The right preparation can turn an interview into an opportunity to showcase your expertise. This guide to Histochemical and immunohistochemical staining techniques interview questions is your ultimate resource, providing key insights and tips to help you ace your responses and stand out as a top candidate.
Questions Asked in Histochemical and immunohistochemical staining techniques Interview
Q 1. Describe the process of tissue processing for histological examination.
Tissue processing for histological examination is a crucial step that prepares tissue samples for microscopic analysis. The goal is to preserve the tissue’s morphology and allow for proper staining. This multi-step process involves several key stages:
Fixation: This initial step prevents tissue autolysis (self-digestion) and bacterial degradation. Common fixatives include formalin (formaldehyde solution), which crosslinks proteins, maintaining tissue structure. The choice of fixative depends on the target tissue and the intended staining methods.
Dehydration: Water is removed from the tissue using a graded series of alcohols (e.g., 70%, 80%, 95%, 100%). This prepares the tissue for embedding in paraffin wax.
Clearing: The alcohol is replaced with a solvent that is miscible with both alcohol and paraffin wax, typically xylene or a similar agent. This process makes the tissue transparent.
Infiltration/Embedding: The tissue is infiltrated with molten paraffin wax, which fills the tissue spaces and provides support for sectioning. The wax-infiltrated tissue is then embedded in a paraffin block.
Sectioning: A microtome is used to cut thin (3-5 µm) sections of the paraffin block. These sections are then mounted onto glass slides.
Dewaxing and Rehydration: Before staining, the paraffin wax must be removed, and the tissue rehydrated through a series of decreasing alcohol concentrations to water.
Improper processing can lead to artifacts such as shrinkage, distortion, or loss of antigens, impacting the quality of the final histological assessment. For example, insufficient fixation can lead to poor preservation of cellular morphology and antigenicity.
Q 2. Explain the principles of Hematoxylin and Eosin (H&E) staining.
Hematoxylin and Eosin (H&E) staining is the gold standard for routine histological examination. It’s a basic staining technique that provides excellent contrast between different cellular components. Hematoxylin, a basic dye, stains basophilic structures (those with a negative charge) such as nuclei a dark purplish-blue color. Eosin, an acidic dye, stains eosinophilic structures (those with a positive charge) such as cytoplasm and extracellular matrix a pink color. This differential staining allows pathologists to easily identify various cellular components and tissue architectures.
The process is relatively simple. Sections are first stained with hematoxylin, then rinsed, and subsequently stained with eosin. Finally, the sections are dehydrated, cleared, and mounted with a coverslip for microscopic viewing.
For instance, in a tissue section stained with H&E, the nuclei of cells will be distinctly blue, and the cytoplasm will be pink, offering crucial information on cellular density, shape, and arrangement within the tissue.
Q 3. What are the different types of fixatives used in histology, and what are their advantages and disadvantages?
Several fixatives are used in histology, each with its advantages and disadvantages. The choice depends on the tissue type and the subsequent staining procedure.
Formaldehyde (Formalin): Widely used, relatively inexpensive, and penetrates tissues well. However, it can induce crosslinking artifacts and generate formaldehyde-induced fluorescence.
Glutaraldehyde: Excellent for electron microscopy, providing superior ultrastructural preservation. However, it penetrates tissues slowly and can mask certain antigens.
Bouin’s solution: Contains picric acid, acetic acid, and formaldehyde. Good for preserving tissue morphology and nuclear detail. However, picric acid is a hazardous substance and requires special handling.
Zenker’s solution: Contains mercuric chloride, potassium dichromate, and sodium sulfate. Excellent for preserving connective tissue and cell detail but requires special handling due to the toxicity of mercuric chloride.
Alcoholic fixatives (e.g., methanol, ethanol): Good for cytology preparations and rapid fixation but may cause shrinkage artifacts.
For example, in situations where ultrastructural detail is crucial, glutaraldehyde would be preferred. Conversely, if cost-effectiveness and good overall morphology are priorities, formalin is usually the method of choice.
Q 4. Explain the process of immunohistochemical staining, including antigen retrieval techniques.
Immunohistochemistry (IHC) is a powerful technique used to visualize specific proteins within tissue sections using antibodies. The process involves several key steps:
Antigen Retrieval: This step is crucial for many IHC procedures as formalin fixation can mask epitopes (the antigen binding sites). Methods include heat-induced epitope retrieval (HIER) using a pressure cooker or microwave, or enzymatic retrieval using enzymes like protease. The choice of method depends on the target antigen.
Blocking: Non-specific binding of antibodies to the tissue is blocked using agents such as normal serum or avidin/biotin blocking solutions. This minimizes background staining.
Incubation with Primary Antibody: The tissue section is incubated with the primary antibody, which is specific to the target protein. This step allows for the antibody to bind to its antigen.
Detection System: The detection system uses secondary antibodies conjugated to enzymes (e.g., horseradish peroxidase, alkaline phosphatase) or fluorescent molecules. These secondary antibodies bind to the primary antibody, allowing visualization of the target protein.
