Feeling uncertain about what to expect in your upcoming interview? We’ve got you covered! This blog highlights the most important Neuropsychiatric Disorders interview questions and provides actionable advice to help you stand out as the ideal candidate. Let’s pave the way for your success.
Questions Asked in Neuropsychiatric Disorders Interview
Q 1. Describe the diagnostic criteria for schizophrenia according to DSM-5.
The DSM-5 diagnostic criteria for Schizophrenia require the presence of at least two of the following symptoms for a significant portion of time during a 1-month period, with at least one being from the first three (delusions, hallucinations, disorganized speech):
- Delusions: Fixed, false beliefs that are not based in reality. For example, believing one is being controlled by external forces or that they have special powers.
- Hallucinations: Sensory perceptions that occur without an external stimulus. These can be auditory (hearing voices), visual (seeing things), tactile (feeling things), olfactory (smelling things), or gustatory (tasting things). A common example is hearing voices that are critical or give commands.
- Disorganized speech: This can manifest as loose associations (jumping from one topic to another unrelated one), tangentiality (going off on tangents), incoherence (speech that is difficult to understand), or neologisms (making up new words).
- Grossly disorganized or abnormal motor behavior: This includes behaviors ranging from childlike silliness to unpredictable agitation. Catatonia, a marked decrease in reactivity to the environment, is also included.
- Negative symptoms: These represent a diminution or absence of normal behaviors and include flat affect (reduced emotional expression), alogia (poverty of speech), avolition (lack of motivation), and anhedonia (inability to experience pleasure).
In addition to these active symptoms, significant social or occupational dysfunction must be present for a considerable duration. The disturbance must not be attributable to another medical condition or substance use. The symptoms must also persist for at least six months, with at least one month of active-phase symptoms. A thorough clinical assessment, including a detailed history and examination, is crucial for accurate diagnosis and to rule out other possible conditions.
Q 2. Differentiate between Bipolar I and Bipolar II disorder.
Bipolar I and Bipolar II disorders are both characterized by episodes of mood elevation (mania) and depression, but they differ significantly in the severity and duration of these episodes:
- Bipolar I Disorder: Defined by at least one manic episode. A manic episode is a distinct period of abnormally and persistently elevated, expansive, or irritable mood, lasting at least one week (or any duration if hospitalization is necessary). During this period, individuals experience symptoms such as inflated self-esteem, decreased need for sleep, racing thoughts, increased goal-directed activity, and risky behavior. Major depressive episodes are often present but not required for diagnosis. Think of it as the more severe form, where full-blown manic episodes are a defining feature.
- Bipolar II Disorder: Defined by at least one hypomanic episode and at least one major depressive episode. Hypomania is similar to mania but less severe; symptoms are not severe enough to cause marked impairment in social or occupational functioning or to necessitate hospitalization. The depressive episodes are typically longer-lasting and more prominent than the hypomanic periods. Imagine this as a less intense, but still significantly debilitating, variation.
A key difference is the severity of the mood episodes. Manic episodes in Bipolar I are significantly more disruptive than hypomanic episodes in Bipolar II. Proper diagnosis requires careful assessment of mood episode characteristics and duration, taking into account the individual’s functional impairment.
Q 3. Explain the neurobiological basis of depression.
The neurobiological basis of depression is complex and multifactorial, involving interactions between genetic, environmental, and neurochemical factors. No single cause exists. However, several key neurobiological mechanisms are implicated:
- Neurotransmitter imbalances: Reduced levels of serotonin, norepinephrine, and dopamine in specific brain regions are frequently observed in individuals with depression. These neurotransmitters play crucial roles in mood regulation, motivation, and reward processing.
- Brain structure and function: Studies have shown structural and functional abnormalities in various brain regions, including the hippocampus, amygdala, and prefrontal cortex. These areas are involved in emotion regulation, memory, and cognitive function. For instance, hippocampal volume reduction is commonly seen.
- Neuroendocrine system dysfunction: The hypothalamic-pituitary-adrenal (HPA) axis, responsible for the stress response, often exhibits dysregulation in depression. This leads to increased cortisol levels, which can have negative effects on the brain over time.
- Inflammation: Emerging evidence suggests a role for inflammation in depression. Increased levels of inflammatory markers have been linked to the development and severity of depressive symptoms.
- Genetics: Family and twin studies indicate a strong genetic component to depression, suggesting that certain genes may increase susceptibility to the disorder. However, genetic predisposition does not equal certainty of development.
It’s important to note that these factors interact in complex ways, and the specific neurobiological mechanisms vary depending on individual characteristics and the type of depression.
Q 4. What are the common side effects of first-generation antipsychotics?
First-generation antipsychotics (FGAs), also known as typical antipsychotics, can cause a range of side effects, some of which can be severe. These are often categorized into extrapyramidal symptoms (EPS) and other metabolic effects:
- Extrapyramidal Symptoms (EPS): These are movement disorders caused by the blockage of dopamine receptors in the basal ganglia. Common EPS include:
- Acute dystonia: Sudden, involuntary muscle contractions, often involving the neck, face, or eyes.
- Parkinsonism: Symptoms resembling Parkinson’s disease, including tremor, rigidity, bradykinesia (slow movement), and postural instability.
- Akathisia: A feeling of inner restlessness and inability to sit still.
- Tardive dyskinesia (TD): A potentially irreversible movement disorder characterized by involuntary repetitive movements, typically of the face, mouth, and tongue. This is a serious late-onset side effect.
- Other Side Effects:
- Anticholinergic effects: Dry mouth, blurred vision, constipation, urinary retention.
- Sedation: Drowsiness and fatigue.
- Weight gain: Significant weight gain can occur, increasing the risk of metabolic syndrome.
- Cardiovascular effects: Changes in heart rate and blood pressure.
- Neuroleptic malignant syndrome (NMS): A rare but life-threatening condition characterized by high fever, muscle rigidity, altered mental status, and autonomic instability.
