Unlock your full potential by mastering the most common Medical Decision-Making and Diagnostic Reasoning interview questions. This blog offers a deep dive into the critical topics, ensuring you’re not only prepared to answer but to excel. With these insights, you’ll approach your interview with clarity and confidence.
Questions Asked in Medical Decision-Making and Diagnostic Reasoning Interview
Q 1. Explain the process of formulating a differential diagnosis.
Formulating a differential diagnosis is a crucial step in medical decision-making. It’s essentially a systematic process of identifying all possible diseases or conditions that could explain a patient’s presenting symptoms and signs. Think of it like a detective solving a case – you start with the clues (symptoms) and build a list of potential suspects (diagnoses).
The process typically involves these steps:
- Data Collection: Thoroughly gather information from the patient’s history (including family history), perform a physical examination, and review any relevant investigations (lab results, imaging).
- Symptom Analysis: Analyze the patient’s symptoms, noting their character, onset, duration, and severity. For example, a ‘cough’ needs further clarification: Is it dry or productive? When did it start? Is it worse at night?
- Hypothesis Generation: Based on the collected data, generate a list of possible diagnoses. This involves considering the prevalence of diseases in the population, the patient’s risk factors, and the patterns of symptoms.
- Hypothesis Prioritization: Prioritize the diagnoses based on their likelihood, using clinical judgment and available evidence. Consider the pre-test probability – how common is this condition in a patient with this presentation?
- Diagnostic Testing: Select and order appropriate diagnostic tests to help rule in or rule out the most likely diagnoses. It’s important to use tests that have high sensitivity and specificity for the condition of interest.
- Diagnosis Confirmation/Refutation: Evaluate the results of the diagnostic tests, and adjust the differential diagnosis accordingly. Often, the process iteratively refines the list of possibilities until a definitive diagnosis is reached, or the most likely working diagnosis is established for management.
Example: A patient presents with chest pain. The differential diagnosis could initially include myocardial infarction, pericarditis, angina, pneumothorax, esophageal spasm, and musculoskeletal pain. Further investigation, such as an ECG and cardiac enzymes, would help narrow down the possibilities.
Q 2. Describe your approach to interpreting laboratory results.
Interpreting laboratory results requires careful consideration of several factors, going beyond simply looking at the numerical values. It’s about understanding the context of the results within the individual patient’s clinical picture.
- Reference Ranges: First, I always check if the values fall within the normal reference range provided by the laboratory. It’s crucial to remember that these ranges are population-based and may not perfectly represent an individual’s ‘normal’.
- Test Sensitivity and Specificity: I need to understand the characteristics of the test. High sensitivity means it’s good at detecting the condition when it’s present; high specificity means it rarely gives false positive results. This informs how to interpret positive and negative findings.
- Clinical Correlation: The most important aspect is correlating the lab results with the patient’s clinical presentation, history, and other investigation results. An abnormal lab value in isolation may not be significant; it’s the clinical picture as a whole that dictates meaning.
- Pre-Test Probability: Before receiving the lab results, I should already have an estimation of the likelihood of a particular diagnosis based on the patient’s clinical presentation. This pre-test probability helps in interpreting the post-test probability after considering the lab results.
- Potential for Error: I’m aware of the possibility of pre-analytical errors (e.g., sample collection, handling) and analytical errors (e.g., machine malfunction). If there are discrepancies or unexpected results, I’d repeat the test or seek further clarification.
Example: A slightly elevated white blood cell count might be insignificant in a healthy individual but could be crucial in a patient presenting with symptoms of infection. The context is everything.
Q 3. How do you evaluate the reliability and validity of diagnostic tests?
Evaluating the reliability and validity of diagnostic tests is fundamental to making informed decisions. Reliability refers to the consistency of the test, while validity refers to how accurately it measures what it’s intended to measure.
- Reliability: We assess reliability through measures like inter-rater reliability (do different clinicians get the same result?), intra-rater reliability (does the same clinician get the same result on repeat testing?), and test-retest reliability (does the test give consistent results over time?).
- Validity: Assessing validity involves multiple aspects:
- Content Validity: Does the test cover all aspects of the condition it aims to diagnose?
- Criterion Validity: Does the test correlate with a gold standard test (the most accurate method available)? This can be assessed through sensitivity (proportion of true positives identified) and specificity (proportion of true negatives identified).
- Construct Validity: Does the test measure the theoretical construct it is designed to measure?
Example: A new blood test for a specific cancer needs to demonstrate high sensitivity (few false negatives) and high specificity (few false positives) compared to a biopsy (the gold standard) to be considered valid and reliable. Studies evaluating these parameters are essential.
We use metrics such as positive and negative predictive values, likelihood ratios, and receiver operating characteristic (ROC) curves to further quantify test performance.
Q 4. What are the key elements of a well-structured clinical decision support system?
A well-structured clinical decision support system (CDSS) aims to improve the quality, efficiency, and safety of healthcare by providing clinicians with relevant information at the point of care. Key elements include:
- Knowledge Base: A comprehensive, up-to-date database of medical knowledge, including guidelines, research findings, and drug information. This might be structured using ontology and knowledge representation techniques.