Chromogen Development (for enzyme-based systems): The enzyme converts a chromogen substrate into a colored precipitate, allowing for visualization of the antigen at the microscopic level.
Counterstaining: A counterstain (like hematoxylin) is often used to visualize the tissue architecture.
Mounting: The stained section is mounted with a coverslip.
For instance, HIER is often necessary when using formalin-fixed tissue for detecting certain proteins. Using the wrong retrieval method can result in no or weak staining.
Q 5. What are the different types of immunohistochemical detection systems?
Various immunohistochemical detection systems are available, each with its advantages and disadvantages:
Direct Method: The primary antibody is directly conjugated to an enzyme or fluorophore. This method is simple but less sensitive than indirect methods.
Indirect Method: A secondary antibody, which recognizes the primary antibody, is conjugated to an enzyme or fluorophore. This method amplifies the signal, resulting in higher sensitivity.
Avidin-Biotin-Peroxidase Complex (ABC): A very sensitive method that uses biotinylated secondary antibodies and avidin-biotin complex to amplify the signal. However, endogenous biotin in some tissues can lead to background staining.
Polymer-based detection systems: These systems conjugate multiple enzymes or fluorophores to a polymer that binds to the secondary antibody, further amplifying the signal and reducing background staining.
The choice of detection system often depends on the abundance of the target protein, the desired sensitivity, and the potential for background staining. For example, the ABC method might be avoided in tissues with high endogenous biotin.
Q 6. How do you troubleshoot problems encountered during immunohistochemical staining, such as weak or non-specific staining?
Troubleshooting IHC is a critical skill. Weak or non-specific staining can result from various factors:
Insufficient Antigen Retrieval: Optimize antigen retrieval method (HIER vs. enzymatic, temperature, time).
Antibody Problems: Use a new antibody batch, check antibody concentration and dilution, and verify antibody specificity.
Blocking Inefficiency: Use a longer blocking time or try a different blocking solution.
Improper Antibody Incubation: Ensure optimal incubation time and temperature. Increase incubation time for weak staining.
Detection System Issues: Ensure detection reagents are fresh and properly diluted. Try a different detection system.
Endogenous Enzyme Activity: Use enzyme blockers to inhibit endogenous peroxidase or alkaline phosphatase activity.
High Background: Reduce the concentration of primary or secondary antibodies, optimize blocking steps, use more stringent washes.
A systematic approach, starting with the simplest solutions (e.g., checking reagent concentration), and progressing to more complex solutions (e.g., optimizing antigen retrieval) is recommended. Keeping detailed records of each step is essential for effective troubleshooting.
Q 7. Describe the importance of positive and negative controls in immunohistochemistry.
Positive and negative controls are essential in IHC to validate the results and ensure the specificity of the staining.
Positive Control: A tissue sample known to express the target protein is included in the staining procedure. This serves to confirm that the staining method is working correctly and that the reagents are functional. If the positive control doesn’t stain, there’s an issue with the staining protocol.
Negative Control: A tissue sample that does not express the target protein, or a section stained with omission of primary antibody, is included. This helps to assess the level of non-specific binding. Positive staining in the negative control indicates non-specific binding, necessitating troubleshooting.
For example, in an IHC experiment targeting a specific cancer marker, a positive control might be a tissue section known to express this marker, while a negative control might be a normal tissue sample. The absence of staining in the negative control ensures that the observed positive staining in the experimental samples is specific to the target protein.
Q 8. What are the common artifacts observed in histological sections, and how can they be avoided?
Histological sections, while aiming for perfect tissue representation, often suffer from artifacts – imperfections that distort the true image. These can arise during any stage of the process, from tissue collection to staining. Common artifacts include:
- Folding/Tears: These are visible creases or breaks in the section, often resulting from improper handling during embedding or sectioning. Prevention involves careful tissue handling and using a sharp blade on the microtome.
- Compression: The tissue can be squeezed during sectioning, resulting in uneven thickness and distorted structures. This is less common with modern microtomes and can be mitigated by adjusting the microtome settings.
- Chatter: A vibrating or uneven cut, creating a ‘wavy’ appearance. This usually points to a blunt blade, improper microtome settings, or vibrations in the environment. Regularly changing the blade and ensuring a stable work surface are crucial.
- Shrinkage/Expansion: Changes in tissue volume due to processing reagents. Careful dehydration and embedding techniques minimize this. Using proper fixatives and standardized protocols is key.
- Precipitation of Stain: Crystals or uneven staining due to poor quality reagents or inadequate rinsing. Using fresh, high-quality reagents and following rigorous washing protocols resolves this.
- Sectioning Problems: Incomplete sections or excessively thick/thin sections, again largely dependent on microtome settings and blade sharpness.
Avoiding artifacts requires meticulous attention to detail at each step: proper fixation, careful processing, sharp microtome blades, appropriate embedding, and precise staining protocols. Regular maintenance of equipment and a good understanding of the underlying principles of each step are crucial for minimizing these imperfections.
Q 9. Explain the principles of in situ hybridization (ISH).
