Feeling uncertain about what to expect in your upcoming interview? We’ve got you covered! This blog highlights the most important Patient Management and Education interview questions and provides actionable advice to help you stand out as the ideal candidate. Let’s pave the way for your success.
Questions Asked in Patient Management and Education Interview
Q 1. Describe your experience developing patient education materials.
Developing effective patient education materials requires a multi-faceted approach, focusing on clarity, accuracy, and patient-centeredness. My experience spans creating a wide range of materials, from concise handouts and interactive workshops to engaging videos and online modules. I begin by thoroughly researching the topic, ensuring the information is evidence-based and aligned with current clinical guidelines. Then, I tailor the content to the specific needs and literacy levels of the target audience. This often involves simplifying complex medical terminology, using clear and concise language, and incorporating visuals such as diagrams, charts, and photographs to enhance comprehension. For example, when developing materials on diabetes management, I’ve used infographics to visually represent blood sugar control and its relationship to diet and exercise. I also prioritize patient feedback throughout the development process, ensuring the materials are not only informative but also easy to understand and use.
For instance, I once developed a series of short videos explaining post-operative care instructions for joint replacement patients. These videos utilized simple language, clear visuals, and real-patient testimonials to enhance engagement and comprehension. The use of visuals and relatable stories proved more effective than a lengthy printed document.
Q 2. How do you assess a patient’s understanding of their treatment plan?
Assessing a patient’s understanding is crucial for ensuring effective treatment adherence. I use a combination of methods, including direct questioning, observation, and the use of teach-back techniques. Direct questioning involves asking specific questions about the treatment plan, such as medication dosages, side effects, and follow-up appointments. Observation involves paying close attention to a patient’s nonverbal cues, such as facial expressions and body language, which can indicate confusion or lack of understanding. The teach-back method is particularly effective; it involves asking the patient to explain the treatment plan in their own words, allowing me to identify any gaps in knowledge and clarify any misconceptions. For example, after explaining a medication regimen, I might ask the patient, “Can you please explain to me how you will take this medication?” Their response helps determine their understanding.
This multi-pronged approach provides a comprehensive assessment, enabling me to adjust my educational strategies as needed and ensuring patients feel comfortable and confident in managing their care. I always ensure the environment is conducive to open communication, making the patient feel comfortable asking questions without fear of judgment.
Q 3. Explain your approach to tailoring patient education to diverse learning styles.
Tailoring patient education to diverse learning styles is essential for effective communication. I utilize a multimodal approach, incorporating various methods catering to visual, auditory, and kinesthetic learners. Visual learners benefit from diagrams, charts, and videos. Auditory learners respond well to verbal explanations, discussions, and audio recordings. Kinesthetic learners learn best through hands-on activities, role-playing, and demonstrations. For instance, when teaching about medication administration, I might show a video for visual learners, explain the process verbally for auditory learners, and allow hands-on practice with a model for kinesthetic learners. I might use a combination of all three methods. I also consider literacy levels and cultural backgrounds when designing materials, ensuring they are accessible and culturally sensitive. This includes using plain language, avoiding jargon, and adapting the content to match the patient’s preferred communication style.
For example, I once worked with a patient who was visually impaired. I adapted the education strategy by using audio recordings and large-print materials to ensure the information was accessible and understandable. This demonstrates adaptability and personalized attention to each patient’s unique needs.
Q 4. How do you handle patient resistance to following treatment plans?
Patient resistance to treatment plans can stem from various factors, including fear, lack of understanding, or mistrust. My approach involves actively listening to the patient’s concerns, validating their feelings, and collaboratively developing solutions. I begin by exploring the reasons behind the resistance through open-ended questions, creating a safe space for honest dialogue. Then, I address any misconceptions or concerns by providing clear and accurate information in a non-judgmental way. Sometimes, adjusting the treatment plan to better align with the patient’s preferences and abilities is necessary. I also emphasize the benefits of adherence and collaborate to set realistic goals that the patient can achieve. For example, if a patient is hesitant about making significant dietary changes, we might start with small, manageable changes rather than drastic overhauls. Building a strong therapeutic relationship based on trust and empathy is paramount in overcoming resistance.
In cases where resistance persists, I might involve other healthcare professionals, such as social workers or family members, to offer additional support and guidance. The key is to approach the situation with patience, understanding, and a collaborative spirit.
Q 5. Describe a time you had to adapt a patient education strategy due to unforeseen circumstances.
During a patient education session on managing asthma, an unexpected power outage occurred. My initial plan involved using a digital presentation with interactive elements. Quickly, I adapted by utilizing my backup plan – a set of printed educational materials and a whiteboard. I transitioned smoothly, maintaining engagement by using the whiteboard to illustrate key concepts, and by engaging the patient in a more conversational style. This impromptu shift demonstrated my adaptability and resourcefulness. The session remained successful, proving that a flexible approach and well-prepared backup strategies are essential for effective patient education, even when unforeseen circumstances arise.
