Every successful interview starts with knowing what to expect. In this blog, we’ll take you through the top Pediatric Neuro-Otology interview questions, breaking them down with expert tips to help you deliver impactful answers. Step into your next interview fully prepared and ready to succeed.
Questions Asked in Pediatric Neuro-Otology Interview
Q 1. Describe the different types of hearing loss seen in pediatric patients.
Hearing loss in children can be classified in several ways. The most common classification is based on the location of the problem within the auditory system:
- Conductive Hearing Loss: This occurs when sound waves cannot effectively travel through the outer or middle ear. Think of it like a clogged pipe – sound can’t reach the inner ear. Common causes include ear infections (otitis media), fluid buildup in the middle ear (otitis media with effusion), and abnormalities of the ear canal or eardrum. A child might have difficulty hearing soft sounds but hear loud sounds normally.
- Sensorineural Hearing Loss: This involves damage to the inner ear (cochlea) or the auditory nerve. It’s like a problem with the receiver or the wires leading to the brain. This type of loss can affect the ability to hear a range of sounds and often causes difficulty understanding speech, even at loud volumes. Causes can include genetic factors, prematurity, infections like cytomegalovirus (CMV), and noise exposure.
- Mixed Hearing Loss: This combines elements of both conductive and sensorineural hearing loss. The child might have a problem with sound transmission *and* damage to the inner ear or nerve.
- Central Hearing Loss: This is less common and involves problems with the brain’s processing of auditory information. Even if the ears and nerve are working correctly, the brain may struggle to interpret sounds. This type often presents with difficulties in speech comprehension despite relatively normal hearing tests.
It’s crucial to remember that the underlying cause of hearing loss varies greatly and needs thorough investigation.
Q 2. Explain the diagnostic process for auditory neuropathy spectrum disorder (ANSD).
Diagnosing Auditory Neuropathy Spectrum Disorder (ANSD) requires a multi-step approach because it presents with unusual characteristics. ANSD involves normal outer and middle ear function, but abnormal auditory nerve function. Think of it as the message getting scrambled along the way to the brain, even though the phone line is clear.
- Comprehensive Hearing Evaluation: This includes auditory brainstem response (ABR) testing, which assesses the nerve’s response to sound. In ANSD, the ABR waves will be abnormal or absent despite normal hearing thresholds in some tests. Otoacoustic emissions (OAEs) are usually present, indicating normal cochlear function.
- Behavioral Tests: These assess how the child responds to sounds, often showing inconsistent hearing across different tests. This inconsistency is a hallmark of ANSD.
- Imaging Studies: Although often normal, MRI or CT scans of the brainstem might be considered to rule out other conditions.
- Genetic Testing: Genetic causes are being explored more now, and testing might be considered if a genetic condition is suspected.
The diagnostic process focuses on distinguishing ANSD from other hearing disorders and identifying the degree of hearing impairment. A team approach involving audiologists, neurologists, and geneticists is often necessary.
Q 3. What are the common causes of vertigo in children?
Vertigo in children, a sensation of spinning or dizziness, can stem from various sources. It’s essential to consider the child’s age and associated symptoms.
- Benign Paroxysmal Positional Vertigo (BPPV): This is common in children and involves the displacement of tiny calcium crystals in the inner ear. It triggers brief episodes of vertigo with specific head movements. Imagine tiny rocks irritating the balance sensors.
- Vestibular Migraine: Migraine headaches are often accompanied by vestibular symptoms, including dizziness, imbalance, and nausea. It’s frequently misdiagnosed as other conditions.
- Viral Labyrinthitis/Vestibular Neuronitis: Viral infections can inflame the inner ear, causing vertigo, nausea, and hearing loss.
- Central Nervous System (CNS) Disorders: In rare cases, vertigo might result from brain tumors, stroke, or other neurological conditions. This is particularly important to consider with persistent or severe vertigo.
- Ototoxicity: Certain medications, particularly antibiotics, can damage the inner ear, leading to hearing loss and vertigo.
A thorough history, including the characteristics of the vertigo, associated symptoms, and medical history, is critical for accurate diagnosis.
Q 4. Discuss the management of Meniere’s disease in a pediatric population.
Meniere’s disease, characterized by episodic vertigo, tinnitus (ringing in the ears), hearing loss, and a feeling of fullness in the ear, is uncommon in children. When it does occur, the diagnosis and management are complex.
