The right preparation can turn an interview into an opportunity to showcase your expertise. This guide to Diagnostic Lumbar Puncture interview questions is your ultimate resource, providing key insights and tips to help you ace your responses and stand out as a top candidate.
Questions Asked in Diagnostic Lumbar Puncture Interview
Q 1. Describe the anatomy relevant to performing a lumbar puncture.
Understanding the anatomy of the lumbar spine is crucial for a successful and safe lumbar puncture. The procedure targets the subarachnoid space, which lies between the arachnoid mater and pia mater, the innermost layers of the meninges surrounding the spinal cord. This space contains cerebrospinal fluid (CSF).
Specifically, we need to visualize the landmarks of the lumbar vertebrae, the spinous processes, and the intervertebral spaces. The lumbar puncture typically accesses the subarachnoid space between L3-L4 or L4-L5. This region is chosen because the spinal cord typically ends at the level of L1-L2 in adults, minimizing the risk of spinal cord injury. The needle passes through the skin, subcutaneous tissue, supraspinous ligament, interspinous ligament, ligamentum flavum, epidural space, dura mater, and arachnoid mater before reaching the subarachnoid space.
Imagine the spine like a stack of building blocks. The spinous processes are the easily palpable projections at the back of each vertebra. The intervertebral spaces are the gaps between these blocks. Finding the correct space is vital to accurately performing the procedure. We also need to be aware of the surrounding vasculature and nerves, to avoid accidental puncture.
Q 2. What are the contraindications for performing a lumbar puncture?
Several contraindications exist for performing a lumbar puncture. These can be broadly categorized into absolute and relative contraindications.
- Absolute Contraindications: These are situations where a lumbar puncture should absolutely be avoided due to a high risk of significant harm. This includes localized skin infection at the puncture site (cellulitis), increased intracranial pressure (ICP) as indicated by papilledema or signs of brainstem herniation, severe thrombocytopenia (low platelet count), and patients who refuse the procedure.
- Relative Contraindications: These are situations where the benefits of the lumbar puncture need to be carefully weighed against the potential risks. Examples include severe spinal stenosis, spinal deformity, coagulation disorders (although carefully managed with appropriate precautions), and recent spinal surgery.
For instance, a patient with a significant infection at the intended puncture site risks spreading the infection into the CSF. A patient with elevated intracranial pressure risks brainstem herniation, a life-threatening complication.
Q 3. Explain the steps involved in performing a diagnostic lumbar puncture.
Performing a diagnostic lumbar puncture is a meticulous procedure requiring sterile technique. The steps involved are:
- Patient Preparation and Positioning: The patient is typically positioned in the lateral decubitus position (lying on their side with their knees flexed towards their chest). The back should be appropriately draped and cleaned with an antiseptic solution.
- Landmark Identification: Palpate the spinous processes to identify the appropriate intervertebral space (usually L3-L4 or L4-L5).
- Local Anesthesia: Inject a local anesthetic (e.g., lidocaine) into the skin and subcutaneous tissue at the puncture site.
- Needle Insertion: Insert the appropriately sized spinal needle (usually 22-27 gauge) in the midline, aiming slightly cephalad (towards the head), advancing until CSF is obtained.
- CSF Collection: Once CSF is obtained, collect the required amount of CSF into sterile tubes for laboratory analysis, usually several tubes to avoid contamination between specimens and ensure enough for all testing.
- Needle Removal: Remove the needle, apply pressure to the puncture site with a sterile dressing to minimize post-puncture headache, and instruct the patient to lie flat for a designated period.
- Post-Procedure Monitoring: Monitor the patient for any complications, such as headache, leakage of CSF, or neurological changes.
Throughout the procedure, constant monitoring of the patient’s vital signs and neurological status is imperative. The entire process requires precision and a calm, methodical approach.
Q 4. What are the potential complications of a lumbar puncture?
While generally a safe procedure, lumbar puncture carries potential complications. These can range from minor to life-threatening.
- Post-dural puncture headache (PDPH): This is the most common complication, characterized by a severe headache that worsens when sitting or standing and improves when lying down. It’s believed to be caused by leakage of CSF from the puncture site.
- Bleeding: Hematoma formation at the puncture site is a rare but serious complication, potentially requiring intervention. The risk is elevated in patients with bleeding disorders.