Q 6. What methods do you use to evaluate the effectiveness of your patient education efforts?
Evaluating the effectiveness of patient education involves a combination of quantitative and qualitative methods. Quantitative methods involve measuring changes in knowledge, attitudes, and behaviors. This can be done through pre- and post-education questionnaires, surveys, and assessments of treatment adherence. For example, I might use a short quiz before and after an education session to measure knowledge gain. Qualitative methods involve gathering feedback from patients through interviews or focus groups, gaining insights into their experiences and understanding. This helps identify areas for improvement and ensures the materials resonate with the intended audience. Observational data, such as the patient’s ability to correctly administer medication or follow dietary guidelines, provides further valuable insight. By combining these methods, I gain a comprehensive picture of the effectiveness of my education strategies and make data-driven adjustments to refine my approach.
Q 7. How do you incorporate technology into your patient education strategies?
Technology plays a significant role in enhancing patient education. I use several technological tools to improve patient engagement and comprehension. These include patient portals for secure messaging and access to educational materials, telehealth platforms for virtual consultations and remote monitoring, and mobile apps that provide medication reminders and personalized health tracking. Videos and interactive simulations can make complex medical information more accessible and engaging. For instance, I use a diabetes management app that allows patients to track their blood sugar levels, set reminders for medication, and receive personalized feedback. I also create short, informative videos explaining various aspects of disease management, making it convenient for patients to access information at their own pace. Technology helps overcome geographical barriers and enables more frequent and personalized interactions with patients, leading to improved health outcomes.
However, I am also mindful of digital literacy and ensure that technology is used in a way that is accessible and inclusive to all patients. I always provide alternative methods for patients who are not comfortable with technology.
Q 8. How do you maintain patient confidentiality when providing education?
Maintaining patient confidentiality is paramount in patient education. It’s the cornerstone of trust and a legal obligation under HIPAA (Health Insurance Portability and Accountability Act). I adhere to strict confidentiality protocols in every interaction. This includes ensuring all conversations, whether face-to-face, over the phone, or via email, occur in private settings. I never discuss patient information with anyone not directly involved in their care without explicit consent.
For example, when discussing a patient’s medication regimen, I would never mention their name or other identifying information in a public area. I always use identifiers like ‘the patient’ or ‘this individual’ when discussing cases in educational settings or team meetings. Furthermore, I only access patient records as necessary for providing direct care or education and strictly follow the organization’s guidelines on data storage and access.
Electronic health records (EHRs) require extra vigilance. I always log out of the system when finished and report any security breaches immediately. Protecting patient information isn’t just a rule; it’s the foundation of a strong therapeutic relationship built on trust and respect.
Q 9. Explain your understanding of health literacy and its impact on patient outcomes.
Health literacy is the ability to obtain, process, and understand basic health information and services needed to make appropriate health decisions. It’s not just about reading ability; it encompasses numeracy, communication skills, and the confidence to use health information effectively. Low health literacy significantly impacts patient outcomes, leading to poorer adherence to treatment plans, increased hospital readmissions, and worse overall health management. Patients with low health literacy may misunderstand instructions, miss appointments, or struggle to manage their conditions effectively.
For instance, a patient with low health literacy might misinterpret dosage instructions on a prescription label, leading to medication errors. They might also struggle to understand complex medical jargon used during consultations, hindering their ability to ask informed questions or actively participate in their care. Addressing health literacy is crucial for achieving positive health outcomes, requiring healthcare professionals to tailor their communication style to ensure clarity and comprehension.
Q 10. How do you address cultural considerations in patient education?
Cultural considerations are vital in patient education. Different cultures have varying health beliefs, communication styles, and preferences for information delivery. Ignoring these differences can lead to misunderstandings, mistrust, and ultimately, ineffective education.
For example, some cultures may emphasize family involvement in healthcare decisions, while others prioritize individual autonomy. Some cultures might prefer direct communication, while others favour more indirect approaches. I make it a point to learn about the patient’s cultural background – their preferred language, communication style, and any relevant beliefs about health and illness – before tailoring my educational approach. I utilize culturally sensitive materials and ensure all information is presented in a clear and easily understandable manner, avoiding medical jargon or culturally insensitive examples. If needed, I seek assistance from interpreters or cultural brokers to ensure effective communication and comprehension.
Q 11. Describe your experience working with patients from diverse socioeconomic backgrounds.
I have extensive experience working with patients from diverse socioeconomic backgrounds. Socioeconomic factors significantly influence health outcomes and access to care. Patients from lower socioeconomic backgrounds often face barriers like limited access to transportation, healthcare insurance, and reliable internet access – all impacting their ability to attend appointments, manage their health, and participate fully in their care.
