The right preparation can turn an interview into an opportunity to showcase your expertise. This guide to U.S. Food and Drug Administration (FDA) Regulations interview questions is your ultimate resource, providing key insights and tips to help you ace your responses and stand out as a top candidate.
Questions Asked in U.S. Food and Drug Administration (FDA) Regulations Interview
Q 1. Explain the difference between a GMP and a GLP.
GMP stands for Good Manufacturing Practices, while GLP stands for Good Laboratory Practices. Both are sets of quality guidelines enforced by the FDA, but they apply to different aspects of the product lifecycle.
GMP focuses on ensuring the consistent production of high-quality products. Think of it as the rules for making the product safely and reliably. It covers everything from the manufacturing process and facility cleanliness to personnel training and record-keeping. A pharmaceutical company adhering to GMP would meticulously control the environment, equipment calibration, and raw materials to guarantee consistent drug quality and potency.
GLP, on the other hand, applies to the non-clinical laboratory studies conducted to evaluate the safety of a product before it’s manufactured. It’s the set of rules governing how experiments are conducted to ensure reliability and integrity of the data used in, for example, determining toxicity. For instance, the GLP would specify details about the personnel qualifications, the method of handling and storing samples, and the way that data is documented and analyzed in a toxicology study.
In essence, GMP is about making a quality product, while GLP is about generating reliable data to support the safety of that product.
Q 2. Describe the FDA’s role in approving new drugs.
The FDA plays a crucial role in the approval of new drugs in the United States, ensuring both safety and efficacy. This involves a rigorous process spanning several phases.
- Pre-clinical Testing: Before even submitting an application, companies conduct extensive laboratory and animal studies to evaluate the drug’s safety and potential efficacy. GLP regulations guide this phase.
- Investigational New Drug (IND) Application: Companies submit an IND application to the FDA before beginning clinical trials in humans. This application provides pre-clinical data and a detailed plan for clinical trials.
- Clinical Trials (Phases I-III): These trials involve testing the drug in humans, progressively increasing the number of participants and the duration of the study. Each phase assesses different aspects, such as safety, dosage, and efficacy.
- New Drug Application (NDA): Once clinical trials are completed, the company submits an NDA to the FDA. This comprehensive application contains all data from pre-clinical and clinical studies, demonstrating that the drug is safe and effective for its intended use.
- FDA Review: The FDA reviews the NDA thoroughly, often taking months or even years. This review involves expert panels and careful scrutiny of the submitted data.
- Approval or Rejection: The FDA will either approve the drug for marketing, approve it with restrictions, or reject it. If approved, the FDA monitors the drug’s safety and efficacy post-market.
Imagine building a skyscraper. The FDA acts as the building inspector, ensuring the blueprint (IND/NDA) is sound and the construction (clinical trials) meets rigorous safety standards before the building (drug) is allowed to be occupied (used by the public).
Q 3. What are the key requirements of 21 CFR Part 11?
21 CFR Part 11 sets forth the FDA’s guidelines for electronic records and electronic signatures in regulated industries. It aims to ensure the integrity, authenticity, and reliability of electronic data submitted to the FDA. Key requirements include:
- Validation: Systems and processes must be validated to ensure they reliably produce accurate and trustworthy results. This often involves rigorous testing and documentation.
- Security: Systems must be secured to prevent unauthorized access, modification, or deletion of data. Access controls, audit trails, and data backups are essential components.
- Authentication: Electronic signatures must be unique and securely linked to the signatory. This is crucial for establishing accountability and ensuring the legitimacy of electronic documents.
- Data Integrity: Data must be complete, accurate, and consistent throughout its lifecycle. This necessitates rigorous data management practices and the implementation of robust systems for handling electronic documents.
- Audit Trails: Detailed audit trails must record all actions performed on the system, including who, what, when, and where. This information is vital for tracking changes and identifying any potential data integrity issues.
Imagine a bank’s online system. 21 CFR Part 11 mandates similar controls to protect against fraud and ensure reliable transaction records. The regulations ensure that electronic data are as trustworthy as paper records – a critical requirement for compliance within regulated environments.
Q 4. Explain the process of submitting a 510(k) premarket notification.
A 510(k) premarket notification is a submission to the FDA demonstrating that a new medical device is substantially equivalent to a legally marketed predicate device. This means it has the same intended use and technological characteristics as the predicate, with any differences not raising new questions about safety or effectiveness. The process involves:
- Identify a Predicate Device: Find an already FDA-cleared device that’s substantially similar to your new device.
- Gather Supporting Data: Collect evidence showing substantial equivalence, such as design documents, test results, and comparisons to the predicate device.
- Prepare the 510(k) Submission: Compile all necessary information and submit it electronically through the FDA’s eSubmitter system.
- FDA Review: The FDA reviews the submission to determine if the device meets the criteria for substantial equivalence.
- Approval or Rejection: The FDA either clears the device for marketing or requests more information or rejects the submission.
Think of it like presenting a case to a judge. You’re arguing that your new device is essentially the same as a previously approved one (your precedent), so it doesn’t need a full review. The FDA acts as the judge and decides if your case is convincing.
Q 5. What is a recall and what are the different classes of recalls?
A recall is the removal of a product from the market after it has been sold due to safety concerns. The FDA classifies recalls into three classes based on the severity of the health risk:
- Class I Recalls: These involve products with a reasonable probability that use will cause serious adverse health consequences or death. This is the most serious type of recall. Example: A contaminated food product leading to widespread illness.
- Class II Recalls: These involve products where use might cause temporary or medically reversible adverse health consequences, but the probability of serious adverse health consequences is low. Example: A medical device with a minor defect that could potentially cause discomfort.
