Unlock your full potential by mastering the most common Ability to conduct comprehensive neuropsychological evaluations interview questions. This blog offers a deep dive into the critical topics, ensuring you’re not only prepared to answer but to excel. With these insights, you’ll approach your interview with clarity and confidence.
Questions Asked in Ability to conduct comprehensive neuropsychological evaluations Interview
Q 1. Describe the process of administering a comprehensive neuropsychological battery.
Administering a comprehensive neuropsychological battery is a meticulous process requiring a deep understanding of neuroanatomy, cognitive function, and psychometrics. It begins with a thorough case history review, gathering information about the individual’s medical, social, educational, and occupational history. This helps shape the specific tests selected. The evaluation itself usually spans several hours, sometimes across multiple sessions, and is tailored to the individual’s suspected deficits and referral question.
The process involves administering a series of tests, encompassing domains like attention, memory, executive functions, language, visuospatial skills, and motor skills. Examples include the Wechsler Adult Intelligence Scale (WAIS), Wechsler Memory Scale (WMS), Trail Making Test, Wisconsin Card Sorting Test, and Boston Naming Test. After the testing is complete, I carefully score the tests, analyzing the raw scores, considering the individual’s demographic characteristics (like age and education), and generating normative-based comparisons (percentile ranks, standard scores).
Finally, the interpretation involves synthesizing the test results with the case history information to generate a comprehensive neuropsychological report. This report includes a description of the cognitive strengths and weaknesses, potential underlying neurological or psychological factors contributing to the observed deficits, and recommendations for further assessment, treatment, or rehabilitation. For example, if someone exhibits significant memory impairments on the WMS, coupled with a history of head trauma, I might suggest further neuroimaging.
Q 2. What are the key differences between standardized and non-standardized neuropsychological tests?
The key difference between standardized and non-standardized neuropsychological tests lies in their administration and scoring procedures. Standardized tests are meticulously developed with established norms, precise administration protocols, and specific scoring criteria. This ensures consistency and allows for comparisons across individuals. Think of it like a recipe—you follow the steps exactly to get a reliable outcome. Examples include the WAIS and WMS.
Non-standardized tests, on the other hand, lack formal norms, consistent administration protocols, and standardized scoring. They often are more flexible and tailored to the specific needs of the individual. This flexibility is beneficial for exploring particular cognitive processes in more detail but makes comparisons to other individuals more challenging. They’re more like a chef’s improvisation, creatively adapting the dish based on available ingredients and the palate of the diner.
For example, a simple request to describe the events of the previous day is a non-standardized measure of recent memory, while the Logical Memory subtest of the WMS is standardized, meaning its administration, scoring, and interpretation are firmly established.
Q 3. Explain the importance of rapport-building in neuropsychological evaluations.
Rapport-building is absolutely crucial in neuropsychological evaluations. Neuropsychological testing can be lengthy and demanding, requiring patients to perform complex cognitive tasks. A strong rapport helps reduce anxiety, enhance cooperation, and ensure the patient gives their best effort. Think of it as setting the stage for a successful performance. A relaxed and trusting environment fosters more accurate and reliable results.
I achieve this through active listening, empathetic communication, and a genuine interest in the patient’s story and experience. I clearly explain the purpose of each test, emphasizing its importance in understanding their cognitive abilities and addressing their concerns. Humor, when appropriate, and adapting the testing pace to the patient’s comfort level also contribute to building a collaborative atmosphere. In a recent evaluation, a patient was initially hesitant and apprehensive; however, after I spent time discussing their hobbies and building a connection, their performance improved considerably, providing a more accurate reflection of their cognitive abilities.
Q 4. How do you interpret results from the Wechsler Adult Intelligence Scale (WAIS)?
The Wechsler Adult Intelligence Scale (WAIS) provides a comprehensive assessment of intellectual abilities. Interpretation involves looking at both the Full Scale IQ (FSIQ), which provides an overall measure of intelligence, and the index scores (Verbal Comprehension, Perceptual Reasoning, Working Memory, Processing Speed). The index scores reveal specific cognitive strengths and weaknesses. A lower score in a particular index might indicate a specific cognitive impairment. For example, a lower Processing Speed score might suggest difficulties with attention or executive functions.
I also analyze the individual subtest scores. A pattern of subtest scores can reveal valuable information beyond the index scores. For instance, poor performance on the Digit Span subtest (working memory) might highlight attentional deficits. Furthermore, comparing the patient’s scores to the normative data—considering age and education—is essential for a meaningful interpretation. The results are not interpreted in isolation but within the context of the individual’s history, medical status, and the other test results.
Q 5. How do you interpret results from the Wechsler Memory Scale (WMS)?
The Wechsler Memory Scale (WMS) evaluates various aspects of memory, including immediate, delayed, and visual memory. Similar to the WAIS, interpretation begins by looking at the index scores (Auditory Memory, Visual Memory, Visual Working Memory, Immediate Memory, Delayed Memory). These scores provide a broad overview of different memory systems.
Just like with the WAIS, the individual subtest scores provide more detailed information. For example, a poor performance on the Logical Memory subtest (verbal memory) may indicate difficulty with encoding and retrieval of verbal information. I examine the discrepancy between immediate and delayed recall to assess consolidation, the process of transferring information from short-term to long-term memory. The WMS also includes recognition tasks that help differentiate between encoding and retrieval problems.