The risk and severity of side effects vary depending on the individual, the specific FGA used, and the dose. Careful monitoring and management of these side effects are essential during treatment with FGAs.
Q 5. Discuss the efficacy and limitations of cognitive behavioral therapy (CBT) in treating anxiety disorders.
Cognitive Behavioral Therapy (CBT) is a widely used and effective treatment for anxiety disorders. It helps individuals identify and change negative thought patterns and behaviors that contribute to their anxiety.
- Efficacy: CBT has demonstrated significant efficacy in reducing anxiety symptoms across various anxiety disorders, including generalized anxiety disorder, panic disorder, social anxiety disorder, and obsessive-compulsive disorder. Numerous studies show that CBT is often as effective as, or even more effective than, medication in the long term, especially in preventing relapse.
- Limitations: While generally effective, CBT is not a one-size-fits-all solution. Some individuals may find it challenging to engage in the required self-monitoring and cognitive restructuring exercises. The therapy can be time-consuming, requiring multiple sessions over several weeks or months. Moreover, the effectiveness of CBT may vary depending on the therapist’s expertise, the client’s motivation, and the severity of the anxiety. Some individuals might also benefit from a combination of CBT and medication.
Example: In treating social anxiety, CBT might involve identifying negative automatic thoughts (e.g., “Everyone will judge me”) during social situations, challenging the validity of those thoughts, and developing coping strategies (e.g., relaxation techniques, behavioral experiments) to manage anxiety responses. The process often involves gradual exposure to feared social situations to reduce avoidance behaviors. CBT’s success hinges on active patient participation and a collaborative therapeutic relationship.
Q 6. How would you assess a patient presenting with symptoms of dementia?
Assessing a patient presenting with symptoms of dementia requires a multi-faceted approach, combining several assessment tools and techniques. The goal is to identify the type of dementia, assess its severity, and evaluate the patient’s functional abilities and support needs.
- Detailed history: Gathering information about the patient’s medical history, family history of dementia, current medications, and the onset and progression of cognitive symptoms is crucial. This includes interviewing the patient and their family members or caregivers.
- Neurological examination: This involves assessing reflexes, cranial nerve function, motor skills, and sensory function. It helps rule out other neurological conditions.
- Cognitive assessment: Several standardized tests are used to assess various cognitive domains, including memory, attention, language, and executive function. Common examples include the Mini-Mental State Examination (MMSE) and Montreal Cognitive Assessment (MoCA). These tests provide a quantifiable measure of cognitive impairment.
- Functional assessment: Evaluating the patient’s ability to perform activities of daily living (ADLs), such as bathing, dressing, eating, and toileting, is essential to determine their level of independence and support needs.
- Neuroimaging: Brain imaging techniques, such as MRI and CT scans, help visualize brain structure and rule out other potential causes of cognitive decline. Specific imaging findings can often help distinguish between different types of dementia.
- Laboratory tests: Blood tests may be used to rule out other medical conditions that can mimic dementia, such as thyroid disorders, vitamin deficiencies, and infections.
A comprehensive assessment is crucial to reach an accurate diagnosis, guide treatment, and plan for appropriate care and support. It is a collaborative process involving clinicians, the patient, and their family or caregivers.
Q 7. What are the different types of dementia, and how do they differ in presentation and prognosis?
Several types of dementia exist, each with a distinct underlying cause, clinical presentation, and prognosis:
- Alzheimer’s Disease: The most common type, characterized by progressive cognitive decline, including memory loss, language problems, and impaired judgment. It involves the buildup of amyloid plaques and neurofibrillary tangles in the brain. Prognosis is variable but generally involves progressive decline in function, with a life expectancy of several years after diagnosis.
- Vascular Dementia: Caused by reduced blood flow to the brain, often due to stroke or other vascular events. Symptoms can vary depending on the location and extent of brain damage. The progression is often stepwise, with periods of relative stability followed by sudden declines in function. Prognosis is variable and depends on the severity and extent of vascular damage.
- Lewy Body Dementia: Characterized by the presence of Lewy bodies, abnormal protein deposits in brain cells. Common symptoms include fluctuations in cognition, visual hallucinations, Parkinsonism (movement disorders), and falls. The progression is often rapid, with significant cognitive and functional decline.
- Frontotemporal Dementia (FTD): A group of disorders affecting the frontal and temporal lobes of the brain. Symptoms often include personality changes, behavioral problems, language difficulties, and impaired executive function. The prognosis is usually poor, with rapid progression and a shorter life expectancy compared to Alzheimer’s disease.
- Mixed Dementia: Individuals may have a combination of different types of dementia, such as Alzheimer’s disease and vascular dementia. This makes diagnosis and management more complex.
The differentiation between these dementias relies on detailed history, neurological examination, cognitive assessment, neuroimaging, and potentially genetic testing. Each type has a unique presentation and trajectory, influencing the treatment approach and prognosis.
Q 8. Describe your approach to managing a patient with treatment-resistant depression.
Managing treatment-resistant depression (TRD) requires a multifaceted approach, acknowledging that what works for one patient may not work for another. It’s a process of iterative refinement, carefully considering the patient’s unique circumstances and response to previous treatments.
My approach begins with a thorough reassessment. This includes reviewing the patient’s complete history: all past diagnoses, treatments (including dosages and duration), response to those treatments, any co-occurring conditions (comorbidities), and their current psychosocial situation. We explore potential contributing factors such as adherence issues, substance use, or undiagnosed medical conditions.
- Augmentation Strategies: If the patient is already on an antidepressant, I’d consider adding a second medication, such as a mood stabilizer (like lithium or lamotrigine), an atypical antipsychotic (like quetiapine or olanzapine), or a thyroid hormone supplement (if hypothyroidism is suspected).
- Switching Antidepressants: If augmentation fails, I’d consider switching to a different class of antidepressant. For example, if they haven’t responded to an SSRI, we might try an SNRI, a tricyclic antidepressant (TCA – cautiously, due to side effects), or a MAOI (also cautiously, due to dietary restrictions).