- User Interface: An intuitive and user-friendly interface that seamlessly integrates into the electronic health record (EHR) system. It should be easily accessible and customizable to individual user preferences.
- Reasoning Engine: This core component processes information from the knowledge base and patient data to generate recommendations, alerts, or other decision support. This might employ Bayesian networks, rule-based systems, or machine learning algorithms.
- Alerting System: The system should alert clinicians to potential problems, such as drug interactions, allergy warnings, or abnormal lab results. Alerts should be prioritized and designed to minimize alert fatigue.
- Contextual Awareness: The CDSS should understand the context of the patient encounter, considering the patient’s history, current medications, and other relevant information.
- Evaluation and Feedback Mechanism: A system for monitoring the effectiveness of the CDSS and gathering feedback from clinicians. This is crucial for continuous improvement.
- Data Security and Privacy: Robust security measures to protect patient data and ensure compliance with relevant regulations.
A well-designed CDSS will not replace clinical judgment but augment it, helping clinicians make more informed and timely decisions.
Q 5. Discuss the role of Bayesian reasoning in medical diagnosis.
Bayesian reasoning is a powerful tool in medical diagnosis because it allows us to update our beliefs about the probability of a disease based on new evidence. It’s a probabilistic approach that starts with a prior probability (pre-test probability) and then modifies it based on the likelihood of observing the evidence given the disease (likelihood ratio) to arrive at a posterior probability (post-test probability).
Let’s break this down using Bayes’ Theorem:
P(Disease|Evidence) = [P(Evidence|Disease) * P(Disease)] / P(Evidence)
Where:
P(Disease|Evidence)is the posterior probability (probability of the disease given the evidence).P(Evidence|Disease)is the likelihood ratio (probability of observing the evidence given the disease).P(Disease)is the prior probability (pre-test probability of the disease).P(Evidence)is the probability of observing the evidence (this is often complex to calculate directly, but we can use the other elements of the equation).
Example: Imagine a patient presents with symptoms suggestive of a particular disease, which has a 5% prevalence (prior probability). A diagnostic test is performed, and its positive predictive value indicates a higher probability of having the disease when the test is positive. Using Bayesian reasoning, we can calculate the posterior probability considering both the prior probability and the test result. This allows for a more accurate assessment of the risk.
Bayesian reasoning helps us integrate prior knowledge with new data, leading to more refined and evidence-based diagnoses.
Q 6. How do you handle uncertainty in medical decision-making?
Uncertainty is inherent in medical decision-making. We rarely have all the information we need, and tests aren’t always perfect. Handling uncertainty effectively is crucial. Here’s my approach:
- Acknowledge and Quantify Uncertainty: I explicitly acknowledge the uncertainties involved, rather than pretending they don’t exist. This may involve considering multiple scenarios or ranges of probabilities.
- Use Probabilistic Reasoning: I utilize Bayesian reasoning, as previously described, to incorporate prior knowledge and new evidence in a probabilistic framework. This allows me to express diagnostic uncertainty quantitatively.
- Sensitivity Analysis: I explore how sensitive the decision is to variations in the input parameters (e.g., test results, patient history). This helps identify the critical pieces of information that need further clarification or investigation.
- Shared Decision-Making: I involve the patient in the decision-making process, clearly communicating the uncertainties and possible outcomes. I explain the tradeoffs between different treatment options, weighing benefits and risks.
- Seek Expert Consultation: If faced with significant uncertainty or a complex case, I consult with colleagues or specialists to obtain a broader perspective and leverage their expertise.
- Serial Monitoring: In situations where uncertainty remains after initial assessment, I implement a strategy of close monitoring and reassessment, allowing me to adjust the approach based on the patient’s response to treatment or the emergence of new information.
Handling uncertainty is not about eliminating it but about managing it responsibly, ensuring patient safety and optimal outcomes.
Q 7. Describe a situation where you had to make a critical decision under pressure.
During my residency, I was faced with a critically ill patient who presented to the emergency room with severe abdominal pain, hypotension, and signs of septic shock. The initial assessment was challenging because the patient was unstable, and the symptoms were non-specific. The differential diagnosis included a ruptured abdominal aortic aneurysm (a life-threatening condition), bowel perforation, and other less critical causes.
The pressure was immense because the patient’s condition was rapidly deteriorating. I had to make swift decisions, prioritizing immediate life-saving measures while simultaneously conducting rapid investigations to refine the diagnosis. We immediately started fluid resuscitation and broad-spectrum antibiotics while simultaneously obtaining imaging studies (ultrasound, CT scan). The initial ultrasound suggested a large abdominal aortic aneurysm, which increased the urgency of the situation.
With the help of senior colleagues, we rapidly proceeded to the operating room, and I participated in the emergency surgery. It turned out to be a ruptured AAA. The rapid assessment, communication, and decisive actions contributed significantly to a successful outcome, in which the patient’s life was saved.
This experience reinforced the importance of systematic clinical reasoning, even under high-pressure situations. It showed me the power of teamwork, the critical role of rapid data acquisition, and the need to prioritize life-saving interventions while continuing to refine the diagnostic process.