Again, the interpretation isn’t solely based on the raw scores. It involves a synthesis of the scores with the patient’s history and other test results. A pattern of impaired visual memory, for example, combined with a history of visual neglect, can provide crucial insights into the underlying pathology.
Q 6. How do you handle conflicting results from different neuropsychological tests?
Conflicting results between neuropsychological tests are not uncommon. They often highlight the complexity of the brain and the limitations of any single test. I approach these situations systematically. First, I rigorously review the administration and scoring procedures of each test to identify any potential errors. I then consider the test characteristics: some tests are more sensitive to certain types of cognitive deficits than others. For example, a test emphasizing speed might be more impacted by fatigue than a test relying on accuracy.
Next, I examine the pattern of strengths and weaknesses across the entire battery. Sometimes a single test result might be an outlier, not reflecting the overall cognitive profile. I also integrate information from the patient’s history, clinical observation, and other sources, such as collateral information from family members or previous medical records. This allows for a more nuanced interpretation of the findings.
For instance, if one test suggests significant memory problems, but other tests of memory and executive functions are within normal limits, this might point toward a specific memory impairment rather than a generalized cognitive decline. A careful consideration of all available data, instead of focusing on isolated findings, is crucial for generating a valid and reliable interpretation.
Q 7. Describe your experience with different types of memory assessments.
My experience with memory assessments is extensive, covering a broad range of methodologies. This includes standardized tests like the WMS, California Verbal Learning Test (CVLT), and Rey Auditory Verbal Learning Test (RAVLT), which allow for objective comparison to normative data. I’m also experienced with non-standardized assessments such as those involving autobiographical memory, face-name association tests, and narrative recall tasks which provide deeper insights into the nature of memory deficits and their impact on daily life.
Furthermore, I utilize various approaches to assess different types of memory, including verbal and visual memory (e.g., word lists versus complex figures), immediate and delayed recall (assessing short-term versus long-term storage), recognition and free recall (differentiating between encoding and retrieval difficulties), and prospective memory (the ability to remember to perform future actions). The choice of assessment method depends on the clinical question, the patient’s condition, and the available time. For example, I may use a narrative recall task for assessing semantic memory and the ability to connect events chronologically.
In addition to direct memory assessment, I also consider indirect measures like those that evaluate attention and executive functions, as these cognitive domains significantly affect memory performance. This holistic approach provides a comprehensive understanding of an individual’s memory functioning, assisting in accurate diagnosis and effective treatment planning.
Q 8. What are some common cognitive impairments you assess?
Neuropsychological evaluations assess a wide range of cognitive functions. Common impairments I assess include:
- Memory: This encompasses various memory systems, including short-term memory (remembering a phone number briefly), long-term memory (recalling childhood events), working memory (manipulating information in mind), and episodic memory (remembering specific events).
- Attention: This includes sustained attention (maintaining focus over time), selective attention (filtering distractions), divided attention (multitasking), and alternating attention (switching between tasks).
- Executive Functions: These higher-order cognitive processes govern planning, problem-solving, decision-making, inhibitory control (resisting impulses), and cognitive flexibility (adapting to changing demands). Examples include the Tower of London test and the Wisconsin Card Sorting Test.
- Language: Assessment covers verbal fluency (generating words within a category), comprehension (understanding spoken and written language), naming (retrieving word labels for objects), and repetition.
- Visuospatial Skills: These involve perceiving, processing, and manipulating visual information, including visual construction (copying complex designs), visual perception (identifying objects), and spatial reasoning.
- Processing Speed: This refers to the speed at which an individual can process and respond to information, often measured through simple reaction time tasks.
The specific cognitive domains assessed depend on the individual’s presenting concerns and referral questions.
Q 9. How do you differentiate between cognitive deficits due to neurological vs. psychiatric conditions?
Differentiating between cognitive deficits stemming from neurological versus psychiatric conditions requires a thorough evaluation incorporating multiple data sources. Neurological conditions, such as stroke or TBI, often present with focal cognitive deficits – that is, impairments affecting specific cognitive domains based on the location of brain damage. For example, damage to the hippocampus may predominantly affect memory. In contrast, psychiatric conditions, like depression or schizophrenia, may present with more diffuse cognitive impairments affecting multiple domains, albeit often less severe than in neurological conditions.
Furthermore, neurological conditions often exhibit objective evidence of brain dysfunction (e.g., abnormal neurological examination findings, neuroimaging abnormalities), which is usually absent in primary psychiatric conditions. However, it’s crucial to remember that comorbidity is common. For example, someone with depression can also experience a stroke, leading to a complex presentation requiring careful clinical judgment.
The assessment process relies heavily on detailed history, neuropsychological testing, and, when appropriate, neuroimaging studies (like MRI or CT scans) to determine the underlying cause of cognitive impairment. I also consider the pattern of cognitive strengths and weaknesses, the course of the cognitive difficulties, and the presence of other symptoms to arrive at a comprehensive diagnosis.
Q 10. Describe your experience with individuals with traumatic brain injury (TBI).
My experience with individuals with traumatic brain injury (TBI) is extensive. I’ve worked with patients across the spectrum of severity, from mild concussions to severe TBI resulting in prolonged coma. The presentation is incredibly variable, depending on the location and severity of the injury.