In situ hybridization (ISH) is a powerful technique used to visualize the location of specific nucleic acid sequences (DNA or RNA) within cells and tissues. It works by using a labeled probe – a short, single-stranded DNA or RNA sequence complementary to the target sequence.
The principle is simple: complementary base pairing. The labeled probe is introduced to the tissue section. If the target sequence is present, the probe will hybridize (bind) to it, forming a stable double-stranded structure. The label on the probe allows for detection of the hybridized probe, directly indicating the location of the target sequence.
Different labels are used, including fluorescent dyes (fluorescence in situ hybridization or FISH), radioactive isotopes (radioactive ISH), or enzymes (enzyme ISH). The choice of label dictates the detection method. Fluorescent labels are viewed under a fluorescence microscope, while enzymatic labels require an additional substrate to produce a visible color reaction. ISH is widely used in research and diagnostics to study gene expression, detect viral infections, and analyze chromosomal abnormalities.
Q 10. What is the difference between direct and indirect immunofluorescence?
Both direct and indirect immunofluorescence are techniques used to detect specific antigens in tissues using fluorescently labeled antibodies. The key difference lies in how the fluorescence is delivered:
- Direct Immunofluorescence: A fluorescently labeled primary antibody directly binds to the target antigen. This method is simpler and faster but usually less sensitive.
- Indirect Immunofluorescence: Uses an unlabeled primary antibody that binds to the target antigen, followed by a fluorescently labeled secondary antibody that binds to the primary antibody. This amplification step significantly increases sensitivity, allowing for brighter signals and detection of smaller amounts of antigen. It also offers greater flexibility, as multiple secondary antibodies can be used with the same primary antibody.
Imagine it like this: direct immunofluorescence is like directly attaching a light bulb to the target (antigen). Indirect immunofluorescence is like attaching a light switch (primary antibody) to the target, and then connecting a powerful light bulb (secondary antibody) to the switch. The secondary antibody method makes the light brighter.
Q 11. How do you assess the quality of histological sections?
Assessing the quality of histological sections involves a multi-faceted evaluation that considers both technical aspects and the overall informative value. Key parameters include:
- Tissue Morphology: Are the tissues well-preserved and properly oriented? Are cellular details clearly visible?
- Section Thickness and Uniformity: A consistent thickness allows for accurate interpretation. Uneven sections indicate problems during microtomy. This is checked microscopically and also by assessing the ribbon of sections created on the microtome.
- Artifact Presence: The presence and extent of artifacts (folding, tears, chatter, shrinkage, etc.) should be noted. These artifacts can lead to misinterpretation of results.
- Stain Quality: Is the staining even and of appropriate intensity? Are there any precipitates or background staining?
- Overall Clarity and Resolution: Are the cellular structures well-defined? Can you clearly differentiate different cell types and tissue components?
A good-quality section will display well-preserved tissue architecture, even staining, minimal artifacts, and optimal resolution, allowing for accurate and reliable analysis. Documentation, including photographic records, is crucial in quality assessment.
Q 12. What are the safety precautions you need to take when working with histological stains and chemicals?
Working with histological stains and chemicals requires stringent safety precautions due to their potential toxicity and hazards. These include:
- Personal Protective Equipment (PPE): Always wear appropriate PPE, including lab coats, gloves (nitrile or similar), eye protection (goggles), and face masks, especially when handling volatile or hazardous substances.
- Proper Ventilation: Work in a well-ventilated area or under a fume hood, especially when dealing with volatile solvents such as xylene and alcohol. This helps to minimize inhalation risks.
- Safe Handling of Chemicals: Follow the manufacturer’s instructions carefully. Always handle chemicals with care, avoiding spills and splashes. Label all containers properly.
- Waste Disposal: Dispose of chemical waste according to the institutional guidelines and regulations. Many histological stains and solvents are considered hazardous waste.
- Emergency Procedures: Familiarize yourself with emergency procedures in case of spills or accidents. Know the location of safety showers, eyewash stations, and fire extinguishers.
- Training and Education: Receive appropriate training on the safe handling and use of histological stains and chemicals before undertaking any procedures.
Safety is paramount in a histology lab. Adherence to these precautions significantly reduces the risks of exposure and potential health hazards. Regular safety training and awareness are essential.
Q 13. Describe your experience with different types of microtomes.
My experience encompasses a range of microtomes, from rotary to cryostats, reflecting diverse needs in tissue processing. Rotary microtomes are workhorses for paraffin-embedded tissues, allowing for precise sectioning at various thicknesses. I’m proficient in optimizing settings such as feed rate and cutting angle to obtain high-quality sections, minimizing artifacts like compression and chatter. I’ve extensively used different blade types (disposable, steel) and understand their impact on section quality.
Furthermore, I’m skilled in using cryostats for frozen sections, crucial for immunofluorescence and rapid diagnostics where speed is essential. This involves optimizing the freezing process, adjusting the cryostat temperature, and mastering techniques to avoid ice crystal formation and ensure optimal section quality. Experience with ultramicrotomes is limited but I understand their application in electron microscopy.
