Unlock your full potential by mastering the most common Stress and Anxiety Management interview questions. This blog offers a deep dive into the critical topics, ensuring you’re not only prepared to answer but to excel. With these insights, you’ll approach your interview with clarity and confidence.
Questions Asked in Stress and Anxiety Management Interview
Q 1. Explain the difference between acute stress and chronic stress.
Acute stress is a short-term response to a specific stressor, like a deadline at work or a public speaking engagement. It’s like a surge of energy – your body kicks into gear to handle the immediate challenge. Once the stressor is gone, your body usually returns to its normal state. Chronic stress, on the other hand, is prolonged exposure to stressors that your body doesn’t have time to recover from. This could be due to ongoing work pressure, relationship difficulties, or financial worries. Imagine it like a constantly running faucet – the drip, drip, drip of stress never stops, leading to exhaustion and potential health problems. The key difference lies in the duration and the body’s ability to recover.
Q 2. Describe the physiological responses to stress.
The physiological response to stress is a complex interplay of systems orchestrated by the hypothalamic-pituitary-adrenal (HPA) axis. When faced with a perceived threat, the brain triggers the release of hormones like cortisol and adrenaline. This leads to a cascade of effects: increased heart rate and blood pressure, faster breathing, heightened senses, and mobilization of energy stores (fight-or-flight response). These responses are beneficial in short-term, acute stress situations. However, chronic stress leads to sustained activation of these systems, which can negatively impact cardiovascular health, immune function, digestion, and sleep. For example, consistently high cortisol levels can weaken the immune system, making you more susceptible to illness. Similarly, chronic activation of the sympathetic nervous system can contribute to hypertension and heart disease.
Q 3. What are the key symptoms of generalized anxiety disorder (GAD)?
Generalized Anxiety Disorder (GAD) is characterized by persistent and excessive worry about various aspects of life, lasting at least six months. Key symptoms include:
- Excessive worry and anxiety about numerous events and activities.
- Difficulty controlling worry.
- At least three of the following physical symptoms: restlessness, fatigue, difficulty concentrating, irritability, muscle tension, sleep disturbance.
- Significant impairment in social, occupational, or other important areas of functioning.
It’s important to note that everyone experiences worry from time to time. GAD is distinguished by the intensity, duration, and pervasiveness of the worry, as well as the impact it has on daily life. For example, someone with GAD might worry excessively about their job security, their children’s health, and their finances, all at the same time, leading to significant distress and impacting their ability to function effectively.
Q 4. Explain the cognitive behavioral therapy (CBT) model for treating anxiety.
Cognitive Behavioral Therapy (CBT) for anxiety focuses on identifying and changing negative thought patterns and maladaptive behaviors that contribute to anxiety. It works on the principle that our thoughts, feelings, and behaviors are interconnected. The therapist helps the individual identify their anxious thoughts (e.g., “I’m going to fail this presentation”), the resulting feelings (e.g., fear, panic), and the behaviors they engage in to cope (e.g., avoidance, procrastination).
CBT employs several techniques including:
- Cognitive restructuring: Challenging and modifying unhelpful thoughts.
- Exposure therapy: Gradually facing feared situations to reduce avoidance.
- Behavioral experiments: Testing out negative beliefs in real-life situations.
- Relaxation techniques: Learning to manage physical symptoms of anxiety.
For example, a person with social anxiety might use CBT to challenge their thought that everyone will judge them negatively, practice social interactions in a safe and controlled environment, and learn relaxation techniques to manage physical symptoms like rapid heartbeat before social events.
Q 5. How does mindfulness meditation help manage stress and anxiety?
Mindfulness meditation helps manage stress and anxiety by shifting focus from ruminative thoughts and future anxieties to the present moment. It cultivates awareness of thoughts, feelings, and sensations without judgment. This non-judgmental awareness helps break the cycle of negative thought patterns that fuel anxiety. By anchoring oneself in the present, the mind is less likely to wander into worry about the past or future.
Techniques like focusing on the breath, body scan meditation, and mindful movement help ground the individual and reduce the intensity of anxious feelings. Regular practice can strengthen the prefrontal cortex, the brain region involved in emotional regulation, leading to improved self-awareness and emotional control. Think of it like training a muscle – the more you practice mindfulness, the stronger your ability to manage stress and anxiety becomes.
Q 6. Describe the techniques used in Dialectical Behavior Therapy (DBT).