- Treatment Resistance and its causes: Treatment resistance can stem from various factors, including inaccurate diagnosis, inadequate treatment duration, comorbid conditions, medication interactions or side effects, patient non-adherence, or genetic factors. A thorough investigation is crucial.
- Beyond Medication: Psychotherapy, particularly Cognitive Behavioral Therapy (CBT) and Interpersonal Therapy (IPT), plays a vital role. These therapies help patients identify and modify negative thought patterns and improve coping mechanisms. Other adjunctive therapies might include Transcranial Magnetic Stimulation (TMS) or electroconvulsive therapy (ECT), both used when other options have failed.
- Regular Monitoring: Close monitoring of the patient’s response to treatment is essential, including regular assessments of mood, suicidal ideation, and side effects. Adjustments are often made based on these assessments.
Ultimately, managing TRD is a collaborative effort between the psychiatrist, the patient, and their support system, aiming for a personalized and effective treatment strategy.
Q 9. Explain the ethical considerations surrounding involuntary commitment.
Involuntary commitment, also known as civil commitment, raises significant ethical concerns centered on individual autonomy and the balance between protecting the individual and society. The fundamental ethical principle at stake is the right to liberty.
The ethical considerations include:
- Least Restrictive Environment: The principle of least restrictive environment mandates that individuals should receive treatment in the setting that imposes the fewest limitations on their freedom. Involuntary commitment should only be considered when less restrictive options, such as outpatient treatment or voluntary hospitalization, have been exhausted or are deemed inadequate to protect the individual or others.
- Due Process: Individuals facing involuntary commitment have a right to due process, including a fair hearing before a judge or other impartial authority. This ensures that the decision to commit is based on evidence and not on prejudice or discrimination.
- Informed Consent: Even in cases of involuntary commitment, efforts should be made to obtain the individual’s informed consent for treatment whenever possible. This involves explaining the risks and benefits of treatment in a way that the individual can understand, while acknowledging their limited capacity due to the condition.
- Confidentiality: Maintaining patient confidentiality remains crucial, even in cases of involuntary commitment, respecting the limits imposed by the legal mandate and necessity for treatment.
- Stigma: The stigma associated with involuntary commitment can have devastating long-term consequences on the individual’s life, career, and relationships. This must be taken into careful consideration.
In practice, involuntary commitment decisions should be made judiciously and only when there’s clear and imminent danger to the individual or others. A multidisciplinary approach involving psychiatrists, legal professionals, and social workers is essential to ensure ethical and legal compliance.
Q 10. What are the key risk factors for suicide?
Suicide is a complex issue with multiple interacting risk factors. It’s not simply one thing, but rather a confluence of factors that increase vulnerability.
Key risk factors can be broadly categorized as:
- Mental Health Disorders: Depression, bipolar disorder, schizophrenia, anxiety disorders, and personality disorders significantly increase suicide risk. Untreated or poorly managed mental health conditions are a major contributor.
- Substance Use Disorders: Alcohol and drug abuse impair judgment and increase impulsivity, heightening suicide risk. The combination of substance abuse and mental illness is particularly dangerous.
- Previous Suicide Attempts: A prior suicide attempt is a powerful predictor of future attempts. This underscores the urgency of comprehensive follow-up care.
- Hopelessness and Despair: A pervasive sense of hopelessness and lack of perceived control over one’s life are strong indicators of elevated suicide risk.
- Family History of Suicide: A family history of suicide increases an individual’s risk, suggesting a possible genetic or environmental influence.
- Access to Lethal Means: Easy access to firearms, medications, or other lethal means significantly increases the likelihood of a successful suicide attempt.
- Social Isolation: Lack of social support and feelings of loneliness and isolation are strong risk factors.
- Life Stressors: Major life events, such as job loss, relationship breakdown, financial difficulties, or legal trouble, can significantly increase vulnerability.
- Chronic Pain: Patients with chronic pain have increased risk due to the impact on their mental and physical well-being.
It is important to note that the presence of risk factors doesn’t automatically predict suicide. A comprehensive assessment is necessary to evaluate the overall risk level for each individual.
Q 11. How would you approach a patient with substance use disorder?
Approaching a patient with a substance use disorder (SUD) requires a compassionate, non-judgmental, and collaborative approach. It’s crucial to understand that SUDs are complex medical conditions, not simply moral failings.
My approach involves:
- Building Rapport and Trust: Establishing a strong therapeutic alliance is paramount. This involves active listening, empathy, and validation of the patient’s experiences. Creating a safe and non-judgmental space is vital.
- Comprehensive Assessment: A thorough assessment includes exploring the type and severity of substance use, duration, patterns of use, the patient’s personal history, social support systems, co-occurring mental health conditions (often present), and medical history.
- Motivational Interviewing: This technique helps to elicit the patient’s intrinsic motivation to change. It emphasizes their personal strengths and goals and focuses on their ambivalence towards change.
- Treatment Planning: Treatment plans are individualized and might include detoxification (if necessary), medication-assisted treatment (MAT) – like methadone for opioid addiction or naltrexone for alcohol dependence – psychotherapy (CBT, contingency management), and support groups (e.g., Alcoholics Anonymous or Narcotics Anonymous).
- Relapse Prevention: Relapse is a common part of the recovery process. Therefore, developing a comprehensive relapse prevention plan, including identifying potential triggers and coping strategies, is essential.
- Addressing Co-occurring Disorders: If co-occurring mental health disorders are present, they need to be addressed simultaneously as part of an integrated treatment plan.
A collaborative approach with other healthcare professionals, such as addiction specialists, social workers, and family therapists, is crucial for comprehensive care.
Q 12. What are the common pharmacological treatments for ADHD?