Management focuses on symptom control, as there is no cure. It typically involves:
- Medical Management: Low-sodium diets might help manage fluid balance. Medications to control vertigo (antiemetics and vestibular suppressants) and tinnitus are often used. Diuretics can be considered in some instances.
- Vestibular Rehabilitation Therapy (VRT): Exercises help the brain adapt to inner ear problems and reduce dizziness.
- Surgical Interventions: Surgery is rarely indicated in children. Options might include endolymphatic sac surgery (to reduce inner ear pressure) or vestibular neurectomy (severing the vestibular nerve) in severe cases refractory to medical management. However, the risks associated with surgery often outweigh the benefits in young patients.
Given the rarity in children, careful consideration of the diagnosis and rigorous non-surgical management is crucial before resorting to invasive procedures.
Q 5. How would you approach a child with suspected otitis media with effusion?
Otitis media with effusion (OME), or middle ear effusion, is the presence of fluid behind the eardrum without infection. Think of it as a build-up of fluid that doesn’t cause pain like an active ear infection.
My approach involves:
- Comprehensive History and Physical Exam: I’d assess the child’s hearing, check the eardrum using an otoscope (looking in the ear with a special instrument), and ask about symptoms like hearing loss, speech delay, or balance issues.
- Tympanometry: This test measures the movement of the eardrum and helps determine the presence and nature of the middle ear fluid.
- Watchful Waiting: Many cases of OME resolve spontaneously within a few months. I might recommend observing for improvement, especially if the hearing loss is minimal.
- Hearing Screening: This is vital to assess the impact of the fluid on hearing and speech development.
- Medical Management (if indicated): If the OME persists, hearing loss is significant, or speech development is affected, I might consider antibiotics if there’s suspicion of underlying infection, or even myringotomy (placing pressure-equalizing tubes) to drain the fluid.
The decision for intervention depends on the severity of the effusion, the duration, the child’s age, and the impact on hearing and speech development.
Q 6. What are the different surgical options for cholesteatoma in children?
Cholesteatoma, a growth of skin cells in the middle ear, requires surgical removal to prevent complications like hearing loss, facial nerve paralysis, and meningitis. In children, surgical options include:
- Tympanomastoidotympany: This is the most common approach. It involves removing the cholesteatoma and reconstructing the middle ear structures. This can be done via a canal wall up or canal wall down approach, depending on the extent of the cholesteatoma.
- Modified Radical Mastoidectomy: Used in cases where the cholesteatoma has extensively damaged the middle ear. It involves removing the cholesteatoma, the diseased ossicles, and a portion of the mastoid bone.
- Radical Mastoidectomy: Reserved for severe cases where extensive damage necessitates the removal of a significant portion of the middle ear and mastoid.
The choice of surgical technique depends on the size and location of the cholesteatoma, the extent of middle ear involvement, and the surgeon’s preference. Post-operative management is vital to monitor for complications and ensure proper healing.
Q 7. Explain the role of vestibular rehabilitation in pediatric patients.
Vestibular rehabilitation therapy (VRT) plays a crucial role in helping children recover from vestibular disorders. It involves a series of exercises designed to improve balance, reduce dizziness, and retrain the brain to compensate for inner ear dysfunction. Think of it as physical therapy for the balance system.
VRT exercises can include:
- Gaze Stabilization Exercises: These improve the ability to maintain clear vision while the head is moving. Examples include tracking a moving object while changing head positions.
- Balance Exercises: These improve balance and postural control. This might involve standing on one leg, tandem walking, or using balance boards.
- Habituation Exercises: These involve repeatedly performing movements that trigger dizziness to help the brain adapt and reduce the sensation.
VRT is tailored to the child’s specific needs and age. It often requires close collaboration between the therapist, child, and parents to ensure adherence and progress. Early intervention is beneficial in helping children adapt and improve their functional abilities.
Q 8. How do you differentiate between central and peripheral vertigo in children?
Differentiating between central and peripheral vertigo in children requires a careful clinical evaluation. Peripheral vertigo originates from the inner ear or vestibular nerve, while central vertigo stems from the brainstem or cerebellum. Think of it like this: peripheral vertigo is a problem with the phone line itself (inner ear/vestibular nerve), while central vertigo is a problem with the phone switchboard (brainstem/cerebellum) that processes the signal.