- Class III Recalls: These involve products where use is not likely to cause adverse health consequences. Example: A cosmetic product with incorrect labeling.
Imagine a car manufacturer discovering a critical brake failure. A Class I recall would be mandatory, immediately pulling all affected cars off the road. A minor paint flaw would likely be a Class III recall, handled through less urgent corrective actions.
Q 6. Describe the requirements for current Good Manufacturing Practices (cGMP).
Current Good Manufacturing Practices (cGMP) are regulations enforced by the FDA to ensure that products are consistently produced and controlled according to quality standards appropriate for their intended use and as required by the applicable regulations. Key requirements include:
- Facility and Equipment: Facilities must be designed and maintained to prevent contamination, and equipment must be calibrated and maintained to ensure reliable operation.
- Personnel: Personnel must be properly trained and qualified to perform their assigned tasks. Hygiene and gowning procedures are crucial to preventing contamination.
- Materials: Raw materials and packaging components must be of appropriate quality and stored correctly to prevent degradation or contamination.
- Manufacturing Processes: Manufacturing processes must be documented and controlled to ensure consistency and reproducibility. Deviation management processes are crucial for addressing any issues.
- Quality Control: Robust quality control procedures must be in place to monitor the quality of materials, processes, and finished products.
- Documentation: Meticulous record-keeping is essential, including batch records, testing results, and personnel training records.
Think of it like baking a cake. cGMP ensures you use the right ingredients, follow the recipe precisely, and have a clean kitchen – all essential for producing a consistently delicious and safe cake. Any deviation is documented.
Q 7. What are the key components of a quality system?
A robust quality system is crucial for any organization subject to FDA regulations. It’s a comprehensive framework designed to ensure consistent production of high-quality products that meet regulatory requirements and customer expectations. Key components include:
- Management Responsibility: Top management must actively demonstrate commitment to quality through clear policies and resources.
- Quality Planning: A well-defined plan for ensuring quality throughout the product lifecycle, from design and development to manufacturing and post-market surveillance.
- Resource Management: Provision of appropriate resources, including personnel, equipment, and facilities, to support quality objectives.
- Product Realization: Effective processes for designing, manufacturing, and testing products to meet specified requirements.
- Measurement, Analysis, and Improvement: Regular monitoring and measurement of quality indicators, analysis of results, and implementation of corrective and preventive actions.
- Continual Improvement: Ongoing efforts to enhance the quality system through continuous improvement methods such as Lean and Six Sigma.
Imagine an orchestra. A quality system is like the conductor, ensuring all sections (departments) work together harmoniously to produce a flawless performance (high-quality product) that meets expectations (regulatory compliance and customer satisfaction).
Q 8. How does the FDA ensure the safety of food products?
The FDA employs a multi-pronged approach to ensure food safety, focusing on preventing contamination rather than solely reacting to problems. This involves a combination of regulations, inspections, and surveillance.
- Regulations: The FDA sets stringent standards for food production, processing, packaging, and labeling. These regulations cover everything from safe handling practices to acceptable levels of contaminants. For example, the Food Safety Modernization Act (FSMA) shifted the focus from responding to contamination to proactively preventing it.
- Inspections: FDA inspectors regularly visit food facilities to verify compliance with these regulations. Inspections can range from routine checks to more in-depth investigations triggered by consumer complaints or other concerns. Inspectors assess things like sanitation practices, temperature controls, and employee training.
- Surveillance: The FDA monitors foodborne illnesses through data analysis and collaborates with state and local health agencies. This helps them identify emerging risks and trends, allowing for timely interventions.
- Testing and Analysis: FDA laboratories conduct testing on food samples to detect contaminants or adulterants. This helps ensure that food products meet established safety standards.
Think of it like this: the FDA acts as a diligent guardian, setting the rules, regularly checking on food producers to ensure they are following the rules, and constantly monitoring for any potential threats to public health.
Q 9. Explain the concept of risk-based inspection by FDA.
Risk-based inspection means the FDA prioritizes inspections based on the level of risk a particular facility poses to public health. Instead of inspecting every facility equally, they focus their resources on those deemed to present the highest risk.
This involves analyzing various factors to assess risk. Factors might include the type of food produced (e.g., ready-to-eat foods are higher risk than shelf-stable foods), the facility’s history (previous violations increase risk), the type of processing involved (complex processes might have more potential for error), and the scale of operation (larger facilities generally process more food and thus have greater potential impact).
For instance, a small facility producing low-risk products might receive an inspection less frequently than a large facility manufacturing ready-to-eat products with a history of non-compliance. This strategy makes the FDA’s inspection resources more efficient and effective.
Q 10. What are the different types of FDA inspections?
The FDA conducts several types of inspections, each with a different purpose:
- Routine Inspections: These are regular inspections to verify compliance with regulations. They are often scheduled but can also be unannounced.
- For-Cause Inspections: These inspections are triggered by specific events, such as consumer complaints, outbreaks of foodborne illness, or information suggesting non-compliance.
- Pre-Approval Inspections: These occur before a new facility or product is allowed to operate or be marketed (especially relevant for medical devices and some foods).
- Post-Approval Inspections: These inspections follow a product’s approval to ensure ongoing compliance and safety.
- Surveillance Inspections: These are more targeted inspections focused on specific issues or trends identified through surveillance activities.
The type of inspection and its intensity directly depends on the risk assessment.
Q 11. What is the role of the FDA in regulating medical devices?
The FDA plays a crucial role in regulating medical devices, ensuring their safety and effectiveness. This involves a complex process of premarket review and postmarket surveillance.
- Premarket Review: Before a medical device can be marketed, it must typically undergo a rigorous review process, often including testing, clinical trials, and submission of extensive data to demonstrate safety and effectiveness. The level of scrutiny varies depending on the device’s risk classification.
