: Muscular dystrophies, spinal muscular atrophies (SMAs), congenital myopathies.
- Metabolic disorders: Many inborn errors of metabolism can cause hypotonia, including organic acidemias, fatty acid oxidation disorders, and lysosomal storage diseases.
- Central nervous system disorders: Hypoxic-ischemic encephalopathy, infections (meningitis, encephalitis), chromosomal abnormalities (Down syndrome, Prader-Willi syndrome).
- Connective tissue disorders: Ehlers-Danlos syndrome.
- Endocrine disorders: Hypothyroidism.
- Other causes: Prenatal drug exposure, prematurity, and other genetic conditions.
The diagnostic pathway is iterative. Initial investigations typically include blood tests, genetic testing, and imaging (such as MRI of the brain and spine). Muscle biopsy or electromyography (EMG) might be necessary in certain cases. A multidisciplinary approach involving neurologists, geneticists, and metabolic specialists is often crucial for accurate diagnosis and management.
Q 12. Discuss the use of MRI in evaluating neurometabolic disorders.
MRI plays a vital role in evaluating neurometabolic disorders, offering detailed anatomical images of the brain and spinal cord. It is particularly useful for identifying structural abnormalities that can be associated with these disorders. Specific findings on MRI can help narrow the differential diagnosis.
For example, in Leigh syndrome, MRI might reveal characteristic lesions in the basal ganglia and brainstem. In other conditions, MRI may show diffuse brain atrophy, white matter abnormalities, or specific patterns of signal changes that are suggestive of specific metabolic disorders. Advanced MRI techniques such as magnetic resonance spectroscopy (MRS) can provide information about the metabolic composition of tissues, further aiding in diagnosis. MRI helps visualize brain structure to assess the extent of damage and monitor disease progression. It’s crucial to remember that MRI is just one piece of the diagnostic puzzle and needs to be considered alongside clinical findings and laboratory results.
Q 13. How do you interpret laboratory findings suggestive of a specific metabolic disorder?
Interpreting laboratory findings suggestive of a specific metabolic disorder requires a systematic approach and expertise in biochemical pathways. The results need to be interpreted within the clinical context of the patient’s presentation. A single abnormal value rarely confirms a diagnosis; rather, a pattern of abnormal findings often points toward a particular disorder.
For example, elevated levels of lactate and pyruvate in blood may suggest a mitochondrial disorder or a defect in pyruvate metabolism. Similarly, elevated levels of certain amino acids or organic acids in urine (detected through urine organic acid analysis) can be highly indicative of specific organic acidemias or aminoacidopathies. Genetic testing complements laboratory findings and is often needed for definitive diagnosis. The interpretation of these results requires close collaboration between the clinician, laboratory personnel, and often genetic counselors to provide the most accurate and informative results for families.
Q 14. What are the ethical considerations surrounding genetic testing for metabolic disorders?
Genetic testing for metabolic disorders presents several ethical considerations. The potential benefits of early diagnosis and intervention need to be carefully weighed against the potential risks and psychosocial implications.
- Informed consent: Obtaining fully informed consent from parents or guardians is paramount, ensuring they understand the purpose, limitations, and potential consequences of testing. This includes discussing the possibility of incidental findings and the implications for reproductive decisions.
- Incidental findings: Genetic tests may uncover unexpected genetic variations unrelated to the initial concern, raising ethical questions about whether to disclose such findings and their potential impact on individuals and families.
- Genetic discrimination: Concerns exist about potential discrimination in insurance, employment, or other areas based on the results of genetic testing. This underscores the need for appropriate legislation and protection of patient privacy.
- Psychological impact: Receiving a diagnosis of a serious genetic disorder can have profound psychological effects on patients and their families. Access to appropriate genetic counseling and support services is crucial.
- Reproductive implications: The results may influence family reproductive decisions, leading to challenging ethical considerations around prenatal diagnosis, selective termination, or preimplantation genetic diagnosis.
Careful consideration of these ethical issues and a patient-centered approach, emphasizing shared decision-making and patient autonomy, are essential in providing responsible and ethical genetic testing services.