In my assessments, I focus on identifying the specific cognitive and behavioral deficits resulting from the TBI. This includes evaluating attention, memory, executive functions, and processing speed, often using standardized neuropsychological tests tailored to the patient’s functional level. I also assess for emotional and behavioral changes, such as irritability, impulsivity, or apathy, which are common sequelae of TBI.
One case that stands out involved a young adult who sustained a moderate TBI in a car accident. Initially, he presented with significant impairments in attention and memory, impacting his ability to return to college. Through targeted neuropsychological rehabilitation and therapy, we were able to significantly improve his cognitive skills, enabling him to successfully re-enroll and graduate.
Q 11. Describe your experience with individuals with stroke.
My work with stroke patients often involves assessing cognitive deficits related to the affected brain regions. A stroke in the left hemisphere, for example, may result in language problems (aphasia) and right-sided weakness, while a right hemisphere stroke can impact visuospatial skills, attention, and neglect of the left side of the body. The assessment process aims to pinpoint these specific deficits and determine their impact on daily functioning.
I utilize standardized neuropsychological tests sensitive to stroke-related impairments, carefully selecting measures based on the patient’s presenting symptoms and the suspected location of the brain lesion (information often obtained from neuroimaging). The ultimate goal is to help patients and their families understand the nature and extent of the cognitive impairments, to facilitate rehabilitation planning, and to provide guidance on adaptive strategies for managing difficulties in daily life.
One memorable case involved a patient who suffered a stroke affecting the left parietal lobe. This resulted in significant visuospatial difficulties, impacting their ability to dress, read maps, and even navigate their own home. Through intensive rehabilitation, including occupational therapy, we made significant progress in restoring their functional abilities.
Q 12. Describe your experience with individuals with dementia.
My experience with individuals with dementia is extensive, encompassing various types, including Alzheimer’s disease, vascular dementia, frontotemporal dementia, and Lewy body dementia. Each type exhibits a distinct pattern of cognitive and behavioral changes, which informs the assessment approach.
In assessing individuals with dementia, I use a combination of neuropsychological tests sensitive to different aspects of cognitive decline, along with informant interviews to gather historical information and contextualize the patient’s current functioning. I pay close attention to the progression of symptoms, the presence of behavioral changes such as agitation or apathy, and the impact on daily activities. The goal is not just to diagnose the type of dementia but also to stage the severity of cognitive decline and evaluate the patient’s functional capacity, which informs care planning.
For example, I recently evaluated a patient experiencing increasing memory difficulties, impacting their independent living skills. Through the assessment, we were able to diagnose early-stage Alzheimer’s disease and implement strategies to help maximize their independence and quality of life, involving their family in the process.
Q 13. How do you adapt your evaluation approach for patients with different communication abilities?
Adapting my evaluation approach for patients with varying communication abilities is paramount. I employ several strategies, including:
- Modified Test Administration: For individuals with aphasia (language impairment) or other communication difficulties, I modify test instructions, allow more response time, and use alternative response methods (e.g., pointing, gestures) as needed. I may also choose tests that are less verbally demanding.
- Use of Alternative Assessment Tools: I utilize nonverbal tests that rely less on language skills, such as visual-spatial tasks or performance-based assessments. Observation of the patient’s behavior during the assessment provides valuable supplemental information.
- Incorporating Informant Reports: I rely heavily on information from caregivers or family members to obtain a comprehensive understanding of the patient’s cognitive functioning and history, especially when direct patient communication is limited.
- Collaboration with Other Professionals: I collaborate with speech-language pathologists and occupational therapists to gather complementary information and leverage their expertise in communication and functional abilities.
The key is flexibility and creativity in tailoring the assessment process to the individual’s unique needs and limitations, ensuring a fair and comprehensive evaluation.
Q 14. Explain your understanding of malingering and how you address it in your assessments.
Malingering, the intentional feigning of symptoms, is a significant concern in neuropsychological evaluations. It can significantly impact the accuracy and validity of the assessment. I address this through a multifaceted approach:
- Careful Review of History: Inconsistencies between the reported symptoms, the patient’s history, and collateral information (from family or other sources) raise suspicion.
- Use of Validity Measures: I incorporate standardized validity tests specifically designed to detect exaggerated or fabricated symptoms. These tests assess response patterns and consistency across different tasks, which can reveal inconsistencies suggestive of malingering. Examples include the Test of Memory Malingering (TOMM) and the Rey 15-Item Test.
- Observational Data: I meticulously observe the patient’s behavior and performance throughout the assessment, looking for inconsistencies or unusual patterns that might indicate intentional symptom exaggeration.
- Comparison with Baseline Data: If prior neuropsychological data are available, comparing current performance to past assessments can help identify significant discrepancies suggestive of malingering.
- Integration of Multiple Data Sources: A comprehensive approach integrates data from neuropsychological tests, history, observation, and collateral information to paint a complete picture. Rarely will a single indicator definitively confirm or rule out malingering.
It’s crucial to approach the issue of malingering with sensitivity and professionalism. While it’s important to identify potential malingering, it’s equally important to consider potential alternative explanations for unusual test performance, such as underlying cognitive or emotional distress.