- Postmarket Surveillance: Even after a device is approved, the FDA continues to monitor its safety and performance through post-market surveillance programs, including adverse event reporting systems and periodic inspections.
- Classifications: Medical devices are classified into different risk categories (Class I, II, III), with higher-risk devices facing more stringent regulatory requirements. This ensures that high-risk devices, such as implantable pacemakers, undergo extremely thorough review and are subject to stricter post-market monitoring.
The FDA’s authority extends to almost every aspect of the device lifecycle, from its design and manufacturing to its distribution and use.
Q 12. Explain the difference between pre-approval and post-approval inspections.
The key difference lies in timing and purpose.
- Pre-approval inspections occur before a product or facility is allowed to operate or market a product. They’re designed to verify that the facility or product meets FDA standards before they are released to the public. Think of it as a final check before launch.
- Post-approval inspections are conducted after a product or facility has been approved. These inspections monitor ongoing compliance with regulations, identify potential problems, and ensure that previously-met standards continue to be upheld. These are essentially follow-up checks to ensure continued safety and efficacy.
Both are vital for ensuring the safety of products and the public, just at different points in the product lifecycle.
Q 13. What is the significance of a Warning Letter from the FDA?
Receiving a Warning Letter from the FDA is extremely serious. It’s an official notification indicating that the agency has found significant violations of FDA regulations. These violations often pose a serious risk to public health or safety.
A Warning Letter is not a minor issue; it’s a strong indication that the FDA is gravely concerned about the company’s practices. It usually demands immediate corrective action and can lead to severe consequences, including:
- Import Alerts: Preventing the company from importing its products into the U.S.
- Product Recalls: Requiring the recall of affected products from the market.
- Seizures: Confiscation of products and materials.
- Injunctions: Court orders halting production or distribution.
- Civil Penalties: Significant financial penalties.
- Criminal Prosecution: In extreme cases, criminal charges may be filed.
A Warning Letter is a public document, potentially damaging the company’s reputation and affecting investor confidence. Responding appropriately and promptly is crucial.
Q 14. Describe the process of responding to an FDA 483.
An FDA Form 483 is issued at the conclusion of an inspection and lists the observations made by the inspector indicating that violations of FDA regulations have been observed. Responding to a 483 is a critical step that requires careful attention to detail.
The response process generally involves:
- Acknowledgement: Acknowledge receipt of the Form 483 within a reasonable timeframe (often specified by the FDA).
- Investigation: Thoroughly investigate each observation listed on the Form 483. This might involve reviewing company records, conducting interviews, and gathering supporting evidence.
- Corrective Actions: Develop and implement corrective actions to address each observation. This should be more than simply stating that the company will fix the issue; it needs detailed explanations of the steps taken to prevent recurrence.
- Documentation: Document all corrective actions taken, including dates, individuals involved, and specific actions performed. This documentation will become crucial in demonstrating that the company is taking the violations seriously.
- Response Preparation: Prepare a comprehensive written response to the FDA, addressing each observation point-by-point. This response should include a description of the violation, the corrective actions taken, and evidence demonstrating the effectiveness of those actions. Use concise and factual language, avoiding excuses or blaming others.
- Submission: Submit the written response to the FDA within the specified timeframe.
A well-prepared response is critical. It demonstrates the company’s commitment to compliance and helps mitigate potential further consequences.
Q 15. How do FDA guidelines on labeling apply to dietary supplements?
FDA labeling guidelines for dietary supplements are distinct from those for conventional foods and drugs. They emphasize truthfulness and avoid misleading claims. Supplements must clearly state the product name, net contents, manufacturer’s name and address, and a supplement facts panel.
The supplement facts panel is crucial. It lists the amount of each dietary ingredient per serving size, using standardized terms. Claims about the supplement’s effects on the body are subject to strict regulations. The FDA scrutinizes claims to ensure they’re substantiated by significant scientific evidence, prohibiting unsubstantiated claims that suggest a treatment or cure for diseases. For example, a supplement claiming to ‘cure cancer’ would be immediately flagged for violation. Claims about structure/function, (like ‘supports immune health’), are permitted as long as they are not misleading and meet specific criteria. The statement ‘This statement has not been evaluated by the Food and Drug Administration. This product is not intended to diagnose, treat, cure, or prevent any disease.’ must also be included.
Think of it this way: while the FDA doesn’t pre-approve dietary supplements before they hit the market, they actively monitor the marketplace and take action against products making false or misleading claims. Companies are responsible for ensuring the safety and accuracy of their labeling.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What are the requirements for submitting an Investigational New Drug (IND) application?
Submitting an Investigational New Drug (IND) application is the crucial first step in bringing a new drug to market in the U.S. It’s a formal request to the FDA for permission to test an experimental drug in humans. The application is incredibly detailed and requires extensive pre-clinical data.
- Pre-clinical data: This includes pharmacology, toxicology, and pharmacokinetic studies in animals, demonstrating the drug’s safety and potential efficacy. This is a pivotal section as the FDA will assess whether the drug is sufficiently safe for human testing, given the results.
- Manufacturing information: The IND must describe the drug’s manufacturing process, ensuring quality control and consistency. The FDA needs to understand how the drug is being made to evaluate the reliability of the product.
- Investigational plan: A detailed protocol outlining the planned clinical trials, including objectives, methodology, patient selection, and safety monitoring measures. This clarifies the investigative goals and establishes a thorough strategy for clinical assessment.
- Chemistry, Manufacturing, and Controls (CMC): This section provides the FDA with detailed information about the drug’s chemical composition, its manufacturing process, and the quality control measures employed during production. This ensures the purity and consistency of the drug across batches.