Pharmacological treatments for Attention-Deficit/Hyperactivity Disorder (ADHD) primarily focus on stimulants and non-stimulants. The choice depends on factors such as the patient’s age, medical history, response to prior treatments, and the presence of co-occurring conditions.
Stimulants:
- Methylphenidate (Ritalin, Concerta, etc.): This is a commonly prescribed stimulant that works by increasing dopamine and norepinephrine levels in the brain, improving focus and attention.
- Amphetamine-based medications (Adderall, Vyvanse, etc.): These also increase dopamine and norepinephrine levels and are often effective in managing ADHD symptoms.
Non-Stimulants: These are often used as an alternative for patients who cannot tolerate stimulants or have contraindications.
- Atomoxetine (Strattera): This non-stimulant norepinephrine reuptake inhibitor improves attention and reduces impulsivity.
- Alpha2-adrenergic agonists (Guanfacine, Clonidine): These medications can be helpful for managing impulsivity and irritability, but may cause sedation.
It’s important to note that these medications should be prescribed and monitored by a qualified healthcare professional. Dosage adjustments are often necessary to find the optimal balance between symptom control and side effects. Regular monitoring for efficacy and side effects, such as appetite suppression, sleep disturbances, and cardiovascular effects, is essential.
Q 13. Describe the neurodevelopmental trajectory of autism spectrum disorder.
The neurodevelopmental trajectory of Autism Spectrum Disorder (ASD) is characterized by early-emerging differences in brain development, though the exact mechanisms are still under investigation. The course is highly variable, making generalizations challenging.
Early Development (Infancy and Toddlerhood): Early signs often include atypical social interaction (reduced eye contact, lack of response to name), communication difficulties (delayed speech or absence of language), and restricted, repetitive behaviors (e.g., lining up toys, repetitive movements).
Childhood and Adolescence: As children grow, diagnostic features may become more apparent. Challenges can persist in social communication and interaction, including difficulties with understanding social cues, making and maintaining friendships, and engaging in reciprocal conversations.
Adulthood: While some individuals experience significant improvement in social communication and adaptive skills, others continue to face persistent challenges throughout adulthood. Support systems are critical for successful adaptation to adult life. Some individuals may achieve independence, while others require ongoing support.
Individual Variability: It’s crucial to remember that the neurodevelopmental trajectory of ASD is highly heterogeneous. The severity of symptoms, areas of strengths and weaknesses, and the rate of development vary considerably from one individual to another. Some individuals may show significant improvements over time, while others may experience more persistent challenges. This underscores the need for personalized support and interventions tailored to the individual’s unique needs.
Ongoing Research: Research continues to shed light on the neurological, genetic, and environmental factors that contribute to ASD’s diverse developmental trajectories. This research offers hope for better interventions and support for individuals across the lifespan.
Q 14. What are the challenges in diagnosing personality disorders?
Diagnosing personality disorders presents significant challenges due to several factors:
- Overlap of Symptoms: The symptoms of different personality disorders often overlap, making differential diagnosis difficult. For instance, a patient might exhibit traits of both borderline and histrionic personality disorders, making a clear distinction challenging.
- Subjectivity in Assessment: Diagnosis relies heavily on subjective clinical judgment based on observations of the patient’s behavior, patterns of thinking, and interpersonal relationships. There’s less reliance on objective biological markers compared to other mental health conditions.
- Comorbidity: Personality disorders frequently co-occur with other mental health disorders, further complicating diagnosis and treatment. Differentiating between the symptoms of the personality disorder and the co-occurring condition can be difficult.
- Lack of Clear Diagnostic Criteria: While the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) provides diagnostic criteria for personality disorders, these criteria are not always precise or easily applicable in clinical practice. The categorical nature of the diagnosis also proves challenging in cases of significant symptom overlap.
- Patient Defensiveness: Patients may be reluctant to acknowledge personality problems, making it difficult to gather a complete and accurate picture of their functioning.
- Cultural Factors: Cultural norms and expectations can influence the presentation and interpretation of personality traits, potentially leading to misdiagnosis or underdiagnosis in certain populations.
Addressing these challenges requires a thorough assessment that goes beyond the structured interviews, using multiple methods (clinical interviews, self-report measures, observational data) across multiple clinical encounters. Clinicians need a strong understanding of personality theory and considerable experience in order to make appropriate and reliable diagnoses.
Q 15. Explain the role of neuroimaging in the diagnosis and treatment of neurological disorders.
Neuroimaging plays a crucial role in both diagnosing and guiding the treatment of neurological disorders. It provides a visual representation of the brain’s structure and function, allowing clinicians to identify abnormalities that may be contributing to a patient’s symptoms. Techniques like Magnetic Resonance Imaging (MRI) and Computed Tomography (CT) scans offer detailed anatomical images, revealing structural damage from trauma, stroke, or tumors. Functional MRI (fMRI) and Positron Emission Tomography (PET) scans show brain activity, helping to identify areas of dysfunction in conditions like epilepsy, Alzheimer’s disease, or Parkinson’s disease.
For example, an MRI might reveal a lesion in the brain consistent with a stroke, while an fMRI could show reduced activity in the hippocampus of a patient with early-stage Alzheimer’s. This information is crucial for diagnosis. Furthermore, neuroimaging can help monitor disease progression and assess the effectiveness of treatment. For instance, a patient undergoing treatment for a brain tumor might have repeated scans to track the tumor’s response to therapy. Ultimately, neuroimaging allows for a more precise and personalized approach to neurological care.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you manage a patient experiencing a severe anxiety attack?
Managing a severe anxiety attack requires a calm and reassuring approach, prioritizing the patient’s safety and comfort. The immediate goal is to help the individual regulate their physiological responses and reduce the intensity of their symptoms. This involves creating a safe and quiet environment, encouraging slow, deep breathing exercises, and using grounding techniques to bring the person back to the present moment. These techniques might involve focusing on their senses (what they see, hear, feel, smell, and taste) or repeating calming phrases.