Dialectical Behavior Therapy (DBT) is a type of cognitive-behavioral therapy specifically designed for individuals struggling with intense emotions and self-destructive behaviors. It emphasizes the importance of both acceptance and change. DBT uses a range of techniques including:
- Mindfulness skills: Similar to mindfulness meditation, but with a focus on observing emotions without judgment and responding skillfully.
- Distress tolerance skills: Techniques to cope with overwhelming emotions in the moment, such as radical acceptance, self-soothing, and distraction.
- Emotion regulation skills: Identifying, understanding, and managing emotions effectively.
- Interpersonal effectiveness skills: Improving communication and assertiveness skills to build healthy relationships.
For instance, DBT might help someone with borderline personality disorder learn to tolerate intense emotional distress without resorting to self-harm, identify triggers for emotional outbursts, and develop strategies for communicating their needs more effectively in relationships. It’s a holistic approach focusing on both emotional regulation and behavioral change.
Q 7. What is Acceptance and Commitment Therapy (ACT), and how is it applied?
Acceptance and Commitment Therapy (ACT) is a mindfulness-based therapy that focuses on accepting difficult thoughts and feelings without judgment, while committing to valued actions. Instead of trying to control or eliminate unwanted thoughts and emotions, ACT helps individuals learn to observe them as mental events, without getting caught up in their content. This creates psychological flexibility – the ability to adapt and respond effectively to life’s challenges.
ACT utilizes various techniques including:
- Acceptance: Learning to acknowledge and accept difficult emotions and thoughts without trying to suppress them.
- Cognitive defusion: Creating distance from thoughts by noticing them as mental events rather than absolute truths.
- Self-as-context: Recognizing oneself as the observer of thoughts and feelings, rather than being defined by them.
- Values clarification: Identifying personal values and setting goals aligned with these values.
- Committed action: Taking action towards valued goals, even when facing difficult emotions.
For example, someone struggling with fear of public speaking might use ACT to accept their anxiety, practice cognitive defusion to reduce the power of anxious thoughts, and commit to giving presentations despite their fear, because speaking publicly aligns with their career goals. ACT helps individuals live a more meaningful and fulfilling life, even in the face of difficult experiences.
Q 8. How would you assess a client’s level of stress and anxiety?
Assessing a client’s stress and anxiety involves a multi-faceted approach, combining subjective and objective measures. It’s crucial to understand that everyone experiences stress and anxiety differently, so a personalized assessment is key.
- Clinical Interviews: A thorough interview allows me to understand the client’s history, current stressors, symptoms (both physical and emotional), and their perception of their own stress levels. I’ll use open-ended questions to encourage them to express their experiences freely. For example, I might ask, “Tell me about a typical day for you and how you feel throughout it.” or “Can you describe a recent situation that caused you significant stress?”
- Standardized Questionnaires: Validated tools like the Generalized Anxiety Disorder 7-item (GAD-7) scale or the Patient Health Questionnaire-9 (PHQ-9) for depression (as anxiety and depression often co-occur) provide objective data about the severity and frequency of symptoms. These scores offer a baseline and track progress over time.
- Observation: Nonverbal cues like body language, restlessness, and vocal tone can provide valuable insights during the session. For instance, rapid speech, fidgeting, or difficulty maintaining eye contact might indicate elevated anxiety.
- Physiological Measures: In some cases, physiological measures like heart rate variability or blood pressure may be helpful, particularly when assessing the physical manifestations of stress and anxiety. However, these are often used in conjunction with other assessment methods.
By integrating information from these various sources, I can build a comprehensive picture of the client’s stress and anxiety levels, paving the way for a tailored treatment plan.
Q 9. What are some common coping mechanisms people use to deal with stress, and which are healthy/unhealthy?
People employ various coping mechanisms to manage stress, some healthy and others detrimental to their well-being in the long run.
- Healthy Coping Mechanisms: These strategies help individuals manage stress constructively and promote emotional regulation. Examples include:
- Exercise: Physical activity releases endorphins, reducing stress hormones.
- Mindfulness and Meditation: These practices cultivate present moment awareness and reduce overthinking.
- Social Support: Connecting with supportive friends and family provides emotional resilience.
- Healthy Diet and Sleep Hygiene: Nourishing the body and ensuring adequate rest are fundamental to stress management.
- Time Management Techniques: Prioritization and planning can reduce feelings of overwhelm.
- Unhealthy Coping Mechanisms: These strategies offer temporary relief but can exacerbate stress and lead to further problems. Examples include:
- Substance Abuse: Using drugs or alcohol to numb emotions is a dangerous coping mechanism.