Q 15. Describe the genetic counseling process for families affected by neurometabolic disorders.
Genetic counseling for families affected by neurometabolic disorders is a crucial process that helps families understand the inheritance patterns, risks, and options available to them. It begins with a thorough family history review, identifying affected relatives and the mode of inheritance (autosomal recessive, autosomal dominant, X-linked).
We then explain the specific genetic defect causing the disorder in a clear and empathetic manner, using analogies and visual aids if necessary. For example, if explaining a defect in an enzyme involved in a metabolic pathway, we might use the analogy of a car assembly line where a missing part (enzyme) prevents the final product (metabolite) from being assembled correctly.
We discuss recurrence risks for future pregnancies, including the probability of having another affected child. We also outline available prenatal diagnostic tests such as chorionic villus sampling (CVS) or amniocentesis, which can detect the genetic defect during pregnancy. Finally, we help families navigate their emotional responses to the diagnosis, providing support and connecting them with relevant support groups. We always leave time for questions, ensuring the family feels understood and empowered.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What are the psychosocial implications for families with children with neurometabolic disorders?
Families coping with a child with a neurometabolic disorder face significant psychosocial challenges. The diagnosis itself can be incredibly stressful, bringing feelings of guilt, anxiety, and grief. Parents often grapple with the uncertainty of the prognosis and the potential long-term effects on their child’s development and quality of life.
The demanding nature of caring for a child with complex medical needs can strain family relationships and lead to parental burnout. Financial burdens associated with medical care, specialized therapies, and adaptations to the home environment can add to the stress. Furthermore, the child may experience social isolation due to their disability, and siblings may feel neglected or experience emotional distress. Therefore, psychosocial support is essential, including access to support groups, counseling for parents and siblings, and respite care services.
Q 17. How do you communicate complex medical information to parents of affected children?
Communicating complex medical information to parents requires empathy, patience, and a tailored approach. I begin by gauging their understanding of medical terminology and adjusting my language accordingly. I use plain language, avoiding jargon whenever possible, and illustrate concepts with clear analogies. For instance, explaining mitochondrial dysfunction can be simplified by comparing the mitochondria to ‘powerhouses’ within cells that, when faulty, affect energy production across the body.
I use visual aids, such as diagrams and flowcharts, to visualize metabolic pathways or disease processes. I break down information into smaller, manageable chunks, checking for understanding after each point. I provide written summaries of key information and encourage parents to take notes or record the conversation. Finally, I create a safe space where parents can openly share their concerns and ask questions without feeling judged, ensuring they leave feeling informed and supported.
Q 18. Discuss the role of genetic testing in the diagnosis of neurometabolic disorders.
Genetic testing plays a pivotal role in diagnosing neurometabolic disorders. The process often begins with a thorough clinical evaluation, focusing on symptoms, family history, and metabolic investigations such as blood and urine analyses. Depending on the suspicion, various genetic tests may be employed.
These include:
- Next-Generation Sequencing (NGS): This allows for simultaneous analysis of numerous genes, significantly accelerating the diagnostic process.
- Targeted gene sequencing: This focuses on specific genes associated with a particular suspected disorder.
- Chromosomal microarray analysis (CMA): This detects large chromosomal deletions or duplications that may be responsible for the condition.
- Biochemical testing: Assays that directly measure levels of certain metabolites in blood, urine or cerebrospinal fluid.
Interpreting genetic test results requires expertise, considering the potential for variant of uncertain significance (VUS). This involves careful assessment of the variant’s impact on protein function and its correlation with the clinical phenotype.
Q 19. What are the limitations of current treatment options for neurometabolic disorders?
Current treatment options for neurometabolic disorders are often limited and vary greatly depending on the specific condition. Many disorders lack curative treatments, and therapies primarily aim to manage symptoms, slow disease progression, or prevent complications.
Limitations include:
- Lack of disease-specific treatments: For many disorders, there’s no specific therapy to target the underlying genetic defect.