If the anxiety is severe or prolonged, medication may be necessary. Benzodiazepines, such as alprazolam, can be administered to quickly reduce anxiety symptoms; however, their use is often reserved for acute situations due to the potential for dependence. Throughout the process, validation and empathy are essential. Reassuring the patient that their feelings are valid and that the attack will eventually pass can help reduce their distress. After the attack subsides, it’s crucial to discuss potential triggers and develop coping strategies to prevent future episodes, which might involve therapy like Cognitive Behavioral Therapy (CBT).
Q 17. What are the early warning signs of psychosis?
Early warning signs of psychosis can be subtle and often mistaken for other conditions, making early detection challenging but crucial for intervention. Changes in thinking, perception, and behavior are key indicators. These might include unusual thoughts or beliefs (e.g., believing others are controlling their thoughts), perceptual disturbances like hallucinations (seeing or hearing things that aren’t there), disorganized speech or thought processes, unusual motor behavior (e.g., catatonia), and social withdrawal or isolation. There may also be changes in mood, such as increased anxiety, depression, or irritability.
It’s important to note that not all individuals experiencing these changes will develop psychosis. However, their presence, especially when combined with a family history of psychosis or significant life stress, warrants careful evaluation by a mental health professional. Early intervention can significantly improve outcomes, often involving medication and psychosocial therapies.
Q 18. How would you assess a patient’s risk for self-harm or violence?
Assessing a patient’s risk for self-harm or violence is a critical aspect of mental health care, requiring a comprehensive and multi-faceted approach. It involves a thorough clinical interview, exploring the patient’s current mental state, history of self-harm or violence, access to means (e.g., weapons), and presence of specific risk factors like hopelessness, command hallucinations, or substance abuse. The clinician will need to assess the patient’s level of insight into their condition and their willingness to cooperate with safety plans.
Several validated risk assessment tools are available to assist clinicians in this process. These instruments help structure the assessment and improve consistency in evaluating risk. The clinician must also consider contextual factors, such as the patient’s social support system, housing stability, and access to resources. Based on the assessment, appropriate interventions can be implemented, ranging from increased monitoring and safety planning to hospitalization if the risk is deemed imminent or severe.
Q 19. Discuss the importance of patient confidentiality in the context of mental health care.
Patient confidentiality is paramount in mental health care, forming the cornerstone of the therapeutic relationship and promoting trust. Ethical guidelines and legal regulations, such as HIPAA in the United States, strictly protect the privacy of patient information. This includes all forms of communication, records, and diagnoses. Disclosure of confidential information is only permitted under very limited circumstances, such as when there is a clear and imminent threat to the patient or others (duty to warn), or when mandated by court order.
Maintaining confidentiality is crucial for fostering open communication and ensuring patients feel safe disclosing sensitive information, which is essential for effective treatment. Breaches of confidentiality can severely damage the patient-clinician relationship, leading to mistrust and hindering recovery. Clinicians have a professional obligation to uphold confidentiality and must take appropriate measures to protect patient information.
Q 20. What are some common challenges faced by mental health professionals?
Mental health professionals face numerous challenges, both personal and professional. One significant challenge is the emotional toll of working with individuals experiencing severe mental illness. Compassion fatigue, burnout, and secondary trauma are common occurrences. The demanding nature of the work, combined with often limited resources and high caseloads, can lead to stress and frustration. Another significant challenge is navigating the complexities of the healthcare system, including insurance reimbursement issues, access to care disparities, and the stigma associated with mental illness.
Furthermore, mental health professionals often face ethical dilemmas, such as balancing patient autonomy with their safety. Keeping up-to-date with research and best practices in a rapidly evolving field also poses a challenge. Finally, the lack of adequate funding and support for mental health services is a persistent and widespread concern, impacting the quality of care available to patients.
Q 21. Explain the concept of differential diagnosis in neuropsychiatric disorders.
Differential diagnosis in neuropsychiatric disorders involves systematically comparing and contrasting various possible diagnoses to arrive at the most accurate and comprehensive explanation for a patient’s symptoms. Because many neuropsychiatric disorders share overlapping symptoms, it is crucial to consider multiple possibilities before making a final diagnosis. This process typically involves a thorough clinical interview, a review of the patient’s medical history, neurological examination, and possibly neuropsychological testing or neuroimaging.
For instance, a patient presenting with depression and anxiety could potentially have major depressive disorder, generalized anxiety disorder, or another condition altogether, such as bipolar disorder (depressed phase) or an underlying medical condition. The clinician must systematically assess the symptoms, their duration, severity, and pattern of presentation to differentiate between these possibilities. Accurate differential diagnosis is essential for guiding appropriate and effective treatment. Misdiagnosis can lead to ineffective treatment strategies and potentially worsen the patient’s condition.
Q 22. Describe your experience with various therapeutic interventions.
My experience encompasses a wide range of therapeutic interventions for neuropsychiatric disorders. I’m proficient in evidence-based practices, tailoring my approach to the individual needs of each patient. This includes:
- Pharmacotherapy: I’m adept at prescribing and managing psychotropic medications, carefully monitoring for efficacy and side effects. For example, I’ve successfully managed treatment-resistant depression using a combination of antidepressants and augmentation strategies like adding a mood stabilizer or atypical antipsychotic.
- Psychotherapy: I utilize various therapeutic modalities, including Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), and psychodynamic therapy. I adapt my approach depending on the diagnosis and the patient’s preferences and response to treatment. For instance, I’ve used CBT to help a patient with obsessive-compulsive disorder (OCD) identify and challenge their negative thought patterns and develop coping mechanisms.
- Rehabilitation: I incorporate rehabilitation strategies into treatment plans, focusing on functional recovery and improving the patient’s quality of life. This can involve referrals to occupational therapy, physical therapy, or vocational rehabilitation programs. For a patient recovering from a traumatic brain injury, this might include exercises to improve cognitive function and daily living skills.
