Unlock your full potential by mastering the most common Neuropsychological Assessment and Interpretation interview questions. This blog offers a deep dive into the critical topics, ensuring you’re not only prepared to answer but to excel. With these insights, you’ll approach your interview with clarity and confidence.
Questions Asked in Neuropsychological Assessment and Interpretation Interview
Q 1. Describe the process of administering the Wechsler Adult Intelligence Scale (WAIS).
Administering the Wechsler Adult Intelligence Scale (WAIS) is a multifaceted process requiring careful attention to detail and adherence to standardized procedures. It begins with establishing rapport with the examinee to ensure they feel comfortable and understand the task. The test itself is comprised of several subtests, each measuring different aspects of cognitive ability. These subtests are administered in a specific order, typically starting with verbal comprehension subtests and progressing to perceptual reasoning, working memory, and processing speed subtests. The examiner carefully observes the examinee’s behavior throughout the testing session, noting any unusual responses, fatigue, or difficulty concentrating. Each subtest has specific instructions, and the examiner ensures the examinee understands before beginning. The examiner meticulously records all responses, including both correct and incorrect answers, as well as any qualitative observations. After completion of all subtests, the raw scores are converted to scaled scores and then to index scores (Verbal Comprehension, Perceptual Reasoning, Working Memory, Processing Speed) and a Full Scale IQ (FSIQ) score using standardized tables provided in the WAIS manual. This process allows for a comprehensive assessment of the individual’s cognitive strengths and weaknesses.
For example, during the Digit Span subtest (working memory), the examiner might observe if the examinee uses any strategies to remember the digits, like chunking. During the Block Design subtest (perceptual reasoning), the examiner might note how quickly the examinee completes the tasks and the level of accuracy displayed. This rich data goes beyond just a final score to paint a complete picture of cognitive functioning.
Q 2. Explain the differences between declarative and non-declarative memory.
Declarative and non-declarative memory represent two fundamental types of long-term memory. Think of it this way: declarative memory is what you can consciously recall and declare, while non-declarative memory is expressed through performance rather than conscious recollection.
- Declarative memory encompasses our knowledge of facts and events. It’s further subdivided into episodic memory (personal experiences and events) and semantic memory (general knowledge about the world). For example, remembering your last birthday party is episodic memory, while knowing the capital of France is semantic memory.
- Non-declarative memory, also known as implicit memory, includes skills and habits (procedural memory), priming (enhanced processing of previously encountered stimuli), and classical conditioning (learning through association). Riding a bicycle is a classic example of procedural memory; you don’t consciously think about each step, but you can do it smoothly. Priming might be how you faster recognize a word you recently saw.
These memory systems are distinct neuroanatomically and functionally. Declarative memory is strongly associated with the medial temporal lobes (hippocampus and surrounding structures), while non-declarative memory relies on various brain regions including the basal ganglia (procedural memory), cerebellum (motor skills), and amygdala (emotional learning). Neuropsychological assessments often evaluate both types to achieve a complete understanding of memory functioning.
Q 3. How do you interpret discrepancies between performance on different cognitive tests?
Discrepancies between performance on different cognitive tests are common and often highly informative. They rarely indicate error; rather, they point towards specific cognitive strengths and weaknesses, or the potential influence of extraneous factors. Interpretation requires a nuanced approach, considering several factors:
- Test Characteristics: Some tests are more sensitive to specific cognitive functions than others. A discrepancy might reflect a true difference in abilities, not just test sensitivity.
- Individual Factors: The examinee’s motivation, anxiety, fatigue, or educational background can affect test performance. For example, someone with low motivation might underperform on some tasks but not others.
- Neurological Factors: Specific brain regions might be affected differently by neurological conditions or injury. For example, left hemisphere damage could disproportionately impact verbal fluency scores compared to visuospatial abilities.
Interpreting discrepancies involves a systematic process: First, examine the pattern of strengths and weaknesses, not just the raw scores. Next, consider the above factors and look for a consistent pattern across multiple tests. A careful review of the qualitative observations made during testing is crucial. Finally, integrate test results with other information available (medical history, behavioral observations) to arrive at a comprehensive interpretation.
For example, a patient with a strong performance on visual-spatial tests but significantly impaired verbal fluency could suggest a right hemisphere lesion. However, this needs further investigation, taking into account other clinical findings.
Q 4. What are the ethical considerations in neuropsychological assessment?
Ethical considerations in neuropsychological assessment are paramount and govern every aspect, from informed consent to report writing. Key considerations include:
- Informed Consent: The examinee must understand the purpose, procedures, and potential limitations of the assessment. They should be given the opportunity to ask questions and withdraw at any time.
- Confidentiality: Test results are strictly confidential and should only be shared with authorized individuals (e.g., the referring physician, the examinee with their consent). Compliance with HIPAA regulations is critical.
- Competence: Neuropsychologists should only conduct assessments within their area of expertise, using validated and reliable tests. Ongoing professional development is essential to maintain competence.
- Cultural Sensitivity: Cultural background and linguistic differences can significantly impact test performance. Neuropsychologists must be aware of potential biases in tests and interpretations and adapt their approach accordingly.
- Test Security: Preventing the unauthorized disclosure of test materials is vital to maintaining the integrity of the assessments.
- Avoiding Bias: The examiner must remain objective during the testing and interpretation processes and avoid making value judgments about the patient’s performance.
