Preparation is the key to success in any interview. In this post, we’ll explore crucial Cognitive Neurology interview questions and equip you with strategies to craft impactful answers. Whether you’re a beginner or a pro, these tips will elevate your preparation.
Questions Asked in Cognitive Neurology Interview
Q 1. Explain the difference between Broca’s and Wernicke’s aphasia.
Broca’s and Wernicke’s aphasias are two distinct types of aphasia, a language disorder caused by brain damage. They are differentiated primarily by the type of language impairment they cause.
Broca’s aphasia, also known as expressive aphasia, results from damage to Broca’s area in the frontal lobe, typically the left hemisphere. Individuals with Broca’s aphasia struggle to produce fluent speech. Their speech is often halting, slow, and grammatically simplified, though they generally understand language relatively well. Think of it as having the right ideas but difficulty expressing them verbally. For example, a patient might say, “Walk… dog… park,” instead of “I walked the dog in the park.”
Wernicke’s aphasia, or receptive aphasia, arises from damage to Wernicke’s area in the temporal lobe, again typically the left hemisphere. Patients with Wernicke’s aphasia can produce fluent speech, but it often lacks meaning or coherence. They struggle with comprehension – understanding spoken or written language. They may use neologisms (made-up words) and have difficulty following instructions. Imagine a sentence like, “The purple cow jumped over the lazy moon and sang a song about the splendiferous gloom.” It sounds fluent but makes little sense.
In essence, Broca’s aphasia affects the production of speech, while Wernicke’s aphasia impacts the comprehension of language. Both highlight the localization of language functions within the brain.
Q 2. Describe the neural pathways involved in memory consolidation.
Memory consolidation is the process by which memories are stabilized and become long-term. It’s not a single event but a complex interplay of brain regions and processes. The hippocampus plays a crucial role, acting as a temporary holding area for new memories. Over time, these memories are transferred to the cortex for long-term storage.
The process typically involves several stages: encoding (initial processing of information), consolidation (stabilization and strengthening of memory traces), and retrieval (accessing stored memories). The hippocampus interacts with the amygdala (emotional processing) and various cortical regions (depending on the type of memory – visual, auditory, etc.).
Imagine it like this: The hippocampus is a librarian, temporarily filing newly acquired books (memories). Over time, the librarian transfers these books to the appropriate shelves in the library (cortex), categorizing them for easier retrieval later. The amygdala tags certain books with emotional significance, making them easier to remember.
Neurochemically, processes like long-term potentiation (LTP) – a strengthening of synaptic connections – are crucial. Sleep also plays a vital role in memory consolidation, allowing for the reorganization and transfer of memories.
Q 3. What are the key diagnostic criteria for Alzheimer’s disease?
Diagnosing Alzheimer’s disease requires a multifaceted approach. There isn’t a single definitive test, but a combination of clinical evaluation, neuropsychological testing, and often neuroimaging.
- Cognitive decline: A gradual decline in cognitive abilities, including memory, thinking, and judgment, significantly impacting daily life is a core criterion.
- Impaired memory: Difficulty remembering recently learned information is usually an early and prominent symptom.
- Other cognitive impairments: Problems with language (aphasia), visual-spatial skills (agnosia), executive function (planning, problem-solving), or praxis (performing learned movements) often develop.
- Gradual onset and progressive worsening: The symptoms typically start subtly and worsen over time.
- Exclusion of other causes: Other conditions that can mimic Alzheimer’s (e.g., depression, vitamin deficiencies, stroke) need to be ruled out.
- Neuroimaging: Brain scans like MRI or PET can show characteristic changes in brain structure and metabolism, supporting the diagnosis. For example, PET scans can show reduced metabolism in certain brain regions.
It’s important to note that a definitive diagnosis often requires observing the progressive nature of the cognitive decline over time.
Q 4. How do you assess executive function in patients?
Assessing executive function involves evaluating a range of higher-order cognitive processes that enable goal-directed behavior. This requires a comprehensive approach using a variety of neuropsychological tests.
- Inhibition: The ability to suppress inappropriate responses. Tests like the Stroop test assess this by asking patients to name the color of ink used to print a word, where the word itself is a different color (e.g., the word “red” printed in blue ink).
- Working memory: The ability to hold and manipulate information in mind. Digit span tasks (repeating sequences of numbers) and complex span tasks assess this ability.
- Cognitive flexibility: The ability to switch between tasks or mental sets. The Wisconsin Card Sorting Test (WCST) measures this by requiring patients to learn and adapt to changing sorting rules.
- Planning and problem-solving: The ability to plan and organize actions to achieve goals. Tower of London or Tower of Hanoi tasks, which involve moving disks to achieve a specific configuration, are frequently used.