- Electroconvulsive Therapy (ECT): I have experience in recommending and monitoring ECT for patients with severe depression or other treatment-resistant conditions, ensuring careful patient education and monitoring for potential side effects. This is always a last resort after other treatment options have been exhausted and involves close collaboration with an anesthesiologist.
I believe in a holistic approach, integrating these interventions as needed to achieve optimal outcomes. Regular monitoring and collaborative discussions with patients are central to my therapeutic process.
Q 23. How do you maintain professional boundaries with patients?
Maintaining professional boundaries is paramount in my practice. I adhere to strict ethical guidelines, prioritizing the patient’s well-being and avoiding any situations that could lead to a conflict of interest or exploitation. This involves:
- Clear communication: I establish clear expectations from the beginning, defining the therapeutic relationship and its limits. This includes outlining the parameters of our sessions, confidentiality, and contact outside of appointments.
- Appropriate self-disclosure: I maintain a professional demeanor, avoiding excessive self-disclosure that could blur the boundaries of the therapeutic relationship. I only share personal information if it’s clinically relevant and serves the patient’s needs.
- Avoiding dual relationships: I avoid engaging in any social, business, or personal relationships with patients, preventing potential conflicts of interest. For instance, I would never accept gifts from a patient or socialize with them outside of the therapeutic setting.
- Seeking supervision: I regularly participate in clinical supervision, engaging in peer review and case discussions to ensure ethical and professional practices.
By consistently upholding these boundaries, I create a safe and effective therapeutic environment that fosters trust and promotes healing.
Q 24. How do you approach a case where there’s disagreement between the patient and family members?
Disagreements between patients and family members are common, particularly in cases involving challenging behaviors or differing opinions about treatment. My approach is to:
- Facilitate open communication: I create a space for open dialogue, encouraging each party to express their concerns and perspectives. I use active listening and reflective statements to validate their feelings.
- Identify underlying issues: I explore the root causes of the conflict, identifying any misunderstandings or unmet needs that may be contributing to the disagreement. Sometimes, family members may have unrealistic expectations about treatment outcomes or the patient’s recovery progress.
- Collaborate on solutions: I work collaboratively with the patient and family members to develop a shared decision-making plan. This may involve compromise, negotiation, or exploring alternative approaches to address everyone’s concerns.
- Set boundaries: While fostering collaboration, I maintain professional boundaries. I clarify my role as the patient’s advocate and ensure the patient’s autonomy is respected. I may need to mediate communication rather than take sides.
- Utilize family therapy: In some cases, family therapy can be helpful in resolving conflicts and improving communication dynamics.
My goal is to build a collaborative therapeutic alliance that respects individual preferences while also fostering a supportive and understanding environment.
Q 25. What are your strengths and weaknesses in dealing with challenging patients?
Strengths: My strengths lie in my empathy, patience, and ability to build rapport with challenging patients. I possess excellent communication skills and can adapt my approach to meet individual needs. I remain calm under pressure and effectively manage difficult situations, such as managing aggression or emotional outbursts.
Weaknesses: I am sometimes overly invested in my patients’ well-being, potentially leading to emotional exhaustion. I’m actively working on maintaining better personal boundaries and utilizing self-care strategies to mitigate this. I am also continuously striving to improve my skills in dealing with patients who exhibit manipulative behavior.
Q 26. Describe your experience working with diverse populations.
I have extensive experience working with diverse populations, including individuals from various cultural, socioeconomic, and ethnic backgrounds. I recognize that cultural factors significantly influence mental health experiences and treatment preferences. My approach involves:
- Cultural sensitivity: I am mindful of cultural nuances and beliefs that may affect treatment engagement and adherence. For example, I tailor my communication style and treatment strategies based on individual cultural backgrounds.
- Linguistic competency: I am proficient in [mention specific languages here], allowing me to effectively communicate with patients who speak those languages. For patients who don’t speak a language I know, I utilize interpreter services.
- Addressing health disparities: I actively work to address healthcare disparities that may disproportionately affect certain populations. This involves considering socioeconomic factors, access to resources, and systemic barriers to care.
- Collaboration with community resources: I collaborate with community organizations and support groups that serve specific populations, enhancing my capacity to provide culturally appropriate care.
I believe in providing equitable and culturally competent care to ensure all individuals have access to high-quality mental health services.
Q 27. How do you stay updated on the latest advancements in neuropsychiatric research?
Staying updated on the latest advancements in neuropsychiatric research is crucial for providing optimal patient care. My strategies include:
- Regularly reviewing scientific literature: I subscribe to relevant journals and online databases (e.g., PubMed, PsycINFO) and actively search for the latest research findings in my areas of interest.
- Attending conferences and workshops: I participate in professional conferences and workshops to learn about the latest research, treatment techniques, and emerging technologies.
- Engaging in continuing medical education (CME): I actively engage in CME activities to maintain my professional license and stay abreast of new developments in the field.
- Networking with colleagues: I regularly network with colleagues and other professionals, exchanging information and perspectives on research and clinical practice.
- Following key researchers and organizations: I follow leading researchers and organizations in neuropsychiatry on social media and through their publications to keep up with the most recent breakthroughs.
By utilizing these strategies, I ensure that my clinical practice is grounded in the most current scientific evidence and best practices.
Q 28. How do you handle stress and burnout in a demanding mental health setting?
The mental health field is inherently demanding, and it’s crucial to implement effective stress management strategies to prevent burnout. My approach includes:
- Maintaining a healthy work-life balance: I prioritize time for personal activities, hobbies, and social connections, recognizing the importance of self-care and downtime.
- Practicing mindfulness and relaxation techniques: I incorporate mindfulness meditation, yoga, or other relaxation techniques into my daily routine to manage stress and improve emotional well-being.
- Seeking support from colleagues and supervisors: I actively engage in peer support groups and maintain open communication with my supervisors to address work-related stress and challenges.