- Investigator information: Information about the principal investigator and other key personnel involved in the clinical trials, highlighting their experience and qualifications. This highlights the credibility of the team conducting the research.
The FDA reviews the IND application to assess the safety of the proposed research and whether the plan is well-designed to generate useful data. Approval doesn’t guarantee the drug will be successful; it simply permits human testing to begin, under strict FDA oversight.
Q 17. What is a New Drug Application (NDA)?
A New Drug Application (NDA) is a comprehensive submission to the FDA providing all the necessary data to support the approval of a new drug for marketing in the United States. Think of it as the culmination of years of research and development. It’s a rigorous process, with the FDA undertaking an intense review of every aspect of the drug’s development.
The NDA includes:
- Results from clinical trials: Extensive data on the drug’s safety and efficacy, including details on patient populations studied, outcomes, and adverse events. This data is critical for determining the drug’s effectiveness and risk-benefit profile.
- Chemistry, manufacturing, and controls (CMC) information: Information about the drug’s chemical composition, manufacturing process, and quality control procedures. This is paramount to guarantee product consistency and quality.
- Proposed labeling: The text that will appear on the drug’s packaging, providing information about its use, dosage, warnings, and potential side effects. This is essential for patient safety and informed use.
- Pre-clinical data: Summary of non-clinical studies performed during the development of the drug. This section summarizes earlier data.
After submission, the FDA conducts a thorough review, often taking several months to several years depending on complexity and completeness. The approval process includes several phases, with potential requests for additional data or clarification. Once approved, the drug can be marketed and sold in the U.S.
Q 18. Describe the process of obtaining FDA approval for a new food additive.
The process for obtaining FDA approval for a new food additive is rigorous and multifaceted, emphasizing the safety of the additive for its intended use. Manufacturers must submit a detailed petition to the FDA, providing comprehensive data to support their claim that the additive is safe.
Key steps include:
- Data submission: This includes toxicity studies in animals, demonstrating the absence of harmful effects at anticipated usage levels, and metabolic studies, showing how the body processes the additive. These studies are fundamental for assessing the safety profile.
- Manufacturing details: Precise information on the additive’s manufacturing process, including purity, quality control methods, and any potential byproducts or contaminants. This information is crucial for ensuring consistent quality and safety.
- Proposed use and intended food: Clear specification of the food(s) where the additive will be used and the intended function (e.g., preservation, color, flavor). This establishes the context for the safety evaluation.
- FDA review and evaluation: The FDA conducts a thorough review, considering the data, evaluating potential risks and benefits, and making a final determination based on the established safety standards. This process can take years.
- Public comment period: Following the submission, the FDA typically initiates a period of public comment to gather input from experts and stakeholders before reaching a final decision. This allows for broader perspectives.
If the FDA approves the petition, the additive can be legally used in food products according to the approved specifications. Approval is not granted lightly, as the FDA prioritizes the protection of public health.
Q 19. What is a bioequivalence study and why is it important?
A bioequivalence study compares the rate and extent to which the active ingredient in a drug product becomes available at its site of action. It’s critical for generic drug approvals. Think of it as comparing two versions of the same drug: a brand-name drug and its generic counterpart.
The FDA requires that generic drugs demonstrate bioequivalence to their brand-name counterparts. This means that the generic drug must deliver the same amount of active ingredient to the body at the same rate, resulting in comparable therapeutic effects. A bioequivalence study involves administering both the brand-name drug and the generic drug to a group of volunteers, then meticulously measuring the levels of the active ingredient in their blood over time. Statistical analysis is then employed to determine whether there are any significant differences in absorption.
Why is it important? Bioequivalence ensures that generic drugs are therapeutically equivalent to their brand-name counterparts, guaranteeing patient safety and efficacy. Without bioequivalence studies, the FDA couldn’t confidently approve generic drugs, potentially leaving patients without affordable alternatives to expensive brand-name medications.
Q 20. Explain the concept of adverse event reporting to the FDA.
Adverse event reporting to the FDA is a critical process for ensuring drug safety after a drug has been approved and is on the market. It’s a system for tracking and evaluating potential harms associated with the use of pharmaceuticals and other regulated products. Essentially, it’s a post-market surveillance system.
Various parties are responsible for reporting adverse events. These include:
- Pharmaceutical companies: They are obligated to report adverse events based on information gathered from various sources, including post-marketing surveillance, clinical trials, and spontaneous reports from healthcare professionals or consumers.
- Healthcare professionals (physicians, pharmacists): They have a responsibility to report serious and unexpected adverse events to the FDA, particularly those that could be related to a drug’s use. This plays a crucial role in early detection.
- Consumers: While not legally required, patients are encouraged to report suspected adverse events, as their accounts can add valuable context and details that might be overlooked otherwise.
The FDA analyzes the reported adverse events to identify patterns, assess risks, and take appropriate action, ranging from updated labeling to drug withdrawal from the market, if necessary. This constant monitoring system is vital for the detection of rare but potentially severe side effects that might not have been evident during the pre-market clinical trials.
Q 21. What are some common FDA violations in the pharmaceutical industry?
Common FDA violations in the pharmaceutical industry often stem from lapses in Good Manufacturing Practices (GMP), data integrity, and labeling accuracy.
- GMP violations: These include issues with facility cleanliness, equipment calibration, raw material sourcing, and quality control testing. Failure to adhere to GMP guidelines compromises product safety and consistency. An example would be inadequate documentation of cleaning and sterilization procedures.
- Data integrity issues: This involves manipulating, falsifying, or failing to properly record data related to drug development, manufacturing, or clinical trials. Falsified data undermines the validity of research and approval processes. An example would be deleting data points that don’t support the desired outcome.