Ethical violations can have severe consequences, impacting the credibility of the profession and potentially harming the examinee. Adherence to professional guidelines and ethical codes is paramount.
Q 5. How do you differentiate between aphasia and dysarthria?
Aphasia and dysarthria both affect communication but involve different mechanisms. Aphasia is a language disorder affecting the production or comprehension of spoken or written language. Dysarthria is a motor speech disorder affecting the physical production of speech sounds. Think of it this way: aphasia is a problem with the *language* system, whereas dysarthria is a problem with the *motor* system.
- Aphasia: Individuals with aphasia might have difficulty finding words (anomia), forming grammatically correct sentences (agrammatism), understanding spoken or written language (receptive aphasia), or expressing themselves clearly (expressive aphasia). Their language comprehension and production abilities are impaired despite intact motor control of their speech muscles.
- Dysarthria: Individuals with dysarthria have difficulty articulating speech sounds due to weakness, incoordination, or other motor problems affecting the muscles of the mouth, tongue, and larynx. Their language comprehension and production abilities are generally intact, but their speech is slurred, slow, or difficult to understand.
Differentiating between them involves a thorough assessment of language skills and motor speech abilities. A neuropsychologist might use standardized language tests (e.g., Boston Diagnostic Aphasia Examination) and assess motor speech control by observing articulation, rate of speech, and muscle strength. Sometimes, both conditions can co-occur.
Q 6. Explain the use of neuropsychological testing in diagnosing traumatic brain injury.
Neuropsychological testing plays a crucial role in diagnosing traumatic brain injury (TBI). It helps assess the cognitive, behavioral, and emotional consequences of the injury and provides a comprehensive picture of the patient’s functional limitations. The tests employed are tailored to the suspected nature and severity of the injury, and can identify problems that might not be readily apparent through observation alone. Common tests used include measures of attention, memory, executive functions, processing speed, and language.
For instance, a patient with a TBI might demonstrate deficits in attention, indicated by poor performance on tasks requiring sustained or divided attention. Impaired memory might be revealed through difficulties recalling stories or lists of words. Difficulties with planning and problem-solving (executive functions) are also frequently observed. The pattern of cognitive deficits helps determine the location and extent of the brain injury and aids in formulating a rehabilitation plan. Neuropsychological evaluation is vital not only for initial diagnosis but also for monitoring recovery over time and assessing the efficacy of interventions.
The results of neuropsychological testing contribute to the overall clinical picture alongside medical imaging (CT scan, MRI) and neurological examination findings. This integrated approach ensures an accurate diagnosis and effective management of the patient’s recovery.
Q 7. What are the key components of a comprehensive neuropsychological report?
A comprehensive neuropsychological report is a detailed document summarizing the findings of a neuropsychological assessment. It aims to provide a clear and concise description of the patient’s cognitive functioning, and its clinical implications. The key components include:
- Identifying Information: Patient demographics, referral source, and reason for referral.
- Background Information: Medical history, social history, educational background, and occupational history relevant to the assessment.
- Behavioral Observations: Observations of the patient’s behavior during the testing session (e.g., attention, effort, emotional state).
- Test Results: A detailed description of the tests administered, raw scores, scaled scores, and interpretive comments for each test.
- Summary of Findings: A synthesis of the test results, highlighting the patient’s cognitive strengths and weaknesses.
- Neuropsychological Diagnosis: A formal diagnosis based on the assessment findings, such as mild cognitive impairment, specific types of aphasia, or executive dysfunction.
- Clinical Impressions: An interpretation of the findings in relation to the patient’s presenting problems, and a discussion of potential contributing factors.
- Recommendations: Recommendations for further testing, treatment, or intervention based on the assessment findings.
The report should be written in clear, concise language, avoiding technical jargon whenever possible. The language used should be readily understandable by the referring physician and other healthcare professionals involved in the patient’s care.
Q 8. Describe your experience with different types of neuropsychological tests (e.g., achievement tests, executive function tests).
My experience encompasses a wide range of neuropsychological tests, categorized by the cognitive domains they assess. Achievement tests, like the Wide Range Achievement Test (WRAT-4), measure acquired academic skills in reading, spelling, and arithmetic, providing insights into learning difficulties and the impact of neurological conditions on educational attainment. Executive function tests, such as the Wisconsin Card Sorting Test (WCST) and the Trail Making Test (TMT), evaluate higher-order cognitive abilities including planning, problem-solving, cognitive flexibility, and inhibitory control. These are crucial for assessing frontal lobe function and its impact on daily life. I also have extensive experience with tests assessing memory (e.g., Wechsler Memory Scale-IV), attention (e.g., Test of Variables of Attention), language (e.g., Boston Naming Test), visuospatial skills (e.g., Rey-Osterrieth Complex Figure Test), and processing speed (e.g., Digit Symbol-Coding).
For instance, I recently used the WCST with a patient experiencing difficulties with workplace decision-making following a traumatic brain injury. Their performance revealed significant perseverative errors, indicating impaired cognitive flexibility, directly impacting their ability to adapt to changing work demands. This informed recommendations for cognitive rehabilitation focusing on strategy training and environmental modifications.
Q 9. How do you handle a patient who becomes anxious or frustrated during testing?
Patient anxiety and frustration during testing are common and require a sensitive, empathetic approach. My strategy involves building rapport before testing begins, explaining the purpose and process clearly and simply, using reassuring language, and providing frequent breaks as needed. I also carefully observe nonverbal cues for distress and adjust the pace or complexity of the tasks accordingly. Sometimes, a brief informal conversation can help reduce anxiety. If a patient is significantly distressed, I may shorten the session or postpone it to another time. Flexibility is key; the goal isn’t to push through but to obtain valid and reliable data within the patient’s capacity.