- Utilizing professional supervision: Regular clinical supervision provides an invaluable avenue for processing challenging cases and discussing potential burnout risks.
- Setting realistic expectations: I strive to set realistic expectations for myself and my patients, avoiding overcommitment and prioritizing self-care.
By prioritizing my well-being, I can better support my patients and maintain a sustainable and fulfilling career in mental health.
Key Topics to Learn for Neuropsychiatric Disorders Interview
- Classification and Diagnosis: Understand the DSM-5 criteria for various neuropsychiatric disorders, including differentiating between similar conditions and applying diagnostic reasoning.
- Neurobiology of Neuropsychiatric Disorders: Explore the underlying neurochemical imbalances, structural abnormalities, and genetic factors contributing to conditions like schizophrenia, depression, and anxiety disorders. Consider the role of neurotransmitters and brain regions.
- Assessment and Treatment Modalities: Familiarize yourself with various assessment tools (e.g., clinical interviews, neuropsychological testing) and treatment approaches (e.g., pharmacotherapy, psychotherapy, ECT) for different neuropsychiatric disorders.
- Ethical and Legal Considerations: Understand the ethical implications of diagnosis, treatment, and patient confidentiality, including legal frameworks related to involuntary commitment and informed consent.
- Specific Disorder Knowledge: Deepen your understanding of at least three common neuropsychiatric disorders (e.g., schizophrenia, major depressive disorder, bipolar disorder, obsessive-compulsive disorder, anxiety disorders, PTSD). Focus on their presentation, prognosis, and management.