Q 15. How do you ensure the cultural fairness of neuropsychological assessments?
Ensuring cultural fairness in neuropsychological assessments is paramount to obtain accurate and unbiased results. It’s not simply about translating tests; it’s about understanding how cultural background can influence performance. This involves several key strategies:
- Test Selection: Choosing tests with established norms representing diverse populations, or using tests less reliant on cultural knowledge. For example, using nonverbal tests or those with minimal verbal instructions reduces bias against individuals with limited language proficiency.
- Test Administration: Adapting the administration style to the individual’s communication preferences and comfort level. This might include adjusting the pace of testing, providing clear and concise instructions, and being sensitive to nonverbal cues suggesting discomfort or confusion. Building rapport is crucial, especially with patients from different cultural backgrounds.
- Interpretation of Results: Recognizing that performance can be affected by factors beyond cognitive ability, such as acculturation level, education, and exposure to similar test formats. We must carefully consider these factors when interpreting scores and avoid making generalizations based solely on test performance. For instance, a lower score on a culturally loaded test doesn’t automatically indicate cognitive impairment; it may simply reflect unfamiliarity with the test materials.
- Using Interpretive Frameworks: Employing interpretive frameworks that account for cultural influences, such as considering the patient’s sociocultural history and experiences during the evaluation process and report writing.
For example, I once worked with a refugee who scored lower than expected on a verbal fluency task. Initially, this might suggest language difficulties or cognitive deficits. However, understanding their traumatic experiences and limited formal education allowed me to interpret this result more accurately, highlighting the impact of their life experiences on performance rather than solely focusing on the test scores.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What are your strategies for managing challenging or emotionally distressed patients during testing?
Managing emotionally distressed or challenging patients during testing requires patience, empathy, and a flexible approach. My strategies focus on building rapport and creating a safe and comfortable testing environment. This involves:
- Establishing rapport: Beginning with a warm and welcoming introduction, taking the time to understand their concerns, and addressing any anxieties they might have about the testing process. A calm and reassuring demeanor is crucial.
- Providing clear and concise explanations: Explaining the purpose and procedures of each test in simple, easy-to-understand language. I adjust my communication style based on the patient’s cognitive abilities and emotional state.
- Offering breaks when needed: Recognizing that lengthy testing can be overwhelming, especially for patients who are already experiencing distress. I incorporate frequent breaks to allow patients to rest, collect themselves, and resume the assessment feeling more comfortable.
- Using flexible testing approaches: Adapting the testing procedures to accommodate the patient’s needs. This might involve shortening testing sessions, changing the order of tests, or modifying the instructions as needed.
- Collaborating with other professionals: In cases of severe distress or challenging behaviors, consulting with psychiatrists, psychologists, or other healthcare professionals may be necessary to manage the situation effectively and ensure the patient’s well-being.
For instance, I once assessed a patient with significant anxiety related to memory testing. By using a conversational approach, incorporating breaks, and focusing on their strengths, I was able to build trust and complete the assessment successfully. The rapport created allowed for accurate results and a more positive experience.
Q 17. Discuss your experience with interpreting neuroimaging data in conjunction with neuropsychological findings.
Integrating neuroimaging data (such as fMRI, MRI, or CT scans) with neuropsychological findings is crucial for a comprehensive understanding of brain-behavior relationships. It allows for a more nuanced interpretation of cognitive deficits and provides a stronger basis for diagnosis and treatment planning. My experience involves:
- Correlating structural and functional abnormalities with cognitive performance: For example, observing atrophy in the hippocampus on an MRI scan can be correlated with memory impairments on neuropsychological tests. This provides objective evidence supporting subjective findings.
- Identifying patterns of brain damage: Neuroimaging helps pinpoint the location and extent of brain lesions, which can inform the type and severity of cognitive deficits observed. This allows for more precise predictions regarding recovery potential.
- Differentiating between various neurological and psychiatric conditions: Neuroimaging can help differentiate between conditions that may present with similar cognitive symptoms. For example, distinguishing between Alzheimer’s disease and frontotemporal dementia based on characteristic patterns of atrophy visible on MRI.
- Monitoring treatment response: Neuropsychological assessments combined with neuroimaging can track the effectiveness of interventions such as medication or rehabilitation programs by monitoring changes in cognitive function and correlating those with changes in brain structure or function over time.
In one case, a patient presented with memory difficulties. Neuropsychological testing revealed significant impairments, and an MRI scan showed hippocampal atrophy consistent with early-stage Alzheimer’s disease. This integrated approach allowed for an accurate diagnosis and facilitated early intervention.
Q 18. How do you write a comprehensive and clinically relevant neuropsychological report?
Writing a comprehensive and clinically relevant neuropsychological report requires a structured approach to ensure clarity, accuracy, and clinical utility. My reports typically include:
- Identifying information: Patient demographics, referral source, and reason for referral.
- Background information: Relevant medical, social, and developmental history, including premorbid cognitive functioning (level of function before the onset of any illness or injury).
- Behavioral observations: Detailed observations of the patient’s behavior, mood, and cooperation during the assessment.
- Test results: A detailed description of the neuropsychological tests administered, including scores, percentile ranks, and interpretations. I avoid using solely raw scores, preferring to contextualize these within normative data for age and education.