- Avoidance: Consistently avoiding stressors prevents facing and resolving underlying issues.
- Emotional Eating: Using food to soothe negative emotions can lead to weight gain and other health issues.
- Excessive Social Media Use: Can lead to social comparison, anxiety, and decreased real-life interaction.
- Isolation: Withdrawing from social support diminishes emotional resilience.
It’s important to help clients identify their coping mechanisms and learn healthier alternatives to manage stress more effectively.
Q 10. Describe a situation where you helped a client overcome a significant stressor.
I once worked with a client, Sarah, who was experiencing significant stress related to her demanding job and impending wedding. She was struggling with insomnia, irritability, and difficulty concentrating. She felt overwhelmed and constantly on edge.
We started by exploring her stressors using a combination of interviews and questionnaires. Through these sessions, we identified several key issues contributing to her distress, including unrealistic expectations at work, a lack of boundary setting, and perfectionistic tendencies.
We implemented a multi-pronged approach: We practiced mindfulness techniques to help her manage her racing thoughts and anxiety, we developed time management strategies to prioritize tasks and improve work-life balance, and we worked on assertiveness skills to help her communicate her needs more effectively at work and with her fiancé. We also incorporated regular physical activity into her routine.
Over several sessions, Sarah showed significant improvement in her sleep, mood, and overall well-being. She felt more in control of her life and learned effective strategies to manage stress going forward. This case highlighted the importance of a holistic approach that addresses both the psychological and behavioral aspects of stress management.
Q 11. How would you develop a personalized stress management plan for a client?
Developing a personalized stress management plan is a collaborative process that involves careful consideration of the client’s unique needs and preferences. It’s not a one-size-fits-all approach.
- Assessment: Thoroughly assess the client’s stress levels, identifying triggers, symptoms, and current coping mechanisms (as discussed in question 1).
- Goal Setting: Collaboratively establish realistic and measurable goals. These could focus on reducing specific symptoms, improving coping skills, or enhancing overall well-being.
- Strategy Selection: Choose evidence-based strategies tailored to the client’s individual needs and preferences. Options might include:
- Relaxation techniques: Progressive muscle relaxation, deep breathing exercises, guided imagery, meditation.
- Cognitive behavioral techniques (CBT): Identifying and challenging negative thoughts and beliefs.
- Lifestyle changes: Improving diet, sleep, exercise, and social support.
- Time management skills: Prioritizing tasks, setting boundaries, and delegating responsibilities.
- Problem-solving skills: Developing strategies to address specific stressors.
- Implementation and Monitoring: Guide the client in implementing chosen strategies. Regular check-ins allow for progress monitoring, adjustment of strategies, and addressing any challenges encountered.
- Relapse Prevention: Develop a plan to address potential setbacks and maintain long-term stress management skills. This involves equipping the client with tools to handle future stressors.
Regular feedback and open communication are essential for a successful stress management plan. The plan should be flexible and adapted as needed throughout the process.
Q 12. What are the ethical considerations in treating clients with stress and anxiety?
Ethical considerations in treating clients with stress and anxiety are paramount. Maintaining professional boundaries, ensuring client autonomy, and safeguarding confidentiality are key.
- Confidentiality: Protecting client information is crucial. This includes adhering to relevant privacy regulations and ensuring informed consent before disclosing any information.
- Informed Consent: Clients must fully understand the treatment process, potential risks and benefits, and their right to withdraw at any time.
- Competence: Practitioners should only undertake treatments within their scope of expertise. Referrals to specialists are necessary when dealing with complex cases beyond one’s skillset.
- Boundaries: Maintaining clear professional boundaries is vital to prevent dual relationships or conflicts of interest that could compromise the therapeutic relationship.
- Cultural Sensitivity: Respecting cultural diversity and adapting treatment approaches to meet the unique needs of clients from diverse backgrounds is essential.
- Self-Care: Practitioners must prioritize their own well-being to avoid burnout and maintain the capacity to provide effective care. This is crucial, especially when dealing with clients experiencing intense emotional distress.
Ethical practice ensures the client’s safety, promotes trust, and maximizes the effectiveness of therapy.
Q 13. How would you handle a client experiencing a panic attack during a session?
If a client experiences a panic attack during a session, my immediate priority is to ensure their safety and comfort.
- Stay Calm and Reassure: My calm demeanor helps to de-escalate the situation. I would let the client know that I’m there to support them and that panic attacks are manageable.