- Limited effectiveness: Existing treatments may only offer modest improvements in symptoms and may not prevent long-term complications.
- Significant side effects: Some treatments, such as enzyme replacement therapy, can have side effects that need careful monitoring and management.
- Difficulties in drug delivery to the brain: Many neurometabolic disorders affect the central nervous system, making it challenging to deliver medication effectively to the brain.
Research into novel therapeutic strategies, including gene therapy and precision medicine approaches, holds promise for future improvements.
Q 20. Describe the potential benefits and risks of gene therapy in neurometabolic disorders.
Gene therapy offers a potential paradigm shift in treating neurometabolic disorders by addressing the root cause of the disease. It involves introducing a functional copy of a mutated gene into the patient’s cells or correcting the faulty gene.
Potential Benefits:
- Disease correction: Gene therapy could potentially cure the disorder by replacing the faulty gene or correcting the defect.
- Improved quality of life: Successful gene therapy could significantly improve the patient’s symptoms and overall quality of life.
- Long-term benefits: The therapeutic effect might be long-lasting, reducing or eliminating the need for ongoing medication.
Potential Risks:
- Off-target effects: The therapeutic gene may integrate into the wrong location in the genome, causing unexpected consequences.
- Immune responses: The body’s immune system may reject the introduced gene, limiting the effectiveness of the therapy.
- Insertional mutagenesis: The introduced gene may disrupt other genes, potentially leading to cancer or other disorders.
- Delivery challenges: Efficiently delivering the therapeutic gene to the target cells, particularly in the brain, remains a major hurdle.
Rigorous preclinical and clinical studies are crucial to ensure the safety and efficacy of gene therapy before widespread application.
Q 21. How do you monitor treatment response in patients with neurometabolic disorders?
Monitoring treatment response in neurometabolic disorders requires a multi-faceted approach. It involves regular clinical assessments, biochemical tests, and often neuroimaging studies. Clinical evaluations focus on tracking changes in symptoms, developmental milestones, and overall health.
Methods include:
- Regular clinical examinations: Assessing neurological status, motor skills, cognitive function, and growth parameters.
- Biochemical tests: Measuring levels of specific metabolites in blood, urine, or cerebrospinal fluid to monitor disease activity and treatment efficacy.
- Neuroimaging: Techniques such as MRI or MRS may be used to assess brain structure and function, aiding in tracking disease progression or treatment response.
- Cognitive assessments: Standardized tests evaluate cognitive abilities and track changes in intellectual function over time.
- Genetic testing (follow-up): Post-treatment genetic testing can assess the effectiveness of gene therapy or other interventions targeting a specific genetic defect.
The frequency of monitoring varies based on the specific disorder, treatment regimen, and the individual patient’s needs. Close collaboration between physicians, geneticists, nurses and other specialists is essential for effective management and optimal outcome.
Q 22. Describe the importance of multidisciplinary team approach in managing neurometabolic disorders.
Managing neurometabolic disorders requires a truly collaborative approach. Think of it like a complex orchestra – each musician (specialist) plays a vital role, and their combined performance (patient care) is far superior to any individual effort. A multidisciplinary team typically includes a pediatric neurologist, metabolic geneticist, biochemical geneticist, dietitian, neuropsychologist, physical therapist, occupational therapist, and social worker.
- Pediatric Neurologist: Diagnoses and manages neurological symptoms.
- Metabolic Geneticist/Biochemical Geneticist: Identifies the underlying genetic defect and guides metabolic management.
- Dietitian: Creates and monitors specialized diets to manage metabolic imbalances.
- Neuropsychologist: Assesses cognitive and behavioral effects and develops strategies for support.
- Therapists: Address physical and developmental challenges.
- Social Worker: Provides psychosocial support to the family and helps navigate resources.
This coordinated effort ensures comprehensive care, optimizing treatment, improving patient outcomes, and providing invaluable support for families facing these challenging conditions. For example, a child with phenylketonuria (PKU) needs a carefully designed diet (dietitian), regular monitoring of blood phenylalanine levels (biochemist), and management of any neurological complications (neurologist).