- Labeling violations: Incorrect or misleading information on drug labels is a serious offense that could harm patients. This could include errors in dosage instructions or the omission of crucial safety information.
- Failure to report adverse events: Pharmaceutical companies have a legal obligation to report serious adverse events to the FDA promptly. Failure to do so endangers public health and undermines patient safety.
- Off-label promotion: Promoting a drug for uses not approved by the FDA is illegal and potentially dangerous. For instance, marketing a drug for a specific ailment it hasn’t been explicitly approved for.
These violations can lead to significant consequences, including warnings, fines, product recalls, and even criminal prosecution.
Q 22. How does the FDA regulate advertising for drugs and medical devices?
The FDA regulates drug and medical device advertising through a combination of statutes, regulations, and guidance documents. The primary goal is to ensure that such advertising is truthful, not misleading, and provides sufficient information for healthcare professionals and consumers to make informed decisions. This means ads cannot make unsubstantiated claims about efficacy or safety.
For prescription drugs, advertising is primarily directed towards healthcare professionals (HCPs) through journals, detailing, and presentations. These ads must be supported by substantial evidence of effectiveness, as determined through rigorous clinical trials. Direct-to-consumer (DTC) advertising of prescription drugs is also permitted, but it must include a ‘brief summary’ of risk information, though the exact requirements for this summary are a complex area of regulation that often undergoes revisions.
Medical device advertising, similarly, must be truthful and not misleading. The level of substantiation required depends on the type of claim made, with more rigorous evidence needed for claims of effectiveness. The FDA uses warning letters and enforcement actions against companies violating these regulations. For example, an ad claiming a device cures a disease without sufficient clinical data would be deemed unlawful.
Q 23. What are the key elements of a successful FDA inspection?
A successful FDA inspection hinges on meticulous preparation and thorough documentation. The agency aims to verify that a company is compliant with all relevant Good Manufacturing Practices (GMPs), current Good Laboratory Practices (cGLPs), and other applicable regulations. Key elements include:
- Prioritization of compliance: The company must demonstrate a strong culture of compliance, evidenced by comprehensive standard operating procedures (SOPs) and a well-defined quality system. Imagine a factory where every step has a documented procedure—that’s the goal.
- Complete documentation: All records, from batch production records to employee training logs, must be readily accessible and accurate. This is crucial for demonstrating compliance and tracing any potential problems.
- Effective quality control: A robust quality control system, including testing and release procedures, must be in place to ensure product quality and safety. Imagine a rigorous quality-control check before shipping goods to ensure only top-notch products reach consumers.
- Corrective and Preventive Actions (CAPA): A company’s ability to identify, investigate, and correct deviations from GMPs is essential. A good CAPA system shows the FDA that the company learns from mistakes and prevents future occurrences. It’s about continuous improvement and proactively avoiding errors.
- Personnel training: Employees at all levels must be adequately trained on relevant GMPs and SOPs.
An inspection involves a thorough review of documents and facilities, with observations and sampling. Failures to meet these standards can result in warning letters, import alerts, or even facility closures.
Q 24. What are some strategies for preventing FDA violations?
Preventing FDA violations requires a proactive and comprehensive approach. Key strategies include:
- Establish a robust quality system: Implementing a comprehensive quality management system that aligns with current Good Manufacturing Practices (cGMP) is crucial. This system should incorporate detailed SOPs, comprehensive training programs, and effective change control procedures.
- Invest in employee training: Employees at all levels need thorough training on GMPs, relevant regulations, and SOPs. Ongoing training ensures everyone understands their role in compliance.
- Maintain meticulous documentation: Accurate and complete records are essential. This includes batch records, testing results, training records, and any deviations from SOPs.
- Implement a strong CAPA system: A proactive approach to identifying, investigating, and correcting deviations is vital. This shows the FDA that the company is committed to continuous improvement.
- Regular internal audits: Conduct regular internal audits to assess compliance and identify potential weaknesses before an FDA inspection. It’s like a self-checkup, catching problems early.
- Stay updated on regulations: The FDA’s regulations are constantly evolving. Staying informed through subscriptions to newsletters and updates is critical to ensuring ongoing compliance.
Proactive compliance is far more cost-effective than reacting to an FDA warning letter or enforcement action.
Q 25. How does the FDA handle the approval of generic drugs?
The FDA approves generic drugs through an abbreviated approval pathway, known as the 505(b)(2) pathway. This process relies on demonstrating bioequivalence to the brand-name drug, meaning the generic drug performs the same way as the reference drug in terms of absorption, distribution, metabolism, and excretion.
Unlike the lengthy and costly process for new drug approvals, generic drug applications focus on proving bioequivalence rather than conducting extensive clinical trials to show safety and efficacy. They must demonstrate that the generic drug is pharmaceutically equivalent (same active ingredient, dosage form, and route of administration) and bioequivalent (same rate and extent of absorption) to the innovator drug. This process is significantly faster and less expensive, making generic medications more accessible to the public.
The FDA reviews the data submitted by the generic drug manufacturer to determine bioequivalence, analyzes the manufacturing processes and quality control measures, and assesses the overall safety and purity of the generic drug. If all criteria are met, the FDA approves the generic drug, allowing it to be marketed and sold.
Q 26. Explain the FDA’s role in regulating cosmetics.
The FDA’s role in regulating cosmetics is significantly different from its role in regulating drugs and medical devices. The FDA has a much more limited regulatory authority over cosmetics. While the agency doesn’t pre-approve cosmetics before they go to market, it does regulate them after they’re on the market. The FDA regulates the safety of cosmetics under the Federal Food, Drug, and Cosmetic Act.