- Infection: Although rare with proper sterile technique, meningitis or abscess formation is possible.
- Nerve damage: Injury to a nerve root during needle insertion can lead to pain or weakness.
- Herniation of the cerebellar tonsils (rare): This is more likely in patients with increased intracranial pressure.
- Spinal cord injury (very rare): This is a rare but severe complication resulting from inappropriate needle placement.
Knowing the potential complications allows for careful pre-procedure risk assessment and timely management of any adverse events.
Q 5. How do you select the appropriate needle size for a lumbar puncture?
Needle size selection for lumbar puncture depends on various factors, including the patient’s age, clinical indication, and the operator’s preference. Generally, smaller-gauge needles (22-27 gauge) are preferred to minimize trauma to the tissues and reduce the risk of complications. A 22-gauge needle is often used for CSF studies requiring larger fluid volumes, whereas a 27-gauge needle might be considered for patients with increased risk of bleeding disorders.
Smaller gauge needles offer the benefit of reduced trauma and lower risk of bleeding, but they may require more force to penetrate the dura. Conversely, larger-gauge needles are easier to insert but potentially increase the risk of complications like bleeding.
Choosing the appropriate needle size is a balance between ease of insertion and minimizing patient trauma.
Q 6. How do you determine the appropriate puncture site for a lumbar puncture?
The ideal puncture site for a lumbar puncture is usually between the L3-L4 or L4-L5 intervertebral spaces. This location is chosen because the spinal cord typically ends around L1-L2 in adults, reducing the risk of spinal cord injury. These spaces are easily palpable and provide sufficient depth for needle insertion into the subarachnoid space.
To identify the puncture site accurately, the clinician palpates the spinous processes of the lumbar vertebrae. A line drawn between the posterior superior iliac crests (the bony prominences on the hips) usually intersects the spinous process of L4. The intervertebral space above (L3-L4) or below (L4-L5) is then targeted. The final decision of the site often takes the anatomy of the individual patient into consideration to avoid any potential difficulty with the procedure.
Q 7. Describe the proper patient positioning for a lumbar puncture.
Proper patient positioning is essential for a successful and safe lumbar puncture. The most common position is the lateral decubitus position, where the patient lies on their side with their back parallel to the edge of the examination table, knees flexed towards the chest, and head flexed onto the chest. This position helps to widen the intervertebral spaces, making needle insertion easier and safer.
The patient’s spine should be in a straight line to avoid any undue curvature or misalignment. The hips and shoulders should be aligned, and the knees should be flexed to help relax the back muscles and minimize discomfort. This relaxed posture is beneficial to both the patient’s comfort and the success of the procedure. Proper support during the procedure also adds to the comfort and safety of the patient.
Q 8. What are the signs and symptoms of a post-lumbar puncture headache?
A post-lumbar puncture headache (PLPH), also known as a spinal headache, is a common complication following a lumbar puncture. It’s caused by leakage of cerebrospinal fluid (CSF) from the puncture site in the dura mater, the tough outer membrane surrounding the brain and spinal cord. This leakage lowers the pressure within the skull, causing the brain to sag slightly and pull on pain-sensitive structures.
The hallmark symptom is a headache that typically begins within one to two days after the procedure and gradually worsens. It’s often described as a positional headache, meaning it’s worse when sitting or standing and improves when lying down. Other symptoms can include:
- Headache that is throbbing or dull
- Neck stiffness
- Nausea and vomiting
- Blurred vision
- Sensitivity to light (photophobia) and sound (phonophobia)
The severity varies widely, ranging from a mild inconvenience to a debilitating condition. It’s important to note that not everyone who undergoes a lumbar puncture experiences a PLPH.
Q 9. How do you manage a post-lumbar puncture headache?
Management of a PLPH focuses on relieving symptoms and promoting CSF resorption. The cornerstone of treatment is conservative management. This includes:
- Hydration: Increased fluid intake helps replenish CSF volume.
- Bed rest: Limiting activity, particularly upright positions, reduces the pull on pain-sensitive structures.
- Analgesics: Over-the-counter pain relievers like acetaminophen or ibuprofen can provide relief. Stronger analgesics may be necessary in severe cases.
- Caffeine: Caffeine is sometimes used because it is a vasoconstrictor and may reduce leakage, though the efficacy is debatable.