For example, with a child undergoing testing, I might incorporate playful elements into the instructions or offer small rewards for participation. For adults, acknowledging their feelings and validating their experience can be very helpful. In cases of extreme anxiety, consultation with the referring physician or a mental health professional might be warranted before proceeding with the assessment.
Q 10. Discuss the role of neuropsychological assessment in rehabilitation planning.
Neuropsychological assessment plays a pivotal role in rehabilitation planning by providing a detailed profile of cognitive strengths and weaknesses. This information is crucial for developing individualized treatment plans targeting specific deficits. For example, if a patient demonstrates impaired memory after a stroke, the assessment will highlight the nature and severity of the deficit (e.g., verbal vs. visual memory). This allows clinicians to tailor interventions such as memory strategies training, compensatory techniques, and environmental adaptations. The assessment also helps predict the patient’s potential for recovery and guides the selection of appropriate rehabilitation settings and therapies.
Imagine a patient with a traumatic brain injury exhibiting deficits in executive functions. The assessment will identify specific areas of difficulty, such as planning or problem-solving. This allows for targeted interventions, such as executive function training, which involves practicing skills like goal setting, time management, and organization through structured exercises and real-world simulations. The ultimate goal is to improve the patient’s functional independence and quality of life.
Q 11. Explain the limitations of neuropsychological testing.
Neuropsychological testing, while valuable, has inherent limitations. Test performance can be influenced by factors other than neurological conditions, such as motivation, anxiety, education level, cultural background, and pre-morbid cognitive abilities. For instance, a patient with low pre-morbid intelligence might perform poorly on certain tests regardless of neurological impairment. Similarly, a patient experiencing high levels of anxiety may underperform on tests requiring sustained attention. Furthermore, test results provide a snapshot of cognitive functioning at a specific point in time and may not accurately reflect the patient’s overall functional abilities or their response to rehabilitation. It’s vital to consider these limitations and interpret results cautiously, integrating them with information from other sources.
It’s crucial to avoid overinterpreting test scores. A single test score doesn’t define a person; it’s just one piece of the puzzle. We must always consider the clinical picture as a whole, taking into account the patient’s history, behavioral observations, and information from other sources such as family members and medical records.
Q 12. How do you incorporate information from collateral sources (e.g., family members, medical records) into your assessment?
Collateral information is indispensable in neuropsychological assessment. Information from family members, caregivers, and medical records provides valuable context and helps validate or challenge the findings from the testing session. Family members can offer insights into the patient’s pre-morbid personality, daily functioning, and the progression of symptoms. Medical records provide objective data on medical history, medications, and previous diagnoses. I carefully review all available collateral information and integrate it into my interpretation of test results, looking for converging evidence to support my conclusions. Discrepancies between test findings and collateral information may warrant further investigation.
For example, a patient might perform poorly on a memory test, but if their family reports no noticeable memory problems in daily life, this discrepancy requires careful consideration. It could suggest factors like test anxiety or a specific test sensitivity affecting their score.
Q 13. Describe your experience with different patient populations (e.g., pediatric, geriatric, forensic).
My experience spans diverse patient populations, including pediatric, geriatric, and forensic settings. Working with children requires specialized knowledge of developmental norms and the use of age-appropriate tests. Geriatric neuropsychological assessment often focuses on detecting and characterizing cognitive decline associated with aging or neurodegenerative diseases, requiring an understanding of age-related changes in cognitive functioning. Forensic neuropsychological evaluations involve assessing the impact of brain injury or illness on legal capacities, such as competency to stand trial or testamentary capacity, demanding familiarity with legal principles and ethical considerations.
The approach differs significantly across these groups. For instance, a child might need more frequent breaks and engaging test materials, whereas an elderly person might require longer processing times and adjustments for physical limitations. In forensic settings, thorough documentation and adherence to strict ethical guidelines are paramount.
Q 14. What are some common neuropsychological findings associated with Alzheimer’s disease?
Alzheimer’s disease typically presents with a characteristic pattern of neuropsychological findings. Memory impairment, particularly for recent events (anterograde amnesia), is a hallmark feature, often accompanied by difficulties with learning new information. As the disease progresses, other cognitive domains become affected, including language (aphasia), visuospatial skills (apraxia), executive functions, and attention. Specific neuropsychological tests often reveal impairments in delayed recall tasks, verbal fluency, visual constructional abilities, and set-shifting tasks. However, the presentation can be quite variable, and the specific pattern of deficits may vary between individuals.
Early detection is crucial, and a combination of neuropsychological testing, clinical examination, and neuroimaging is often used to make a diagnosis. Neuropsychological assessment helps track the progression of the disease and monitor the effectiveness of interventions.
Q 15. What are some common neuropsychological findings associated with stroke?
Stroke, a disruption of blood supply to the brain, frequently leads to a range of neuropsychological deficits. The specific impairments depend heavily on the location and extent of the brain damage.
- Cognitive Impairments: Commonly observed are problems with attention (difficulty focusing, sustaining attention), memory (both short-term and long-term, impacting recall and learning new information), executive functions (planning, problem-solving, decision-making), and processing speed (slower reaction times, difficulties with complex tasks).