This authority includes:
- Prohibiting the use of unsafe ingredients: The FDA has the authority to take action against companies if they’re using ingredients that are unsafe or cause harm.
- Requiring proper labeling: Companies must accurately label their products with ingredients and any other necessary information.
- Taking action against misbranded products: The agency can take action against companies making false or misleading claims about their cosmetics.
However, it’s important to note that the FDA doesn’t have the same pre-approval process for cosmetics as it does for drugs and medical devices. Companies are generally responsible for ensuring the safety of their products before they are marketed.
Q 27. What is the significance of the Delaney Clause?
The Delaney Clause, part of the Food Additives Amendment of 1958, originally prohibited the approval of food additives found to induce cancer in humans or animals. It established a zero-tolerance policy for carcinogens in food. Think of it as a strict ‘no cancer-causing substances allowed’ rule.
However, the Delaney Clause has been largely superseded by the more flexible approach of the Food Quality Protection Act (FQPA) of 1996. The FQPA considers the benefits of a substance alongside its risks, including carcinogenic risks, and allows for a ‘reasonable certainty of no harm’ standard. This means that a small amount of a carcinogen might be permitted if the benefit outweighs the risk, and the exposure is at a low enough level that there’s reasonable certainty it won’t cause harm. While the Delaney Clause still exists in law, it’s rarely applied in practice due to the FQPA’s prevalence.
Q 28. How does the FDA enforce its regulations?
The FDA enforces its regulations through a multi-pronged approach, using a combination of education, cooperation, and enforcement actions. The agency prioritizes working collaboratively with industry to foster compliance. This often involves providing guidance documents, conducting inspections, and offering educational resources.