In each case, proper maintenance, including regular cleaning and lubrication, is essential for optimal performance and section quality. Proficiency across various microtome types allows for flexibility and adaptability to diverse research and diagnostic needs.
Q 14. What is your experience with digital pathology?
My experience with digital pathology is steadily growing. I am familiar with whole slide image scanners and their integration into laboratory workflows. I understand the advantages of digital pathology, including improved accessibility, remote consultations, and quantitative analysis capabilities. I’m adept at navigating digital pathology software, viewing and analyzing whole slide images, and utilizing image analysis tools for quantitative measurements.
Moreover, I have experience in image management and archiving, recognizing the importance of data security and efficient storage of large image datasets. I understand the growing role of artificial intelligence (AI) in digital pathology, including the application of machine learning for image analysis and automated diagnosis. While still developing my expertise in AI-driven analyses, I keep abreast of latest developments in this field. My ongoing professional development includes exploring advanced image analysis techniques and integrating them into routine workflow for enhanced diagnostics and research.
Q 15. How do you maintain quality control in a histology laboratory?
Maintaining quality control in a histology lab is paramount for accurate diagnoses and reliable research. It’s a multifaceted process involving meticulous attention to detail at every stage, from tissue acquisition to final reporting. We employ a robust system encompassing several key aspects:
- Reagent Quality Control: We utilize validated reagents and strictly adhere to manufacturers’ instructions and expiration dates. Regular testing of reagents (e.g., verifying pH, concentration) is implemented using control slides to ensure consistent staining quality. We maintain detailed logs of reagent preparation, usage, and quality control results.
- Instrumentation Maintenance: Our microtomes, stainer, and other instruments undergo regular preventative maintenance and calibration according to a strict schedule. We maintain meticulous records of service and calibration to ensure optimal performance and minimize technical errors. This includes daily checks of equipment functions and prompt reporting of any malfunctions.
- Proficiency Testing: Participation in external quality assurance programs (EQA) is vital. These programs provide blind samples, allowing us to compare our results with those of other labs and identify areas for improvement. This provides objective assessment of our performance and highlights any biases or inconsistencies.
- Internal Quality Control: We incorporate positive and negative controls in every staining batch. This helps to monitor the staining process, validate the specificity of our antibodies, and identify any issues with reagent performance or staining technique. A dedicated QC log tracks these controls.
- Personnel Training and Competency: Our team undergoes regular training and competency assessments to maintain a high level of expertise. This ensures consistency in technique and minimizes human error. We have detailed Standard Operating Procedures (SOPs) for every process.
- Record Keeping: Comprehensive documentation is critical. We meticulously record every step of the process, including specimen identification, staining protocols, and results. This allows us to track potential sources of error and ensures traceability.
For instance, during one EQA round, we identified a slight variation in our hematoxylin staining. By analyzing our logs, we traced the problem to a recent batch of hematoxylin that was slightly off in pH. This highlighted the importance of our rigorous reagent control measures.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Explain your understanding of different types of microscopy used in histology.
Histology utilizes various microscopy techniques to visualize tissue structures. The choice of microscopy depends on the specific application and the desired level of detail.
- Brightfield Microscopy: This is the most common technique, utilizing transmitted light to visualize stained tissue sections. It’s simple, widely available, and suitable for routine histological examination. We use brightfield microscopy for the majority of our histological and immunohistochemical stainings.
- Fluorescence Microscopy: This technique uses fluorescent dyes or antibodies to visualize specific structures or molecules within the tissue. It’s crucial for immunofluorescence studies, where fluorescently labeled antibodies bind to target proteins. For example, we frequently use immunofluorescence to identify specific cell types in tissue sections.
- Confocal Microscopy: A specialized type of fluorescence microscopy that provides high-resolution optical sections of thick specimens. It eliminates out-of-focus light, resulting in clearer images. We use confocal microscopy for advanced research projects requiring detailed three-dimensional visualization of tissue architecture.
- Electron Microscopy (Transmission and Scanning): These techniques provide much higher resolution than light microscopy, allowing visualization of subcellular structures. Transmission electron microscopy (TEM) is used to study the ultrastructure of cells and tissues, while scanning electron microscopy (SEM) provides three-dimensional surface images. We utilize electron microscopy in collaboration with other departments for highly specialized investigations.
The selection of the appropriate microscopy technique is crucial for obtaining meaningful and accurate results. For instance, while brightfield microscopy might suffice for routine diagnosis, confocal microscopy may be necessary to analyze complex interactions between cells in a tumor microenvironment.
Q 17. Describe your experience with automated staining systems.
I have extensive experience with automated staining systems, having worked with several models from different manufacturers. These systems offer significant advantages over manual staining, including increased throughput, improved consistency, and reduced technician workload. They typically incorporate features such as:
- Automated reagent dispensing: Precise and consistent delivery of reagents, minimizing variations between slides and batches.
- Precise timing and temperature control: Ensures optimal staining conditions, leading to higher quality results.