Key differences often include the nature of vertigo. Peripheral vertigo typically presents with intense, spinning sensations (vertigo) often triggered by specific head movements (e.g., benign paroxysmal positional vertigo, or BPPV). It’s often accompanied by nausea, vomiting, and nystagmus (involuntary eye movements) that usually has a specific direction and is suppressed by visual fixation. In contrast, central vertigo may be less intense, less clearly spinning, and may be associated with other neurological symptoms such as diplopia (double vision), ataxia (difficulty with coordination), numbness, or weakness. The nystagmus in central vertigo is often less predictable and not always suppressed by fixation.
Clinical tests such as the head impulse test (HIT), Dix-Hallpike maneuver (for BPPV), and assessment of nystagmus characteristics are crucial. Neuroimaging (MRI) might be necessary to rule out central causes in ambiguous cases. A thorough history focusing on the onset, duration, character of vertigo, and associated symptoms is paramount.
Q 9. Describe the assessment and management of a child with sensorineural hearing loss.
Assessing a child with sensorineural hearing loss begins with a comprehensive history, including family history of hearing loss, prenatal and perinatal events (e.g., infections, prematurity), and any exposure to ototoxic drugs or noise. A detailed physical examination focusing on the ears, head, and neurologic system is crucial. Auditory testing is paramount and usually involves several techniques.
- Otoscopy: Visual examination of the ear canal and eardrum to rule out middle ear problems.
- Tympanometry: Measures middle ear function.
- Pure-tone audiometry: Determines the thresholds of hearing at different frequencies using behavioral responses (if the child is old enough to cooperate) or objective measures such as auditory brainstem response (ABR) for infants and young children.
- Speech audiometry: Assesses speech understanding.
Management is individualized and depends on the degree and type of hearing loss. Hearing aids are often the first line of management for mild to moderate hearing loss. Early intervention programs are essential, involving speech-language pathologists, audiologists, and educators to support the child’s speech and language development. For severe to profound hearing loss, cochlear implantation may be considered.
Q 10. Discuss the indications and contraindications for cochlear implantation in children.
Indications for cochlear implantation in children typically include bilateral, severe-to-profound sensorineural hearing loss that doesn’t respond adequately to hearing aids and significantly impacts speech and language development. Other factors considered include the child’s age, overall health, and family support.
Contraindications are relatively rare but can include active middle ear infections, certain medical conditions that might interfere with surgery or device function, or lack of adequate family support to facilitate post-implantation rehabilitation. A thorough multidisciplinary assessment is always necessary before recommending cochlear implantation.
Q 11. What are the potential complications of cochlear implantation?
Potential complications of cochlear implantation can be categorized into immediate post-operative and long-term complications. Immediate complications might include wound infection, bleeding, cerebrospinal fluid leak, facial nerve paralysis, and device malfunction. These are usually managed with appropriate medical and surgical interventions.
Long-term complications are less frequent but can include device malfunction (requiring revision surgery), meningitis (rare but serious), and persistent dizziness or tinnitus. Regular follow-up appointments are vital for monitoring device function and addressing any emerging issues. Good hygiene practices to minimize infection risk are also crucial.
Q 12. How would you counsel parents regarding their child’s hearing loss diagnosis?
Counseling parents about their child’s hearing loss diagnosis requires empathy, patience, and a collaborative approach. I start by explaining the diagnosis clearly and simply, avoiding overly technical jargon. I provide information on the type and severity of hearing loss, its impact on speech and language development, and available interventions like hearing aids or cochlear implants.
I emphasize the importance of early intervention and provide resources to support the family. This includes referrals to audiologists, speech-language pathologists, educational support services, and support groups for families with hearing-impaired children. I address the parents’ concerns and emotions, acknowledging the emotional impact of the diagnosis, and offer ongoing support and guidance. I emphasize that their child can lead a full and fulfilling life with appropriate interventions and support.
Q 13. Describe your experience with auditory brainstem response (ABR) testing.
Auditory Brainstem Response (ABR) testing is an electrophysiological test that measures the electrical activity in the auditory brainstem in response to sound stimuli. It’s invaluable for assessing hearing in infants and young children, as well as for identifying auditory neuropathy spectrum disorder (ANSD). I have extensive experience performing and interpreting ABRs. The test involves placing electrodes on the scalp to record the electrical activity. Different sound stimuli are presented, and the latency and amplitude of the waves are analyzed to determine the integrity of the auditory pathway.
I use ABR to objectively assess hearing sensitivity in infants and young children who cannot provide behavioral responses. It is particularly helpful for diagnosing hearing loss in newborns and infants, identifying the presence of retrocochlear lesions, and monitoring the progress of patients with certain neurological conditions. ABR results are interpreted in conjunction with other auditory tests and clinical findings for a comprehensive diagnosis.