Observations during clinical interviews, such as assessing a patient’s ability to organize their thoughts, follow instructions, and engage in complex problem-solving, are also crucial components of the assessment.
Q 5. Explain the role of neuroimaging techniques (e.g., fMRI, EEG) in diagnosing cognitive disorders.
Neuroimaging techniques are invaluable in diagnosing cognitive disorders. They provide objective measures of brain structure and function, complementing clinical and neuropsychological assessments.
fMRI (functional magnetic resonance imaging) measures brain activity by detecting changes in blood flow. It helps identify areas of the brain that are under- or overactive in patients with cognitive disorders. For example, fMRI might reveal reduced activity in the hippocampus in individuals with Alzheimer’s disease.
EEG (electroencephalography) measures electrical activity in the brain using electrodes placed on the scalp. It’s particularly useful for detecting abnormalities in brain rhythms, which can be indicative of certain neurological conditions such as epilepsy or sleep disorders that might impact cognition. Changes in EEG patterns can suggest the presence of encephalopathy.
Other techniques such as CT scans (structural imaging) and PET scans (metabolic imaging) also play important roles. CT scans can identify structural damage like strokes or tumors, while PET scans can visualize metabolic changes in the brain, such as reduced glucose metabolism in Alzheimer’s disease.
Combining neuroimaging findings with clinical and neuropsychological data provides a more comprehensive understanding of the patient’s condition, leading to more accurate diagnoses and treatment planning.
Q 6. Discuss the different types of dementia and their characteristic symptoms.
Dementia is an umbrella term encompassing a range of progressive neurological disorders that affect cognitive function. Several types exist, each with characteristic symptoms.
- Alzheimer’s disease: The most common type, characterized by progressive memory loss, cognitive decline, and behavioral changes. Early symptoms often include memory problems, followed by language difficulties, disorientation, and personality changes.
- Vascular dementia: Caused by damage to blood vessels in the brain, often from strokes or other vascular events. Symptoms can vary depending on the location and extent of the damage, but often include problems with thinking, memory, and judgment.
- Lewy body dementia: Characterized by the presence of abnormal protein deposits (Lewy bodies) in the brain. Symptoms can include fluctuations in cognitive abilities, visual hallucinations, Parkinsonian features (slow movement, rigidity), and sleep disturbances.
- Frontotemporal dementia: Affects the frontal and temporal lobes of the brain. Symptoms often include changes in personality, behavior, language (aphasia), and executive function.
Other less common types of dementia include mixed dementia (a combination of different types), and dementia caused by specific conditions like Creutzfeldt-Jakob disease or Huntington’s disease. Proper diagnosis requires a thorough evaluation by a neurologist or geriatrician.
Q 7. Describe your approach to evaluating a patient with suspected traumatic brain injury.
Evaluating a patient with suspected traumatic brain injury (TBI) requires a systematic approach focusing on both immediate and long-term consequences.
- Initial assessment: This involves evaluating the patient’s level of consciousness (Glasgow Coma Scale), pupillary reflexes, and vital signs. Imaging studies (CT scan) are crucial to identify any intracranial hemorrhages or other structural damage.
- Neurological examination: A thorough assessment of cranial nerves, motor strength, sensory function, reflexes, and coordination is necessary to determine the extent of neurological impairment.
- Cognitive assessment: Neuropsychological testing is used to evaluate cognitive functions like memory, attention, executive functions, and language. This helps identify specific cognitive deficits caused by the injury.
- Behavioral assessment: Assessment for behavioral changes, such as irritability, aggression, or emotional lability, is important as these are common consequences of TBI.
- Long-term follow-up: Patients with TBI require ongoing monitoring for both physical and cognitive recovery. Regular neuropsychological evaluations can track progress and identify potential complications.
The approach is tailored to the severity of the injury and the patient’s individual needs. Collaboration with other healthcare professionals, such as rehabilitation specialists and therapists, is often crucial for optimal management.
Q 8. How do you differentiate between cognitive impairments due to age versus pathology?
Differentiating between age-related cognitive decline and pathological cognitive impairment requires a careful and comprehensive approach. Normal aging involves some gradual slowing of processing speed and minor memory lapses, particularly for recent events. These changes are typically subtle and don’t significantly impact daily functioning. Pathological conditions, on the other hand, demonstrate a more pronounced and rapid decline in cognitive abilities, often affecting multiple domains such as memory, attention, executive function, and language. The decline interferes with daily life and independent functioning.