In my practice, I address these barriers by providing flexible appointment scheduling, ensuring access to affordable resources and transportation assistance, and offering educational materials in various formats (printed, digital, audio) to accommodate different learning styles and access limitations. I also collaborate with social workers and community organizations to connect patients with essential resources like food banks, housing assistance, and financial aid programs. A crucial aspect is building rapport and trust – understanding their challenges and tailoring my approach to their specific needs.
Q 12. How do you identify and address patient learning barriers?
Identifying and addressing patient learning barriers is essential for successful patient education. These barriers can be cognitive (e.g., low health literacy, learning disabilities), sensory (e.g., visual or hearing impairments), emotional (e.g., anxiety, depression), or environmental (e.g., noise, lack of privacy). I utilize a variety of strategies to assess these barriers. This includes directly asking patients about their preferred learning style and any challenges they anticipate, observing their comprehension during educational sessions, and collaborating with other healthcare professionals who might have insights into the patient’s needs and challenges.
For example, if a patient has low vision, I would provide large-print materials or use audio recordings. For a patient struggling with cognitive impairment, I would break down information into smaller, easily digestible chunks, using visual aids and repetition. If anxiety is a barrier, I would create a safe, supportive environment and provide ample time for questions.
Q 13. How do you collaborate with other healthcare professionals to provide comprehensive patient education?
Collaborative patient education is crucial for comprehensive care. I regularly collaborate with other healthcare professionals, including physicians, nurses, social workers, and pharmacists, to ensure consistent and coordinated education. Effective communication and clear role delineation are key. We utilize shared patient portals, team meetings, and case conferences to discuss patient progress, identify educational gaps, and strategize interventions.
For instance, I might work with a physician to clarify complex medical information before presenting it to the patient, or I might collaborate with a pharmacist to address medication concerns. Working as a team ensures the patient receives a holistic and integrated educational experience.
Q 14. Describe your experience using motivational interviewing techniques.
Motivational interviewing (MI) is a patient-centered counseling style that helps patients explore and resolve their ambivalence towards behavior change. It’s a collaborative, guiding approach that empowers patients to take ownership of their health decisions. I utilize MI techniques to help patients overcome barriers to adherence and make informed choices aligned with their personal goals.
In practice, I employ open-ended questions, affirmations, reflective listening, and summaries to understand the patient’s perspective and guide them toward their desired health outcomes. For example, if a patient is struggling with adherence to a diabetic diet, I wouldn’t lecture them but rather collaboratively explore their challenges, identify their strengths, and support them in setting realistic, achievable goals. The focus is on eliciting intrinsic motivation, rather than imposing external pressure. MI is incredibly effective in fostering patient autonomy and engagement in their care journey.
Q 15. Explain your experience with patient portals and telehealth platforms for education.
Patient portals and telehealth platforms are invaluable tools for patient education. My experience encompasses utilizing these platforms to deliver tailored educational materials, schedule virtual appointments for education sessions, and track patient engagement with resources. For example, I’ve used patient portals to upload personalized videos explaining complex treatment plans, ensuring patients have easy access to information at their convenience. Telehealth platforms allow for interactive sessions, where I can answer questions in real-time, demonstrate techniques, and provide immediate feedback. This personalized approach significantly enhances understanding and improves adherence to treatment plans. I’ve also leveraged these platforms to offer remote monitoring of vital signs, allowing for proactive identification of potential issues and timely educational interventions.
In one instance, I developed a series of short, easily digestible videos on a patient portal explaining the proper use of an inhaler. Patient feedback indicated a significant improvement in their understanding and confidence in self-managing their asthma compared to traditional in-person instruction alone.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you prioritize patient education needs among competing demands?
Prioritizing patient education needs requires a systematic approach. I use a combination of factors to determine the urgency and importance of educational needs. Firstly, I assess the patient’s risk level—higher-risk patients needing immediate attention, such as those with newly diagnosed conditions or facing potential complications, receive priority. Secondly, I consider the patient’s readiness to learn and their learning style. Some patients may require more immediate and intensive education, while others may benefit from a phased approach. Thirdly, I integrate the patient’s goals and preferences. It’s crucial to involve the patient actively in the process, ensuring they feel heard and understood.
For example, if I have a patient post-surgery needing pain management education and another with a chronic condition needing general health maintenance information, I’d prioritize the post-surgery patient due to immediate needs and risk of complications. However, a comprehensive plan would include scheduling follow-up sessions for both, tailoring the content and timing to meet individual needs.
Q 17. Describe a challenging patient education situation you successfully managed.