If conservative management fails, a blood patch is typically performed. This involves injecting a small amount of the patient’s own blood into the epidural space at the lumbar puncture site. The blood clots, sealing the leak and restoring CSF pressure. This procedure is usually very effective in resolving PLPH.
In rare instances, more aggressive interventions may be required, but these are usually only considered after conservative and blood patch methods have failed.
Q 10. What are the indications for a lumbar puncture?
A lumbar puncture, also known as a spinal tap, is a diagnostic procedure used to collect a sample of cerebrospinal fluid (CSF) from the subarachnoid space in the spinal canal. It’s a valuable tool for diagnosing a wide range of neurological conditions. The indications include:
- Suspected infection of the central nervous system (CNS): This includes meningitis, encephalitis, and brain abscesses. Analyzing the CSF helps identify the causative organism.
- Suspected hemorrhage into the CNS: A lumbar puncture can detect blood in the CSF, indicating a subarachnoid hemorrhage or other intracranial bleed.
- Diagnosis of neurological disorders: Conditions like multiple sclerosis (MS) and Guillain-Barré syndrome often show characteristic changes in CSF composition.
- Measurement of CSF pressure: Elevated or decreased pressure can provide clues to various neurological conditions.
- Administration of medications or contrast agents into the CSF: In certain cases, this may be part of therapeutic or diagnostic procedures.
The decision to perform a lumbar puncture is made on a case-by-case basis, considering the patient’s clinical presentation, risk factors, and potential benefits compared to risks.
Q 11. How do you interpret the results of a lumbar puncture analysis?
Interpreting lumbar puncture results requires careful consideration of multiple parameters. The analysis includes:
- Appearance: Normal CSF is clear and colorless. Cloudy CSF may indicate infection, while blood suggests hemorrhage.
- Opening pressure: This reflects intracranial pressure. Elevated pressure can be seen in conditions like increased intracranial pressure (ICP), while decreased pressure can be due to dehydration or CSF leakage.
- Cell count: A high white blood cell (WBC) count indicates inflammation or infection. An elevated red blood cell (RBC) count suggests hemorrhage.
- Protein level: Elevated protein levels can be seen in various conditions, including infection, inflammation, and CNS disorders.
- Glucose level: Decreased glucose levels often indicate bacterial meningitis.
- Microbial cultures: These identify the causative organism in suspected infections.
- Other tests: Additional tests may be performed to detect specific antibodies, tumor markers, or other indicators of disease.
The interpretation is complex and should be done by experienced medical professionals, considering the patient’s clinical picture and other findings. A single abnormal result doesn’t necessarily indicate a specific diagnosis; rather, it’s the overall pattern of results that is crucial.
Q 12. What is the normal opening pressure for cerebrospinal fluid (CSF)?
The normal opening pressure for cerebrospinal fluid (CSF) varies depending on the patient’s age, position, and other factors. However, generally, the normal range is considered to be between 7-20 cm H2O when the patient is lying laterally on their side. Pressures outside this range can indicate several different issues, necessitating further investigation. Factors like obesity and the patient’s posture can slightly alter the reading.
Q 13. What are the different types of CSF analyses performed?
Several types of CSF analyses are performed, depending on the suspected condition. These include:
- Cell count and differential: This determines the number and types of cells present (RBCs and WBCs).
- Chemistry analysis: This measures glucose, protein, lactate, and other substances.
- Microbial cultures: This involves culturing CSF samples to identify bacteria, viruses, or fungi.
- Gram stain: A rapid test to identify bacteria in CSF.
- Polymerase chain reaction (PCR): A highly sensitive test to detect specific DNA or RNA sequences of viruses or bacteria.
- Immunological tests: These detect specific antibodies associated with certain neurological conditions (e.g., oligoclonal bands in MS).
The specific analyses performed depend on the clinical suspicion. For example, suspected bacterial meningitis would prompt bacterial cultures and Gram stain, while suspected viral meningitis might focus on PCR tests.
Q 14. Describe the appearance of normal CSF.
Normal CSF is typically clear and colorless, like water. It should be free of visible blood or cloudiness. The presence of blood or cloudiness can indicate pathological conditions. A slightly yellow tinge (xanthochromia) can occur due to the breakdown of red blood cells in the CSF, often indicating prior hemorrhage. However, it’s crucial to remember that visual appearance alone is not sufficient for diagnosis and needs to be correlated with other test results.