- Cognitive profile summary: A concise summary of the patient’s overall cognitive strengths and weaknesses.
- Diagnostic impressions: Potential diagnoses based on the neuropsychological findings, along with differential diagnoses and considerations.
- Recommendations: Specific recommendations for treatment, rehabilitation, or further assessment.
- Limitations: An acknowledgement of any limitations to the interpretation of results, such as the impact of medications, patient effort, or incomplete data.
The report is written in clear, concise language, avoiding jargon where possible and ensuring that the findings are easily understood by the referring physician and other healthcare professionals. I always prioritize clarity and clinical relevance, avoiding overly technical language.
Q 19. How do you maintain confidentiality and adhere to ethical standards in neuropsychological practice?
Maintaining confidentiality and adhering to ethical standards are fundamental to my neuropsychological practice. This involves:
- Strict adherence to HIPAA regulations: Protecting patient information by using secure storage methods, limiting access to authorized personnel only, and following all mandated procedures for handling protected health information (PHI).
- Informed consent: Obtaining informed consent from patients before initiating any assessment, ensuring they understand the purpose, procedures, and potential risks and benefits of the evaluation. This also includes clarifying how the information will be used and stored.
- Maintaining professional boundaries: Avoiding dual relationships and maintaining appropriate professional boundaries with patients. This means refraining from personal relationships and conflicts of interest.
- Accuracy and objectivity: Ensuring that my assessments are conducted and interpreted in a fair, objective, and unbiased manner. This involves acknowledging personal biases and potential limitations in interpretations.
- Appropriate use of technology: Utilizing secure electronic health records (EHRs) and other technologies in compliance with HIPAA and other relevant regulations. Ensuring data encryption and password protection for sensitive information.
- Consulting with colleagues when needed: Seeking consultation with other qualified professionals when faced with ethical dilemmas or challenging situations.
Maintaining confidentiality and ethical standards is not just a policy but a fundamental commitment to responsible patient care. I always prioritize patient well-being and uphold the highest ethical standards in my practice.
Q 20. Describe your familiarity with different neuropsychological software and databases.
My familiarity with neuropsychological software and databases is extensive. I’m proficient in using several commonly used software programs such as:
- Test administration and scoring software: Such as programs that administer and score standardized neuropsychological tests, providing immediate feedback on performance and generating reports.
- Statistical software packages: Such as SPSS or R, for conducting advanced statistical analyses, including correlational analyses, regression analyses, and other statistical tests.
- Neuropsychological databases: I have experience using databases containing normative data for various neuropsychological tests, enabling me to accurately compare individual patient performance to age- and education-matched norms.
- Electronic Health Record (EHR) systems: I am comfortable using different EHR systems to access patient records, document assessment findings, and generate reports electronically.
This technological proficiency enables me to conduct assessments efficiently, analyze data effectively, and generate clear and concise reports. Staying current with technological advancements in the field is an ongoing priority for me.
Q 21. What is your experience with different types of executive function assessments?
Executive function assessments are a cornerstone of my neuropsychological evaluations. I have extensive experience with various tests measuring different aspects of executive function, which include:
- Inhibition: Tests such as the Stroop Color-Word Test, Go/No-Go tasks, and the Hayling Sentence Completion test assess the ability to suppress impulsive responses and control behavior.
- Working memory: Tests like the Digit Span subtest of the Wechsler scales, Corsi Block Tapping, and n-back tasks assess the ability to hold information in mind and manipulate it.
- Cognitive flexibility: The Wisconsin Card Sorting Test (WCST), Trail Making Test (TMT), and the Category Test assess the ability to shift attention between tasks and adapt to changing demands.
- Planning and problem-solving: Tests such as the Tower of London, Tower of Hanoi, and complex figure copying tasks assess the ability to plan ahead, strategize, and solve complex problems.
I often use a combination of these tests to obtain a comprehensive profile of an individual’s executive functioning. This allows me to differentiate between specific executive deficits and provide targeted recommendations for intervention. The choice of specific tests depends on the referral question, patient’s abilities and limitations, and the suspected areas of weakness.
Q 22. Describe your approach to addressing the needs of diverse populations in your neuropsychological evaluations.
Addressing the needs of diverse populations in neuropsychological evaluations requires a multifaceted approach prioritizing cultural sensitivity, linguistic competence, and awareness of potential biases inherent in standardized tests. My approach begins with a thorough understanding of the individual’s background, including their cultural, linguistic, and socioeconomic factors. This involves careful consideration of their communication style, learning history, and potential experiences that could affect test performance.
- Language: If a patient’s primary language isn’t English, I ensure the assessment is conducted in their native language or with the aid of a qualified interpreter. I avoid relying solely on translated versions of tests, as nuances can be lost in translation.
- Culture: I’m mindful of potential cultural differences in communication styles, test-taking behaviors, and interpretations of assessment tasks. For instance, direct eye contact might be considered disrespectful in some cultures, and this could be misinterpreted as disengagement during testing.
- Accessibility: I ensure all aspects of the assessment are accessible to individuals with disabilities, adapting the testing environment and procedures as needed. This may include adjusting the testing room to be quieter or using alternative formats for administering tests.