Q 8. How do you approach a patient presenting with ambiguous symptoms?
Ambiguous symptoms are a common challenge in medicine. My approach involves a systematic process prioritizing a thorough history and physical examination. I begin by actively listening to the patient, asking open-ended questions to understand their concerns and symptoms in detail. This includes exploring the symptom’s onset, duration, character, location, and any aggravating or relieving factors. A detailed review of systems helps identify potentially related symptoms that might not have been initially volunteered. The physical examination is tailored to the patient’s chief complaint and potential differential diagnoses. For example, if a patient presents with chest pain, the examination will focus on cardiovascular and respiratory systems, including auscultation of the heart and lungs, palpation of the chest, and assessment of vital signs. After this initial assessment, I develop a differential diagnosis – a list of possible conditions that could explain the patient’s symptoms. Laboratory tests, imaging studies (like X-rays, CT scans, or MRIs), and potentially specialist consultations are strategically used to narrow down the possibilities and arrive at a definitive diagnosis.
For instance, a patient complaining of fatigue could have underlying anemia, thyroid dysfunction, or depression. The history would reveal clues: anemia might present with pallor and shortness of breath, thyroid issues with weight changes or intolerance to cold, and depression with changes in mood or sleep patterns. Tests would then be ordered accordingly. The key is iterative refinement; as new information is obtained, the differential diagnosis is revised, leading to a more accurate diagnosis and treatment plan.
Q 9. Explain the concept of sensitivity and specificity in diagnostic testing.
Sensitivity and specificity are crucial metrics in evaluating diagnostic tests. Sensitivity refers to a test’s ability to correctly identify those with the disease (true positives). A highly sensitive test will rarely miss someone who has the disease. Specificity, on the other hand, measures the test’s ability to correctly identify those without the disease (true negatives). A highly specific test will rarely label someone who is healthy as diseased.
Let’s consider a blood test for a particular infection. A highly sensitive test means that if someone has the infection, the test will almost always be positive. However, it might also give some false positives in healthy individuals. Conversely, a highly specific test will rarely give a false positive, but it might miss some individuals with the infection (false negatives). The ideal test is both highly sensitive and highly specific, but this is often not achievable, necessitating a careful consideration of the trade-off between the two, particularly considering the prevalence of the disease and the consequences of missing a diagnosis versus giving a false positive.
Imagine screening for a rare but serious disease. You’d prioritize a highly sensitive test even if it has lower specificity, to minimize missing cases. Conversely, for a common but less serious condition, high specificity may be favored to reduce unnecessary treatment.
Q 10. How do you balance the benefits and risks of different treatment options?
Balancing benefits and risks is central to medical decision-making. It’s a shared decision-making process involving the patient, utilizing a structured approach. I begin by clearly outlining the potential benefits of each treatment option, considering factors like improved survival rates, symptom reduction, and quality of life enhancements. Simultaneously, I explain the potential risks associated with each option, including side effects, complications, and potential long-term consequences. This information is presented using clear and accessible language, avoiding medical jargon whenever possible.
For instance, if discussing cancer treatment, I’ll explain the potential efficacy of surgery, chemotherapy, and radiation in detail, but also describe the associated side effects, such as nausea, hair loss, and fatigue, alongside any potential long-term implications for fertility or organ function. The discussion also involves the patient’s values and preferences. What are their priorities? What level of risk are they willing to accept to achieve the potential benefits? Shared decision-making allows us to collaboratively decide on a treatment plan that aligns with the patient’s goals and values.
Q 11. Describe your approach to managing conflicting information from various sources.
Conflicting information is a reality in medicine. My strategy is to critically evaluate each source, considering its credibility, methodology, and potential biases. This means considering whether the source is peer-reviewed, the sample size of any study cited, and whether there are any known conflicts of interest. I look for consistent findings across multiple reputable sources. If discrepancies persist, I prioritize evidence from large, well-designed studies and systematic reviews. In situations where the evidence is truly conflicting or insufficient, I engage in discussions with colleagues, seeking their perspectives and expertise. Ultimately, I aim to make the best decision possible based on the available evidence and the individual patient’s clinical presentation. Transparency with the patient regarding the uncertainty and the decision-making process is key to maintaining trust and shared understanding.
For example, if two studies produce conflicting results regarding the effectiveness of a particular medication, I’d delve into the methodology of each study. Were the patient populations comparable? Were the study designs rigorous? Were there any biases introduced? These considerations will guide me in weighting the evidence from each source, and I’ll be sure to communicate this thought process to my patient.
Q 12. How do you stay current with the latest medical advances and guidelines?
Staying current is paramount in medicine. I utilize several strategies, including regularly reading peer-reviewed medical journals and participating in continuing medical education (CME) activities. I subscribe to reputable medical journals relevant to my specialty and actively search for publications on topics of interest. I attend conferences and workshops to learn about the latest research and advancements from leading experts. Online resources, like reputable medical websites and databases (e.g., PubMed), are frequently utilized to access the latest guidelines and clinical trial results. Membership in professional organizations also keeps me connected to the medical community, offering access to publications, updates, and networking opportunities to stay abreast of changes in clinical practice.