- Washing and rinsing cycles: Automated washing steps reduce human error and ensure thorough removal of excess reagents.
- Slide handling and tracking: Systems automatically track and manage slides, minimizing the risk of misidentification or loss.
In my previous role, we transitioned from manual staining to an automated system. This resulted in a significant increase in our daily processing capacity – we were able to process nearly double the number of slides per day. More importantly, it dramatically improved the consistency and reproducibility of our staining results. The reduction in manual steps reduced human error related to timing or reagent handling. However, regular maintenance and quality control of the automated system are essential for optimal performance. For instance, we have established a detailed maintenance log and proactively address any glitches or alerts to ensure smooth and consistent operation.
Q 18. How do you interpret immunohistochemical staining results?
Interpreting immunohistochemical (IHC) staining results requires careful consideration of several factors.
- Staining Intensity: The intensity of staining (e.g., weak, moderate, strong) indicates the abundance of the target antigen in the tissue.
- Staining Localization: The location of the staining within the tissue provides critical information about the distribution and cellular expression of the antigen. For example, nuclear staining versus cytoplasmic staining implies different subcellular localization of the protein.
- Specificity: The specificity of the antibody is paramount. Positive and negative controls are crucial to assess non-specific binding and ensure the staining is indeed targeting the intended antigen. Poor antibody specificity can lead to false positive or negative results.
- Tissue Morphology: The overall tissue morphology and architecture must be considered in the context of the IHC staining. This provides anatomical context for the protein localization.
- Clinical Correlation: IHC results are always interpreted in the context of the patient’s clinical history, other diagnostic findings, and the overall clinical picture.
For example, strong and diffuse nuclear staining of Ki-67 in a breast biopsy is indicative of high proliferative activity and suggests a more aggressive tumor. But this result should be interpreted along with other markers such as estrogen receptor, progesterone receptor, and HER2 status to fully understand tumor biology and guide treatment decisions.
Q 19. Explain the importance of proper tissue embedding techniques.
Proper tissue embedding is crucial for producing high-quality tissue sections suitable for histological examination. The embedding medium, typically paraffin wax, provides support and protection during sectioning, preventing tissue damage and ensuring the creation of thin, uniform sections.
- Tissue Processing: The tissue undergoes dehydration and infiltration with paraffin wax. This process replaces water with wax, making the tissue firm and facilitating sectioning. Inadequate dehydration can lead to sectioning artifacts, like cracks or crumbly sections.
- Orientation: Careful orientation of the tissue within the cassette is essential to obtain sections in the desired plane. Incorrect orientation can hinder the accurate assessment of tissue architecture and cellular relationships. For example, embedding a biopsy lengthwise versus crosswise drastically alters the appearance of the sections and will impact the diagnosis.
- Cassette Labeling: Accurate and legible labeling of cassettes is crucial for tracking specimens and avoiding errors in processing and sectioning. A unique identifier is assigned to each cassette and carefully documented in the lab information system.
- Paraffin Quality: Using high-quality paraffin wax is important for ensuring uniform embedding and easy sectioning. Old or improperly stored paraffin wax may result in brittle sections or difficulty obtaining consistent thickness.
- Embedding Technique: Proper embedding techniques ensure complete infiltration of the tissue with paraffin, eliminating air bubbles and creating a uniform block. Air bubbles will lead to irregularities during sectioning.
Imagine trying to slice a soft, wet sponge – it would be impossible to get nice, thin, even slices! Embedding provides the necessary structural support so that we can obtain high-quality sections suitable for microscopic analysis.
Q 20. What is your experience with special stains (e.g., PAS, silver stains)?
I have extensive experience with various special stains, including Periodic Acid-Schiff (PAS) and silver stains. These stains highlight specific tissue components that are not readily visualized with routine hematoxylin and eosin (H&E) staining.
- PAS Stain: This stain is used to detect carbohydrates and glycoproteins. It’s commonly used to identify fungi, glycogen, and basement membranes. The magenta color produced by PAS staining is particularly useful in diagnosing conditions like glycogen storage diseases or identifying fungal infections.
- Silver Stains: These stains are used to visualize various tissue components, including nerve fibers, reticulin fibers, and microorganisms like spirochetes. Different types of silver stains exist, each with specific applications. For example, we routinely use Gomori’s methenamine silver stain to highlight the presence of fungi in tissue.
- Other Special Stains: I also have experience with other stains like trichrome stains (e.g., Masson’s trichrome), which differentiate collagen from other tissue components, and oil red O stain, which is used to identify fats and lipids. The choice of special stain depends on the specific diagnostic question.
For instance, in a case of suspected Whipple’s disease, a PAS stain would be used to identify the presence of *Tropheryma whipplei*, a bacterium that stains strongly positive with PAS. Without this stain, the diagnosis would be significantly more challenging.
Q 21. How do you troubleshoot problems with tissue sectioning?
Troubleshooting problems with tissue sectioning requires a systematic approach, considering various potential causes.