One particularly challenging situation involved a patient diagnosed with type 2 diabetes who was resistant to making lifestyle changes. Despite providing extensive information on diet and exercise, he was dismissive and frustrated. I recognized the need for a shift in approach. Instead of lecturing, I encouraged him to share his concerns and barriers. Through empathetic listening, I discovered his frustration stemmed from a feeling of being overwhelmed and lacking confidence in his ability to make lasting changes. We collaboratively developed a manageable plan with small, achievable goals. We focused on one habit at a time, providing consistent support and celebrating his progress. Gradually, he became more engaged and motivated. Regular check-ins, combined with readily available educational resources and positive reinforcement, facilitated successful behaviour changes.
Q 18. How do you document patient education interactions effectively?
Effective documentation is crucial for maintaining accurate records and ensuring continuity of care. My documentation strategy includes noting the date, time, and method of education (e.g., in-person, telehealth, written materials). I detail the specific topics covered, the patient’s understanding and response, and any questions or concerns raised. I also record any educational materials provided and the patient’s feedback. The documentation should clearly reflect any agreed upon action plans and future educational needs. This ensures all healthcare providers involved have access to a comprehensive history of the patient’s educational journey. For example, using standardized templates or electronic health record (EHR) systems improves efficiency and maintains consistency.
Q 19. What are your preferred methods for providing ongoing support to patients after initial education?
Ongoing support is vital for long-term success. I use a multi-faceted approach. This includes scheduling follow-up appointments to review progress, answer questions, and provide additional education as needed. I offer access to support groups and online resources for continued learning and community engagement. I encourage patients to utilize patient portals for accessing educational materials and communicating with the healthcare team. For example, I might offer a monthly check-in phone call to discuss any challenges or concerns, reinforcing positive behaviour changes and addressing any setbacks. Consistent and readily available support systems play a critical role in maintaining compliance with treatment plans.
Q 20. How do you measure patient satisfaction with your education services?
Measuring patient satisfaction is essential for continuous improvement. I employ several methods: firstly, I utilize structured questionnaires or surveys to gather feedback on the clarity, usefulness, and effectiveness of the education provided. Secondly, I actively solicit feedback during interactions with patients, paying attention to their verbal and nonverbal cues. Thirdly, I track patient adherence to treatment plans and health outcomes, as this indirectly reflects the effectiveness of the educational interventions. Analyzing this data helps identify areas needing improvement, providing valuable insights for enhancing future educational strategies. For instance, feedback might reveal a need for more visual aids or simpler language in educational materials.
Q 21. What are some common misconceptions patients have regarding their condition or treatment?
Common misconceptions vary depending on the condition but frequently include misunderstandings about medication, treatment duration, and prognosis. For instance, patients may believe antibiotics cure viral infections, stop taking medications prematurely believing they are cured, or misinterpret the meaning of a long-term condition’s prognosis. Addressing these misconceptions requires clear, evidence-based communication tailored to the patient’s understanding. Using simple language, visual aids, and providing ample opportunities for questions are crucial. For example, I might use analogies to explain complex medical concepts, ensuring the information is not only understood but also retained.
Q 22. How do you use teach-back methods to confirm patient understanding?
The teach-back method is a powerful communication technique to ensure patients understand medical instructions. It’s not about testing their knowledge, but rather confirming their comprehension through a simple, respectful process. Instead of asking if they understand, I ask them to explain the information back to me in their own words, using their own examples. This allows me to identify any gaps in understanding and clarify any misconceptions. For example, if I’ve explained a medication regimen, I might say, “Can you tell me how you will take this medication each day?” Their response reveals whether they truly grasped the dosage, timing, and potential side effects. If they don’t understand fully, I re-explain, using different language or visual aids, until their explanation demonstrates clear comprehension.
This iterative process, of explanation and teach-back, ensures shared understanding and fosters patient engagement and empowerment. It is far more effective than simply asking ‘Do you understand?’ because it actively involves the patient in the learning process and ensures the information is understood, not just heard.
Q 23. What are some effective strategies for promoting patient self-management?
Promoting patient self-management involves empowering patients to actively participate in managing their health conditions. This requires a multifaceted approach:
- Education: Providing clear, concise, and accessible information about their condition, treatment options, and potential complications. This includes using various methods like printed materials, videos, and interactive sessions tailored to their literacy level and learning style. For example, using plain language summaries of complex medical procedures greatly increases comprehension.
- Goal Setting: Collaboratively setting realistic and achievable goals. This could involve tracking blood sugar levels, adhering to a medication regimen, or incorporating more physical activity. Regular check-ins and progress reviews are crucial.
- Skill Building: Teaching patients practical skills relevant to their condition. This might include self-injection techniques, wound care, or techniques for managing symptoms. Hands-on practice and feedback are key components.
- Problem-Solving: Equipping patients with tools and strategies to address challenges they might face in managing their condition, such as dealing with medication side effects or managing stress. Role-playing scenarios can be highly effective.