Q 14. What are the common causes of delayed speech development in children with hearing loss?
Delayed speech development in children with hearing loss is primarily due to limited auditory input. The brain needs consistent auditory stimulation during critical periods of development to learn speech and language. Without adequate hearing, children miss opportunities to learn sound patterns, phonemic distinctions, and the nuances of language.
Other factors can contribute, including the age of onset of hearing loss (earlier onset is associated with more significant delays), the severity of hearing loss, the type of hearing loss, and the effectiveness of intervention strategies. For example, a child with profound hearing loss diagnosed late may have more significant delays than a child with mild hearing loss diagnosed early and provided with appropriate intervention.
In addition to auditory deprivation, limited opportunities for social interaction and linguistic exposure can further impede speech development. This highlights the importance of early identification and intervention to maximize a child’s linguistic and communicative potential.
Q 15. Discuss the impact of hearing loss on language acquisition.
Hearing loss significantly impacts language acquisition, particularly in young children whose brains are rapidly developing language skills. Think of it like this: language learning is like building a house; auditory input is the building material. Without sufficient, clear auditory input, the ‘house’ of language is built imperfectly, leading to delays or difficulties.
- Early detection is crucial: Children with hearing loss may miss crucial early exposures to sounds and speech patterns, hindering their ability to discriminate phonemes (distinct units of sound). This delay can cascade into difficulties with vocabulary development, grammar, and overall comprehension.
- Impact on speech production: Difficulty hearing sounds leads to difficulty producing them correctly, resulting in speech delays or articulation errors. They may not hear their own speech errors, reinforcing incorrect pronunciation.
- Social-emotional development: Children with untreated hearing loss may struggle with social interaction due to communication difficulties, leading to frustration, isolation, and potential behavioral problems.
For example, a child with significant hearing loss might only pick up parts of conversations, leading to incomplete understanding and difficulties participating in classroom discussions. Early intervention, including hearing aids or cochlear implants along with speech therapy, is essential to mitigate these effects.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Explain the role of assistive listening devices (ALDs) in pediatric hearing rehabilitation.
Assistive listening devices (ALDs) play a vital role in bridging the gap between sound and the child’s auditory system. They amplify sounds and improve the signal-to-noise ratio, making it easier for children with hearing loss to participate in daily activities and access auditory information.
- Hearing aids: These are the most common ALDs, amplifying sounds across different frequencies to compensate for hearing loss. Modern hearing aids are technologically advanced, offering features like noise reduction and directional microphones.
- FM systems: These transmit sound directly from a speaker (e.g., teacher) to the child’s hearing aid or a receiver, bypassing background noise. This is particularly beneficial in classrooms or other noisy environments.
- Personal amplifiers: These devices, often smaller than hearing aids, amplify sounds directly to the user’s ears and can be helpful for people with mild hearing loss or in specific situations.
- Cochlear implants: For severe to profound hearing loss, cochlear implants bypass damaged hair cells in the inner ear and directly stimulate the auditory nerve, providing a different type of auditory input.
The choice of ALD depends on the severity and type of hearing loss, the child’s age and developmental needs, and the listening environment. Proper fitting and regular monitoring by an audiologist are essential to ensure optimal benefit.
Q 17. How do you assess balance disorders in children?
Assessing balance disorders in children requires a multi-faceted approach, incorporating both subjective and objective measures. It’s crucial to remember that children may not always be able to accurately describe their symptoms, so observation and play-based assessment are key.
- History: A thorough medical history focusing on the onset, frequency, duration, and associated symptoms (e.g., nausea, vomiting, dizziness) of balance problems is essential. We must consider past medical history and any family history of balance disorders.
- Physical Examination: This involves assessing gait, posture, coordination, and muscle tone. We look for asymmetries and abnormal movements. Cranial nerve examination is also important to assess vestibular function.
- Clinical Tests: We perform age-appropriate balance tests, including:
- Romberg test: Assesses static balance.
- Balance beam walking: Assesses dynamic balance.
- Clinical examination of vestibulo-ocular reflexes (VOR) : To see how the eyes react to head movements.
- Specialized Testing (when indicated): This might include:
- Posturography: Measures balance using a computerized platform.
- Videonystagmography (VNG): Records eye movements to assess vestibular function.
- Rotary chair testing: Assesses the responses of the vestibular system to rotational movements.
The specific tests selected will depend on the child’s age, cooperation level, and the suspected diagnosis.
Q 18. What are the different types of pediatric vestibular disorders?