Q 15. How do you differentiate between bacterial, viral, and fungal meningitis based on CSF analysis?
Differentiating between bacterial, viral, and fungal meningitis relies heavily on cerebrospinal fluid (CSF) analysis. While there’s overlap, certain patterns emerge. Imagine CSF analysis as a detective’s toolkit, providing clues to the culprit.
- Bacterial Meningitis: This is the most serious type. The CSF typically shows a high white blood cell count (predominantly neutrophils), significantly decreased glucose levels (bacteria consume glucose), and elevated protein levels. Think of it as a battlefield – lots of inflammatory cells fighting the infection, depleted glucose resources, and protein leakage from damaged blood vessels. For example, Streptococcus pneumoniae and Neisseria meningitidis are common culprits.
- Viral Meningitis: Generally milder, viral meningitis presents with a moderate increase in white blood cells (mostly lymphocytes), normal or slightly low glucose, and slightly elevated protein. The inflammatory response is less intense compared to bacterial meningitis. Think of this as a smaller skirmish, fewer cells involved, and less damage to the blood-brain barrier. Common viruses include enteroviruses and herpes simplex virus.
- Fungal Meningitis: This is often a chronic infection and the presentation is more insidious. CSF analysis typically shows a lymphocytic predominance, low glucose, and elevated protein, often with a longer time to diagnosis. The immune response is often subdued, meaning the numbers of white cells might not be as dramatically high as in bacterial infections. Cryptococcus neoformans is a common fungal cause.
It’s crucial to remember that these are general patterns, and exceptions exist. Gram stain and culture of the CSF are vital for definitive diagnosis, providing identification of the pathogen responsible. For instance, a patient with a partially treated bacterial infection might show atypical CSF findings.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What are the common causes of elevated protein levels in CSF?
Elevated protein levels in CSF, or hyperproteinorrachia, indicate a disruption of the blood-brain barrier. Imagine the barrier as a tightly sealed dam, regulating what enters and leaves the brain. When damaged, proteins leak into the CSF.
- Infections: Meningitis (bacterial, viral, fungal), encephalitis, and brain abscesses are common causes as infection damages the blood-brain barrier.
- Inflammatory Conditions: Multiple sclerosis, Guillain-Barré syndrome, and sarcoidosis cause inflammation, leading to barrier damage and protein leakage. Think of inflammation as the dam experiencing erosion.
- Tumors: Brain or spinal cord tumors can obstruct CSF flow and compress the blood vessels, increasing protein levels. This is like a blockage causing a build-up of pressure, leading to leaks.
- Subarachnoid Hemorrhage: Bleeding into the subarachnoid space directly introduces protein into the CSF.
- Other Neurological Conditions: Conditions like cerebral infarction (stroke) can also lead to increased protein levels.
Q 17. What are the common causes of elevated glucose levels in CSF?
Elevated glucose levels in CSF are relatively uncommon and typically reflect elevated serum glucose levels. The glucose concentration in the CSF is usually about 60-70% of the serum glucose level. Any increase would simply reflect the underlying hyperglycemia.
- Hyperglycemia: This is the most common cause; high blood sugar (diabetes mellitus) will lead to a proportional increase in CSF glucose.
It’s important to note that simply finding elevated CSF glucose isn’t usually clinically significant on its own. The focus should be on the serum glucose level.
Q 18. What are the common causes of decreased glucose levels in CSF?
Decreased glucose levels in CSF, or hypoglycorrhachia, are a significant finding, often indicating increased glucose utilization by pathogens or inflammatory processes within the central nervous system (CNS). Imagine glucose as fuel for the brain; if it’s being consumed rapidly, something is amiss.
- Bacterial Meningitis: Bacteria actively consume glucose for their metabolic needs, leading to significant hypoglycorrhachia.
- Fungal Meningitis: Similar to bacterial meningitis, fungi can also consume glucose in the CNS.
- Tuberculous Meningitis: This infection is notorious for causing low glucose levels in the CSF.
- Malignant Meningitis: Cancer cells can also consume glucose within the CNS.
Hypoglycorrhachia is a crucial indicator that needs prompt investigation and treatment.
Q 19. How do you interpret the presence of blood in CSF?