For example, forgetting where you placed your keys is a common age-related experience. However, repeatedly forgetting the names of close family members or becoming lost in familiar surroundings points towards a possible pathology like Alzheimer’s disease or another dementia. A thorough neuropsychological assessment, including detailed cognitive testing and medical history, is crucial for accurate differentiation. We also look for other indicators, such as the presence of other neurological symptoms (e.g., motor problems, seizures), family history of neurological disorders, and the rate of cognitive decline.
In practice, I use a combination of standardized neuropsychological tests, clinical interviews, and a detailed review of the patient’s medical history to arrive at a differential diagnosis. This multifaceted assessment allows for a more nuanced understanding of the cognitive changes and helps to distinguish normal aging from pathological conditions.
Q 9. What are the ethical considerations in neuropsychological assessment?
Ethical considerations in neuropsychological assessment are paramount. The primary ethical principles revolve around ensuring patient confidentiality, informed consent, and minimizing potential harm. Confidentiality is maintained through secure storage of test results and adherence to HIPAA regulations. Informed consent involves explaining the purpose of the assessment, the procedures involved, potential risks and benefits, and ensuring the patient understands their right to withdraw at any time. This is especially crucial considering the sensitive nature of the information obtained during the assessment.
Another key ethical consideration is competence. I must ensure I possess the necessary training and expertise to administer and interpret the tests accurately. Misinterpreting results can have significant consequences for patients’ lives, affecting treatment plans, employment, and personal relationships. Furthermore, I need to be aware of potential biases, both my own and those inherent in the assessment instruments. Cultural sensitivity is also crucial, ensuring that the chosen tests and methods are appropriate for the patient’s cultural background and linguistic abilities. Finally, I must communicate results in a clear, understandable manner, avoiding technical jargon and offering appropriate support to the patient and their family.
Q 10. Explain the principles of cognitive rehabilitation.
Cognitive rehabilitation is a therapeutic approach aimed at improving cognitive functions following brain injury or neurological disease. Its principles are grounded in the concept of neuroplasticity – the brain’s ability to reorganize and adapt. The goal is to maximize the patient’s ability to participate in their daily activities by compensating for cognitive deficits or improving remaining abilities.
Several key principles guide cognitive rehabilitation. First, it’s highly individualized, tailoring interventions to the specific cognitive deficits and functional limitations of each patient. Second, it emphasizes active participation and engagement from the patient, promoting self-directed learning and problem-solving. Third, it involves a multidisciplinary approach, often including neuropsychologists, occupational therapists, speech-language pathologists, and other healthcare professionals. Finally, the emphasis is on functional outcomes – translating cognitive improvements into tangible benefits in the patient’s daily life. Strategies employed include memory aids, problem-solving training, strategy instruction, and environmental modifications.
For instance, a patient with memory deficits might benefit from using a daily planner, setting reminders, and engaging in memory training exercises. A patient with executive dysfunction might benefit from strategies like breaking down complex tasks into smaller steps and using checklists. Regular follow-up assessments are crucial to track progress, adapt treatment, and ensure the interventions remain relevant and effective.
Q 11. Describe your experience with administering and interpreting neuropsychological tests.
Throughout my career, I have extensive experience in administering and interpreting a wide range of neuropsychological tests. This includes tests assessing various cognitive domains, such as memory (e.g., Wechsler Memory Scale, Rey Auditory Verbal Learning Test), attention (e.g., Trail Making Test, Stroop Test), executive functions (e.g., Wisconsin Card Sorting Test, Tower of London), language (e.g., Boston Naming Test, Token Test), and visuospatial abilities (e.g., Rey-Osterrieth Complex Figure Test, Judgment of Line Orientation).
My approach emphasizes selecting tests appropriate to the patient’s presentation and suspected cognitive deficits. I’m adept at tailoring the assessment to the individual’s abilities and limitations, creating a comfortable and supportive testing environment. I’m proficient in scoring tests according to standardized procedures and interpreting results within the context of the patient’s overall clinical picture. I regularly utilize statistical software and neuropsychological databases to analyze results and compare them to normative data. This allows me to generate comprehensive reports that provide clinicians and patients with a clear understanding of cognitive strengths and weaknesses, as well as potential diagnoses and treatment recommendations.
For example, I recently worked with a patient who exhibited difficulties with verbal fluency and memory. The neuropsychological assessment revealed a pattern consistent with frontotemporal dementia. This allowed for early intervention and support for the patient and their family.
Q 12. How do you manage challenging patient behaviors during cognitive assessments?
Managing challenging patient behaviors during cognitive assessments requires patience, flexibility, and a strong understanding of the underlying causes of the behavior. These behaviors can range from anxiety and frustration to agitation and disinhibition. My approach focuses on creating a safe and supportive testing environment, building rapport with the patient, and adapting the assessment as needed.