Pediatric vestibular disorders encompass a broad range of conditions affecting the balance system. These can be broadly categorized as:
- Peripheral vestibular disorders: These involve problems within the inner ear itself, such as:
- Benign paroxysmal positional vertigo (BPPV): Caused by displaced calcium carbonate crystals in the inner ear.
- Vestibular neuritis/labyrinthitis: Inflammation of the vestibular nerve or inner ear.
- Ménière’s disease (rare in children): Characterized by episodes of vertigo, tinnitus, and hearing loss.
- Central vestibular disorders: These involve problems within the brain’s vestibular pathways or processing centers, such as:
- Brainstem lesions: These can disrupt vestibular signals, leading to balance problems.
- Cerebellar disorders: The cerebellum plays a crucial role in coordination and balance, so damage can impair these functions.
- Migraine-associated vertigo: Vertigo can be a symptom of migraine headaches.
- Vestibular developmental delay: A group of developmental conditions affecting the balance system.
The exact cause and specific presentation of the vestibular disorder varies widely depending on the underlying pathology.
Q 19. Describe the management of benign paroxysmal positional vertigo (BPPV) in children.
Managing BPPV in children often involves the same techniques used in adults, but the approach needs to be adapted to the child’s age and understanding. The cornerstone of treatment is the Epley maneuver, a series of head repositioning techniques designed to move the displaced crystals out of the semicircular canals.
The Epley maneuver should ideally be performed by a qualified professional who can tailor the technique to the child’s needs. It may need to be performed in several sessions, especially for younger or less cooperative children.
Alternative techniques and approaches may include Brandt-Daroff exercises or other head position strategies that are easier to perform for a child. These exercises, though less effective in some cases, can be safer and more practical when the Epley maneuver proves difficult.
Patient and parental education is critical. Parents need to understand the condition, the treatment rationale, and how to assist their child with the exercises. Reassurance and a positive approach are paramount. Regular follow-up appointments are needed to assess the effectiveness of the treatment and make adjustments as necessary.
Q 20. What are the potential neurological causes of hearing loss in children?
Several neurological conditions can lead to hearing loss in children. These conditions affect the auditory pathways, from the inner ear to the brain’s auditory cortex.
- Meningitis: Infection of the membranes surrounding the brain and spinal cord can damage the auditory nerve or inner ear structures.
- Encephalitis: Inflammation of the brain can also affect auditory pathways.
- Neurofibromatosis type 2 (NF2): This genetic disorder affects the development of tumors on the vestibular and auditory nerves, leading to hearing loss and balance problems.
- Perinatal asphyxia: Oxygen deprivation during birth can cause damage to the auditory system.
- Brain tumors: Tumors located near the auditory pathways can compress and damage them, causing hearing loss.
- Genetic syndromes: Many genetic syndromes, such as Usher syndrome and Waardenburg syndrome, are associated with sensorineural hearing loss and often other neurological manifestations.
The specific neurological cause of hearing loss needs to be diagnosed and addressed on a case-by-case basis. Neuroimaging (MRI, CT) might be necessary to assess the underlying condition, and close collaboration with neurologists and other specialists might be needed.
Q 21. How would you interpret an audiogram in a child?
Interpreting a child’s audiogram requires careful consideration of their age, developmental level, and behavioral responses during the test. It’s not simply a matter of reading the numbers; it involves understanding the context.
An audiogram displays hearing thresholds in different frequencies. A normal audiogram shows thresholds within the normal hearing range (generally 0-20 dB HL). Different patterns of hearing loss can be identified.
- Conductive hearing loss: Indicates a problem with sound transmission to the inner ear (e.g., middle ear infection). Air conduction thresholds are affected, but bone conduction thresholds remain normal.
- Sensorineural hearing loss: Indicates a problem with the inner ear or auditory nerve. Both air conduction and bone conduction thresholds are affected.
- Mixed hearing loss: A combination of conductive and sensorineural hearing loss.
For younger children, we may rely on auditory brainstem response (ABR) or otoacoustic emissions (OAE) tests that assess the hearing system’s response to sound. The audiogram results should be correlated with the child’s behavioral observations and history.
For instance, a child with a sloping sensorineural hearing loss might show difficulty understanding speech in noisy environments, while a child with mild conductive loss might primarily have issues understanding low-pitched sounds.
A thorough interpretation should consider the entire picture and inform appropriate management strategies – including the selection of hearing aids, early intervention services, and ongoing monitoring.