- Create a Safe Space: I would help them find a comfortable position, perhaps encouraging them to sit down and lean back. We would move to a quieter area if possible.
- Breathing Exercises: I would guide them through slow, deep breathing exercises to regulate their breathing and reduce the intensity of physical symptoms.
- Grounding Techniques: To help the client connect to the present moment, I might use grounding techniques. This could involve focusing on their senses: What do they see, hear, feel, smell, and taste?
- Monitor Symptoms: I would monitor their physiological response (heart rate, breathing) and offer reassurance as needed.
- Post-Attack Discussion: Once the panic attack subsides, we would discuss the experience, exploring potential triggers and developing coping strategies to prevent future occurrences. This often involves developing a personalized safety plan.
In severe cases or if the attack is prolonged or concerning, I would not hesitate to seek emergency medical assistance.
Q 14. Explain the role of relaxation techniques in stress reduction.
Relaxation techniques play a vital role in stress reduction by activating the parasympathetic nervous system, counteracting the effects of the stress response (which activates the sympathetic nervous system).
When we experience stress, our bodies release stress hormones like cortisol and adrenaline, leading to increased heart rate, muscle tension, and heightened alertness. Relaxation techniques help to reverse these physiological effects.
- Progressive Muscle Relaxation: This technique involves systematically tensing and releasing different muscle groups, promoting physical relaxation and reducing muscle tension.
- Deep Breathing Exercises: Slow, deep breaths activate the vagus nerve, which helps slow the heart rate and promote a sense of calm. Diaphragmatic breathing is particularly effective.
- Guided Imagery: Visualizing peaceful and calming scenes can reduce anxiety and promote relaxation. This can be self-guided or done with a therapist’s assistance.
- Mindfulness Meditation: Focusing on the present moment without judgment helps to quiet the mind and reduce stress. It involves paying attention to the breath, body sensations, and thoughts without getting carried away by them.
Regular practice of relaxation techniques builds resilience to stress and improves overall well-being. They are not a quick fix but rather tools to be integrated into daily life for ongoing benefit. They can significantly reduce the physiological and psychological impact of stress over time.
Q 15. What are the limitations of Cognitive Behavioral Therapy (CBT)?
Cognitive Behavioral Therapy (CBT) is a highly effective treatment for many mental health conditions, but it’s not a magic bullet. Its limitations stem from several factors.
- Client Factors: CBT requires active participation and commitment from the client. Individuals with severe cognitive impairments, low motivation, or significant resistance to change may find it challenging to engage fully. For example, someone experiencing severe psychosis might struggle to participate in the self-monitoring and cognitive restructuring exercises central to CBT.
- Therapist Factors: The effectiveness of CBT hinges heavily on the therapist’s skill and experience. A poorly trained or inexperienced therapist might not accurately identify maladaptive thought patterns or implement techniques effectively. The therapeutic relationship is also crucial; a poor rapport can significantly hinder progress.
- Complexity of Issues: While CBT excels in treating specific anxiety disorders and depression, it might be less effective for complex or deeply ingrained issues like personality disorders or severe trauma. It may need to be combined with other therapies for best results.
- Time Commitment: CBT typically requires consistent effort over several weeks or months. This can be a barrier for individuals with busy schedules or limited resources.
- Relapse Prevention: While CBT equips individuals with coping mechanisms, relapse is always a possibility, particularly without ongoing support or maintenance sessions.
In summary, CBT’s effectiveness depends on various factors, highlighting the need for careful assessment and potentially integrating it with other therapeutic approaches for optimal outcomes.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you differentiate between anxiety and depression?
Anxiety and depression, while often co-occurring, are distinct conditions with different core features. Anxiety is characterized by excessive worry, fear, and nervousness, often manifesting physically as rapid heartbeat, sweating, and trembling. It’s future-oriented, with a focus on potential threats. Imagine constantly anticipating a job interview or fearing a potential health problem—that’s anxiety.
Depression, on the other hand, is marked by persistent sadness, loss of interest in activities, feelings of hopelessness and worthlessness, and changes in sleep and appetite. It’s typically present-oriented and focused on negative self-perception and the past. Think of someone constantly ruminating on past mistakes or feeling overwhelmed by a sense of failure – that’s a hallmark of depression.
However, the line can blur, as someone with depression might experience anxiety symptoms, and vice-versa. A proper diagnosis requires a comprehensive assessment by a mental health professional.