Before the assessment begins, I clearly explain the process and address any anxieties the patient might have. I use clear, simple language and offer breaks as needed. If agitation arises, I may adjust the testing schedule, choosing shorter testing sessions or incorporating more frequent breaks. I also might modify the instructions or use alternative methods of assessment. If a patient becomes overly frustrated, I actively empathize and offer reassurance. In cases where the patient’s behavior poses a safety risk, I might consult with colleagues, or postpone the assessment until the situation is better managed, potentially utilizing medication adjustments in consultation with the prescribing physician.
For instance, if a patient becomes easily distracted, I might minimize distractions in the testing room and use strategies to maintain focus. If a patient experiences anxiety, I might use calming techniques such as deep breathing exercises or positive reinforcement. The key is to remain flexible and adapt my approach to the individual needs of each patient.
Q 13. What is your experience with different types of memory tests?
My experience with memory tests encompasses a broad range of instruments targeting different aspects of memory. These include tests of immediate recall (e.g., digit span), short-term memory (e.g., Corsi block-tapping test), long-term memory (e.g., California Verbal Learning Test), visual memory (e.g., Rey Complex Figure Test), and recognition memory (e.g., Benton Visual Retention Test). I’m also experienced in using tests that assess different memory processes, such as encoding, storage, and retrieval.
The choice of tests depends on the clinical question and the patient’s specific presentation. For example, if a patient presents with complaints of forgetfulness, I might use a comprehensive battery of memory tests to assess the different aspects of memory. If the concern is primarily related to verbal learning and memory, I would likely include tests such as the California Verbal Learning Test or the Rey Auditory Verbal Learning Test. If visuospatial memory is a concern, I would incorporate tests like the Rey Complex Figure Test or the Benton Visual Retention Test. The interpretation of memory test results requires careful consideration of multiple factors, including age, education, and the presence of other cognitive impairments.
I utilize a combination of quantitative and qualitative data in interpreting memory test results. Quantitative data includes raw scores, percentiles, and standardized scores, which provide objective measures of memory performance. Qualitative data includes observations of the patient’s testing behavior, such as strategy use, effort, and frustration levels, which add a richer understanding of their cognitive functioning. This comprehensive approach allows me to offer accurate and nuanced interpretations, providing invaluable insights into the patient’s memory abilities.
Q 14. Explain the concept of neuroplasticity and its implications for cognitive rehabilitation.
Neuroplasticity refers to the brain’s remarkable ability to reorganize itself by forming new neural connections throughout life. This capacity is crucial for learning, adaptation, and recovery from brain injury or disease. It’s the foundation of cognitive rehabilitation, allowing us to harness the brain’s inherent ability to change and improve cognitive functions.
The principles of neuroplasticity imply that targeted interventions can stimulate specific brain regions and enhance cognitive performance. Repetitive practice, engaging in challenging activities, and creating a stimulating environment all promote the formation of new neural pathways. Cognitive rehabilitation techniques, such as memory strategies, problem-solving training, and compensatory techniques, capitalize on neuroplasticity by encouraging the brain to adapt and compensate for damaged areas. For example, learning a new language or engaging in mentally stimulating activities like puzzles and brain training games can promote the creation of new neural pathways and strengthen existing ones.
However, the extent of neuroplasticity varies depending on factors such as the age of the individual, the severity and location of the brain injury, and the intensity and type of rehabilitation. While neuroplasticity offers hope for recovery and improvement, it’s essential to manage expectations. Cognitive rehabilitation aims to maximize functional improvement but doesn’t necessarily guarantee a complete restoration of pre-morbid abilities. Ongoing research continues to expand our understanding of neuroplasticity and refine cognitive rehabilitation techniques to enhance their efficacy.
Q 15. Discuss the role of genetics in cognitive disorders.
Genetics plays a significant role in many cognitive disorders. Some disorders, like Huntington’s disease, are caused by a single gene mutation, leading to a predictable and inevitable decline in cognitive function. Others, like Alzheimer’s disease, are far more complex, with multiple genes contributing to increased risk, interacting with environmental factors. Think of it like this: some disorders are like a single faulty switch that turns off a critical cognitive function, while others are like a complex network of wires, with multiple points of failure contributing to the overall dysfunction.