Q 22. Describe the differences between conductive, sensorineural, and mixed hearing loss.
Hearing loss is categorized into three main types: conductive, sensorineural, and mixed. Understanding the difference lies in where the problem occurs within the hearing pathway.
- Conductive hearing loss: This occurs when sound waves have difficulty traveling from the outer ear to the inner ear. Think of it like a blockage in a tunnel – sound can’t reach its destination. Common causes in children include ear infections (otitis media), fluid buildup behind the eardrum, and abnormalities in the outer or middle ear structures. For example, a child with impacted earwax would experience conductive hearing loss.
- Sensorineural hearing loss: This type involves damage to the inner ear (cochlea) or the auditory nerve. This is like damage to the receiver or the wires connecting the receiver to the brain. Causes can range from genetic conditions, noise exposure (though less common in young children), certain infections like meningitis, and even some medications. A child born with a genetic abnormality affecting the cochlea would have sensorineural hearing loss.
- Mixed hearing loss: As the name suggests, this is a combination of both conductive and sensorineural hearing loss. A child might have fluid in their middle ear (conductive) *and* damage to the hair cells in their inner ear (sensorineural) due to a viral infection, for example.
Accurate diagnosis requires a thorough audiological evaluation including pure-tone audiometry and tympanometry to pinpoint the location and degree of the hearing loss.
Q 23. Discuss your experience with different types of hearing aids.
My experience encompasses a wide range of hearing aid technologies for pediatric patients. The choice of hearing aid depends heavily on the child’s age, hearing loss severity, and overall developmental stage. I frequently work with:
- Behind-the-ear (BTE) hearing aids: These are commonly used in children, particularly younger ones, because they are robust and can accommodate a wide range of hearing losses. They’re also often easier to maintain and repair.
- In-the-ear (ITE) hearing aids: These are custom-fitted to the child’s ear and are a good option for mild to moderate hearing loss. However, they may not be as durable as BTEs and require more careful handling.
- In-the-canal (ITC) and Completely-in-canal (CIC) hearing aids: These are less common in pediatrics due to their smaller size, which makes them more prone to damage and loss, and often harder for a child to manipulate.
- Bone-anchored hearing aids (BAHAs): These are used in specific cases, such as children with conductive hearing loss that doesn’t respond well to traditional hearing aids or those with atresia (absence of the external ear canal).
Beyond the type, I consider factors like the hearing aid’s features (e.g., directional microphones, noise reduction technology, wireless connectivity), its fit and comfort, and the family’s ability to manage and maintain the device. Patient and family education is crucial for successful hearing aid use.
Q 24. What are the latest advancements in pediatric audiology?
Pediatric audiology is a rapidly evolving field. Some of the most significant advancements include:
- Improved hearing aid technology: Smaller, more powerful, and smarter hearing aids are becoming more readily available, offering better sound quality and more advanced features such as automatic noise reduction and Bluetooth connectivity. This is particularly beneficial for children who need to integrate their hearing aids with classroom technologies.
- Advances in cochlear implant technology: Newer implants have improved speech processing strategies, resulting in better hearing outcomes. Implantable middle ear devices offer another option for sensorineural or mixed hearing loss.
- Early identification and intervention programs: Universal newborn hearing screening has significantly increased the early detection of hearing loss, leading to earlier intervention and improved developmental outcomes. These programs are coupled with improved diagnostic tools that allow more precise characterization of auditory deficits.
- Genetic testing for hearing loss: This allows for earlier diagnosis of genetic conditions causing hearing loss, which is crucial for both medical management and genetic counseling.
- Objective measures of auditory function: New technologies allow for more objective assessment of auditory processing disorders, which can help tailor interventions effectively.
These advancements are improving outcomes and providing children with better access to hearing and communication support.
Q 25. Explain your experience with tympanostomy tube placement.
Tympanostomy tube placement is a common procedure I perform for children with recurrent otitis media with effusion (fluid behind the eardrum). This procedure involves creating a small incision in the eardrum and inserting a tiny tube that allows for ventilation and drainage of fluid. My experience involves:
- Pre-operative assessment: This includes a thorough review of the child’s medical history, a complete hearing evaluation, and assessing the overall health of the child.
- Surgical procedure: I perform the procedure under general anesthesia, using microsurgical techniques to minimize trauma. The size and type of tube are chosen based on the child’s age and anatomy.
- Post-operative care: This includes monitoring for complications (e.g., bleeding, infection), providing pain management, and advising parents on ear care and potential follow-up appointments. I also emphasize the importance of preventing further ear infections.