- Bias Awareness: I’m constantly vigilant for potential biases in test materials and interpretation. For example, some tests may inadvertently favor individuals from specific educational or socioeconomic backgrounds. I actively look for alternative or supplementary measures when necessary to mitigate potential biases.
Ultimately, the goal is to create a comfortable and respectful testing environment that allows each individual to demonstrate their true cognitive abilities, regardless of their background.
Q 23. How do you integrate information from other sources (e.g., medical records, collateral interviews) into your neuropsychological assessment?
Integrating information from multiple sources is crucial for a comprehensive neuropsychological evaluation. It provides a richer understanding of the patient’s condition beyond the test results alone. I treat the neuropsychological evaluation as one piece of a larger puzzle.
- Medical Records Review: I meticulously review medical records, including past medical history, medications, imaging results (MRI, CT scans), and other relevant diagnostic information. This helps me understand the patient’s medical history and potential confounding factors that may influence their performance on neuropsychological tests.
- Collateral Interviews: I conduct interviews with informants who are familiar with the patient, such as family members, caregivers, or employers. These interviews provide valuable information about the patient’s daily functioning, behavioral changes, and premorbid personality. I use a structured interview to ensure consistency and focus on specific aspects of the individual’s functioning.
- Data Integration: I synthesize the data from various sources, looking for patterns and inconsistencies. For example, a discrepancy between the patient’s self-reported symptoms and the observations from a collateral source would necessitate further exploration. I utilize a case formulation approach to integrate findings from all sources to develop a comprehensive understanding of the patient’s strengths and weaknesses.
By combining the objective data from neuropsychological testing with subjective information from other sources, I can develop a more holistic and accurate assessment of cognitive functioning and its impact on the individual’s daily life.
Q 24. How do you determine the appropriate length and scope of a neuropsychological evaluation?
Determining the appropriate length and scope of a neuropsychological evaluation is crucial for efficiency and thoroughness. It depends on several factors, including the referral question, the patient’s presentation, and available time constraints.
- Referral Question: The primary reason for referral directly influences the evaluation’s focus. A referral to assess memory problems after a head injury will require a different battery of tests than an assessment for attention deficits in a child.
- Patient Presentation: The severity of symptoms and the patient’s ability to tolerate testing will guide the assessment’s length and complexity. A patient with severe cognitive impairment might only tolerate a shorter, more focused evaluation, whereas a patient with milder symptoms may require a more extensive assessment.
- Time Constraints: Practical considerations such as the patient’s availability and insurance coverage often influence the scope of testing. Some evaluations may be completed in a single session, while others may require multiple sessions.
- Phased Approach: Sometimes, a phased approach is necessary. An initial brief screening can be followed by a more comprehensive evaluation if indicated by the initial results. This is cost-effective and efficient.
A thorough understanding of the assessment’s goals, combined with clinical judgment, ensures the appropriate balance between comprehensiveness and efficiency in every evaluation.
Q 25. Explain your understanding of the limitations of neuropsychological testing.
Neuropsychological testing, while powerful, has limitations that must be acknowledged. It’s crucial to avoid overinterpreting results or drawing conclusions beyond the scope of the tests used.
- Test Sensitivity and Specificity: No test is perfectly sensitive or specific. A negative result doesn’t necessarily rule out a condition, and a positive result doesn’t automatically confirm a diagnosis. For example, a patient may score poorly on a memory test due to anxiety rather than actual memory impairment.
- Subjectivity in Interpretation: There’s inherent subjectivity in the interpretation of test results. Different clinicians might interpret the same data slightly differently, emphasizing different aspects of the performance.
- Cultural and Linguistic Biases: As mentioned previously, biases in test materials and procedures can affect performance and interpretation. Test scores must be considered in the context of the individual’s background.
- Malinger or Effort: Patients may not always exert maximal effort during testing. Some patients might be deliberately exaggerating symptoms (malingering), while others might be experiencing significant fatigue or emotional distress.
- Individual Differences: Cognitive functioning is complex and multifaceted. Tests measure specific aspects of cognition but may not fully capture the individual’s overall cognitive profile.
Recognizing these limitations is crucial for responsible and ethical neuropsychological practice. It demands a cautious and holistic approach to interpretation, integrating test findings with clinical observation, collateral information, and the patient’s overall context.
Q 26. How do you stay current with the latest advancements in neuropsychological assessment and research?
Staying current in the rapidly evolving field of neuropsychological assessment requires a proactive and multifaceted approach.
- Professional Organizations: Active membership in professional organizations like the National Academy of Neuropsychology (NAN) provides access to journals, conferences, and continuing education opportunities.
- Peer-Reviewed Journals: Regularly reading peer-reviewed journals, such as the Archives of Clinical Neuropsychology and the Journal of the International Neuropsychological Society, keeps me updated on the latest research and methodologies.
- Conferences and Workshops: Attending national and international conferences and workshops allows me to learn from leading experts and network with colleagues.
- Continuing Education: Engaging in continuing education courses and workshops ensures I remain proficient in administering and interpreting the latest neuropsychological tests and integrating new findings into my practice.
- Online Resources: Utilizing reputable online resources, such as databases of psychological tests and research articles, provides additional learning opportunities.
Continuous learning is essential to maintain competence and ensure I provide the highest quality of care to my patients.
Q 27. Describe a situation where you had to modify your approach to neuropsychological testing due to unforeseen circumstances.