- Language Deficits: Aphasia, an impairment in language comprehension or production, can manifest in various forms depending on the affected brain area. For instance, Broca’s aphasia results in difficulty producing speech, while Wernicke’s aphasia affects comprehension.
- Visuospatial Deficits: Damage to the parietal or occipital lobes can lead to difficulties with visual perception, spatial awareness, and constructional abilities (e.g., drawing or copying geometric shapes). Neglect, where a patient ignores one side of their visual field, is another possibility.
- Motor and Sensory Deficits: Stroke can cause weakness (hemiparesis) or paralysis (hemiplegia) on one side of the body, impacting motor skills and dexterity. Sensory impairments, such as numbness or loss of sensation, may also be present.
For example, a patient with a stroke affecting the left hemisphere might experience aphasia and right-sided weakness, while a patient with a right-hemisphere stroke might present with visuospatial deficits and left-sided neglect. The severity and nature of these deficits will greatly vary, influencing the patient’s overall functional capacity.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you differentiate between malingering and genuine cognitive impairment?
Differentiating between malingering (feigning cognitive impairment) and genuine cognitive impairment is crucial for accurate diagnosis and treatment planning. It requires a thorough and multi-faceted approach.
- Inconsistency in Performance: Malingerers may show inconsistencies in their test performance that are not typical of genuine cognitive deficits. For instance, they might perform poorly on easy tasks but surprisingly well on more difficult ones. Genuine impairment usually shows a more consistent pattern of difficulty across different task demands.
- Symptom Validity Testing (SVT): Specialized tests like the Test of Memory Malingering (TOMM) or the Word Memory Test are designed to detect inconsistent or suboptimal effort. These tests assess the likelihood of a patient intentionally underperforming.
- Collateral Information: Information gathered from family members, caregivers, or previous medical records can offer valuable insights into the patient’s premorbid functioning and the consistency of their reported symptoms. Discrepancies between self-report and collateral information raise suspicion of malingering.
- Observation of Behavior: Careful observation of the patient during the assessment can reveal clues. A lack of effort, inconsistent complaints, or unusual behaviors might suggest malingering. However, it’s important to note that depression, anxiety, or other factors could mimic aspects of malingering.
- Neuropsychological Test Profile: A pattern of scores that is highly atypical or doesn’t fit a known neurological or psychiatric condition may indicate feigning. For instance, extremely low performance on tasks sensitive to effort combined with relatively preserved performance on other measures should be scrutinized.
The process requires clinical judgment. It is not simply a matter of a single test, but rather the integration of multiple data points. Often, a combination of SVT, behavioral observations, and collateral information, interpreted in the context of the overall test profile, can lead to a more accurate determination.
Q 17. Discuss your approach to managing test anxiety in patients.
Test anxiety is a common issue in neuropsychological assessment that can significantly impact performance and undermine the accuracy of results. Managing it requires a sensitive and proactive approach.
- Pre-Assessment Preparation: Begin by clearly explaining the purpose and procedures of the assessment in a calming and reassuring manner. Emphasize that there are no right or wrong answers and that the goal is to understand their cognitive strengths and weaknesses.
- Creating a Relaxing Environment: Ensure the testing environment is comfortable and minimizes distractions. A quiet and private room with appropriate lighting and temperature can help reduce anxiety.
- Building Rapport: Establish a strong rapport with the patient, creating a trusting and empathetic atmosphere. This can involve engaging in casual conversation before starting the assessment, demonstrating genuine interest in their well-being.
- Providing Frequent Breaks: Allow for breaks as needed to prevent fatigue and help the patient manage anxiety. Flexibility in scheduling is crucial to accommodate individual needs.
- Using Encouragement and Positive Reinforcement: Offer regular encouragement and positive feedback throughout the assessment, emphasizing their efforts and progress rather than their performance.
- Cognitive Restructuring Techniques: If anxiety is significant, consider employing brief cognitive behavioral techniques such as relaxation exercises or guided imagery to help the patient manage their anxious thoughts and feelings.
In some cases, medication to address anxiety might be necessary, but this should be discussed and managed in coordination with the patient’s physician. The goal is to create an assessment experience that is as stress-free as possible so that the patient can perform to their best ability.
Q 18. What are the different types of attention and how are they assessed?
Attention, the ability to focus on specific stimuli and filter out distractions, is not a unitary construct. Various types of attention exist and are assessed differently.
- Sustained Attention: The ability to maintain focus on a task over a period of time. This is often assessed using continuous performance tests (CPTs), which require the patient to respond to specific stimuli while ignoring others over an extended duration. Examples include the CPT-II and the Test of Variables of Attention (TOVA).
- Selective Attention: The ability to focus on a target stimulus while ignoring competing stimuli. Tests like the Stroop Color-Word Test and the Trail Making Test (Part A) assess this ability. For example, in the Stroop test, individuals must name the color of ink used to print a word, while ignoring the word itself.
- Alternating Attention: The ability to switch attention between different tasks or stimuli. The Trail Making Test (Part B), which involves switching between numbers and letters, is a common assessment.
- Divided Attention: The ability to attend to multiple tasks or stimuli simultaneously. Tests often involve dual-task paradigms, such as simultaneously performing a verbal and a visual task. This might involve listening to a story and tracking a moving object simultaneously.
Assessment of attention involves a combination of behavioral observation and standardized tests, tailored to the specific suspected deficit or clinical question. The results inform the clinical interpretation and are not interpreted in isolation but within the context of the complete neuropsychological evaluation.