Careful patient selection is critical to optimize the success rate of the surgery. Not all children with recurrent ear infections require tubes. We consider the frequency, duration, and impact of the infections on hearing and speech development before recommending surgery.
Q 26. How do you evaluate and manage a child with recurrent ear infections?
Recurrent ear infections in children are a significant concern. My approach involves a multi-faceted strategy:
- Detailed history and examination: This includes inquiring about the frequency, duration, and severity of infections, as well as any associated symptoms like fever or hearing loss. I perform a thorough otoscopic examination to assess the ear canal and eardrum.
- Hearing evaluation: This is essential to determine the impact of the infections on hearing, particularly if there is fluid behind the eardrum.
- Treatment plan: This can range from watchful waiting for mild cases to antibiotics for acute infections. If there’s persistent fluid buildup despite medical management, tympanostomy tubes might be considered.
- Preventive measures: I strongly emphasize preventive strategies such as avoiding secondhand smoke, promoting proper breastfeeding techniques, and ensuring adequate ventilation in the home. Sometimes, allergy testing is done to rule out allergies as a contributing factor.
Close monitoring and follow-up are essential to ensure that the infections are effectively treated and to identify any potential long-term hearing implications.
Q 27. Discuss your approach to a child presenting with sudden sensorineural hearing loss.
Sudden sensorineural hearing loss (SSNHL) in children is a medical emergency requiring prompt attention. My approach is focused on rapid diagnosis and treatment to preserve hearing.
- Immediate audiological evaluation: This is crucial to determine the extent and nature of the hearing loss. Detailed audiograms are performed and compared to any previous data.
- Medical investigations: SSNHL necessitates a comprehensive medical workup to identify the underlying cause. This may include blood tests, imaging studies (MRI), and consultations with other specialists.
- Treatment: Treatment focuses on minimizing further damage to the inner ear. This commonly involves high-dose corticosteroids, either orally or intravenously. The treatment course and response are carefully monitored.
- Referral and support: Depending on the cause and severity, referral to other specialists such as neurologists or infectious disease specialists may be necessary. Support for the family is paramount, including emotional support and counseling.
The prognosis for SSNHL can vary, and early intervention is key to maximizing the chances of hearing recovery. Rehabilitation measures, such as hearing aids or speech therapy, might be needed depending on the outcome.
Q 28. How would you counsel a family about genetic testing for hearing loss?
Genetic testing for hearing loss is becoming increasingly important, especially in children with unknown causes of hearing impairment or a family history of hearing problems. My approach to counseling families involves:
- Explaining the purpose and benefits: I explain that genetic testing can identify the specific gene mutation responsible for the hearing loss, helping to understand the cause and predict the prognosis, and enabling better management and potentially preventing hearing loss in future generations.
- Discussing the limitations: I clearly outline the limitations of genetic testing, such as the fact that not all genes causing hearing loss are currently identifiable. I also discuss the possibility of inconclusive results.
- Exploring potential implications: I address the potential emotional and psychological impact of the results on the family, including the possibility of a severe genetic condition. We offer resources for genetic counseling and support.
- Informed consent: I obtain informed consent from the parents, ensuring they fully understand the procedure, benefits, risks, and alternatives.
- Result interpretation and follow-up: Following the genetic testing, we provide a comprehensive explanation of the results, discussing their implications and providing guidance on management and future planning.
A collaborative approach with genetic counselors is important to provide the family with thorough support and guidance during this process.
Key Topics to Learn for Pediatric Neuro-Otology Interview
- Developmental Auditory Neuroscience: Understanding the maturation of the auditory system in children, including typical and atypical development. Consider the implications for diagnosis and intervention.
- Common Pediatric Hearing Disorders: Deepen your knowledge of congenital hearing loss, auditory neuropathy spectrum disorder, and other common conditions. Be prepared to discuss diagnostic approaches and management strategies.
- Vestibular System Development and Disorders: Explore the development of balance and spatial orientation in children. Familiarize yourself with common vestibular disorders like benign paroxysmal positional vertigo (BPPV) in children and their unique presentation.
- Neurological Conditions Affecting Hearing and Balance: Review conditions like cerebral palsy, autism spectrum disorder, and other neurological conditions that frequently impact the auditory and vestibular systems. Understand the challenges in diagnosis and management within these populations.
- Diagnostic Testing and Interpretation: Master the interpretation of audiological tests (ABR, OAE, etc.) in the pediatric population. Understand the limitations and strengths of various diagnostic tools in relation to developmental considerations.