For instance, the APOE ε4 allele is a well-known genetic risk factor for Alzheimer’s disease. Having one copy increases risk, and having two copies significantly increases risk. However, not everyone with this allele develops Alzheimer’s, highlighting the importance of environmental factors and lifestyle choices. Genetic testing can be useful in identifying individuals at higher risk, allowing for earlier interventions and lifestyle modifications. Research is constantly identifying new genes and gene variants associated with different cognitive disorders, paving the way for personalized risk assessment and potential targeted therapies.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
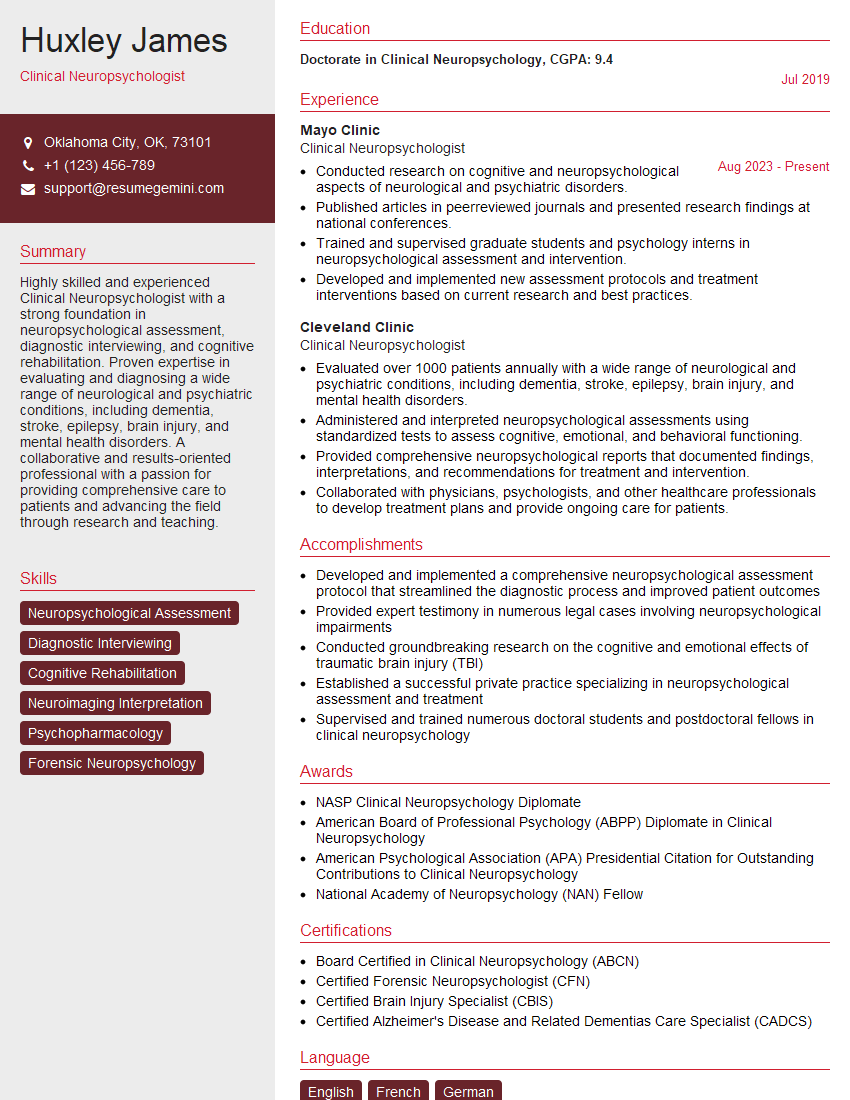
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you incorporate patient and family perspectives into your clinical practice?
Incorporating patient and family perspectives is paramount to effective care. I believe in a collaborative model where the patient and their family are active partners in the diagnostic and treatment process. I begin by actively listening to their concerns, understanding their history of symptoms, and acknowledging the impact the illness has on their daily lives.
For example, I had a patient with suspected dementia whose family initially attributed his memory issues to stress. By engaging in detailed conversations with both the patient and his family, I uncovered additional symptoms that led to a more accurate diagnosis. This collaborative approach fosters trust and improves treatment adherence. I also provide resources and support groups to help families cope with the emotional and logistical challenges of living with a cognitive disorder. Regular check-ins, open communication, and flexibility in appointment scheduling all contribute to a patient-centered approach.
Q 17. Describe your experience with different neuropsychological assessment batteries.
My experience encompasses a wide range of neuropsychological assessment batteries, tailored to the individual’s specific needs and presenting concerns. I routinely utilize comprehensive batteries such as the Halstead-Reitan Neuropsychological Battery, the Luria-Nebraska Neuropsychological Battery, and the Boston Process Approach. These batteries assess various cognitive domains, including attention, memory, executive functions, language, and visuospatial skills.
I also frequently employ shorter, targeted tests, such as the Wechsler Memory Scale, the Trail Making Test, and the Stroop Color-Word Test, depending on the clinical question. The choice of battery is driven by the patient’s symptoms, referral question, and available time. For example, a patient presenting with suspected traumatic brain injury might require a comprehensive battery, while a patient with mild cognitive impairment might benefit from a targeted assessment of memory.