- Blade Issues: A dull or damaged blade is the most frequent cause of sectioning problems, resulting in compressed, torn, or otherwise poor-quality sections. Inspect the blade under a microscope or replace it if necessary. The angle of the blade to the block is also crucial, with even a minor adjustment impacting results significantly.
- Paraffin Block Issues: Cracks, irregularities, or air bubbles in the paraffin block can cause difficulties during sectioning. Check the paraffin block for any issues. If the block is cracked, it’s likely that the tissue wasn’t properly processed or embedded.
- Microtome Adjustments: Incorrect microtome settings, such as the angle of the blade or the feed rate, can result in poor-quality sections. Check and adjust the microtome settings according to the manufacturer’s instructions and the block characteristics.
- Temperature and Humidity: Extreme temperatures or humidity can affect the paraffin block’s consistency, making it more difficult to section. Maintain the laboratory at a stable temperature and humidity.
- Tissue Processing Issues: Problems during tissue processing, such as inadequate dehydration or infiltration, can lead to poor-quality sections. Review the processing steps carefully and check for any abnormalities in the processing protocol.
A systematic approach is key. For example, if sections are consistently tearing, I would first check the blade, then the block for cracks, and finally the microtome settings. Documenting the troubleshooting steps is also important, allowing for identification of recurring problems and improvements in procedures.
Q 22. What is your understanding of different antigen retrieval methods?
Antigen retrieval is a crucial step in immunohistochemistry (IHC) where we aim to unmask epitopes (the specific part of an antigen that an antibody recognizes) that have been masked during tissue processing. This masking often occurs due to formalin fixation, which creates cross-links between proteins, hindering antibody binding. Several methods exist, each with its strengths and weaknesses.
- Heat-Induced Epitope Retrieval (HIER): This is the most common method, involving heating tissue sections in a specific buffer (e.g., citrate buffer, EDTA buffer). The heat breaks the cross-links, exposing the epitopes. The choice of buffer is critical; citrate buffer is generally milder and suitable for many antigens, while EDTA is more effective for certain recalcitrant epitopes. For example, I’ve found citrate buffer works well for most nuclear antigens, while EDTA is often preferred for membrane proteins.
- Enzyme-Induced Epitope Retrieval (EIER): This method uses enzymes like proteinase K or trypsin to digest proteins surrounding the epitopes, thereby uncovering them. This is a gentler approach compared to HIER, reducing the risk of antigen degradation. However, it requires careful optimization to avoid over-digestion, which could lead to loss of tissue morphology or antigen.
- Microwave Retrieval: This is a type of HIER where tissue sections are heated in a microwave oven. It’s a fast method but requires careful monitoring to prevent overheating and tissue damage. Different microwave settings and heating times need to be optimized depending on the antigen and tissue type.
The choice of antigen retrieval method depends on the specific antigen, tissue type, and antibody used. Often, optimization is needed, involving experimenting with different buffers, temperatures, and times. For instance, I once had to optimize the retrieval method for a particular antibody targeting a membrane protein. After multiple trials with different HIER buffers and times, I finally obtained strong and consistent staining using EDTA buffer at 95°C for 20 minutes.
Q 23. Describe your experience with image analysis software used in histology.
I have extensive experience with various image analysis software packages commonly used in histology, including ImageJ/Fiji, Aperio ImageScope, and HALO. These programs allow for quantitative analysis of histological data, going beyond simple visual assessment. ImageJ/Fiji, for instance, is open-source and highly versatile, allowing for customization through plugins. I often use it for tasks like cell counting, measurement of tissue areas, and intensity quantification. Aperio ImageScope is a powerful platform well-suited for high-throughput analysis, particularly with whole-slide images. Its automated features are very useful in large-scale studies.
HALO, on the other hand, offers advanced features like machine learning algorithms for automated image segmentation and classification. I’ve used HALO for complex analyses, such as analyzing tumor microenvironment and immune cell infiltration. For example, I once used HALO to quantify the density of CD8+ T cells in tumor samples, which provided valuable information on the patient’s immune response.
My proficiency in these software packages allows me to accurately quantify and analyze histological data, thereby enhancing the objectivity and reproducibility of research findings. The choice of software depends on the complexity of the analysis and the available resources. The ability to seamlessly navigate and interpret data from different platforms is, in my opinion, crucial for any histologist.
Q 24. How do you handle and store histological specimens appropriately?
Proper handling and storage of histological specimens are paramount to maintain the integrity of the samples and ensure reliable results. The entire process, from tissue collection to archival storage, must adhere to stringent protocols. Immediately after surgical removal, tissues intended for histological processing are usually fixed in 10% neutral-buffered formalin (NBF), a common fixative that prevents tissue degradation and preserves tissue architecture. The fixation time is crucial, usually 12-24 hours for routine histology. Over-fixation leads to hardening and difficult sectioning, while under-fixation can result in poor tissue preservation.