- Surgical and Non-Surgical Management Options: Be familiar with both medical and surgical interventions for pediatric neuro-otological conditions, including hearing aids, cochlear implants, and vestibular rehabilitation therapies. Be prepared to discuss the indications and contraindications for each.
- Ethical and Legal Considerations: Consider the ethical implications of diagnosis and treatment decisions in the pediatric setting, including informed consent and family involvement.
- Research and Current Trends: Stay updated on the latest research and advancements in pediatric neuro-otology. This demonstrates your commitment to the field and your ongoing professional development.
Next Steps
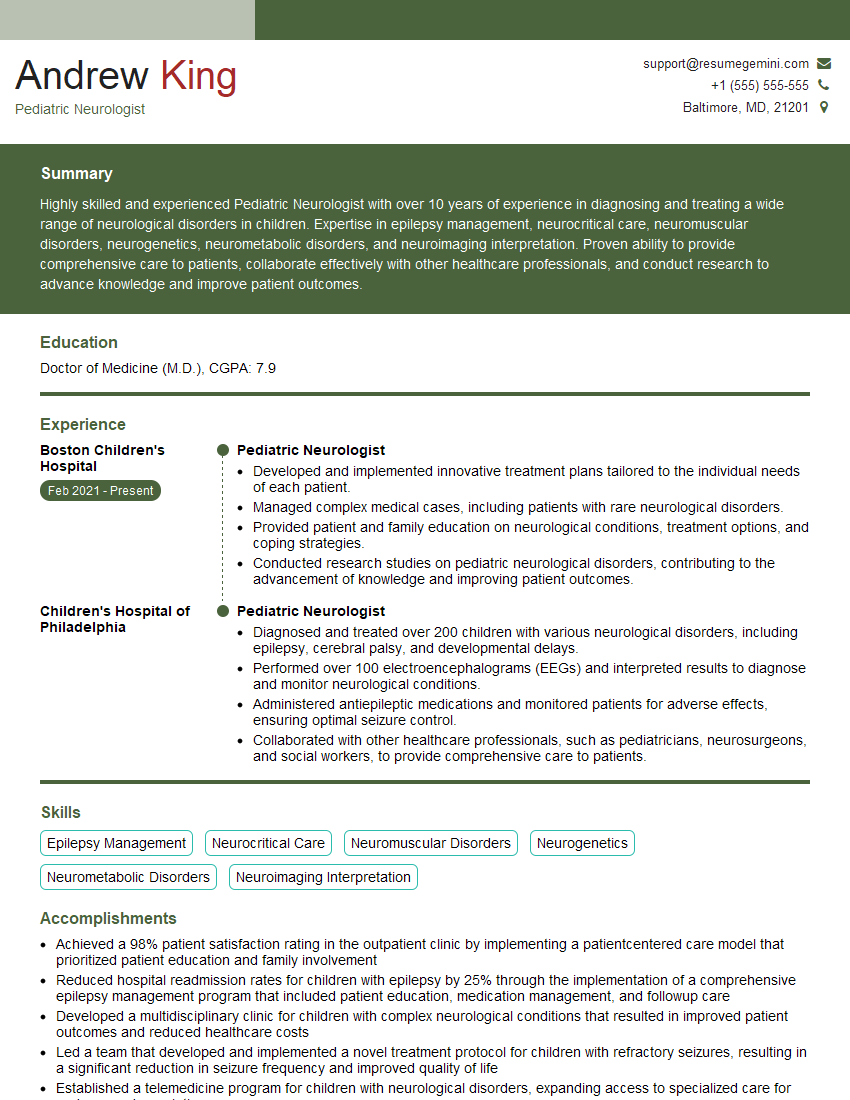
Mastering Pediatric Neuro-Otology is crucial for a successful and rewarding career. A strong foundation in this specialized area opens doors to challenging and fulfilling opportunities within academic institutions, research settings, and private practices. To enhance your job prospects, it’s vital to create a compelling and ATS-friendly resume that highlights your skills and experience effectively. ResumeGemini is a trusted resource that can help you build a professional resume designed to impress potential employers. Examples of resumes tailored to Pediatric Neuro-Otology are available to help guide you. Take the next step in your career journey and build a resume that showcases your expertise!
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
To the interviewgemini.com Webmaster.
Very helpful and content specific questions to help prepare me for my interview!
Thank you
To the interviewgemini.com Webmaster.
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.