Q 18. What are the limitations of neuropsychological testing?
Neuropsychological testing, while powerful, has limitations. It’s crucial to interpret results cautiously and consider their context. One key limitation is that test performance can be influenced by factors other than neurological damage, such as education level, premorbid intelligence, motivation, and anxiety.
For example, a patient with low education might score lower on a verbal fluency test not due to cognitive impairment but due to limited vocabulary. Another limitation is that tests often assess cognitive abilities in isolation, neglecting the complex interactions between different brain regions. Finally, neuropsychological tests can’t definitively diagnose a specific disease, but rather provide information about cognitive strengths and weaknesses that contribute to the overall clinical picture. Therefore, it’s always integrated with other clinical information, including medical history, neurological examination, and imaging studies.
Q 19. Explain the concept of cognitive reserve and its relevance to clinical practice.
Cognitive reserve refers to the brain’s resilience to injury or disease. It’s the brain’s ability to compensate for pathology and maintain cognitive function despite accumulating damage. Think of it as a buffer – some individuals have a larger buffer, allowing them to function relatively normally despite significant brain pathology, while others with a smaller buffer might experience a more pronounced decline.
Factors contributing to cognitive reserve include education level, occupation, intellectual engagement, social networks, and physical activity. For instance, a highly educated individual might maintain better cognitive function with Alzheimer’s disease than someone with limited education, due to a larger cognitive reserve. This concept is clinically relevant because it highlights that even with significant neuropathology, some individuals may still retain relatively intact cognitive function. Understanding cognitive reserve can help predict individual responses to disease and guide interventions that may strengthen the brain’s resilience.
Q 20. How do you use neuropsychological findings to inform treatment plans?
Neuropsychological findings are crucial in shaping individualized treatment plans. The specific cognitive deficits identified inform the selection of appropriate interventions. For example, if a patient demonstrates significant memory impairment, the treatment plan might include memory-enhancing strategies, such as mnemonics, memory aids, and external memory supports.
If executive dysfunction is prominent, strategies to improve organization, planning, and problem-solving would be implemented. The findings also inform decisions regarding medication management. For example, if a patient demonstrates significant difficulties with attention and concentration, a medication that might improve focus would be considered, but only after a careful assessment of potential side effects and patient preference. Treatment plans are regularly reviewed and modified based on patient progress and changing needs, utilizing a collaborative and evidence-based approach.
Q 21. What are the common side effects of medications used to treat cognitive disorders?
Medications used to treat cognitive disorders can have various side effects, which differ depending on the specific medication and the individual’s health status. Cholinesterase inhibitors, commonly used in Alzheimer’s disease, can cause nausea, vomiting, diarrhea, and increased risk of falls. Memantine, another medication for Alzheimer’s, can sometimes cause dizziness, headache, and constipation.
Antidepressants, often prescribed for depression associated with cognitive decline, can have side effects such as sleep disturbances, weight changes, and sexual dysfunction. It is essential to carefully weigh the potential benefits of medication against potential risks. Regular monitoring for side effects, adjusting dosages, or switching medications may be necessary. Open communication with the patient and their family about potential side effects is critical to ensure treatment adherence and patient safety. Thorough education about these side effects and strategies to manage them is key to successful treatment.
Q 22. Explain the principles of evidence-based practice in cognitive neurology.
Evidence-based practice (EBP) in cognitive neurology, like in any medical field, hinges on integrating the best available research evidence with clinical expertise and patient values. It’s not just about the latest study; it’s about critically evaluating that research and applying it thoughtfully to the unique circumstances of each patient.
This involves several key principles:
- Formulating a clear clinical question: For example, “In patients with mild cognitive impairment, does cognitive rehabilitation improve memory function more effectively than a placebo?”
- Searching for relevant research evidence: This requires using reputable databases like PubMed and Medline, searching for systematic reviews and meta-analyses whenever possible, and carefully assessing the quality of studies (considering sample size, study design, and potential biases).
- Critically appraising the evidence: This involves analyzing study methodology, assessing the validity and reliability of results, and determining the applicability of findings to the specific patient. Things like the age of participants, specific cognitive deficits, and comorbid conditions all play a crucial role.
- Integrating evidence with clinical expertise and patient values: Even the highest-quality research may not directly translate to a specific patient’s situation. We need to consider the patient’s preferences, their overall health, and their support system. For example, a patient may be unwilling to commit to an intensive cognitive rehabilitation program, which requires careful consideration and adjustment of treatment plans.
- Evaluating the effectiveness of interventions: After implementing a treatment plan, it’s essential to monitor the patient’s progress and determine if the chosen intervention is achieving the desired outcomes. This may involve neuropsychological testing, functional assessments, or caregiver reports.