The presence of blood in CSF, or bloody tap, requires careful interpretation to distinguish between traumatic tap and subarachnoid hemorrhage (SAH). A traumatic tap is caused by accidental puncture of a blood vessel during the lumbar puncture procedure itself, while SAH involves bleeding into the subarachnoid space.
Differentiating between a traumatic tap and SAH:
- Centrifugation: A traumatic tap will show blood evenly distributed across all tubes collected during the procedure, with the supernatant (the fluid after spinning) remaining clear. In SAH, the supernatant will be xanthochromic (yellow-tinged).
- Macroscopic Appearance: In a traumatic tap, the blood decreases in concentration in subsequent tubes.
- Clinical Context: History of trauma or surgery, along with the overall patient picture, aids in diagnosis. For example, severe headache, sudden onset of symptoms, are more consistent with SAH.
It’s crucial to differentiate between these two scenarios, as failure to do so can lead to delayed diagnosis of a life-threatening condition like SAH.
Q 20. What are the common causes of xanthochromia in CSF?
Xanthochromia refers to the yellow discoloration of the CSF supernatant after centrifugation. This is caused by the breakdown of hemoglobin in red blood cells into bilirubin. Think of it as a discoloration signifying an older hemorrhage.
- Subarachnoid Hemorrhage (SAH): This is the most common cause; blood in the subarachnoid space breaks down over time, releasing bilirubin which stains the CSF yellow.
- Previous Hemorrhage: Even after a significant amount of time following an initial hemorrhage, xanthochromia can persist.
- Increased Bilirubin Levels (Jaundice): In cases of severe jaundice, high levels of bilirubin can seep into the CSF.
- Carotenemia: A rare condition involving high levels of carotenoids (found in carrots and other yellow/orange pigments) in the blood can cause xanthochromia.
Xanthochromia is a critical finding, often indicating past bleeding within the CNS.
Q 21. Explain the significance of finding oligoclonal bands in CSF.
Oligoclonal bands in CSF are restricted bands of immunoglobulins (antibodies) detected by electrophoresis. They are a hallmark of immune system activity within the CNS. These bands are mostly IgG, but IgM and IgA can also be seen. The presence of these bands does not indicate specific disease but rather an indication of a process occurring in the CNS.
- Multiple Sclerosis (MS): The presence of oligoclonal bands in the CSF is highly suggestive of MS. They indicate the presence of intrathecal immunoglobulin synthesis, meaning antibody production within the central nervous system. However, it is not specific to MS and can be seen in other diseases.
- Other Inflammatory Neurological Diseases: Oligoclonal bands can also be found in other inflammatory conditions such as neurosarcoidosis, viral encephalitis, and certain types of meningitis. They represent generalized immune response.
- Neurological Infections: Some neurological infections can also cause the appearance of oligoclonal bands. It is vital to consider the clinical context to interpret the presence of oligoclonal bands.
The presence of oligoclonal bands, combined with other clinical findings and diagnostic tests, assists in the diagnosis of a wide variety of neurological conditions.
Q 22. How do you manage a patient experiencing a spinal fluid leak after a lumbar puncture?
Managing a spinal fluid leak after a lumbar puncture is crucial to prevent complications. A leak occurs when the needle punctures the dura mater, allowing cerebrospinal fluid (CSF) to escape. The severity varies; some leaks resolve spontaneously, while others require intervention.
Initial Management: The first step involves close monitoring of the patient for signs of headaches (especially positional), neurological deficits, or signs of meningeal irritation (e.g., neck stiffness, photophobia). Bed rest with head elevation is often recommended to reduce CSF pressure and promote healing. Fluid intake should be encouraged to maintain hydration. In less severe cases, these conservative measures might suffice.
Further Interventions: If the leak persists or worsens, more aggressive approaches become necessary. These include:
- Blood Patch: This involves injecting the patient’s own blood into the epidural space at the puncture site. The blood clot seals the dural tear, stopping the leak. This is a commonly effective procedure.
- Epidural Blood Patch Failure: If the blood patch fails or isn’t suitable, other options include surgical repair of the dural defect or placement of a lumbar drain to manage CSF pressure.
Patient Education: Educating the patient about the signs and symptoms of a continued leak and the importance of follow-up is vital. They should be advised to contact their physician immediately if symptoms worsen. Each case is unique, and the management strategy should be tailored to the patient’s specific situation and the severity of the leak.
Q 23. What are the safety precautions to take during a lumbar puncture procedure?