Additionally, I actively participate in journal clubs with colleagues, where we discuss recent publications and share our insights. This peer-to-peer learning is invaluable for staying updated and exchanging perspectives.
Q 13. How do you incorporate patient preferences into your decision-making process?
Patient preferences are central to my decision-making. I don’t view myself as solely making decisions for the patient, but rather with the patient. I ensure that patients are fully informed about their diagnosis, treatment options, and associated benefits and risks. This shared decision-making model involves open communication and a collaborative approach where the patient’s values, goals, and lifestyle preferences are considered. I employ tools like decision aids or shared decision-making tools to facilitate this process, providing patients with objective information to support their own informed choices. I always allow ample time for patients to ask questions, express concerns, and clarify any uncertainties they might have. The goal is to reach a consensus on a treatment plan that aligns with both the medical evidence and the patient’s individual needs and preferences.
For example, when discussing treatment for a chronic condition like diabetes, I would not only explain the medical options – medications, diet, exercise – but also engage the patient in discussing their lifestyle, work commitments, and personal preferences to find a plan that’s both effective and sustainable for them.
Q 14. Describe your experience with using clinical decision support tools.
I have extensive experience using various clinical decision support tools (CDSS). These tools range from simple calculators estimating risk of certain conditions based on patient characteristics to sophisticated systems that integrate patient data with guidelines and evidence-based recommendations to offer tailored treatment suggestions. I find CDSS particularly valuable for improving diagnostic accuracy, especially in areas where differential diagnoses are complex or require precise calculations. These tools can flag potential drug interactions, highlight relevant guidelines, and offer tailored recommendations based on the latest research. However, I use CDSS critically, understanding their limitations. I never rely solely on a CDSS’s recommendations. Instead, I consider the output in the context of the individual patient, their unique characteristics, and my clinical judgment. The CDSS is a valuable tool to support my decision-making process, not replace it.
For example, in managing a patient with heart failure, a CDSS might help optimize medication doses based on the patient’s ejection fraction and other relevant parameters, reducing the risk of adverse events. However, I still rely on my clinical assessment and understanding of the patient’s overall health to make the final determination regarding medication selection and dosage.
Q 15. How do you approach a diagnostic dilemma involving rare diseases?
Diagnosing rare diseases presents a unique challenge due to their low prevalence and often non-specific symptoms. My approach involves a systematic process combining clinical acumen with advanced investigative techniques. It begins with a thorough review of the patient’s history, focusing on seemingly insignificant details that might point towards an unusual pattern. This is followed by a comprehensive physical examination, paying close attention to subtle findings. I then utilize a structured approach to differential diagnosis, systematically considering both common and uncommon possibilities. This involves using diagnostic algorithms and clinical decision support tools.
Crucially, I leverage the power of collaborative consultation. I readily consult with specialists in relevant fields, such as geneticists, immunologists, or metabolic specialists, to broaden the diagnostic net. Furthermore, I utilize advanced diagnostic tools including genetic testing (whole exome sequencing, targeted gene panels), advanced imaging techniques, and specialized laboratory tests. Data from these investigations is critically analyzed, always mindful of the potential for false positives and negatives associated with rarer conditions. Finally, I work closely with the patient and their family, providing clear and honest communication throughout the diagnostic journey, understanding the emotional toll rare disease diagnoses can have.
For example, consider a patient presenting with progressive neurological symptoms and unusual skin lesions. While common neurological disorders might be considered initially, the atypical skin findings would trigger the consideration of rare genetic disorders affecting both the nervous system and integumentary system. This would necessitate genetic testing and collaboration with a geneticist.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Explain your understanding of evidence-based medicine and its application.
Evidence-based medicine (EBM) is the conscientious, explicit, and judicious use of current best evidence in making decisions about the care of individual patients. It’s a framework that integrates the best available research evidence with clinical expertise and patient values to provide optimal healthcare.
The application of EBM involves a systematic process: 1. Formulating a clinical question using the PICO framework (Patient, Intervention, Comparison, Outcome). 2. Searching for the best evidence using reliable databases like PubMed and Cochrane Library. 3. Critically appraising the evidence assessing its validity, reliability, and applicability. 4. Integrating the evidence with clinical expertise and patient preferences. 5. Evaluating the outcome of the intervention and adapting the approach as needed.
For instance, if a patient presents with hypertension, I would formulate a clinical question using PICO: In patients with hypertension (P), is ACE inhibitor therapy (I) more effective than thiazide diuretics (C) in lowering blood pressure (O)? I would then search for relevant clinical trials and meta-analyses to evaluate the evidence, comparing the effectiveness and side effects of both therapies. Ultimately, the chosen treatment would be tailored to the individual patient’s preferences, considering their comorbidities and risk factors.
Q 17. How do you critically appraise medical literature?
Critically appraising medical literature involves a structured evaluation of the study’s design, methodology, results, and conclusions to assess its validity and applicability to clinical practice. This involves several steps:
- Assessing the study design: Is it a randomized controlled trial (RCT), cohort study, case-control study, or other design? RCTs generally provide the highest level of evidence.