Q 19. How do you interpret visual-spatial and constructional deficits?
Visual-spatial and constructional deficits refer to difficulties with processing visual information and constructing spatial relationships. These deficits are often associated with damage to the parietal and occipital lobes, but can also stem from other neurological conditions.
- Visual Perception Deficits: Problems recognizing or identifying visual stimuli, distinguishing between similar shapes, or perceiving depth and distance.
- Spatial Awareness Deficits: Difficulties understanding spatial relationships between objects or one’s body in space (e.g., difficulty navigating familiar environments).
- Constructional Apraxia: Difficulty drawing, copying, or constructing objects. Examples include the inability to accurately copy a geometric design or draw a clock face.
- Neglect: The failure to attend to or respond to stimuli in one half of visual space, typically the side opposite to the brain lesion (e.g., unilateral neglect after right-hemisphere stroke).
Interpretation involves careful analysis of performance on standardized tests such as the Rey-Osterrieth Complex Figure Test (RCFT), clock drawing, and line bisection tasks. The patterns of errors (e.g., omissions, distortions, spatial disorganization) provide crucial information for localization and diagnosis. For example, difficulties in copying complex figures with omissions on one side might suggest unilateral spatial neglect. The severity and nature of these deficits profoundly influence everyday activities, such as dressing, drawing, and even reading.
Q 20. Explain the concept of cognitive reserve and its implications for neuropsychological assessment.
Cognitive reserve refers to the brain’s resilience to injury or disease. It represents the brain’s capacity to cope with damage by using alternative neural pathways or compensatory strategies. This concept is crucial in neuropsychological assessment because it influences the relationship between brain pathology and clinical presentation.
Individuals with high cognitive reserve, often due to factors like higher education, complex occupations, and engaging hobbies, may show fewer clinical symptoms despite substantial brain pathology. Conversely, individuals with low cognitive reserve might exhibit more pronounced cognitive impairments even with less extensive brain damage.
In neuropsychological assessment, understanding cognitive reserve is important for:
- Interpreting Test Results: Considering cognitive reserve helps differentiate between true cognitive decline and resilience. For instance, an individual with high cognitive reserve might perform better on neuropsychological tests than expected based on the severity of their brain lesion.
- Predicting Functional Outcomes: Individuals with higher cognitive reserve tend to show better functional outcomes and adaptation following brain injury or disease.
- Tailoring Interventions: Understanding cognitive reserve can inform the development of more effective and personalized interventions. For example, leveraging pre-existing cognitive strengths might be a valuable therapeutic strategy.
Measuring cognitive reserve directly is challenging. However, educational attainment, occupational complexity, and leisure activities are often used as proxies. This information is gathered through detailed history taking and questionnaires and is considered alongside the neuropsychological test data to provide a more comprehensive understanding of the patient’s cognitive functioning.
Q 21. How do you tailor your assessment to a patient’s specific needs and background?
Tailoring neuropsychological assessment to a patient’s specific needs and background is essential for obtaining meaningful and clinically relevant results. This involves considering several factors:
- Patient’s Age and Education: Using age- and education-matched norms is crucial for accurate interpretation. A standardized test score is meaningless without considering the individual’s baseline level of cognitive ability.
- Cultural and Linguistic Background: The assessment should be culturally sensitive and appropriate for the patient’s linguistic background. Using translated or culturally adapted tests might be necessary, and the clinician should be aware of potential cultural biases that might influence performance.
- Medical History and Presenting Complaints: The specific cognitive domains and functions that need to be evaluated should be guided by the patient’s medical history and the reason for referral. For instance, if a patient complains of memory problems, memory tests will be heavily emphasized.
- Premorbid Functioning: Assessing premorbid functioning (prior to illness onset) through collateral information (from family or friends) or prior records can provide a crucial baseline against which to compare current performance.
- Physical and Sensory Limitations: The assessment should be adapted to account for any physical or sensory impairments the patient may have, such as visual or auditory difficulties, or motor limitations that might affect test performance. This may involve choosing alternative methods of administration or using assistive devices.
A flexible and individualized approach ensures the assessment is both thorough and sensitive to the unique characteristics of each patient. The goal is not only to identify deficits but also to understand the patient’s strengths and coping mechanisms, leading to more comprehensive and useful clinical recommendations.
Q 22. Describe your experience with using computerized neuropsychological assessment tools.
My experience with computerized neuropsychological assessment tools is extensive. I’m proficient in utilizing various software platforms, including but not limited to, the computerized versions of the WAIS, WMS, and various other standardized tests. These tools offer several advantages: they automate scoring, reducing the risk of human error, and provide immediate feedback on test performance. They also often include built-in features for generating reports, saving significant time and streamlining the assessment process. For example, I regularly use the computerized version of the Trail Making Test, which automatically records response times and error rates, providing a more objective measure than manual administration. However, it’s crucial to remember that technology is a tool, and clinical judgment remains paramount. Interpretation still necessitates a comprehensive understanding of the patient’s background, presentation, and performance on the test in relation to established normative data. I always prioritize ensuring the technological aspects don’t overshadow the nuanced aspects of human interaction and clinical observation during the assessment.
Q 23. Explain the use of normative data in neuropsychological interpretation.