During an evaluation of a patient with suspected traumatic brain injury, a severe migraine occurred mid-assessment. The patient became unable to continue testing due to intense pain and nausea.
Instead of abandoning the evaluation, I made modifications:
- Postponement: We scheduled a follow-up appointment after the migraine subsided to complete the remaining tests.
- Alternative Measures: For tasks significantly impacted by the interruption, I considered alternative assessments that minimized physical demands or were less susceptible to acute pain interference.
- Communication: I maintained open communication with the patient and their family, reassuring them that the unexpected event wouldn’t compromise the overall accuracy of the assessment. I explained the rationale for the changes in the testing plan.
- Documentation: I thoroughly documented the incident, including the patient’s symptoms, the modifications made to the testing procedure, and the rationale behind those changes.
This experience emphasized the importance of flexibility, adaptability, and clear communication in neuropsychological assessment. It showed that unforeseen circumstances don’t necessarily invalidate the assessment, provided appropriate modifications are made and documented.
Q 28. How do you communicate complex neuropsychological findings to patients and their families?
Communicating complex neuropsychological findings requires clear, concise, and empathetic communication tailored to the patient’s and family’s understanding. I avoid overwhelming them with technical jargon.
- Plain Language: I explain findings using simple, everyday language, avoiding technical terms unless specifically requested or necessary for clarity. I use analogies and examples to illustrate complex concepts.
- Visual Aids: Graphs, charts, and diagrams can be helpful in illustrating test results and summarizing key findings. I may use a profile of the test scores to visually demonstrate cognitive strengths and weaknesses.
- Step-by-Step Explanation: I present information in a structured manner, starting with a summary of the main findings and then elaborating on specific details.
- Addressing Concerns: I encourage patients and their families to ask questions and address any concerns or uncertainties. I create a safe space for open dialogue.
- Collaborative Approach: I view the communication process as a collaborative effort, actively involving the patient and family in understanding the findings and implications for their lives.
- Written Report: I provide a comprehensive written report that summarizes the findings, integrates information from other sources, and offers recommendations. This document serves as a lasting record of the evaluation.
Effective communication ensures that the patient and family understand the assessment’s implications and can make informed decisions about their care. It strengthens the therapeutic relationship and fosters trust.