In essence, EBP ensures that our clinical decisions are not driven by intuition or outdated practices but are grounded in the most reliable and up-to-date scientific evidence, leading to better patient care.
Q 23. Describe your experience with case management in cognitive neurology.
My experience in cognitive neurology case management encompasses the full spectrum of care, from initial assessment to long-term support. This involves coordinating care among various healthcare professionals—neurologists, psychiatrists, therapists, social workers, and caregivers—to create a comprehensive and individualized plan for each patient.
For instance, I’ve worked with patients with Alzheimer’s disease, managing their medication, referring them to appropriate therapies (speech, occupational, physical), and liaising with their families to ensure optimal home care and safety. In cases of traumatic brain injury, my role includes coordinating inpatient rehabilitation, discharge planning, and follow-up care to maximize functional recovery. This includes advocating for appropriate resources like assistive devices or home modifications.
A particularly challenging but rewarding case involved a young adult with a severe stroke resulting in aphasia and hemiparesis. Successfully coordinating the complex needs of speech therapy, physical therapy, occupational therapy, neuropsychological testing, and home health services while working closely with the family to manage their emotional distress was a testament to the importance of comprehensive case management. The patient’s eventual progress and return to semi-independent living was an immense success, highlighting the efficacy of a well-coordinated, holistic approach.
Q 24. How do you communicate complex medical information to patients and families?
Communicating complex medical information effectively requires empathy, patience, and tailoring the message to the patient’s and family’s understanding. I use a layered approach:
- Start with a summary: Begin with a brief, clear overview of the main points, avoiding excessive medical jargon. For example, instead of saying “the patient exhibits signs of frontotemporal dementia,” I might say, “We’ve found changes in the brain that are affecting thinking and behavior.”
- Use plain language: Avoid medical jargon. If technical terms are necessary, explain them clearly and simply, using analogies or metaphors when appropriate. For example, I’ll explain memory impairment as “like losing your car keys more frequently and having trouble finding them.”
- Check for understanding: Regularly ask questions like, “Does that make sense?” or “Do you have any questions?” and encourage them to ask questions without feeling pressured.
- Use visual aids: Diagrams, charts, and other visual aids can make complex information more accessible and easier to understand. This can be particularly helpful when discussing brain scans or treatment options.
- Involve family members: Often, family members play a significant role in the patient’s care, so it is important to make sure that they, too, understand the information.
- Provide written materials: Summarizing key information in writing can help reinforce learning and provide a reference for later review. I’ll always provide written summaries or links to reliable sources of information.
I find that active listening, patience, and a focus on patient empowerment are key to effective communication.
Q 25. What is your approach to working collaboratively with other healthcare professionals?
Collaborative teamwork is crucial in cognitive neurology. I believe in open communication, shared decision-making, and respecting the expertise of each member of the healthcare team.
My approach involves:
- Regular communication: Maintaining frequent and clear communication with other professionals through meetings, email, or phone calls is essential to ensure everyone is on the same page regarding the patient’s diagnosis, treatment plan, and progress.
- Shared decision-making: I actively involve other clinicians in developing and implementing the treatment plan. For example, in collaborating with a physical therapist, we might discuss how to adapt exercises to address cognitive deficits alongside physical limitations.
- Case conferences: Participating in multidisciplinary case conferences allows for a comprehensive review of complex cases, providing an opportunity to share insights and perspectives and make informed decisions collectively.
- Respect for different expertise: I recognize and value the specialized knowledge of other professionals (psychologists, social workers, occupational therapists, etc.) and actively seek their input. For example, I will always consult a neuropsychologist for detailed cognitive assessments to inform my diagnosis and treatment plans.
This collaborative model ensures a holistic approach to patient care, maximizing treatment effectiveness and improving patient outcomes.
Q 26. Describe your experience with research in cognitive neurology.
My research experience in cognitive neurology focuses on the efficacy of non-pharmacological interventions for individuals with Alzheimer’s disease. Specifically, my work has concentrated on the impact of music therapy on cognitive function and mood in patients with varying stages of Alzheimer’s.
I’ve been involved in several studies where we’ve investigated the effect of personalized music interventions tailored to individual patient preferences and memory profiles. We’ve used neuropsychological tests to measure cognitive function before, during, and after the intervention, as well as mood scales and caregiver reports to assess the impact on overall well-being. My research has contributed valuable data to understanding how targeted music interventions can be used as an adjunctive therapy to improve quality of life for these patients.
In addition to this, I’ve been involved in collaborative projects examining the neurobiological mechanisms underlying the effects of music therapy using neuroimaging techniques. This helps us understand how music affects the brain at a deeper level.