Q 23. How do you approach the diagnosis of a suspected new neurometabolic disorder?
Diagnosing a suspected new neurometabolic disorder is a complex process requiring a systematic approach, often involving a detective-like investigation. We start by taking a thorough history, including family history, developmental milestones, and symptom onset. This is followed by a detailed physical examination, assessing for any neurological or metabolic signs.
Next, we delve into laboratory investigations. This can include:
- Blood tests: To measure levels of various metabolites and assess liver and kidney function.
- Urine tests: To identify abnormal organic acids, amino acids, or sugars.
- Enzyme assays: To measure the activity of specific enzymes in cells or tissues.
- Genetic testing: Including whole exome sequencing (WES) or whole genome sequencing (WGS) to pinpoint genetic mutations.
- Brain imaging (MRI, CT): To detect structural abnormalities.
The process involves meticulous interpretation of results, often requiring collaboration with other specialists. Sometimes, the journey to a definitive diagnosis can be long and challenging, and it may involve consultations with experts in other centers, as the prevalence of many neurometabolic disorders are rare, necessitating collaboration within and beyond one’s own practice.
Consider the example of a child presenting with hypotonia, developmental delay, and unusual urine odor. This might prompt investigations for organic acidemias, leading to metabolic testing and subsequent genetic analysis to pinpoint the specific genetic mutation causing the disorder.
Q 24. Explain the concept of metabolic crisis and the appropriate management strategies.
A metabolic crisis is a life-threatening exacerbation of a neurometabolic disorder. Imagine a delicate balance disrupted, leading to a cascade of harmful effects. It’s often triggered by infection, illness, or dietary changes, leading to an accumulation of toxic metabolites or a deficiency of essential substances.
Symptoms can include:
- Lethargy or coma
- Seizures
- Respiratory distress
- Hypoglycemia or hyperglycemia
- Acidosis or alkalosis
Management strategies are crucial and require immediate intervention. These include:
- Supportive care: Managing symptoms such as seizures, respiratory issues, and electrolyte imbalances.
- Dietary modifications: Restriction of specific substances or supplementation with essential nutrients.
- Medication: To control seizures, correct acidosis, or manage other complications.
- Dialysis: To remove toxic substances from the blood.
- Liver or kidney transplantation: In specific situations.
Rapid identification and prompt, aggressive intervention are critical for survival and minimizing long-term complications. The urgency is similar to managing a severe septic shock in a critical care setting. Every moment counts.
Q 25. What are the common neuroimaging findings in various neurometabolic conditions?
Neuroimaging findings vary widely depending on the specific neurometabolic condition. These findings often reflect the underlying metabolic disturbances and their effects on the brain. MRI is the preferred modality.
- Leukodystrophies: Often show diffuse white matter abnormalities, sometimes with specific patterns depending on the disorder (e.g., hypomyelination, demyelination).
- Mitochondrial disorders: Can present with nonspecific findings, including atrophy, white matter changes, and basal ganglia abnormalities.
- Lysosomal storage disorders: May demonstrate various findings depending on the specific disorder, but often involve cerebral and cerebellar atrophy, white matter changes, or specific patterns of involvement (e.g., delayed myelination).
- Peroxisomal disorders: Often exhibit abnormalities in white matter, but patterns can vary significantly.
It’s crucial to remember that neuroimaging findings alone are rarely diagnostic. They are best used in conjunction with clinical presentation, biochemical findings, and genetic testing to arrive at a definitive diagnosis. For example, a child with suspected Krabbe disease might show a characteristic pattern of white matter involvement on MRI, but confirmation requires biochemical and genetic testing.
Q 26. Discuss the prognosis for children with various common neurometabolic disorders.
Prognosis varies significantly depending on the specific neurometabolic disorder, the severity of the condition at presentation, and the effectiveness of treatment. Some disorders may be relatively benign, while others can lead to severe disability or even death.