- Evaluating the methodology: Was the study population appropriately selected? Were there biases in the selection or allocation of participants? Were the measurements valid and reliable?
- Analyzing the results: Were the results statistically significant? Are the effect sizes clinically meaningful? Are the confidence intervals appropriately reported?
- Interpreting the conclusions: Do the conclusions accurately reflect the study findings? Are there any limitations that need to be considered? Is the study applicable to my patient population?
Tools such as the CASP checklists (Critical Appraisal Skills Programme) provide structured guidance for evaluating different study designs. I also consider the publication bias – the tendency for studies with positive results to be published more readily than those with negative results.
Q 18. How do you manage ethical dilemmas in medical decision-making?
Ethical dilemmas in medical decision-making frequently arise, requiring careful consideration of several ethical principles: autonomy, beneficence, non-maleficence, and justice. My approach involves a structured framework:
- Identify the ethical dilemma: Clearly define the conflict of values or principles involved.
- Gather relevant information: Obtain all relevant medical, social, and personal information from the patient and their family.
- Identify stakeholders: Determine who is affected by the decision (patient, family, healthcare team).
- Explore options: Identify potential courses of action and their ethical implications.
- Consult with colleagues: Seek advice from experienced colleagues, ethicists, or legal counsel.
- Make and document the decision: Justify the chosen course of action based on ethical principles and relevant evidence.
For example, a patient with a terminal illness may refuse life-sustaining treatment, exercising their autonomy. However, this decision might conflict with the principle of beneficence, which aims to do good for the patient. In such situations, I strive for shared decision-making, respecting patient autonomy while exploring ways to alleviate suffering and provide the best possible palliative care.
Q 19. Describe a situation where you had to revise your initial diagnosis.
I recall a patient presenting with symptoms suggestive of a common viral infection. My initial diagnosis was influenza. However, despite antiviral treatment, the patient’s condition worsened, and new symptoms emerged, including significant neurological changes. My initial assessment overlooked a rare autoimmune encephalitis.
The revised diagnosis was made after a detailed neurological examination, brain MRI revealing characteristic lesions, and positive autoantibody testing. This case highlighted the importance of reassessing the diagnosis when the initial treatment doesn’t produce the expected outcome, or when new symptoms develop. It emphasizes the dynamic nature of medical decision-making and the need for continued monitoring and reassessment.
Q 20. How do you communicate complex medical information to patients and families?
Communicating complex medical information requires clear, concise, and empathetic language tailored to the patient’s and family’s understanding. I utilize several strategies:
- Assess understanding: Begin by understanding the patient’s existing knowledge and learning style.
- Use plain language: Avoid medical jargon and technical terms whenever possible. If technical terms are necessary, explain them simply.
- Use visual aids: Diagrams, charts, and models can enhance understanding.
- Check for understanding: Regularly ask questions to ensure the information is being absorbed.
- Provide written information: Summarize key information in writing for later reference.
- Involve family members: Involve family members as appropriate, ensuring everyone understands the diagnosis, treatment plan, and prognosis.
I find that using analogies and metaphors can significantly improve understanding. For example, explaining the heart’s function by comparing it to a pump, or describing the immune system as the body’s defense force can help patients visualize complex concepts more effectively.
Q 21. How do you incorporate patient values and preferences into your decision-making process?
Incorporating patient values and preferences is central to shared decision-making, a cornerstone of modern medical practice. This means actively involving patients in the decision-making process, respecting their autonomy, and considering their unique values and circumstances.
I achieve this through open communication, actively listening to the patient’s concerns, beliefs, and preferences. I use tools like decision aids and shared decision-making frameworks to present treatment options clearly and allow patients to weigh the risks and benefits in light of their personal values. I empower them to make informed choices aligned with their goals and priorities, respecting their right to refuse or accept any proposed treatment.
For example, when discussing treatment options for cancer, I would discuss the potential benefits and side effects of each option, including its impact on their quality of life. If a patient prioritizes maintaining their mobility and independence, this would influence our discussion and the final treatment plan, even if an alternative option might offer a slightly higher chance of survival but with significantly increased side effects impacting their daily life.
Q 22. How do you manage disagreements with colleagues regarding patient care?
Disagreements among colleagues regarding patient care are inevitable, given the complexity of medicine and the variability in individual experiences and perspectives. My approach prioritizes a collaborative and respectful resolution, always keeping the patient’s best interests at the forefront. I begin by actively listening to my colleagues’ concerns, ensuring I understand their reasoning and the evidence supporting their viewpoints. I then clearly articulate my own position, presenting the supporting data and rationale for my recommendations. If a consensus isn’t immediately reached, I believe in seeking a neutral third opinion from a senior colleague or specialist, presenting all sides of the argument fairly. This ensures a balanced evaluation and a decision based on the most comprehensive evidence available. Ultimately, the goal is to arrive at a unified, evidence-based plan of care that is in the patient’s best interest.