However, when companies fail to comply, the FDA can take several enforcement actions, including:
- Warning letters: These letters formally notify a company of violations and request corrective actions. It’s like a first strike—a chance to fix the problem.
- Import alerts: These alerts prevent the entry of non-compliant products into the U.S.
- Seizure of products: The FDA can seize products that violate its regulations. This involves physically confiscating products deemed unsafe or mislabeled.
- Injunctions: The FDA can seek court injunctions to halt the production or distribution of non-compliant products. This is a more serious step, involving legal action.
- Civil penalties and criminal prosecution: For severe or repeated violations, the FDA may impose significant fines or even pursue criminal prosecution. This is the most severe action, representing serious breaches of regulations.
The FDA’s enforcement actions are designed to protect public health and ensure compliance with regulations. The severity of the action taken typically reflects the seriousness and nature of the violation.
Key Topics to Learn for U.S. Food and Drug Administration (FDA) Regulations Interview
- Current Good Manufacturing Practices (cGMP): Understanding the principles and applications of cGMP across various FDA-regulated industries (food, drugs, cosmetics). Consider exploring specific regulations like 21 CFR Part 110 (Current Good Manufacturing Practice in Manufacturing, Packing, or Holding Human Food).
- Food Safety Modernization Act (FSMA): Focus on the preventive controls for human food, including hazard analysis and risk-based preventive controls. Explore practical applications such as implementing a food safety plan and managing supplier verification programs.
- Food Labeling Regulations: Master the requirements for accurate and truthful labeling of food products, including nutrition facts, allergen statements, and health claims. Practice applying these regulations to various food scenarios.