Normative data is absolutely essential for interpreting neuropsychological test results. Think of it as a benchmark; it provides a comparison point against which an individual’s performance can be evaluated. These data sets, typically obtained from large, representative samples of the population, indicate the average performance and range of scores for individuals of similar age, education, and demographic characteristics. For instance, if a patient scores below the fifth percentile on a memory test, it suggests their performance is significantly lower than what is expected for their age group. However, it’s important to remember that normative data is not without its limitations. The representativeness of the sample is crucial; if the normative data doesn’t accurately reflect the diversity of the population, interpretations may be skewed. For example, reliance on outdated or culturally biased norms could lead to misinterpretations and inaccurate diagnoses. Therefore, choosing age and education-matched normative data, carefully examining the sample demographics of the data, and being mindful of any cultural considerations are all critical aspects of accurate interpretation.
Q 24. How do you maintain confidentiality and protect patient information?
Maintaining patient confidentiality and protecting their information is my utmost priority. I adhere strictly to HIPAA regulations and all relevant ethical guidelines. This includes securing all patient files both electronically and physically. Electronic records are password-protected and stored on secure servers with appropriate access restrictions. Paper records are kept in locked cabinets. I never discuss patient information with unauthorized individuals. Furthermore, I obtain informed consent before any assessment, explaining the purpose, procedures, and limitations of the evaluation, including how the data will be used and stored. I also emphasize the importance of privacy and data security during the consent process. Finally, I regularly review and update my knowledge of data privacy regulations and best practices to ensure ongoing compliance and to continually improve my ability to safeguard patient information.
Q 25. What is your understanding of the impact of cultural factors on neuropsychological assessment?
Cultural factors can significantly influence performance on neuropsychological tests and, consequently, the interpretation of results. It’s crucial to understand that cultural background can affect language proficiency, familiarity with testing formats, and even the very concept of the task being presented. For example, a patient from a culture that emphasizes collectivism might interpret a task differently than a patient from an individualistic culture. Similarly, a patient with limited English proficiency might struggle with language-based tests regardless of their actual cognitive abilities. To mitigate the impact of these factors, I employ culturally sensitive assessment practices. This includes using interpreters when necessary, selecting tests that minimize cultural bias, and adapting test administration procedures when appropriate. It also involves taking into account the patient’s educational and sociocultural background during the interpretation of test results, ensuring a comprehensive and accurate assessment that doesn’t misattribute cultural differences as cognitive deficits.
Q 26. Describe a challenging case in your experience and how you addressed it.
One particularly challenging case involved a patient who presented with significant memory difficulties and reported experiencing significant emotional distress following a mild traumatic brain injury (mTBI). Standard neuropsychological testing revealed inconsistencies in performance, making it difficult to definitively determine the extent of cognitive impairment. The patient also presented with significant symptoms of anxiety and depression which could have confounded the results. To address this, I used a multi-faceted approach. First, I employed a flexible testing approach, utilizing a combination of standardized and informal measures. Second, I incorporated collateral information from family members and medical records. Third, and most importantly, I collaborated closely with the patient’s psychiatrist and therapist to gain a more holistic understanding of the patient’s presentation. By combining these data sources, and working as part of a comprehensive treatment team, we were able to build a more accurate picture of the patient’s cognitive and emotional state, allowing for a more targeted and effective treatment plan.
Q 27. How do you stay current with advances in neuropsychology?
Staying current with advances in neuropsychology is vital for providing high-quality care. I achieve this through several strategies: I regularly attend professional conferences and workshops, such as those offered by the National Academy of Neuropsychology. I actively participate in continuing education programs to update my knowledge on new assessment tools and techniques. I subscribe to professional journals like the Archives of Clinical Neuropsychology and the Journal of the International Neuropsychological Society. Additionally, I maintain active professional memberships, engaging with colleagues and networking to share knowledge and stay abreast of the latest research findings and clinical guidelines. This continuous learning allows me to refine my skills, adopt best practices, and ensure that my assessment and interpretation methods are evidence-based and up-to-date.
Q 28. Describe your experience working with interdisciplinary teams.
Interdisciplinary collaboration is crucial in neuropsychology. I have extensive experience working with various professionals, including neurologists, psychiatrists, physiatrists, occupational therapists, speech-language pathologists, and social workers. In my experience, these collaborations enhance the comprehensive evaluation and treatment planning for our patients. For example, in cases of traumatic brain injury (TBI), I work closely with the neurologist to understand the extent and nature of the injury, and with the occupational therapist to address the patient’s functional limitations. This collaborative approach helps create a holistic perspective, integrating cognitive data with other relevant medical, psychological, and social information, to create a treatment plan tailored to the patient’s specific needs and to optimize their recovery and rehabilitation process.
Key Topics to Learn for Neuropsychological Assessment and Interpretation Interview
- Cognitive Domains: Understanding the assessment of attention, memory, executive functions, language, visuospatial skills, and motor skills. Consider theoretical frameworks underlying these domains and their interplay.
- Test Selection & Administration: Knowing the appropriate tests for different clinical presentations and populations, including standardized administration procedures and ethical considerations.
- Interpreting Test Results: Mastering the art of integrating quantitative and qualitative data from multiple sources to generate a comprehensive neuropsychological profile. Practice analyzing patterns of strengths and weaknesses.
- Differential Diagnosis: Developing the ability to discriminate between various neurological and psychiatric conditions based on neuropsychological test findings. Focus on case conceptualization and diagnostic reasoning.
- Report Writing: Creating clear, concise, and clinically relevant reports that communicate complex information effectively to other healthcare professionals.