Q 17. What are the warning signs of burnout, and how can it be prevented?
Burnout is a state of emotional, physical, and mental exhaustion caused by prolonged or excessive stress. Warning signs can be subtle at first, but progressively worsen. They include:
- Emotional Exhaustion: Feeling emotionally drained, cynical, or detached from work.
- Depersonalization: Treating others impersonally or developing a negative attitude toward clients or colleagues.
- Reduced Personal Accomplishment: Feeling a sense of incompetence, low self-efficacy, and lack of accomplishment at work.
- Physical Symptoms: Headaches, fatigue, sleep disturbances, gastrointestinal problems.
- Behavioral Changes: Increased irritability, procrastination, difficulty concentrating, increased alcohol or substance use.
Preventing burnout requires a proactive approach:
- Set Boundaries: Learn to say no to additional tasks when feeling overwhelmed. Protect your personal time and prioritize self-care.
- Practice Stress Management Techniques: Incorporate regular exercise, mindfulness meditation, deep breathing exercises, and other relaxation techniques into your daily routine.
- Seek Social Support: Connect with friends, family, or colleagues for emotional support and understanding.
- Take Breaks: Schedule regular breaks throughout the workday to rest and recharge.
- Seek Professional Help: Don’t hesitate to seek help from a therapist or counselor if you’re struggling to manage stress or are experiencing symptoms of burnout.
Regular self-reflection and identifying early warning signs are crucial for preventing burnout. It’s vital to prioritize your well-being to avoid the serious consequences of prolonged stress.
Q 18. Describe your experience working with different types of anxiety disorders.
My experience spans various anxiety disorders, including Generalized Anxiety Disorder (GAD), Panic Disorder, Social Anxiety Disorder (SAD), Specific Phobias, and Obsessive-Compulsive Disorder (OCD). Each presents unique challenges and requires a tailored approach.
For instance, with GAD, the focus is on managing chronic worry and developing coping mechanisms for everyday stressors. This might involve cognitive restructuring, relaxation techniques, and behavioral experiments to challenge avoidance behaviors. In contrast, Panic Disorder requires addressing the physical symptoms of panic attacks and developing strategies to manage them, like breathing retraining and exposure therapy.
With SAD, the emphasis is on gradually exposing the individual to social situations they fear, building self-esteem, and challenging negative self-beliefs. Specific phobias often benefit from systematic desensitization, a gradual exposure therapy. OCD treatment usually combines exposure and response prevention (ERP) to break the cycle of obsessions and compulsions.
In all cases, building a strong therapeutic alliance, fostering self-compassion, and tailoring treatments to the individual’s unique needs and preferences are essential for positive outcomes.
Q 19. How do you assess a client’s readiness for change in therapy?
Assessing a client’s readiness for change is crucial for successful therapy. I employ a multi-faceted approach, integrating several key elements.
- Motivation: I explore the client’s reasons for seeking therapy and their level of commitment to change. Ambivalence is common, and addressing it openly is essential. I might use motivational interviewing techniques to explore their concerns and strengths.
- Self-Efficacy: I assess the client’s belief in their ability to make changes and overcome challenges. A strong sense of self-efficacy is a significant predictor of success.
- Support System: Understanding the client’s support network (family, friends, etc.) is important. A strong support system can provide crucial encouragement and accountability.
- Problem Identification: Clearly identifying the problem(s) and their impact on the client’s life is essential. This process fosters a shared understanding and sets a direction for treatment.
- Goal Setting: Collaboration in setting realistic, achievable goals helps track progress and reinforce motivation. These goals should align with the client’s values and aspirations.
Using these measures, I can tailor treatment to the client’s unique stage of readiness, building a strong foundation for positive change. For example, if a client demonstrates low motivation and lacks self-efficacy, I might initially focus on building hope and self-esteem before delving into more intensive change-oriented techniques.
Q 20. How do you maintain your own well-being while working with clients experiencing stress and anxiety?
Maintaining my own well-being is paramount in this profession. Working with clients experiencing significant stress and anxiety can be emotionally demanding. I prioritize self-care through several strategies.
- Regular Self-Reflection: I regularly reflect on my experiences with clients, identifying potential sources of stress or emotional fatigue. This helps me process emotions and avoid burnout.
- Supervision: I meet regularly with a supervisor to discuss challenging cases and receive guidance. This provides a safe space to process complex emotions and refine my therapeutic approach.
- Stress Management Techniques: I practice the same stress-management techniques I recommend to my clients, including mindfulness, exercise, and spending time in nature.