- Support Systems: Connecting patients with support networks, including family, friends, support groups, or online communities. This creates a sense of shared experience and fosters emotional well-being.
A successful self-management program considers individual needs and preferences, using a combination of these strategies to create a personalized plan.
Q 24. How do you stay current with best practices in patient education?
Staying current in patient education involves a commitment to continuous learning. I achieve this through several methods:
- Professional Development: Attending conferences, workshops, and webinars focused on patient education best practices. This allows me to learn about the latest research, innovative techniques, and emerging technologies.
- Professional Organizations: Membership in relevant professional organizations such as the Patient Advocate Foundation provides access to resources, publications, and networking opportunities.
- Peer Learning: Engaging in discussions and knowledge sharing with colleagues and other healthcare professionals. This allows for learning from each other’s experiences and best practices.
- Evidence-Based Resources: Regularly reviewing reputable journals, publications, and online databases to stay informed about the latest research and guidelines.
- Continuous Feedback: Actively seeking feedback from patients regarding the effectiveness of educational materials and approaches. This helps tailor our materials to meet their specific needs.
This multi-pronged approach ensures I am up-to-date on evidence-based practices and adapt my teaching strategies accordingly. For instance, I recently attended a webinar on using technology in patient education, which inspired me to incorporate more engaging videos and interactive apps into my programs.
Q 25. Describe your experience with developing and delivering educational programs to large groups.
I have extensive experience developing and delivering educational programs to large groups, ranging from workshops on chronic disease management to training sessions for healthcare professionals. My approach involves meticulous planning and delivery to ensure the information is clear, engaging, and accessible to all participants. For example, when delivering a program on diabetes self-management to 50 patients, I used a blended approach combining interactive lectures, small group discussions, and hands-on demonstrations. This ensured participants were actively involved throughout the session. Pre- and post-tests assessed their knowledge and understanding.
I incorporate multimedia elements, such as videos and interactive exercises, to break up the information and keep participants engaged. Clear visual aids, such as charts and infographics, are crucial, particularly for complex information. Question-and-answer sessions are encouraged, allowing me to address individual concerns. Feedback mechanisms, including surveys and follow-up sessions, allow for improvement and gauging the effectiveness of the training.
Q 26. What are your strengths and weaknesses regarding patient education?
Strengths: I possess a strong ability to connect with patients on an individual level, building trust and rapport that enables effective communication and understanding. I’m adept at adapting my communication style to different learning styles and literacy levels. I’m skilled at developing and implementing engaging and informative educational materials. My creativity and patience allow me to explain complex concepts clearly and simply.
Weaknesses: Like any educator, I continually strive to improve my skills in utilizing new technologies and incorporating interactive elements into my teaching. I’m also working on enhancing my ability to manage difficult conversations with patients who may be resistant to learning or have limited health literacy.
Q 27. How do you ensure accessibility of patient education materials for all patients?
Ensuring accessibility of patient education materials is paramount. I employ several strategies to make materials accessible to all patients, regardless of their literacy level, language preference, or disability:
- Plain Language: Using clear, concise language, avoiding medical jargon, and keeping sentences short and simple.
- Multiple Formats: Offering materials in various formats, such as printed materials, audio recordings, videos, and easy-to-read versions.
- Translation Services: Providing materials in different languages to accommodate diverse patient populations.
- Accessibility Features: Incorporating accessibility features, such as large font sizes, high contrast text, and alternative text descriptions for images for patients with visual impairments.
- Universal Design Principles: Applying universal design principles to create materials that are inherently accessible to everyone, regardless of their abilities.
- Health Literacy Assessments: Using validated health literacy assessment tools to identify patients’ needs and tailor education accordingly. This allows me to select the most appropriate format for each individual.
Regularly reviewing and updating materials based on feedback from patients and staff ensures continued accessibility and effectiveness.
Q 28. How do you handle situations where a patient’s family or caregivers are involved in their care and education?
When families or caregivers are involved, I ensure they are included in the education process but always respecting patient autonomy. I begin by assessing the patient’s preference regarding family involvement. I then tailor my communication to include both the patient and family/caregiver, using clear and simple language to explain the condition, treatment plan, and potential complications. This collaborative approach enhances understanding and ensures everyone is on the same page.
I utilize visual aids and teach-back methods with both the patient and their family/caregivers to ensure that everyone has a thorough understanding of the information. I also address any questions or concerns they may have and provide resources for additional support. The family/caregiver’s role and the patient’s level of participation in their own care and education are discussed and negotiated to ensure a team approach and respect for patient-centered decision-making.
Key Topics to Learn for Patient Management and Education Interview
- Patient Assessment and Needs Identification: Understanding patient demographics, medical history, learning styles, and health literacy levels to tailor education plans effectively.