After fixation, tissues undergo processing through a series of alcohol and xylene solutions, which remove water and embed the tissue in paraffin wax for ease of sectioning. These paraffin blocks are stored at room temperature and are stable for many years. Frozen tissue sections, used for immunofluorescence or some enzymatic studies, require storage at -80°C to prevent degradation and ice crystal formation. Proper labeling with patient identifiers, date, and tissue type is crucial, ensuring traceability and compliance with ethical and regulatory guidelines. Furthermore, regular quality control checks are performed to monitor fixative effectiveness, processing quality, and storage conditions.
Q 25. What is your understanding of the ethical considerations in handling patient samples?
Ethical considerations are paramount when handling patient samples. The fundamental principle is respect for patient autonomy and privacy. All procedures must adhere to strict regulations and guidelines, such as HIPAA (in the US) and similar data protection laws in other countries. Informed consent is essential; patients must be fully aware of the purpose of the sample collection and how the data will be used. Anonymization of samples, whenever possible, protects patient confidentiality. Strict adherence to chain of custody ensures sample integrity and traceability. This includes detailed documentation at each stage, from collection to analysis and disposal.
Data security is also vital, employing secure storage methods for both physical samples and digital data. Ethical research practices are essential, and researchers must ensure that all data are treated responsibly, respecting patient dignity and privacy. Any deviation from established ethical guidelines can have serious legal and reputational consequences. For example, I’ve personally been involved in developing and implementing an IRB-approved protocol for a study involving patient tissue samples, ensuring all ethical requirements were meticulously adhered to.
Q 26. Explain your experience with different types of mounting media.
Mounting media are crucial for preserving stained histological sections on slides, preventing fading and improving the clarity of the images. The choice of mounting media depends on the staining technique used. Some common types include:
- Aqueous Mounting Media: Suitable for water-based stains, like hematoxylin and eosin (H&E). These media are generally less expensive, but might not be ideal for long-term preservation or fluorescence microscopy.
- Synthetic Resinous Mounting Media: These are widely used for permanent mounts and offer better protection against fading. Examples include DPX (distrene, plasticizer, xylene) and Permount. They provide excellent clarity and refractive index matching, improving image quality.
- Fluorescence Mounting Media: Specifically designed for fluorescence microscopy, these media minimize autofluorescence and preserve fluorescence signals over time. They often contain antifade agents that help prevent photobleaching.
Each mounting media type has specific properties and requires a different application technique. For example, some require the complete removal of xylene from the slides before application, while others are compatible with xylene. Incorrect application can lead to bubbles or poor adhesion, compromising the quality of the slide. I personally prefer resinous mounting media for long-term storage due to its superior preservation qualities. The selection process considers factors like staining type, required longevity, and microscopic technique to be used for analysis.
Q 27. How do you ensure the accuracy and reproducibility of histological results?
Ensuring accuracy and reproducibility in histological results is crucial for reliable scientific findings. This is achieved through rigorous attention to detail at every stage, starting with standardized protocols for tissue collection, fixation, processing, and staining. Using positive and negative controls during each staining run is essential to assess the specificity and sensitivity of the reagents. Positive controls confirm the antibody or stain is working correctly, while negative controls validate the absence of non-specific binding.
Maintaining meticulously documented procedures and using validated reagents from reputable suppliers is critical. Regular instrument calibration and quality control checks are also crucial. Digital image analysis allows for objective and quantitative evaluation, reducing inter-observer variability. Blind scoring of samples, where the analyst is unaware of the sample identity, eliminates bias. Employing statistical methods to analyze data and properly reporting uncertainties enhances the reproducibility and credibility of the results. For instance, I regularly implement a standardized staining protocol for all immunohistochemical assays to ensure consistent results across multiple experiments and users.
Q 28. Describe your experience with troubleshooting and resolving instrument malfunctions related to histology equipment.
Troubleshooting instrument malfunctions in histology is a common task requiring a systematic and methodical approach. My experience includes addressing issues with microtomes, tissue processors, staining machines, and embedding stations. The process usually starts by identifying the nature of the problem. For instance, a microtome not cutting sections properly could be due to dull blades, incorrect settings, or damaged components. Similarly, a tissue processor malfunction might result from software errors, pump failures, or reagent issues.
My troubleshooting strategy involves carefully checking the instrument’s manual, investigating potential causes, and systematically eliminating them one by one. This often involves simple checks like reagent levels, power connections, and software updates. More complex issues might require consulting manuals, contacting technical support, or even replacing faulty components. I keep detailed records of equipment maintenance, repairs, and troubleshooting steps to facilitate future problem-solving. Proper preventive maintenance is key to minimizing downtime and avoiding costly repairs. Regular maintenance ensures the equipment functions optimally, leading to higher quality results and reduced troubleshooting time. For example, I once successfully resolved a recurring issue with a tissue processor by identifying a faulty sensor and replacing it, preventing further delays in our experiment.
Key Topics to Learn for Histochemical and Immunohistochemical Staining Techniques Interview
- Principles of Histochemistry: Understanding the fundamental chemical reactions underlying staining processes, including chromogenic and fluorogenic substrates.