For instance, some individuals with milder forms of phenylketonuria can live relatively normal lives with dietary management. However, untreated classic PKU can lead to profound intellectual disability and other severe neurological problems. Similarly, prognosis in some lysosomal storage disorders can vary depending on the type and severity of the condition and response to therapies, ranging from relatively mild to severely debilitating.
It’s essential to provide realistic and individualized prognostic information to families. This requires considering the specific disorder, the child’s response to treatment, and the availability of supportive services. It’s not merely about survival but about maximizing quality of life for the child.
Q 27. Describe the role of supportive care in managing neurometabolic disorders.
Supportive care is a cornerstone of managing neurometabolic disorders. It’s not just about treating the underlying metabolic defect but also about addressing the wide range of symptoms and challenges faced by children with these conditions. This may include:
- Nutritional support: Specialized diets, vitamin supplements, or feeding tubes to ensure adequate nutrition.
- Neurological management: Treatment of seizures, spasticity, and other neurological problems.
- Respiratory support: Management of respiratory problems, possibly requiring ventilation.
- Physical, occupational, and speech therapy: To address developmental delays and improve motor skills and communication.
- Educational support: Specialized education tailored to the child’s needs.
- Psychosocial support: Counseling for the child and family to cope with the emotional and psychological challenges.
Supportive care is crucial for optimizing quality of life and helping children reach their full potential, despite the challenges posed by their condition. For example, a child with a severe form of a lysosomal storage disorder might benefit from regular physical therapy to improve mobility and speech therapy to enhance communication skills, even while receiving enzyme replacement therapy.
Q 28. How do you engage in continuing medical education (CME) to stay current in this field?
Staying current in this rapidly evolving field demands ongoing commitment to continuing medical education (CME). My approach is multi-faceted:
- Professional Societies: Active participation in professional organizations such as the American Academy of Neurology, the Society for Inherited Metabolic Disorders, and relevant international societies. Attending conferences and engaging with colleagues is invaluable for learning about latest research and best practices.
- Peer-Reviewed Journals: Regularly reviewing high-impact journals focusing on neurology, genetics, and metabolic disorders. This keeps me abreast of groundbreaking research and clinical trials.
- Online Courses and Webinars: Utilizing online resources to update my knowledge on specific topics or new therapeutic approaches. These platforms often offer CME credits.
- Collaboration: Active engagement with colleagues, especially through participation in case conferences and multidisciplinary team meetings. Sharing knowledge and experiences is highly effective for continuous learning.
- Mentorship: Both mentoring junior colleagues and seeking guidance from experienced clinicians contributes significantly to personal and professional growth.
This holistic approach ensures that I am well-informed about the latest advancements and best practices, ultimately benefiting the children under my care.
Key Topics to Learn for Pediatric Neurometabolic Disorders Interview
- Inborn Errors of Metabolism (IEM): Understanding the diverse range of IEMs, their classification (e.g., carbohydrate, amino acid, fatty acid oxidation disorders), and common diagnostic approaches.
- Clinical Presentation and Diagnosis: Learning to recognize the varied clinical presentations of neurometabolic disorders in children, from subtle developmental delays to acute metabolic crises. This includes mastering diagnostic tools such as newborn screening, metabolic profiling, and genetic testing.
- Specific Disorder Knowledge: Gaining in-depth knowledge of several common neurometabolic disorders such as Phenylketonuria (PKU), Maple Syrup Urine Disease (MSUD), and mitochondrial disorders. Focus on their pathophysiology, clinical manifestations, and management strategies.
- Treatment and Management: Familiarize yourself with the principles of managing neurometabolic disorders, including dietary therapies (e.g., restricting certain amino acids or carbohydrates), enzyme replacement therapy, and supportive care.
- Genetic Counseling and Family Planning: Understanding the genetic basis of these disorders and the implications for genetic counseling and family planning is crucial.
- Ethical Considerations: Explore the ethical dilemmas related to diagnosis, treatment, and prognosis of neurometabolic disorders in children and their families.
- Long-term Outcomes and Prognosis: Develop an understanding of the long-term consequences and potential outcomes for children with neurometabolic disorders, considering the impact on development, cognitive function, and quality of life.