- Developing Educational Materials: Creating clear, concise, and culturally sensitive materials (brochures, handouts, presentations) using various media appropriate for different learning styles and health literacy levels. Practical application: Designing a handout explaining medication adherence for a patient with limited health literacy.
- Teaching and Communication Strategies: Employing effective communication techniques (active listening, motivational interviewing) to engage patients and ensure understanding. Practical application: Role-playing scenarios to practice explaining complex medical information to patients with varying levels of understanding.
- Health Literacy and Cultural Competence: Recognizing and addressing the impact of health literacy and cultural differences on patient understanding and adherence. Practical application: Adapting teaching methods to accommodate diverse cultural backgrounds and literacy levels.
- Documentation and Evaluation: Maintaining accurate records of patient education sessions, including assessment, teaching methods, and patient response. Practical application: Creating a sample patient education documentation template for a specific condition.
- Technology in Patient Education: Utilizing electronic health records (EHRs) and patient portals to deliver and track patient education. Practical application: Exploring the use of telehealth platforms for patient education.
- Collaboration and Teamwork: Working effectively with healthcare professionals (doctors, nurses, social workers) to provide coordinated patient care and education. Practical application: Describing how to collaborate effectively with a multidisciplinary team to address a patient’s complex needs.
- Program Evaluation and Improvement: Assessing the effectiveness of patient education programs and making necessary improvements based on data and feedback.
Next Steps
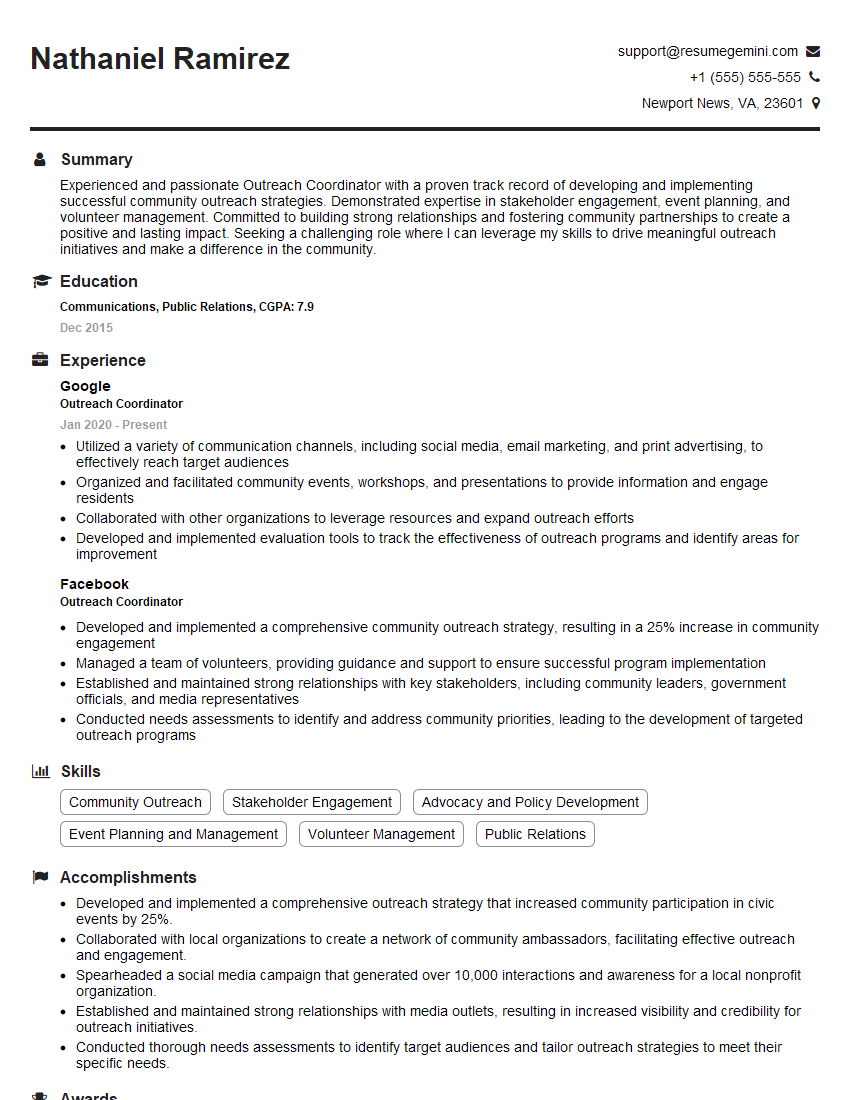
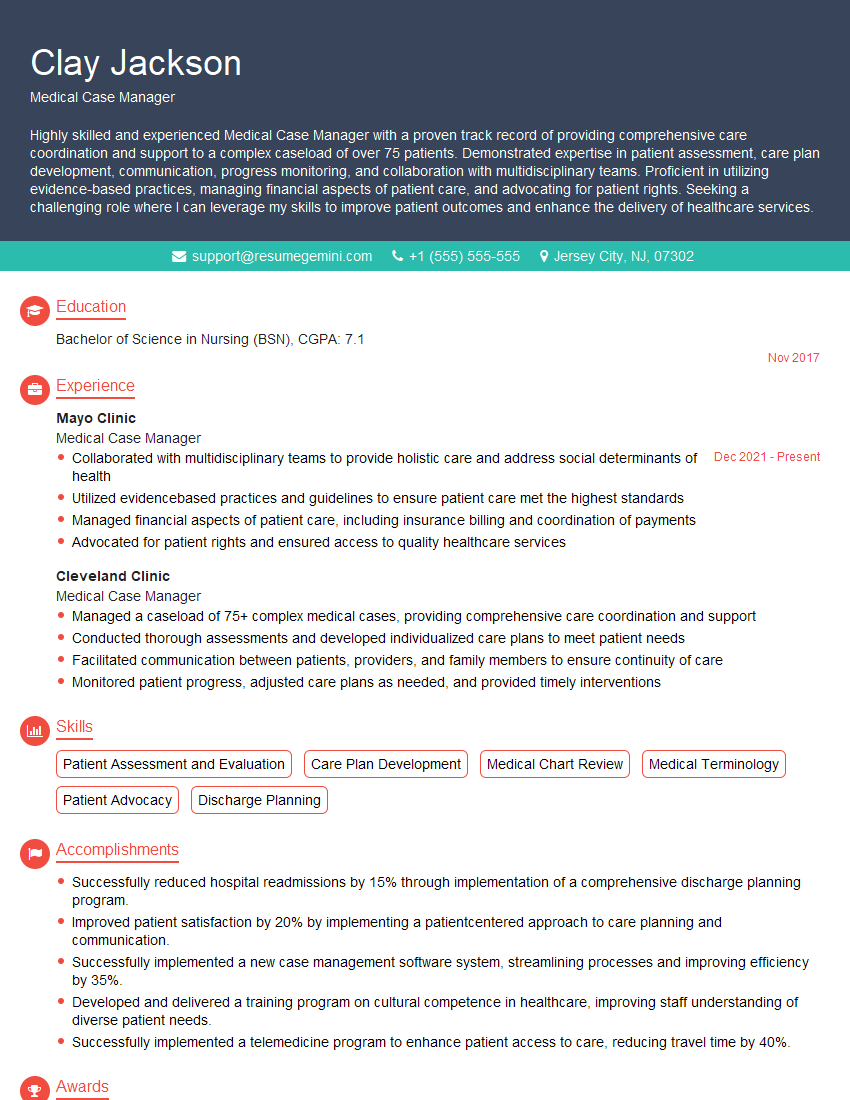