- Boundaries: I maintain clear professional boundaries, ensuring that my work doesn’t bleed into my personal life. This prevents emotional exhaustion and ensures a healthy work-life balance.
- Continued Professional Development: Staying updated on the latest research and best practices helps me remain engaged and confident in my work.
- Seeking Support: I have a strong support network of friends, family, and colleagues who understand the demands of this profession. This provides a valuable outlet for sharing experiences and receiving emotional support.
Prioritizing self-care is not just a personal choice, it’s a professional responsibility. It allows me to show up fully and effectively for my clients.
Q 21. What are some evidence-based interventions for PTSD related to stress?
Post-Traumatic Stress Disorder (PTSD) significantly impacts stress response and regulation. Evidence-based interventions often involve a combination of approaches.
- Trauma-Focused Cognitive Behavioral Therapy (TF-CBT): This integrates CBT techniques with trauma-specific interventions, helping individuals process traumatic memories, challenge maladaptive thoughts, and develop coping skills. Techniques include psychoeducation about PTSD, trauma narrative, cognitive processing, and relaxation skills training.
- Prolonged Exposure (PE): This therapy involves repeated exposure to trauma-related memories, feelings, and situations in a safe and controlled environment. This helps to reduce avoidance behaviors and decrease the emotional intensity associated with the trauma.
- Eye Movement Desensitization and Reprocessing (EMDR): EMDR is a specific type of exposure therapy that uses bilateral stimulation (eye movements, taps, or sounds) while processing traumatic memories. It’s thought to help the brain process and integrate traumatic experiences more effectively.
- Stress Inoculation Training (SIT): This teaches individuals coping skills to manage stress and anxiety in the face of trauma-related triggers. It involves education, rehearsal, and application of coping strategies in increasingly challenging situations.
The choice of intervention depends on individual needs and preferences. Often, a combination of therapies yields the best results. It’s crucial to work with a qualified therapist experienced in treating PTSD.
Q 22. How would you explain the concept of resilience to a client?
Resilience is the ability to bounce back from adversity, trauma, tragedy, threats, or significant sources of stress — such as family and relationship problems, serious health problems, or workplace and financial stressors. It’s not about avoiding hardship, but about adapting and recovering well in the face of challenges.
Think of it like a willow tree bending in the wind. A rigid oak might snap, but the willow, flexible and adaptable, withstands the storm and returns to its upright position. Resilient individuals possess qualities that help them navigate difficulties: They have a strong sense of self-efficacy (belief in their ability to cope), a positive outlook, strong social support networks, and effective coping mechanisms.
For example, a client facing job loss might demonstrate resilience by actively seeking new opportunities, leveraging their network for support, and using positive self-talk to maintain hope. We work together to identify their strengths, build coping skills, and foster a sense of agency in their recovery.
Q 23. What are the potential side effects of common anxiety medications?
Common anxiety medications, such as benzodiazepines (e.g., Xanax, Ativan) and selective serotonin reuptake inhibitors (SSRIs) (e.g., Prozac, Zoloft), can have various side effects. These vary from person to person and depend on the medication and dosage.
- Benzodiazepines: These offer fast relief but can be habit-forming and cause drowsiness, dizziness, impaired coordination, and cognitive impairment. Withdrawal symptoms can be significant if stopped abruptly.
- SSRIs: These take longer to become effective but generally have fewer withdrawal symptoms. Common side effects include nausea, headache, insomnia, sexual dysfunction, and weight changes. Some individuals may experience increased anxiety initially.
It’s crucial that clients understand potential side effects before starting medication and report any concerning symptoms to their prescribing physician. Medication is often used in conjunction with therapy, not as a standalone solution.
Q 24. How do you work with clients who have difficulty expressing their emotions?
Working with clients who struggle to express emotions requires patience, empathy, and a tailored approach. I use various techniques to create a safe and supportive environment where they feel comfortable opening up.
- Creating a safe space: Establishing trust is paramount. This involves active listening, validating their feelings, and ensuring confidentiality.
- Non-verbal cues: I pay attention to body language, facial expressions, and tone of voice, which can offer valuable insights into their emotional state even if they can’t articulate it verbally.
- Creative expression: Art therapy, journaling prompts, or guided imagery can help bypass verbal barriers and access emotions indirectly.
- Mindfulness and somatic exercises: Focusing on bodily sensations can help clients connect with their feelings physically before verbalizing them.