- Case Conceptualization and Treatment Planning: Practice formulating comprehensive case conceptualizations, integrating biopsychosocial factors, and developing individualized treatment plans for hypothetical scenarios.
- Current Research and Trends: Stay updated on current research findings and emerging treatment approaches in the field of neuropsychiatric disorders. This demonstrates your commitment to professional development.
Next Steps
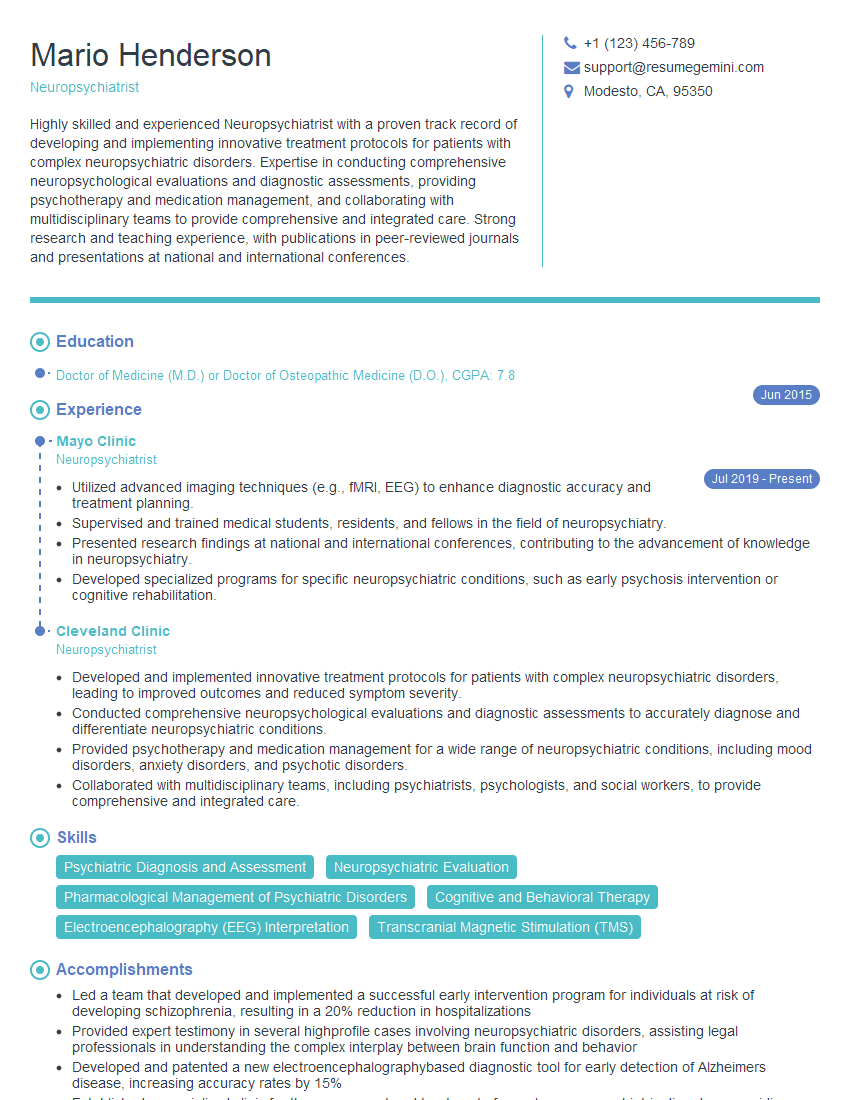
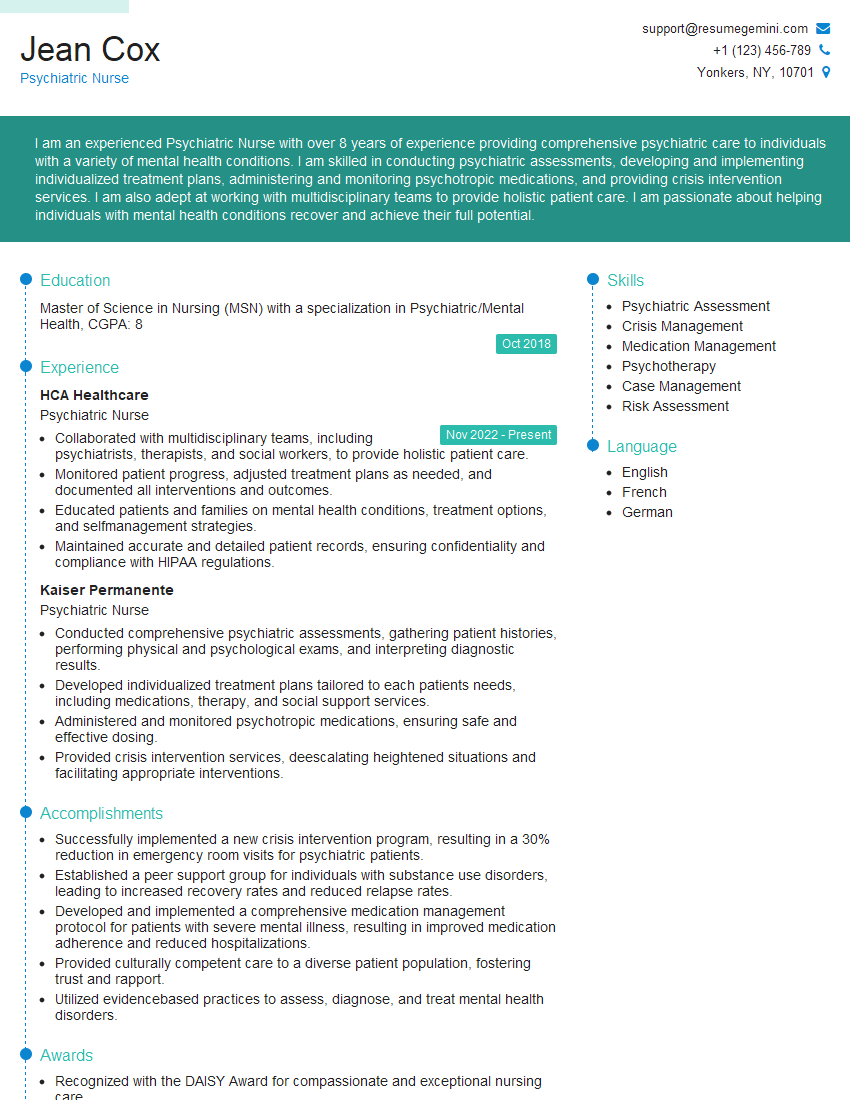
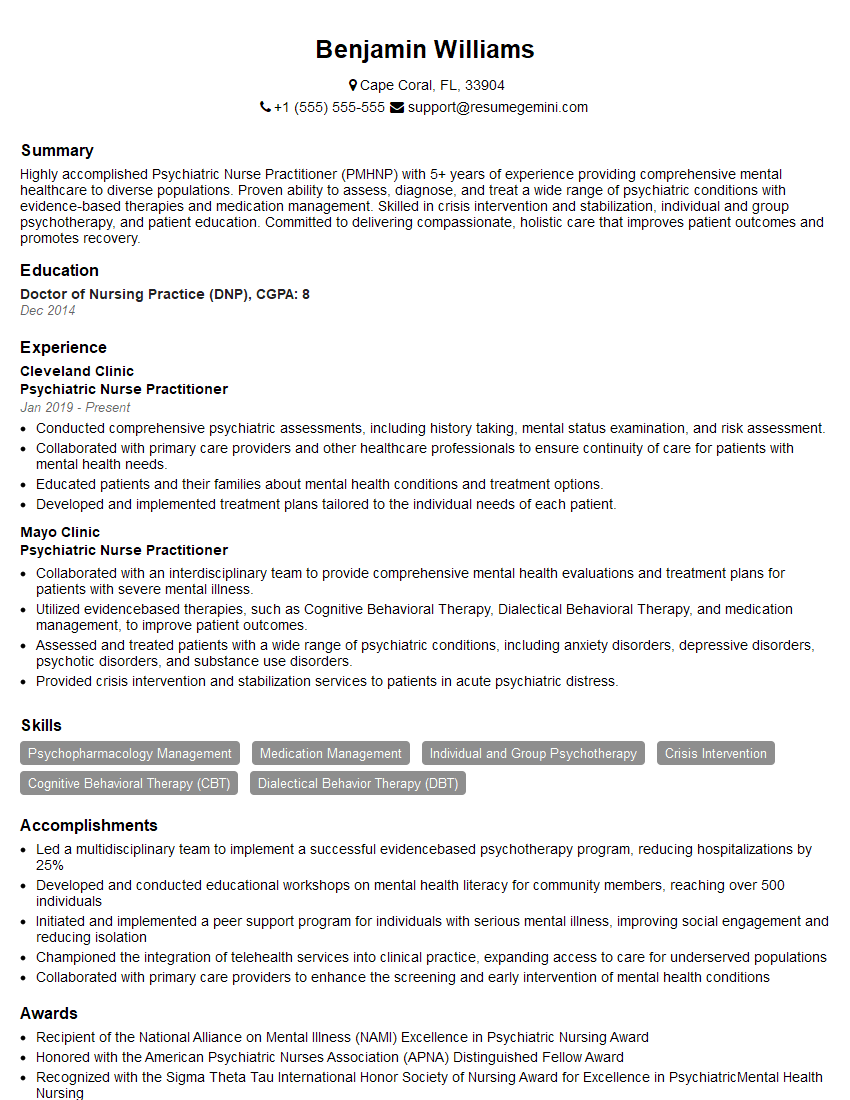
Mastering the complexities of neuropsychiatric disorders is crucial for career advancement in this rapidly evolving field. A strong understanding of these conditions will significantly enhance your clinical skills and open doors to various opportunities. To maximize your job prospects, create an ATS-friendly resume that highlights your skills and experience effectively. ResumeGemini is a trusted resource that can help you build a professional resume tailored to the specific requirements of neuropsychiatric roles. Examples of resumes tailored to Neuropsychiatric Disorders are available within the ResumeGemini platform to help guide your process.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
To the interviewgemini.com Webmaster.
Very helpful and content specific questions to help prepare me for my interview!
Thank you
To the interviewgemini.com Webmaster.
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.