Safety precautions during a lumbar puncture are paramount to minimize risks. The procedure involves inserting a needle into the spinal canal, hence meticulous attention to detail is essential.
- Patient Preparation: A thorough history and physical examination should be conducted to identify contraindications (e.g., increased intracranial pressure, severe thrombocytopenia). The patient should be adequately informed and consent obtained. Positioning is crucial – typically, the patient lies in a lateral recumbent position with their back arched.
- Aseptic Technique: Strict adherence to sterile technique is vital to prevent infection. The puncture site is thoroughly cleaned and disinfected.
- Needle Insertion: The needle is inserted carefully and slowly, with aspiration at intervals to confirm placement within the subarachnoid space. Constant monitoring for signs of discomfort and complications is necessary.
- Post-Procedure Monitoring: After the procedure, the puncture site should be monitored for bleeding or other complications. The patient should be observed for signs of headache, dizziness, or neurological changes. Adequate post-procedure instructions should be provided, such as instructions for proper rest.
- Emergency Preparedness: Having emergency equipment readily available is critical. This includes resuscitation equipment and medications to manage potential complications, such as hypotension or seizures.
These safety measures help ensure patient safety and reduce the risk of complications, including infection, bleeding, and neurological damage.
Q 24. How do you address patient anxiety before a lumbar puncture?
Addressing patient anxiety before a lumbar puncture is critical for a successful procedure. Many patients experience apprehension due to the perceived invasiveness of the procedure.
Communication is Key: A calm, empathetic approach is essential. Explain the procedure clearly, using simple, non-medical language. Answer any questions the patient may have honestly and patiently. It’s important to address specific concerns such as the potential for pain, bleeding, or infection.
Pain Management: Administering appropriate analgesia or anxiolytics can significantly reduce anxiety and pain during the procedure. A local anesthetic is typically used at the puncture site. For particularly anxious individuals, pre-procedural medication might be considered.
Distraction Techniques: Offer distraction techniques to shift the patient’s focus away from the procedure. This might include playing soothing music, engaging in conversation, or providing support to help manage expectations.
Reassurance: Reassure the patient that the procedure is relatively safe and that you will be monitoring them closely for any complications. Share success stories or positive experiences to bolster their confidence.
By addressing these factors, you contribute to a more positive and comfortable experience for the patient, minimizing their stress and facilitating a smooth procedure.
Q 25. What are the differences between a traumatic tap and intracranial hemorrhage?
Differentiating between a traumatic tap and an intracranial hemorrhage is crucial for accurate diagnosis and appropriate management. Both can present with bloody CSF during a lumbar puncture, but they have distinct mechanisms and clinical implications.
Traumatic Tap: A traumatic tap occurs when the needle inadvertently punctures a blood vessel during the lumbar puncture. The CSF sample will typically have blood that is disproportionately more concentrated in the initial fraction of CSF, clearing over the course of the sampling process. There are usually no other clinical signs or symptoms of intracranial hemorrhage.
Intracranial Hemorrhage: This involves bleeding within the brain or surrounding spaces (subarachnoid, subdural, or epidural). It’s a much more serious condition and the CSF is usually uniformly bloody throughout the collection. The patient typically presents with severe headaches, altered mental status, neurological deficits, or other signs related to the location and extent of the bleed.
Key Differences Summarized:
- Blood distribution in CSF: Traumatic tap – blood concentrated in initial sample; Intracranial hemorrhage – blood evenly distributed throughout sample.
- Clinical presentation: Traumatic tap – usually asymptomatic; Intracranial hemorrhage – severe headaches, neurological deficits, altered mental status.
- Imaging: CT or MRI scan is usually needed for intracranial hemorrhage to confirm the diagnosis and assess the extent of the bleed.
If bloody CSF is obtained, additional investigations (including imaging) are vital to determine the cause.
Q 26. How do you differentiate between a subarachnoid hemorrhage and a traumatic tap?
Differentiating between a subarachnoid hemorrhage (SAH) and a traumatic tap is critical. Both can yield bloody cerebrospinal fluid (CSF), making initial diagnosis challenging.
Subarachnoid Hemorrhage: SAH is bleeding into the subarachnoid space, often caused by a ruptured aneurysm or head trauma. CSF will show xanthochromia (yellowing) within a few hours due to the breakdown of hemoglobin. The patient typically presents with a sudden, severe headache (‘thunderclap headache’), neck stiffness (meningismus), and potentially altered mental status or neurological deficits.