- Case Study Analysis: Practice analyzing clinical cases to hone your diagnostic reasoning and problem-solving skills. Consider different scenarios and differential diagnoses.
Next Steps
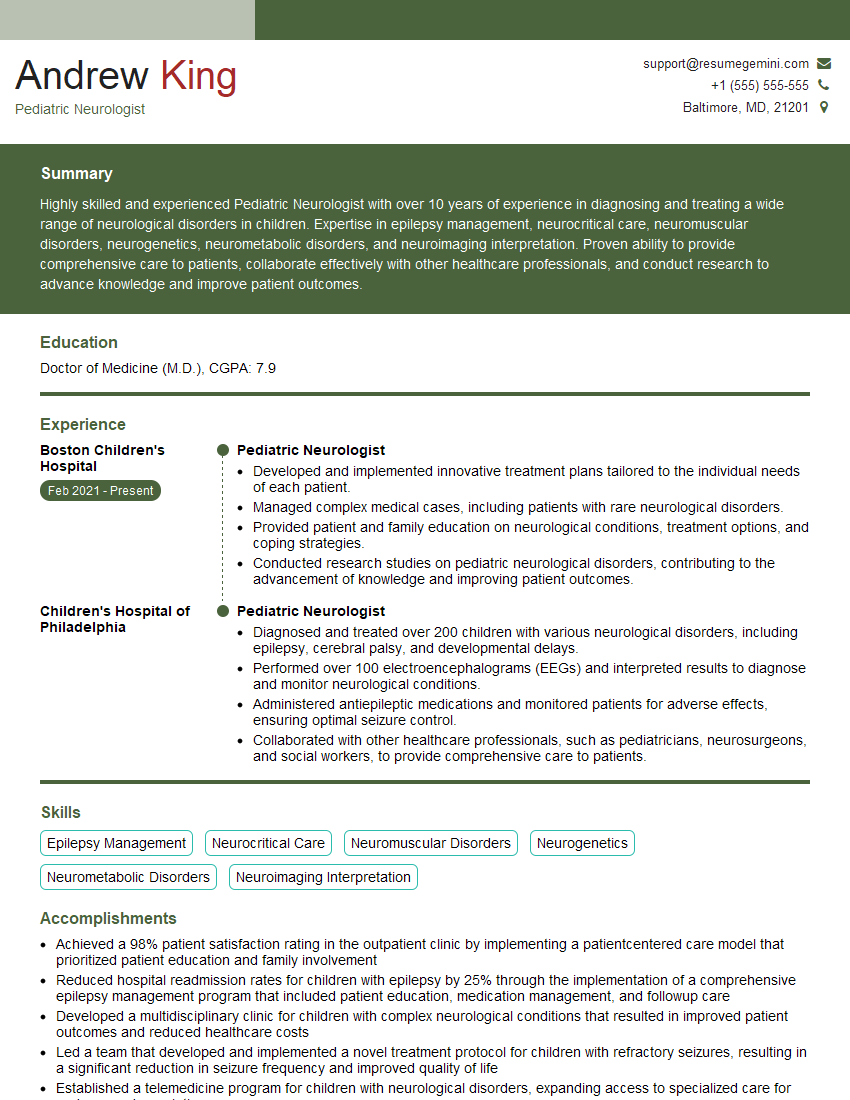
Mastering Pediatric Neurometabolic Disorders significantly enhances your expertise and opens doors to rewarding career opportunities in research, clinical practice, or genetic counseling. A strong resume is vital for showcasing your skills and experience to potential employers. Creating an ATS-friendly resume is crucial for maximizing your job prospects. ResumeGemini is a trusted resource for building a professional and impactful resume that will catch the eye of recruiters. Examples of resumes tailored specifically to Pediatric Neurometabolic Disorders are available to help you create a compelling application.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
To the interviewgemini.com Webmaster.
Very helpful and content specific questions to help prepare me for my interview!
Thank you
To the interviewgemini.com Webmaster.
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.