Q 27. How do you stay up-to-date with the latest advances in cognitive neurology?
Staying current in the rapidly evolving field of cognitive neurology requires a multifaceted approach:
- Regular review of peer-reviewed journals: I subscribe to several leading journals in neurology, psychiatry, and geriatrics, actively reading articles relevant to my practice and research interests.
- Participation in professional organizations: Membership in organizations like the American Academy of Neurology provides access to continuing medical education (CME) courses, conferences, and publications, keeping me updated on the latest advancements and clinical guidelines.
- Attendance at conferences and workshops: Attending national and international conferences provides opportunities to learn from leading experts, network with colleagues, and stay informed about groundbreaking research.
- Online resources and continuing education: Utilizing online platforms and resources, including reputable websites and CME modules, offers convenient and flexible ways to access updated information.
- Networking with colleagues: Discussing cases and new findings with colleagues, both within and outside my institution, is a valuable way to exchange information and gain different perspectives.
This continuous learning process ensures that I am equipped with the most up-to-date knowledge and best practices to provide optimal patient care.
Q 28. How do you handle disagreements with other clinicians regarding diagnosis or treatment?
Disagreements among clinicians regarding diagnosis or treatment are inevitable, especially in a complex field like cognitive neurology. However, it’s crucial to resolve these differences constructively to ensure the best possible care for the patient.
My approach emphasizes:
- Open and respectful dialogue: I start by engaging in a respectful discussion with the other clinician(s), listening carefully to their perspectives and explaining my reasoning clearly and thoroughly.
- Reviewing the available data: We jointly review the patient’s medical history, neuropsychological test results, imaging studies, and other relevant information to identify the basis of the disagreement.
- Consulting relevant literature: We might consult relevant guidelines or recent research findings to inform our decision-making. This collaborative review of evidence strengthens the eventual clinical decision.
- Seeking a second opinion: If the disagreement persists, seeking a second opinion from a senior or more experienced clinician can be beneficial in reaching a consensus.
- Documenting the process: It’s important to document the discussion, the different viewpoints, and the final decision reached in the patient’s medical record. This ensures transparency and avoids future misunderstandings.
The primary goal is to reach a mutually agreeable plan that prioritizes the patient’s best interests. If a consensus cannot be reached, a process of respectful disagreement is essential, and the patient and their family should be kept fully informed.
Key Topics to Learn for Cognitive Neurology Interview
- Cognitive Assessment & Testing: Understanding various neuropsychological tests (e.g., MMSE, MoCA), their administration, interpretation, and limitations. Practical application: Diagnosing cognitive disorders and monitoring disease progression.
- Neuroanatomy & Neurophysiology: A solid grasp of brain structures and their functions relevant to cognition (e.g., hippocampus, prefrontal cortex). Practical application: Correlating brain lesions with observed cognitive deficits.
- Dementia & its subtypes: In-depth knowledge of Alzheimer’s disease, frontotemporal dementia, vascular dementia, and other related conditions. Practical application: Differential diagnosis and management strategies.
- Stroke and its cognitive consequences: Understanding the various types of stroke and their impact on cognitive function. Practical application: Rehabilitation planning and prognosis estimation.
- Traumatic Brain Injury (TBI) and Cognitive Rehabilitation: Knowledge of the effects of TBI on cognition and the principles of cognitive rehabilitation. Practical application: Developing individualized treatment plans.
- Attention-Deficit/Hyperactivity Disorder (ADHD) in adults: Understanding the neurocognitive basis of ADHD and its presentation in adulthood. Practical application: Diagnosis and management strategies for adult ADHD.
- Memory disorders: Exploring different types of memory impairments (e.g., amnesia, working memory deficits). Practical application: Identifying the underlying causes and developing appropriate interventions.
- Research Methods in Cognitive Neurology: Familiarity with research designs, statistical analysis, and the interpretation of neuroimaging data (e.g., fMRI, EEG). Practical application: Critically evaluating research literature and contributing to the field.
Next Steps
Mastering Cognitive Neurology opens doors to exciting career opportunities in research, clinical practice, and academia. A strong foundation in this field significantly enhances your professional prospects and allows you to contribute meaningfully to patient care and scientific advancement. To maximize your chances of landing your dream role, creating an ATS-friendly resume is crucial. ResumeGemini is a trusted resource to help you build a professional and impactful resume that highlights your skills and experience effectively. We provide examples of resumes tailored specifically to Cognitive Neurology to help you get started. Invest time in crafting a compelling resume – it’s your first impression and a key to unlocking your career goals.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
To the interviewgemini.com Webmaster.
Very helpful and content specific questions to help prepare me for my interview!
Thank you
To the interviewgemini.com Webmaster.
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.