Traumatic Tap: A traumatic tap is an accidental puncture of a vessel during the LP procedure. The blood concentration in the CSF will gradually decrease with sequential collection tubes. Clinically, the patient doesn’t usually have symptoms beyond those possibly associated with the LP itself.
Key Distinguishing Features:
- Xanthochromia: Present in SAH, usually absent in traumatic tap.
- Blood distribution in CSF: Evenly distributed in SAH; decreases in successive tubes in a traumatic tap.
- Clinical presentation: Severe headache, neck stiffness, and neurological deficits in SAH; usually absent in traumatic tap.
- Additional Testing: CT scan or MRI is crucial for definitively diagnosing SAH and assessing its extent.
A repeat lumbar puncture is sometimes performed after a few hours to check for xanthochromia, which helps differentiate between these two conditions.
Q 27. What are the limitations of a lumbar puncture?
Lumbar puncture, while a valuable diagnostic tool, has certain limitations. Understanding these limitations helps avoid misinterpretations and ensures appropriate patient management.
- Inability to Diagnose Certain Conditions: A lumbar puncture cannot definitively diagnose all neurological conditions. For instance, it may not always detect early stages of some neurological diseases or subtle central nervous system infections. It may be unable to identify infections localized to certain regions.
- Risk of Complications: As with any invasive procedure, there are risks associated with lumbar puncture, including bleeding, infection, headache, and nerve damage. These risks should be weighed against the potential diagnostic benefits.
- Contraindications: Certain conditions make lumbar puncture contraindicated, such as increased intracranial pressure (ICP), severe coagulopathy, and skin infections at the puncture site. In such cases, alternative diagnostic methods must be considered.
- False-Negative Results: In some cases, the results of a lumbar puncture may be falsely negative due to factors like timing of the procedure relative to disease progression or inadequate sampling technique.
- Patient-Specific Factors: Patient factors such as obesity, spinal stenosis, or previous spinal surgery can make the procedure more difficult to perform or may increase the risk of complications.
It is important to interpret lumbar puncture results in conjunction with other clinical findings, imaging studies, and laboratory data to reach a comprehensive diagnosis.
Q 28. Describe a situation where you had to modify the lumbar puncture procedure due to unexpected circumstances.
I once encountered a situation where I had to modify the lumbar puncture procedure due to unexpected circumstances. A patient presented for lumbar puncture to investigate suspected meningitis, but during the procedure, I encountered significant resistance upon needle insertion. The initial attempt at the standard L3-L4 interspace was unsuccessful.
Modifying the Procedure: Suspecting possible spinal stenosis or anatomical variation, I cautiously attempted the L4-L5 interspace instead, which also proved difficult. After careful palpation and reevaluation of the patient’s anatomy, I decided to try the L5-S1 interspace. Using a smaller gauge needle, and ensuring optimal patient positioning, I finally obtained a successful puncture in the L5-S1 interspace and successfully collected the CSF sample.
Importance of Flexibility: This experience highlighted the importance of being flexible and adaptable during a lumbar puncture procedure. Knowing when to deviate from the standard approach, based on clinical judgment and patient-specific factors, is crucial. The use of a smaller gauge needle minimized the trauma and the risk of complications. Post-procedure, I carefully monitored the patient for any complications due to the multiple attempts.
Lessons Learned: This experience reinforced the importance of thorough patient assessment, careful technique, and the ability to adapt the procedure to individual anatomical variations.
Key Topics to Learn for Diagnostic Lumbar Puncture Interview
- Anatomy and Physiology: Thorough understanding of the lumbar spine, spinal cord, meninges, and cerebrospinal fluid (CSF) pathways. Consider the variations in anatomy and their impact on the procedure.
- Indications and Contraindications: Master the criteria for ordering a lumbar puncture, including neurological symptoms suggestive of infectious, inflammatory, or neoplastic processes. Understand absolute and relative contraindications and how to assess patient suitability.
- Procedure Technique: Detailed knowledge of the steps involved, from patient positioning and preparation to needle insertion, CSF collection, and post-procedure care. Practice visualizing the procedure and anticipate potential complications.
- Complications and Management: Be prepared to discuss potential complications such as headache, bleeding, infection, and nerve damage. Know the preventative measures and management strategies for each complication.