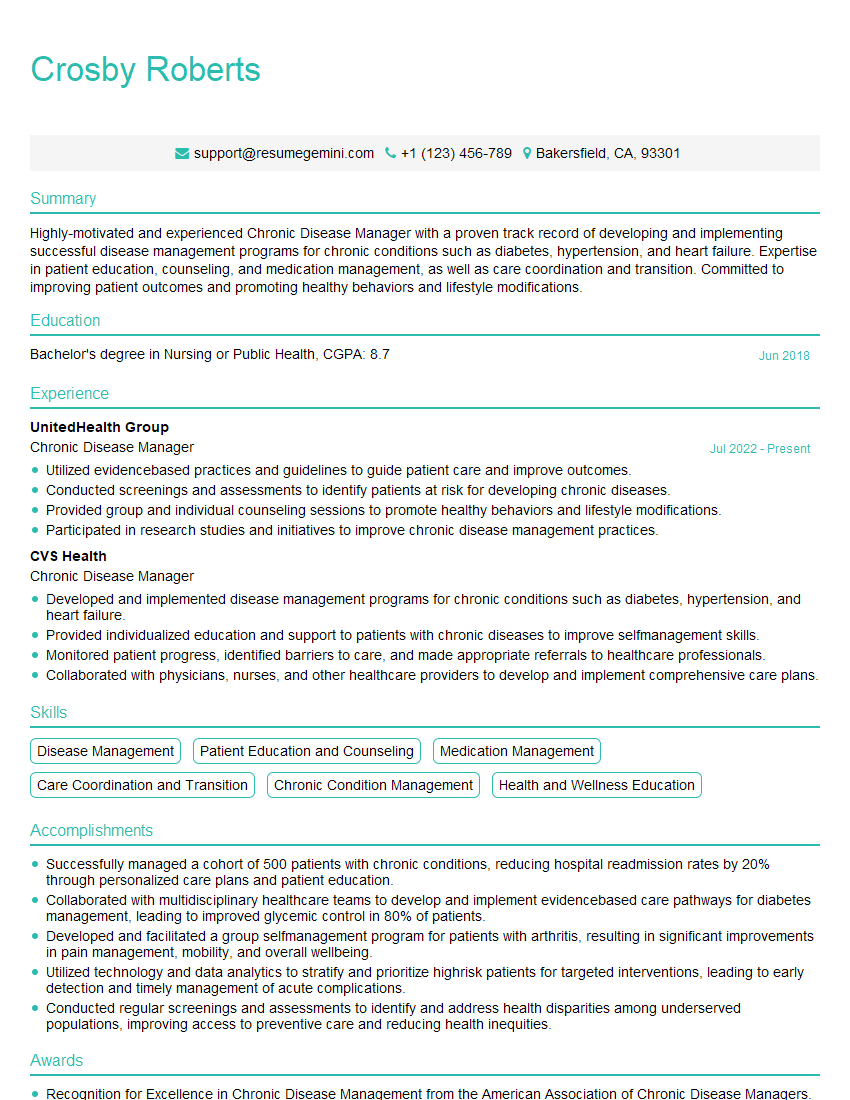
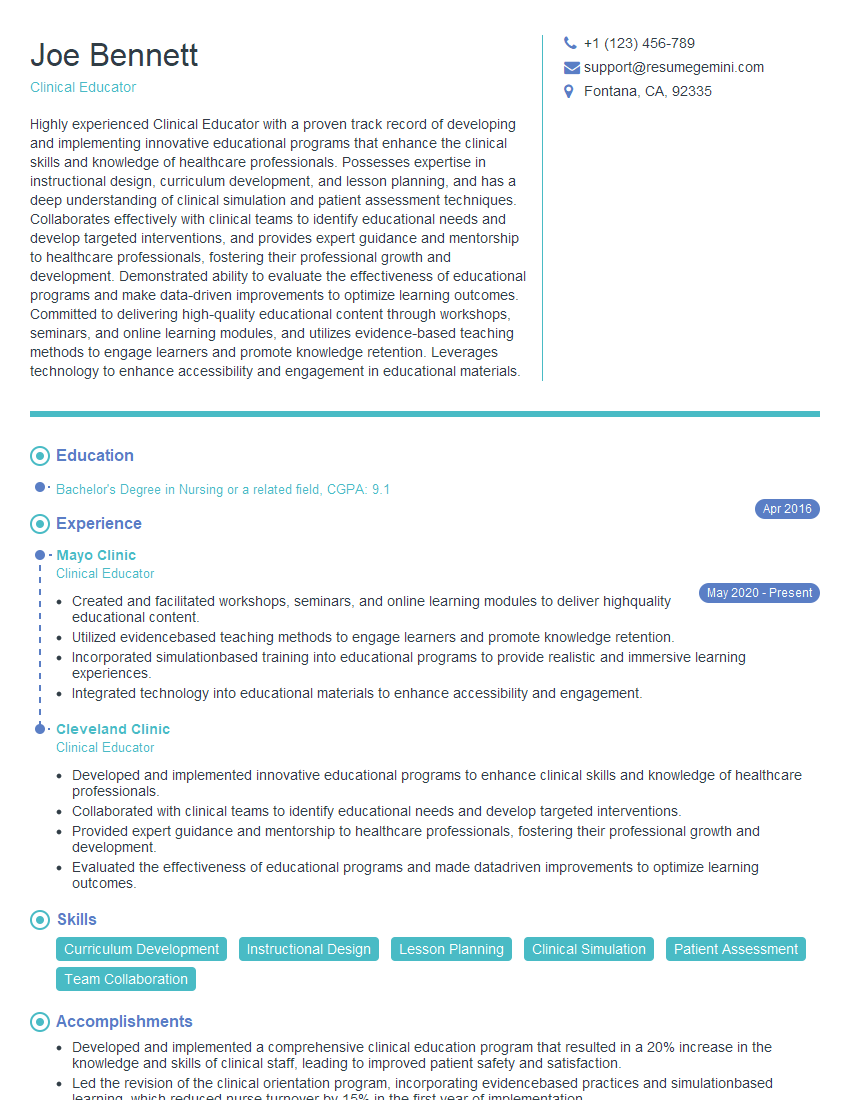
Mastering Patient Management and Education is crucial for career advancement in healthcare. It demonstrates your commitment to patient-centered care and enhances your value as a healthcare professional. To significantly boost your job prospects, invest time in crafting an ATS-friendly resume that highlights your skills and experience effectively. ResumeGemini is a trusted resource that can help you build a professional and impactful resume. They provide examples of resumes tailored to Patient Management and Education, giving you a head start in creating a document that showcases your abilities and lands you that interview.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
To the interviewgemini.com Webmaster.
Very helpful and content specific questions to help prepare me for my interview!
Thank you
To the interviewgemini.com Webmaster.
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.