For example, in a recent case involving a patient with atypical chest pain, a colleague advocated for immediate cardiac catheterization, while I felt further non-invasive testing was warranted. We openly discussed the patient’s presentation, risk factors, and the pros and cons of each approach. We both presented our reasoning, and ultimately, we agreed to conduct further non-invasive testing before proceeding with a potentially invasive procedure. This approach allowed us to reach a decision that we both felt comfortable with and prioritized patient safety.
Q 23. Describe your experience with using medical imaging to aid in diagnosis.
Medical imaging plays a crucial role in my diagnostic process. My experience encompasses a wide range of modalities including X-rays, CT scans, MRI, ultrasound, and fluoroscopy. I am proficient in interpreting images, correlating findings with clinical presentations, and integrating them into the overall diagnostic picture. For instance, in suspected appendicitis, ultrasound can visualize the inflamed appendix, guiding treatment decisions. Similarly, in stroke evaluation, a CT scan can quickly differentiate between ischemic and hemorrhagic stroke, informing treatment strategies. My expertise allows me to not only interpret images but also to select the appropriate imaging modality based on the clinical question and patient-specific factors like allergies or contraindications to certain contrast agents. I always emphasize the importance of considering the radiation dose in the selection of imaging, particularly in pediatric or pregnant patients, opting for lower dose alternatives when possible.
Further, I always integrate imaging findings with other clinical data – patient history, physical exam findings, and lab results – to arrive at a holistic diagnosis. An isolated imaging finding might be inconclusive, but when combined with other clinical data, it significantly contributes to a confident diagnosis. For example, a chest X-ray showing a consolidation may be suggestive of pneumonia, but only when coupled with the patient’s respiratory symptoms and blood tests confirming infection can a conclusive diagnosis be made.
Q 24. What are the limitations of diagnostic tests?
Diagnostic tests, while invaluable, are not infallible. They are subject to several limitations. The most important are sensitivity and specificity. Sensitivity refers to the test’s ability to correctly identify individuals with the disease, while specificity refers to its ability to correctly identify individuals without the disease. A highly sensitive test will have few false negatives but may have many false positives, whereas a highly specific test will have few false positives but may have many false negatives.
Furthermore, test results can be influenced by various pre-analytical factors, such as inadequate sample collection, improper storage, or delays in processing. Analytical factors, including the accuracy and precision of the test itself, also affect the reliability of results. Finally, post-analytical factors, such as incorrect interpretation or reporting of the results, can lead to misdiagnosis. Understanding these limitations is crucial for appropriate test selection, result interpretation, and ultimately, effective patient care. Consider a patient with suspected tuberculosis. The tuberculin skin test has high sensitivity but low specificity. A positive result suggests infection but requires further investigation to confirm. The converse is true for a negative result, which does not rule out tuberculosis, given the test’s low specificity. These limitations dictate a multifaceted approach to diagnosis.
Q 25. How do you address potential biases in clinical reasoning?
Cognitive biases can significantly impair clinical reasoning, leading to inaccurate diagnoses and inappropriate treatment. To mitigate this, I employ several strategies. First, I strive for conscious awareness of common biases such as anchoring bias (over-reliance on initial impressions), confirmation bias (seeking information confirming pre-existing beliefs), and availability bias (overestimating the likelihood of easily recalled diagnoses).
Second, I utilize structured approaches to clinical reasoning, like using diagnostic algorithms or checklists to systematically gather and analyze information. This helps minimize the influence of subjective judgments. Third, I actively seek feedback from colleagues, engaging in peer review and discussion of complex cases. This facilitates critical evaluation of my diagnostic reasoning and helps identify potential biases that may have gone unnoticed. Finally, I rely on evidence-based medicine, basing my decisions on well-established guidelines and research findings rather than gut feelings or anecdotal experiences. For example, in assessing a patient with symptoms suggestive of both anxiety and a heart condition, I might consciously check for anchoring bias – the tendency to focus primarily on one aspect (e.g., anxiety) without adequately investigating the other (e.g., cardiac disease). Employing structured approaches will help guide the investigation.
Q 26. How do you integrate patient history, physical examination findings, and laboratory data to reach a diagnosis?
Reaching an accurate diagnosis involves a systematic integration of patient history, physical examination findings, and laboratory data. I typically follow a structured approach, beginning with a thorough patient history, including the chief complaint, history of present illness, past medical history, family history, social history, and review of systems. This provides valuable context and generates hypotheses.
Next, a focused physical examination is performed, targeting systems relevant to the initial hypotheses. The findings from this examination refine or refute the initial hypotheses. Finally, I order relevant laboratory investigations to confirm or exclude specific diagnoses. The results of these investigations are then integrated with the history and physical examination findings to reach a comprehensive diagnosis. It’s a cyclical process, whereby new findings may lead to modification of the initial hypotheses. For example, a patient presents with fever, cough, and shortness of breath. The history suggests pneumonia. A physical examination reveals crackles in the lungs. Chest X-ray confirms the presence of consolidation in the lungs, supporting the pneumonia diagnosis. Blood tests reveal elevated white blood cell count and inflammatory markers, further solidifying the diagnosis.