- CSF Analysis: Understand the interpretation of CSF findings, including cell count, protein levels, glucose levels, and microbiology results. Be able to correlate these findings with different neurological conditions.
- Alternative Diagnostic Techniques: Familiarize yourself with alternative diagnostic methods used to evaluate similar conditions, enabling you to discuss the relative advantages and disadvantages of each approach compared to lumbar puncture.
- Ethical and Legal Considerations: Understand the informed consent process, patient rights, and potential legal implications related to the procedure.
Next Steps
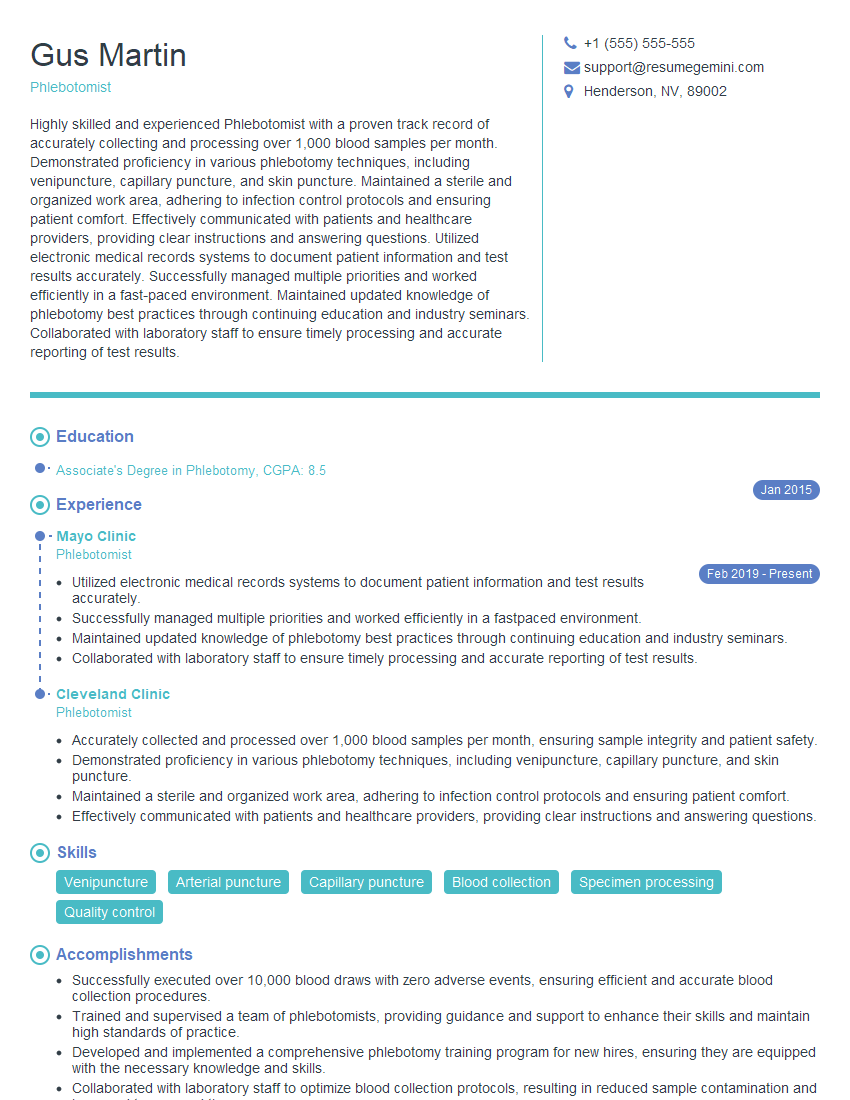
Mastering Diagnostic Lumbar Puncture demonstrates a high level of skill and expertise, significantly enhancing your career prospects in neurology, neurosurgery, and related fields. A strong, ATS-friendly resume is crucial for showcasing your qualifications effectively to potential employers. To create a professional resume that highlights your achievements and skills, we recommend using ResumeGemini. ResumeGemini offers a streamlined process and provides examples of resumes tailored to Diagnostic Lumbar Puncture to help you craft a compelling application.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
To the interviewgemini.com Webmaster.
Very helpful and content specific questions to help prepare me for my interview!
Thank you
To the interviewgemini.com Webmaster.
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.