- Dietary Supplements: Understand the unique regulatory framework for dietary supplements, including cGMP requirements and labeling regulations specific to this category. Explore the process of New Dietary Ingredient (NDI) notifications.
- Enforcement and Compliance: Familiarize yourself with FDA inspection procedures, warning letters, and recall processes. Practice analyzing hypothetical scenarios involving non-compliance and developing solutions.
- Relevant FDA Guidance Documents: Become comfortable navigating and interpreting FDA guidance documents to understand best practices and agency expectations. Practice applying this knowledge to case studies or hypothetical scenarios.
Next Steps
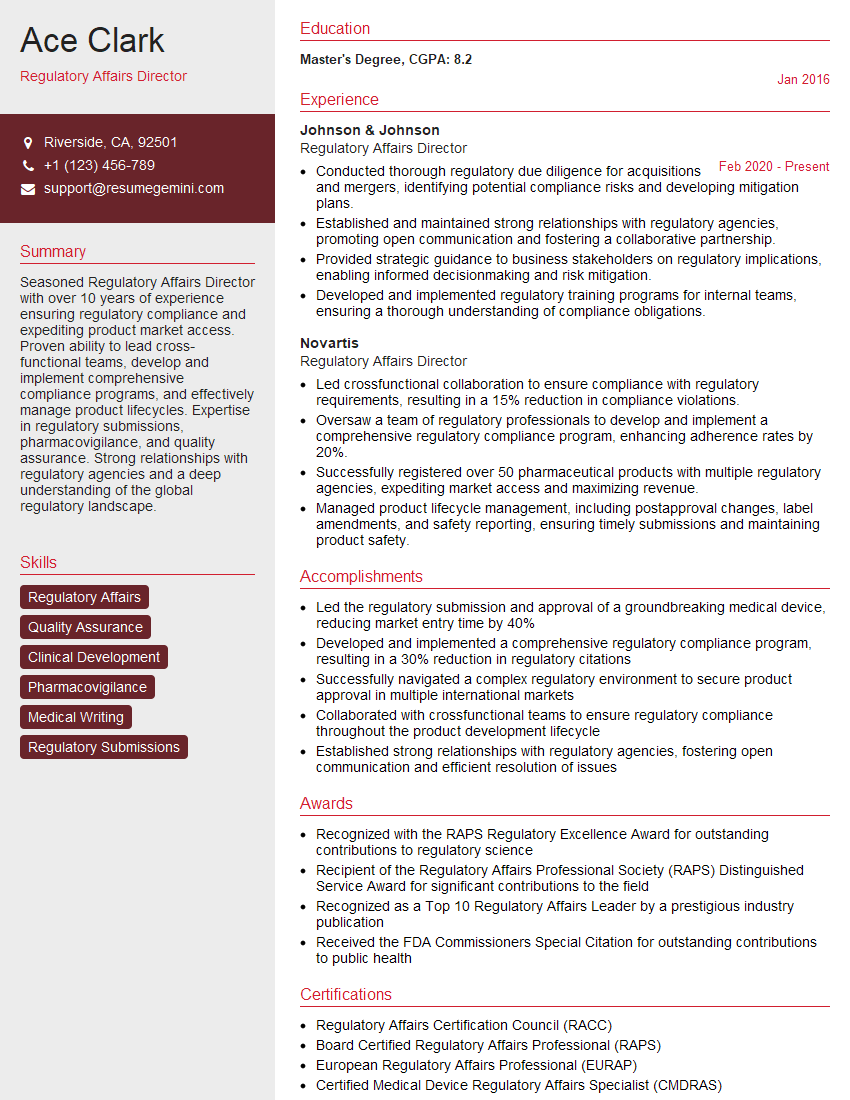
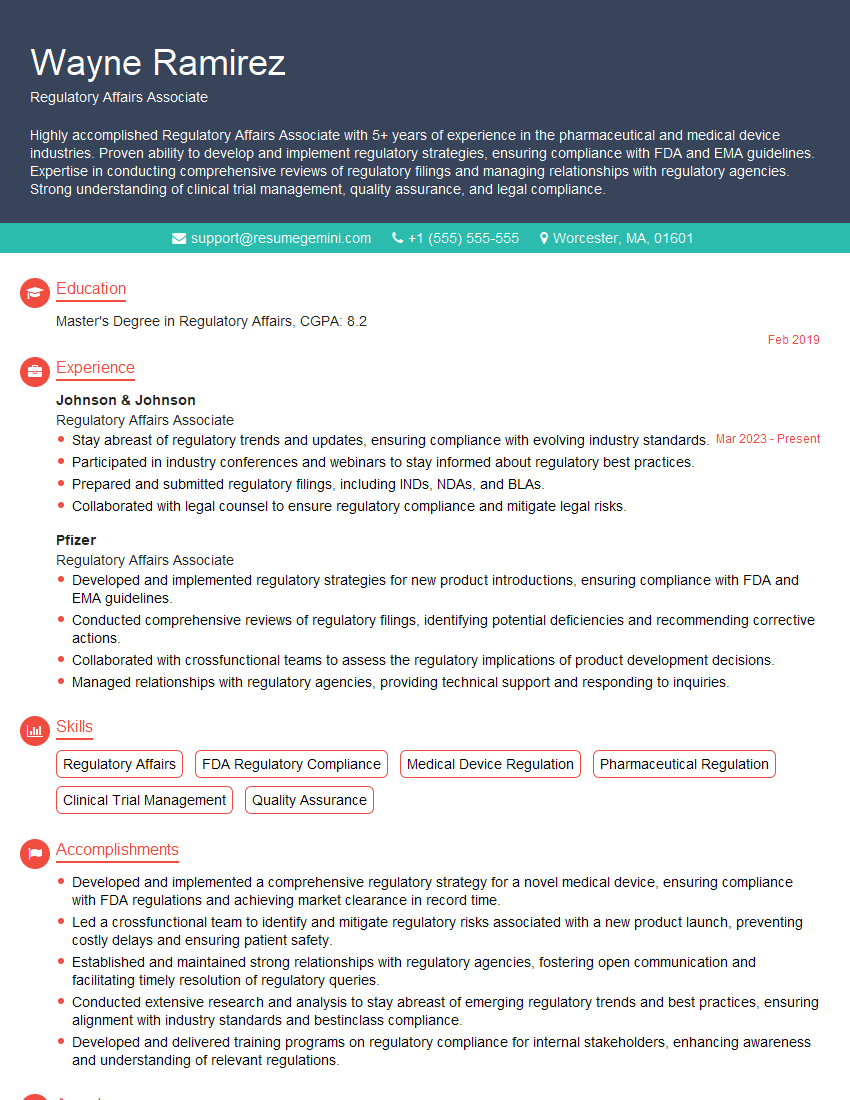
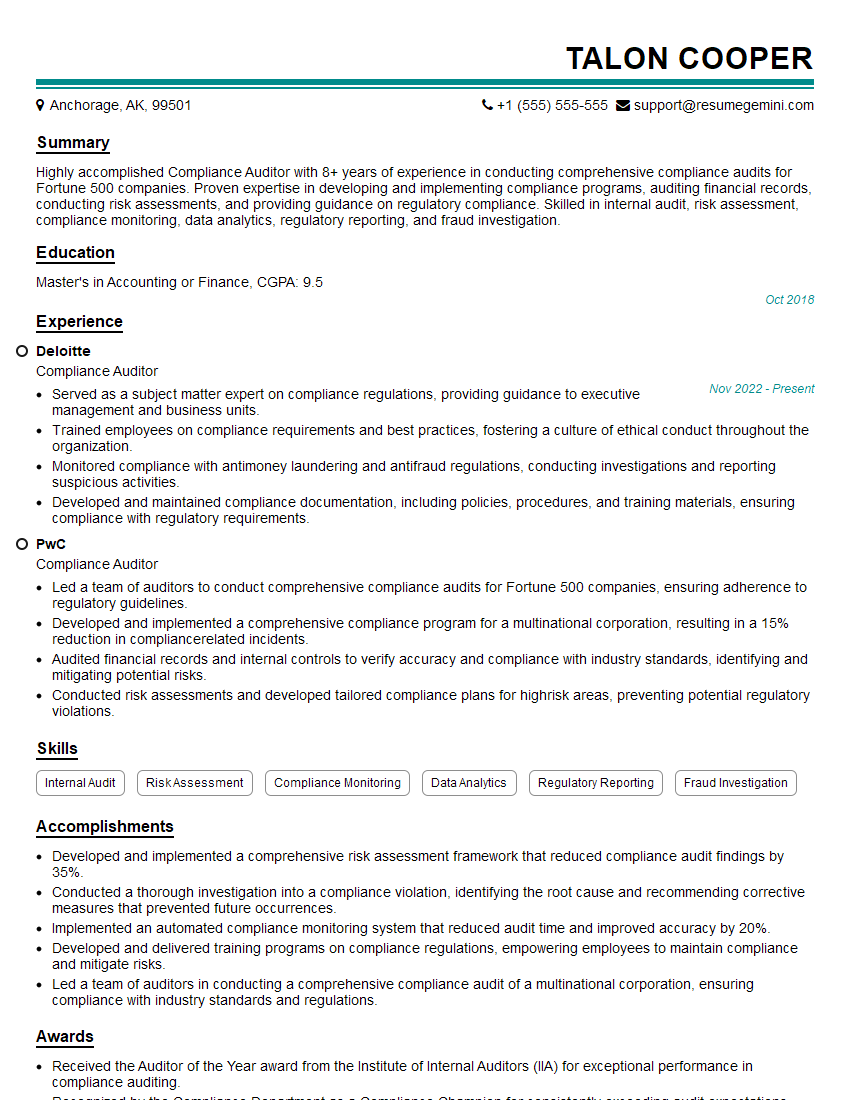
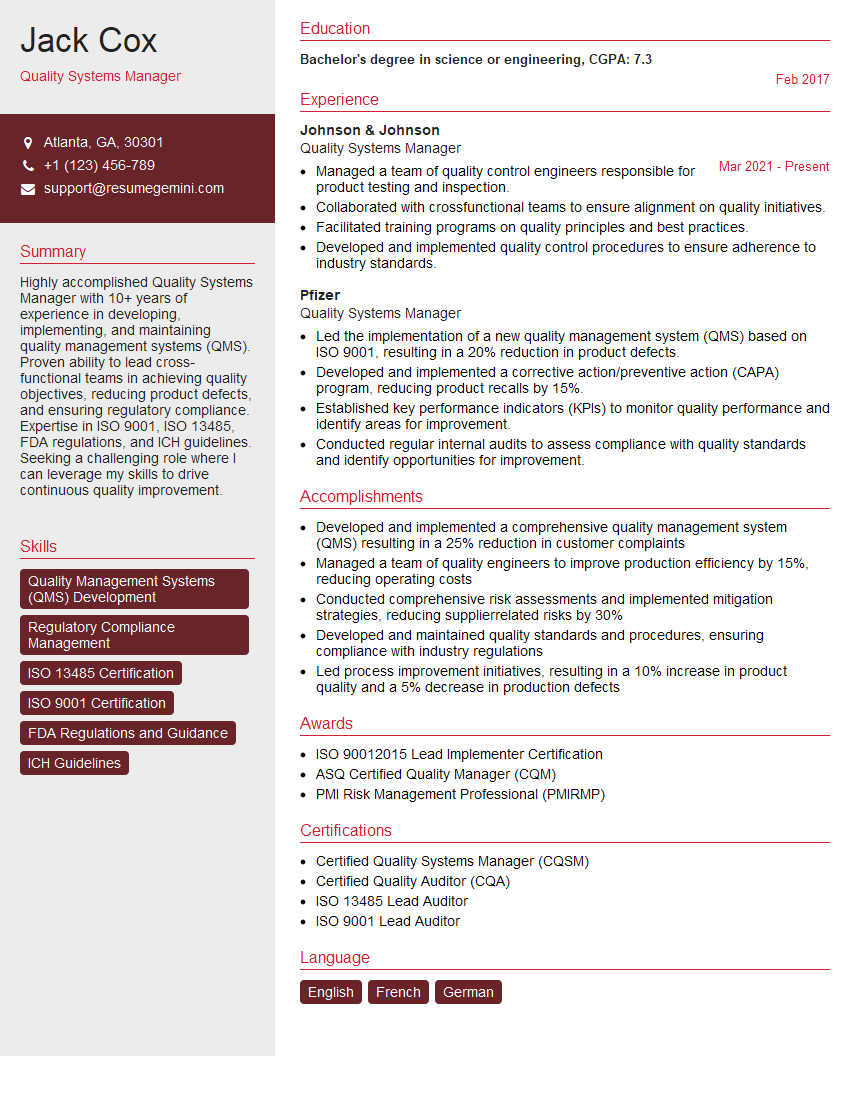
Mastering U.S. Food and Drug Administration (FDA) Regulations is crucial for career advancement in regulated industries. A strong understanding of these regulations demonstrates your commitment to safety and compliance, opening doors to more challenging and rewarding roles. To significantly increase your chances of landing your dream job, it’s essential to create an ATS-friendly resume that highlights your relevant skills and experience. ResumeGemini is a trusted resource that can help you build a professional, impactful resume tailored to your specific career goals. We provide examples of resumes tailored to the U.S. Food and Drug Administration (FDA) Regulations field, giving you a head start in crafting a winning application.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
To the interviewgemini.com Webmaster.
Very helpful and content specific questions to help prepare me for my interview!
Thank you
To the interviewgemini.com Webmaster.
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.