Q 27. Describe your understanding of risk assessment and its role in medical decision-making.
Risk assessment is fundamental to medical decision-making. It involves identifying and quantifying the likelihood of adverse events or outcomes related to a patient’s condition, treatment, or lifestyle choices. This assessment relies on both clinical judgment and objective data, such as age, comorbidities, laboratory results, and imaging findings. It’s a dynamic process, continually updated as new information becomes available.
For example, in a patient with hypertension, risk assessment would consider factors like age, family history of cardiovascular disease, smoking status, cholesterol levels, and blood pressure control. This would inform decisions regarding lifestyle modifications and medication choices. The results help determine the severity of the risk and the urgency of intervention. A patient with high risk of cardiovascular events would require aggressive treatment compared to a low-risk patient. Tools like risk calculators and clinical guidelines often help in this process. Risk assessment facilitates shared decision-making by informing patients of potential benefits and risks, empowering them to actively participate in choices regarding their care.
Q 28. Explain the importance of continuous learning and improvement in medical decision-making.
Continuous learning and improvement are essential for effective medical decision-making. The field of medicine is constantly evolving, with new research, guidelines, and technologies emerging regularly. To maintain competence, I regularly engage in continuing medical education (CME), attending conferences, participating in workshops, and staying updated on relevant literature. This helps me remain abreast of the latest advancements and best practices.
Moreover, I actively seek feedback on my clinical performance, reflecting on my decisions and identifying areas for improvement. This could include reviewing cases with colleagues, seeking mentorship from experienced professionals, or engaging in self-reflection through keeping a clinical log. Furthermore, participating in quality improvement initiatives and utilizing feedback from patient satisfaction surveys allows me to identify areas where systems or individual practices might be enhanced for the betterment of patient care. The pursuit of continuous learning and improvement is not merely a professional obligation but a commitment to providing the highest quality of patient care.
Key Topics to Learn for Medical Decision-Making and Diagnostic Reasoning Interview