- Gradual disclosure: I don’t push clients to share more than they’re ready for. Progress is made at their pace.
For example, I might start by asking open-ended questions about their experiences, focusing on specific situations rather than abstract feelings. Over time, as trust grows, deeper emotional exploration becomes possible.
Q 25. How would you adapt your therapeutic approach for clients from diverse cultural backgrounds?
Cultural sensitivity is crucial in stress and anxiety management. My approach is to adapt my therapeutic style to respect and honor the client’s cultural background and values.
- Cultural competence training: Ongoing education is vital to understanding diverse cultural perspectives on mental health and illness.
- Exploring cultural beliefs: I actively inquire about the client’s cultural beliefs surrounding mental health, stress, and emotional expression. This helps tailor interventions to be culturally appropriate and effective.
- Family involvement: In some cultures, family plays a significant role in decision-making and support. I would involve family members with the client’s consent.
- Language accessibility: Ensuring access to interpreters or resources in their native language is essential.
- Awareness of cultural biases: I am constantly mindful of my own potential biases and actively work to avoid imposing my worldview on the client.
For instance, understanding the importance of family dynamics in some cultures allows for a more effective therapeutic process. Similarly, awareness of stigma surrounding mental health in certain communities can inform strategies for engagement.
Q 26. What are some strategies for managing stress in the workplace?
Managing workplace stress is essential for both individual well-being and productivity. Strategies include:
- Time management techniques: Prioritizing tasks, setting realistic deadlines, and breaking down large projects into smaller, manageable steps can reduce feeling overwhelmed.
- Mindfulness and relaxation exercises: Practicing mindfulness meditation, deep breathing, or progressive muscle relaxation can help reduce stress in the moment.
- Healthy lifestyle choices: Regular exercise, a balanced diet, and sufficient sleep are fundamental to stress resilience.
- Setting boundaries: Learning to say no to extra work or commitments and protecting personal time is crucial.
- Social support network: Connecting with colleagues or friends for support and camaraderie can buffer against stress.
- Seeking professional help: If stress is overwhelming, seeking support from an Employee Assistance Program (EAP) or a mental health professional is essential.
For example, using a time-blocking technique to schedule work and breaks can improve focus and reduce burnout. Regular breaks throughout the day for short mindfulness exercises can help manage stress levels.
Q 27. Describe your experience working within a multidisciplinary team.
I have extensive experience collaborating within multidisciplinary teams, including psychiatrists, physicians, social workers, and occupational therapists. This collaborative approach is vital for holistic client care.
In my previous role, we worked together to develop comprehensive treatment plans for clients experiencing complex trauma. My role involved providing individual therapy, while the psychiatrist managed medication, and social workers provided case management and community resources. Regular team meetings ensured effective communication and coordination of care. This collaborative model ensures that each professional’s unique expertise is utilized to achieve the best possible outcome for the client. It also provides valuable learning opportunities and perspectives.
Q 28. What are your professional development goals related to stress and anxiety management?
My professional development goals focus on enhancing my expertise in stress and anxiety management through continued learning and skill development. This includes:
- Specialization in trauma-informed care: Deepening my understanding of trauma’s impact and developing specialized skills for working with trauma survivors.
- Advanced training in specific therapeutic modalities: Exploring evidence-based approaches like Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), and Acceptance and Commitment Therapy (ACT) to expand my therapeutic toolkit.
- Staying current with research and best practices: Regularly attending workshops, conferences, and engaging with peer-reviewed literature to maintain expertise in the field.
- Supervision and mentorship: Seeking regular supervision and mentorship from experienced professionals to continuously refine my clinical skills and ethical practices.
These goals will allow me to provide increasingly effective and compassionate care to clients struggling with stress and anxiety.
Key Topics to Learn for Stress and Anxiety Management Interview
- Understanding Stress & Anxiety: Differentiate between stress, anxiety, and related conditions. Explore the physiological and psychological responses to stress.
- Assessment & Diagnosis: Discuss various methods for assessing stress and anxiety levels in individuals, including standardized questionnaires and clinical interviews. Understand the diagnostic criteria for anxiety disorders.
- Cognitive Behavioral Therapy (CBT): Explain the principles of CBT and its application in managing stress and anxiety. Include practical examples of cognitive restructuring and behavioral experiments.
- Mindfulness & Relaxation Techniques: Describe mindfulness-based stress reduction (MBSR) and other relaxation techniques, such as deep breathing exercises, progressive muscle relaxation, and meditation. Discuss their effectiveness and application in real-world settings.