- Immunohistochemistry Fundamentals: Mastering antibody-antigen interactions, including antigen retrieval techniques and the selection of appropriate antibodies.
- Staining Protocols: Familiarize yourself with common protocols for H&E staining, PAS staining, IHC for specific markers (e.g., Ki-67, CD3), and in situ hybridization (ISH).
- Practical Applications: Understand the applications of these techniques in various fields, such as cancer diagnostics, pathology, neuroscience, and toxicology. Be prepared to discuss specific examples.
- Troubleshooting Techniques: Develop a strong understanding of common issues encountered during staining procedures (e.g., non-specific staining, background noise, weak signals) and how to troubleshoot them.
- Microscopy and Image Analysis: Demonstrate knowledge of different microscopy techniques (brightfield, fluorescence) and basic image analysis concepts for interpreting stained samples.
- Quality Control and Validation: Discuss the importance of quality control measures to ensure the reliability and reproducibility of staining results. Understand validation processes for new assays.
- Safety and Regulatory Compliance: Understand relevant safety protocols and regulations related to handling hazardous chemicals and biological materials in the laboratory.
- Advanced Techniques: Explore more advanced techniques such as multiplexing IHC, immunofluorescence, and automated staining platforms.
Next Steps
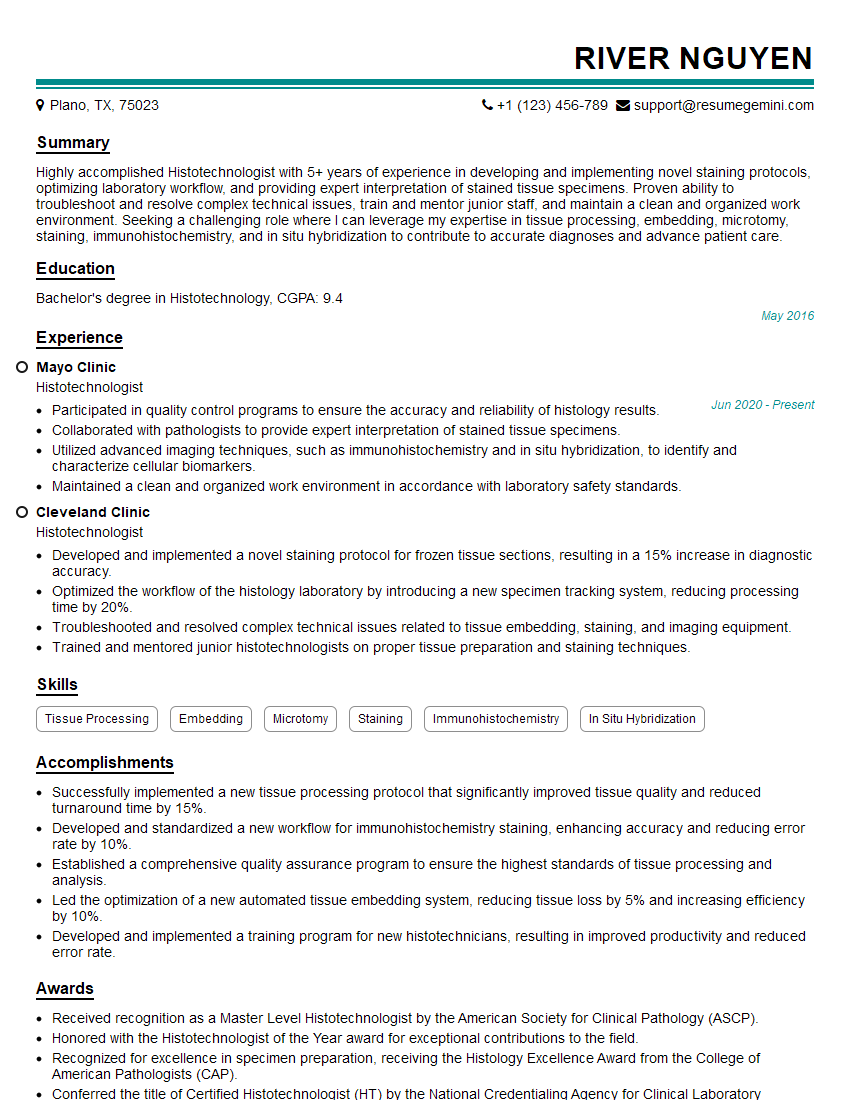
Mastering histochemical and immunohistochemical staining techniques is crucial for career advancement in a wide range of scientific and medical fields. A strong understanding of these techniques demonstrates a high level of technical expertise and problem-solving ability, making you a highly competitive candidate. To maximize your job prospects, creating an ATS-friendly resume is essential. ResumeGemini can help you build a professional and effective resume that showcases your skills and experience effectively. ResumeGemini provides examples of resumes tailored to Histochemical and immunohistochemical staining techniques to guide you through the process. Take the next step towards your dream career; start building your resume today!
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
To the interviewgemini.com Webmaster.
Very helpful and content specific questions to help prepare me for my interview!
Thank you
To the interviewgemini.com Webmaster.
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.