- Ethical and Legal Considerations: Understanding the ethical implications of neuropsychological assessment, including confidentiality, informed consent, and cultural competence. Familiarity with relevant legal frameworks is also crucial.
- Neuroanatomy and Neurophysiology: A foundational understanding of brain structure and function is essential for interpreting test results and understanding the underlying neurological basis of cognitive impairments.
- Specific Disorders & Their Neuropsychological Profiles: Develop expertise in recognizing the characteristic cognitive profiles associated with conditions like traumatic brain injury, stroke, dementia, and ADHD.
- Validity & Reliability: Critically evaluate the psychometric properties of neuropsychological tests, understanding concepts of validity, reliability, and sensitivity/specificity.
- Case Studies & Problem Solving: Practice analyzing hypothetical case studies to refine your diagnostic and interpretive skills. Focus on identifying inconsistencies and developing well-reasoned conclusions.
Next Steps
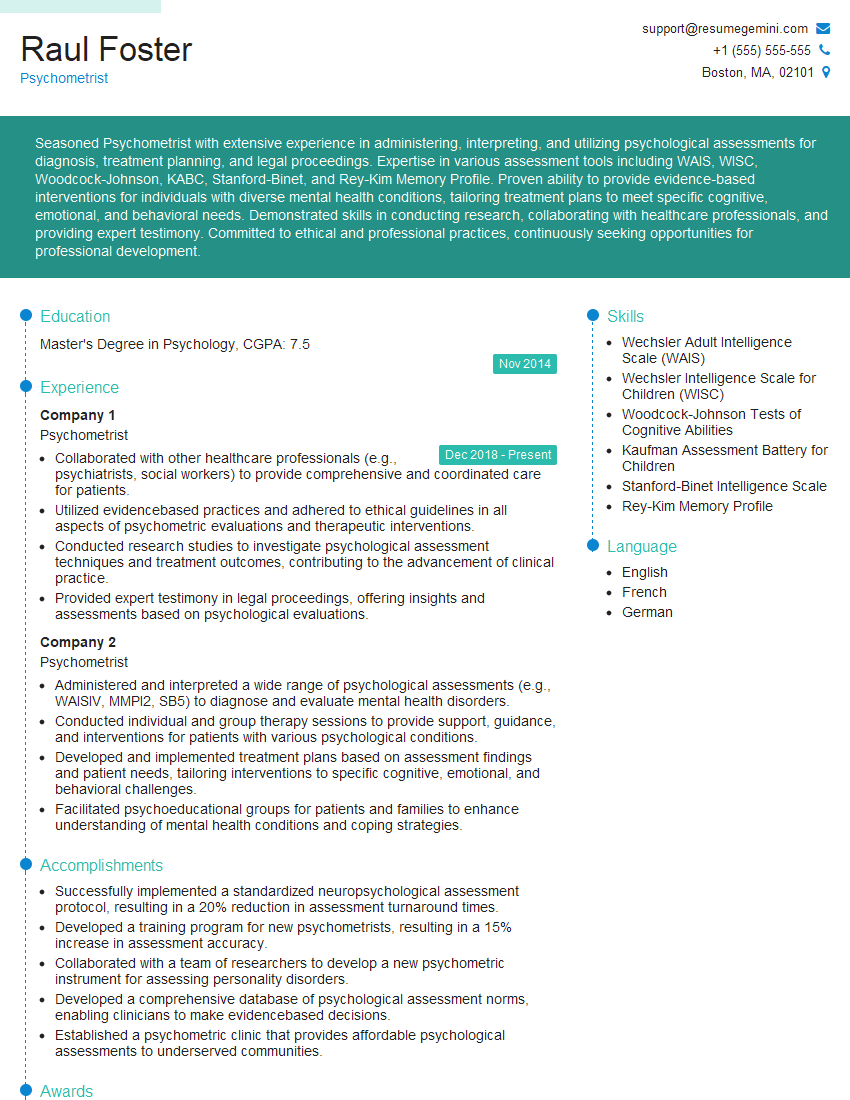
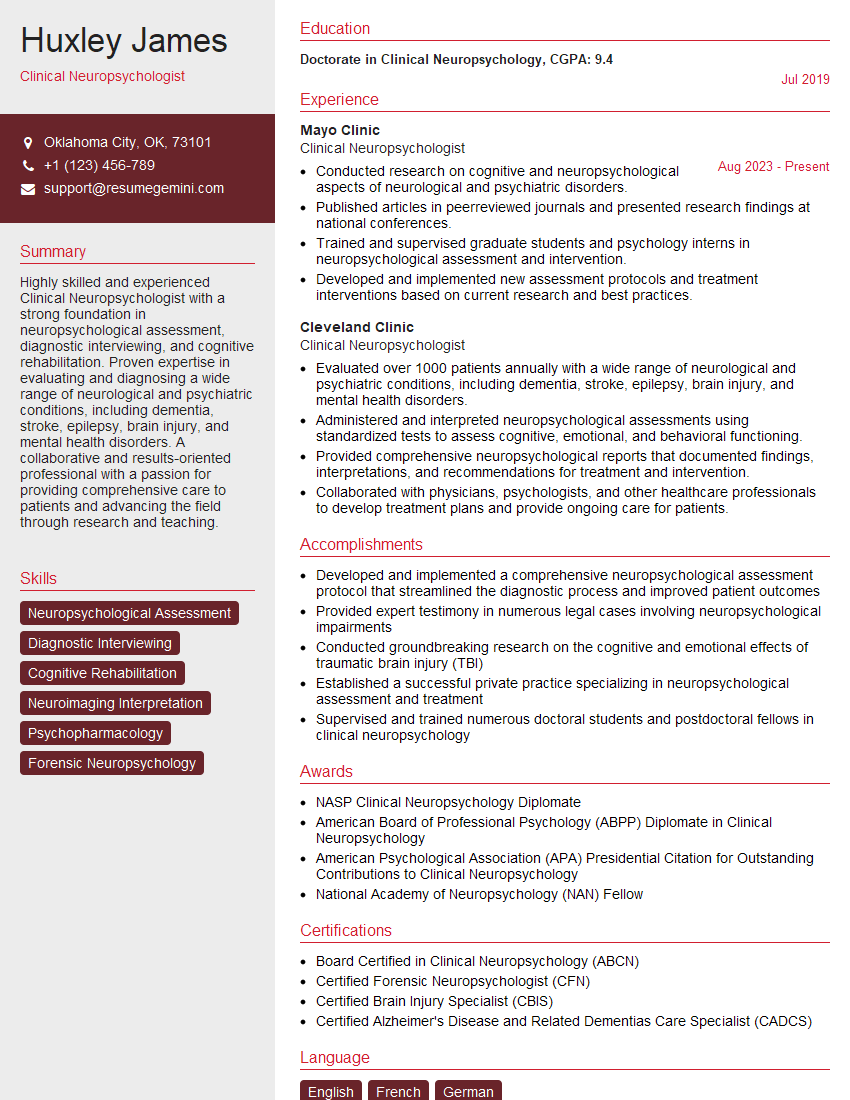
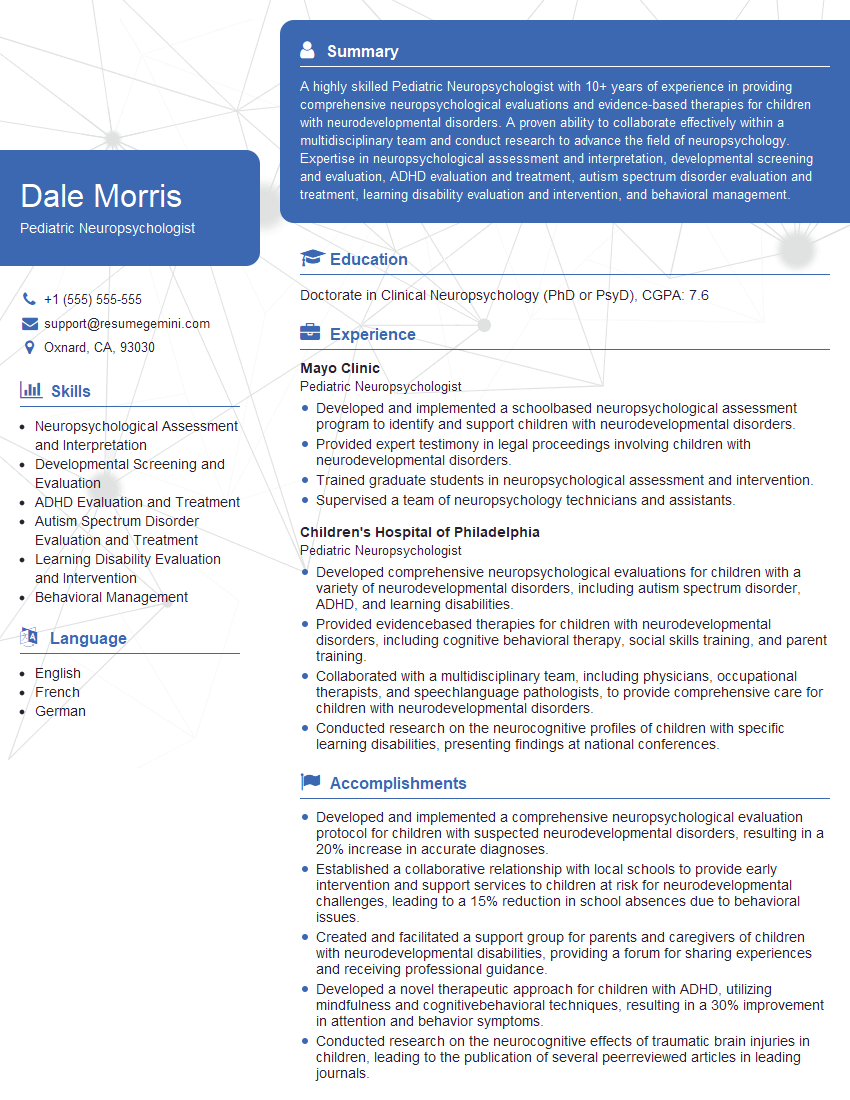
Mastering Neuropsychological Assessment and Interpretation opens doors to rewarding and impactful careers in clinical neuropsychology, research, and related fields. To maximize your job prospects, invest time in creating a strong, ATS-friendly resume that highlights your skills and experience effectively. ResumeGemini is a trusted resource that can help you build a professional resume tailored to the specific demands of this competitive field. Examples of resumes tailored to Neuropsychological Assessment and Interpretation are available to guide you.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
To the interviewgemini.com Webmaster.
Very helpful and content specific questions to help prepare me for my interview!
Thank you
To the interviewgemini.com Webmaster.
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.