- Clinical Reasoning Frameworks: Understand and apply various frameworks like the hypothetico-deductive method, pattern recognition, and Bayesian reasoning to approach patient cases.
- Data Interpretation & Analysis: Practice interpreting various types of patient data (vital signs, lab results, imaging studies) and identifying relevant information to support clinical decisions. This includes understanding the limitations and biases inherent in data.
- Differential Diagnosis: Develop skills in constructing and refining differential diagnoses based on patient presentations, incorporating epidemiological factors and prevalence of conditions.
- Risk Assessment & Probability: Demonstrate your ability to assess and quantify risks associated with various diagnostic and treatment options, applying principles of probability and statistics.
- Evidence-Based Medicine: Show a thorough understanding of how to locate, critically appraise, and apply relevant medical literature to inform clinical decisions.
- Communication & Collaboration: Highlight your abilities in effectively communicating diagnostic reasoning, treatment plans, and uncertainties to patients and healthcare teams.
- Ethical Considerations: Discuss ethical dilemmas that frequently arise in clinical decision-making, demonstrating awareness of ethical principles and professional responsibility.
- Cognitive Biases in Clinical Decision-Making: Understand common cognitive biases (confirmation bias, anchoring bias, etc.) and how to mitigate their influence on clinical judgment.
- Practical Application: Be prepared to discuss specific case scenarios, showcasing your ability to apply these concepts to real-world clinical problems.
Next Steps
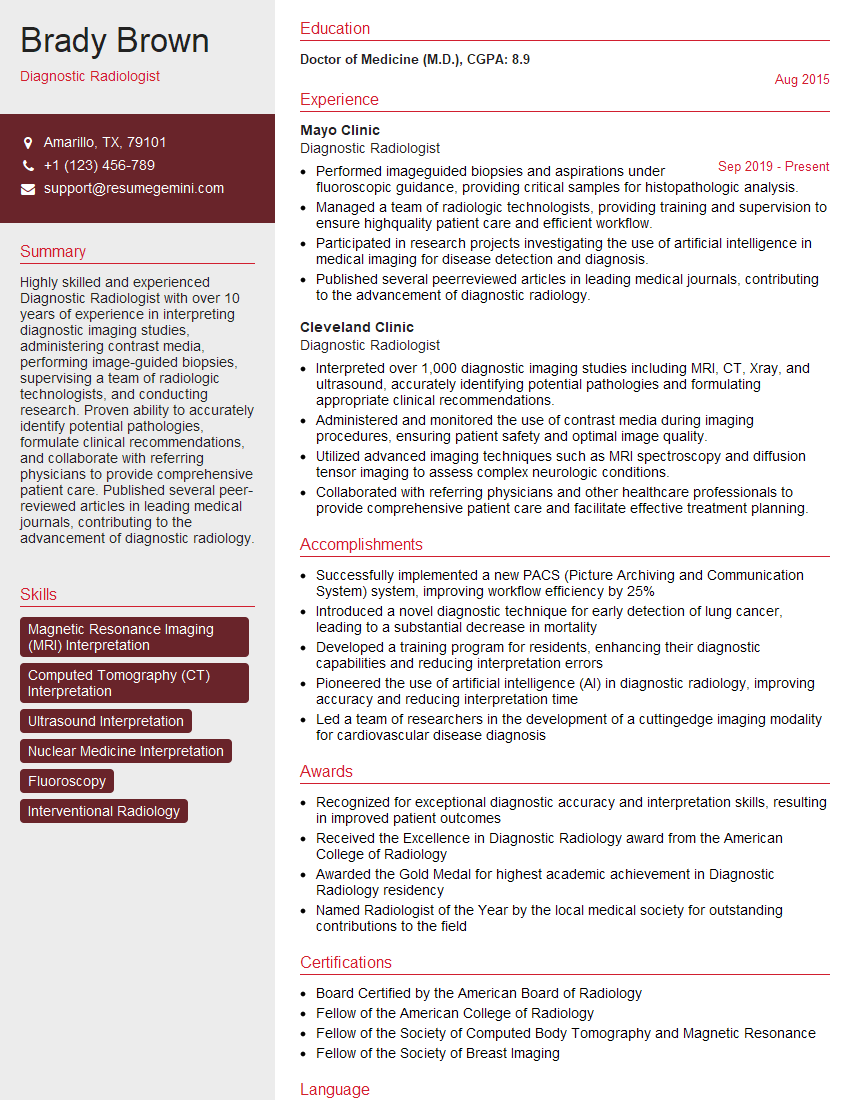
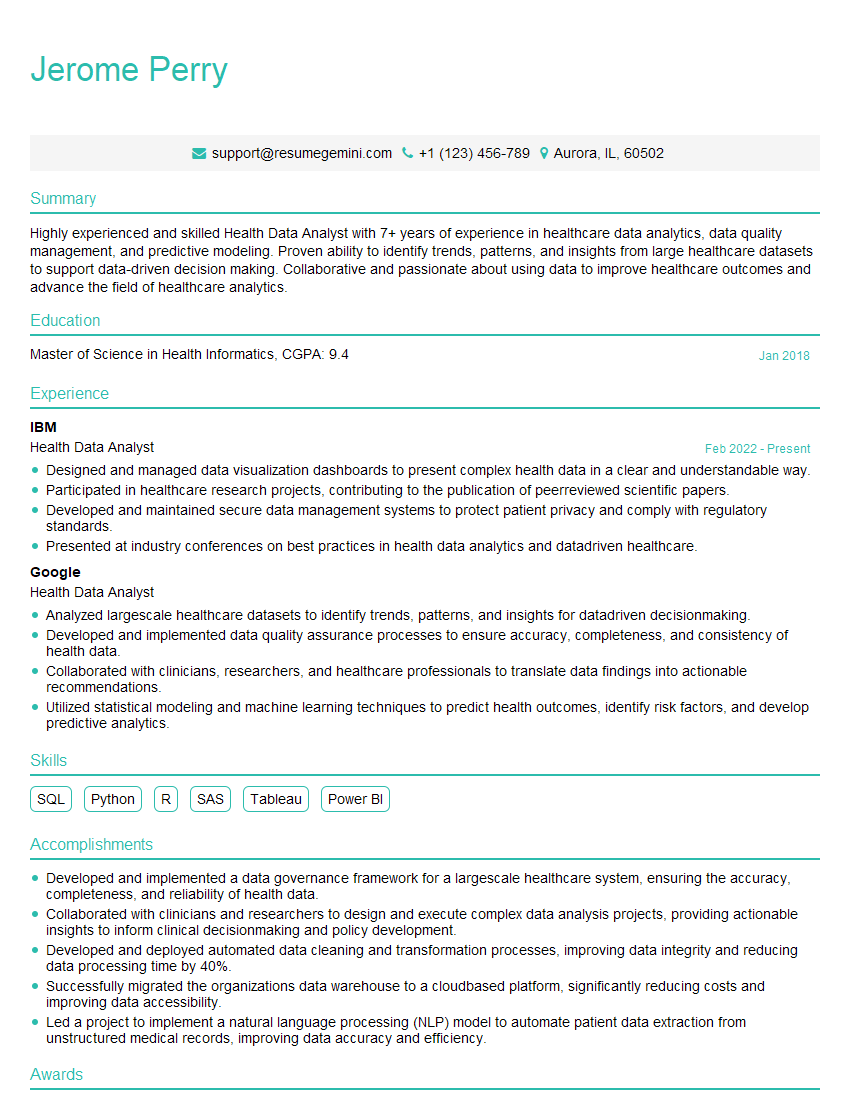
Mastering Medical Decision-Making and Diagnostic Reasoning is crucial for career advancement in healthcare. It demonstrates a high level of clinical competency and problem-solving skills, making you a valuable asset to any team. To stand out, a well-crafted resume is essential. An ATS-friendly resume increases your chances of getting noticed by recruiters. ResumeGemini is a trusted resource for building professional and effective resumes, ensuring your skills and experience shine through. ResumeGemini offers examples of resumes tailored to Medical Decision-Making and Diagnostic Reasoning to help you create a compelling application that showcases your expertise. Take the next step towards your dream career today!
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.