- Lifestyle Interventions: Explain the role of lifestyle factors (diet, exercise, sleep) in managing stress and anxiety. Discuss strategies for promoting healthy habits.
- Pharmacological Interventions: Briefly overview different classes of medications used to treat anxiety disorders, including their mechanisms of action and potential side effects (without going into excessive detail). Emphasize the importance of a collaborative approach with medical professionals.
- Crisis Intervention & Support Systems: Discuss strategies for managing acute anxiety and panic attacks. Explain the importance of establishing and utilizing support systems.
- Ethical Considerations: Discuss ethical considerations in working with individuals experiencing stress and anxiety, including confidentiality, informed consent, and cultural sensitivity.
Next Steps
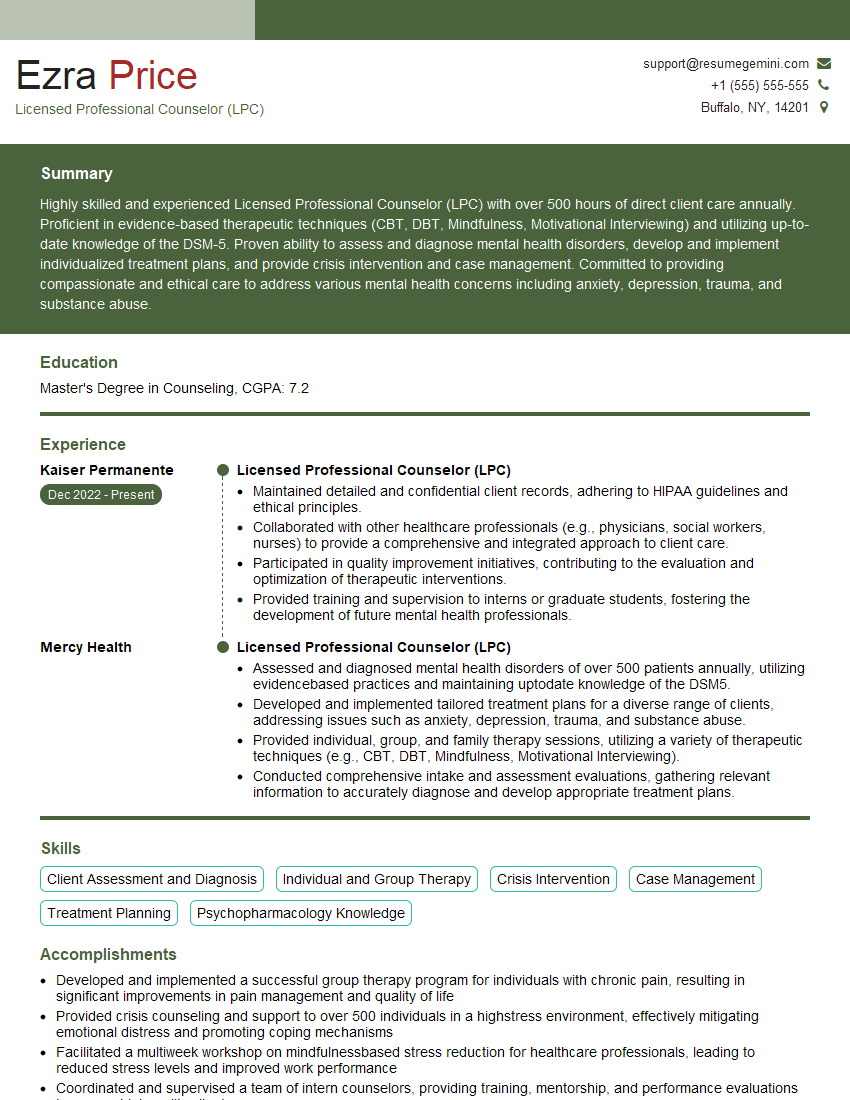
Mastering stress and anxiety management is crucial for a successful career, particularly in helping professions. A strong understanding of these concepts demonstrates your competence and empathy, making you a highly desirable candidate. To significantly boost your job prospects, create a compelling, ATS-friendly resume that highlights your skills and experience. ResumeGemini is a trusted resource that can help you build a professional and impactful resume, ensuring your application stands out. We provide examples of resumes tailored to Stress and Anxiety Management positions to help guide you.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
To the interviewgemini.com Webmaster.
Very helpful and content specific questions to help prepare me for my interview!
Thank you
To the interviewgemini.com Webmaster.
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.