Key Topics to Learn for Ability to conduct comprehensive neuropsychological evaluations Interview
- Neuropsychological Assessment Principles: Understanding the theoretical foundations of neuropsychological testing, including the strengths and limitations of various assessment methods.
- Test Selection and Administration: Mastering the art of selecting appropriate tests based on referral questions and patient characteristics, and administering them accurately and ethically.
- Interpretation of Test Results: Developing proficiency in interpreting raw scores, considering individual patient factors, and integrating findings from multiple sources to form a comprehensive profile.
- Differential Diagnosis: Learning to distinguish between various neurological and psychiatric conditions based on neuropsychological test findings, patient history, and other clinical information.
- Report Writing and Communication: Crafting clear, concise, and clinically relevant reports that effectively communicate findings to referral sources and other healthcare professionals.
- Ethical Considerations and Legal Issues: Understanding the ethical implications of neuropsychological assessment, including confidentiality, informed consent, and cultural competency.
- Practical Application: Case Studies: Analyzing case studies to enhance problem-solving skills and develop a deeper understanding of the application of neuropsychological principles in real-world settings. This includes discussing potential biases and limitations in interpretation.
- Working with Diverse Populations: Understanding the unique considerations when conducting assessments with individuals from various cultural backgrounds, age groups, and abilities.
Next Steps
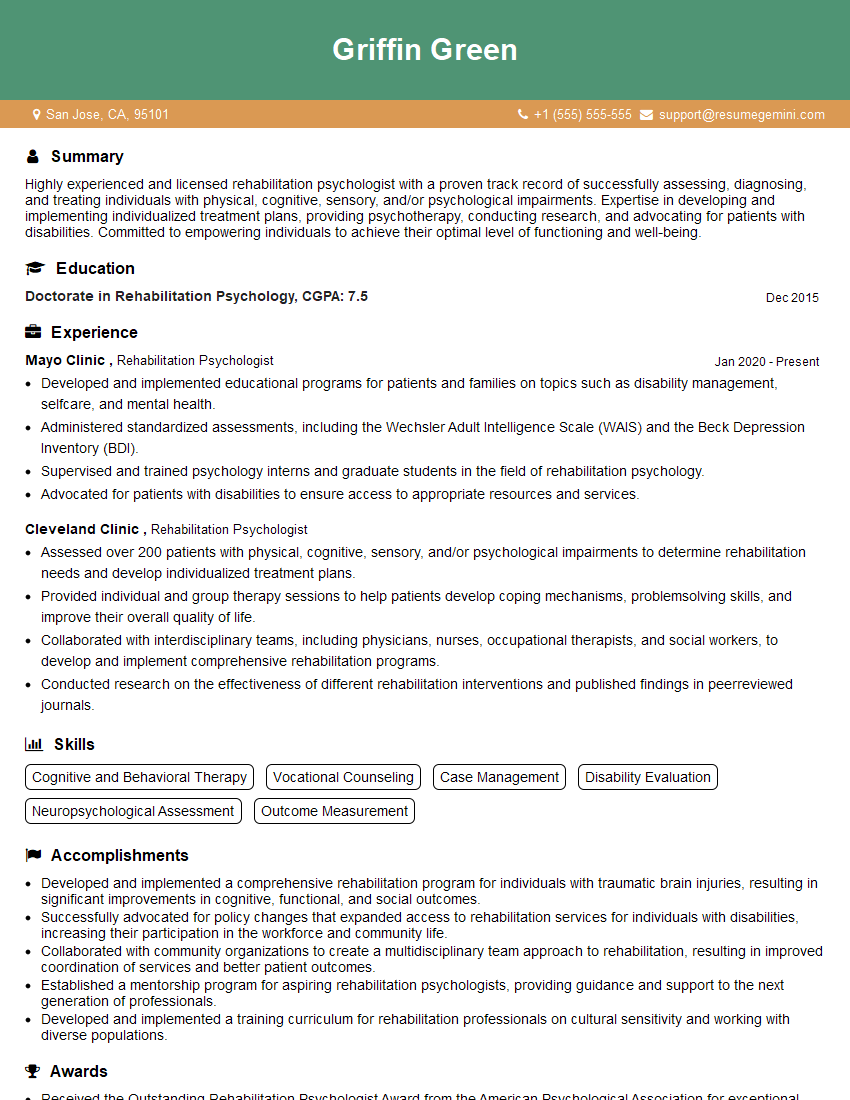
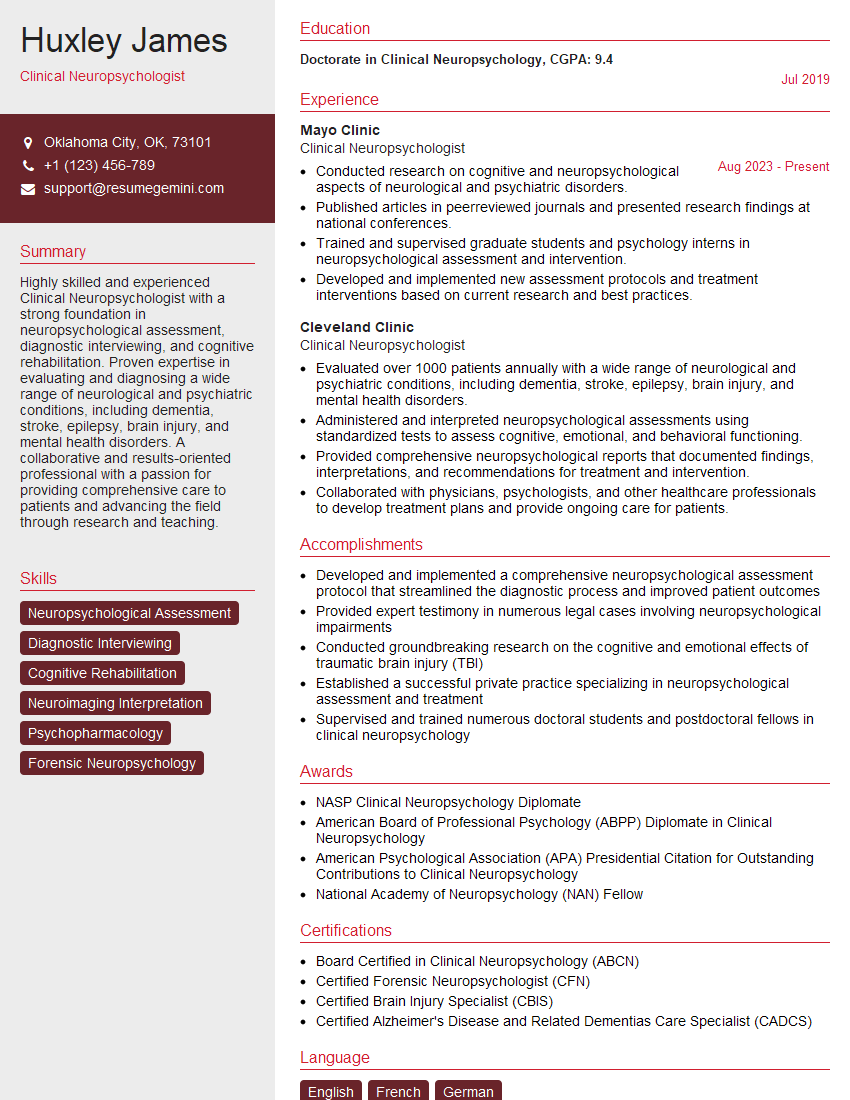
Mastering the ability to conduct comprehensive neuropsychological evaluations is crucial for career advancement in the field of neuropsychology. It opens doors to specialized roles, increased responsibilities, and higher earning potential. To maximize your job prospects, creating an ATS-friendly resume is essential. This ensures your application gets noticed by recruiters and hiring managers. We highly recommend using ResumeGemini to build a professional and impactful resume that highlights your skills and experience effectively. ResumeGemini provides examples of resumes tailored to professionals in neuropsychological assessment, giving you a head start in crafting a compelling application.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
To the interviewgemini.com Webmaster.
Very helpful and content specific questions to help prepare me for my interview!
Thank you
To the interviewgemini.com Webmaster.
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.