Are you ready to stand out in your next interview? Understanding and preparing for Superior Hypogastric Nerve Blocks interview questions is a game-changer. In this blog, we’ve compiled key questions and expert advice to help you showcase your skills with confidence and precision. Let’s get started on your journey to acing the interview.
Questions Asked in Superior Hypogastric Nerve Blocks Interview
Q 1. Describe the anatomical landmarks used for Superior Hypogastric Plexus Block (SHPB).
Locating the superior hypogastric plexus (SHP) for a Superior Hypogastric Plexus Block (SHPB) relies on understanding its anatomical relationship to surrounding structures. The SHP is located anterior to the fifth lumbar vertebra, posterior to the inferior vena cava and aorta, and lateral to the common iliac arteries. We use several key landmarks to guide our approach. These include the:
- Lumbar Vertebrae: Palpating the L5 vertebra provides a crucial posterior landmark. Imaging guidance helps precisely identify this vertebra.
- Iliac Arteries: The common iliac arteries bifurcate at the level of the sacroiliac joints. The SHP lies lateral to these arteries.
- Inferior Vena Cava and Aorta: These major vessels are readily identifiable on imaging and define the medial boundaries of the target area.
- Sacral Promontory: The anterior border of the sacrum serves as a caudal landmark, helping to define the lower extent of the SHP.
Accurate identification of these landmarks is crucial for safe and effective SHPB placement, minimizing the risk of complications such as vascular injury. Remember, anatomical variations exist, hence the importance of image guidance.
Q 2. What are the indications for performing a SHPB?
SHPB is a valuable interventional pain management technique with several key indications. Primarily, it targets chronic pelvic pain of various etiologies. Here are some of the most common indications:
- Chronic Pelvic Pain: This encompasses pain conditions like endometriosis, chronic prostatitis, pelvic inflammatory disease, and post-surgical pelvic pain.
- Interstitial Cystitis/Bladder Pain Syndrome: SHPB can offer significant pain relief for patients suffering from these conditions.
- Non-Malignant Gynecologic Pain: Pain associated with conditions such as adenomyosis or ovarian cysts may respond favorably to SHPB.
- Proctalgia Fugax: While less common, some studies suggest a benefit for recurrent episodes of this rectal pain.
It’s important to note that SHPB is considered for patients who have failed conservative management strategies such as medication and physiotherapy, and it’s crucial that a thorough diagnostic workup is performed to rule out other causes of pain.
Q 3. What are the contraindications for performing a SHPB?
Several contraindications exist for SHPB, and careful assessment of the patient is paramount. Absolute contraindications generally preclude the procedure, while relative contraindications require careful consideration of the risks and benefits.
- Absolute Contraindications: These include active infection at the injection site, coagulopathy (bleeding disorders), and severe patient instability.
- Relative Contraindications: These include pregnancy, severe obesity making anatomical landmark identification difficult, and patient refusal or inability to cooperate. Other relative contraindications include a history of severe allergic reactions to contrast agents (if using fluoroscopy) or local anesthetics.
In cases of relative contraindications, careful consideration of the risk-benefit ratio is required. If the potential benefits outweigh the risks, then the procedure may proceed with appropriate modifications and increased vigilance for potential complications.
Q 4. Explain the different approaches for performing a SHPB (e.g., transperitoneal, retroperitoneal).
Two main approaches exist for SHPB: transperitoneal and retroperitoneal. The choice depends on factors such as operator experience, available imaging, and patient anatomy.
- Transperitoneal Approach: This approach involves inserting the needle through the peritoneal cavity. It’s considered a more challenging technique, requiring expertise in managing potential visceral injury. It is often less preferred due to a higher risk of complications.
- Retroperitoneal Approach: This is the most common approach. The needle is advanced into the retroperitoneal space, typically lateral to the common iliac arteries. This minimizes the risk of visceral injury and is considered a safer approach.
Each approach has its own nuances, and detailed anatomical knowledge is crucial for both. Regardless of the approach, meticulous attention to detail and the use of image guidance are paramount to ensure accuracy and safety.
Q 5. Detail the imaging techniques used to guide SHPB placement (e.g., fluoroscopy, ultrasound).
Image guidance is essential for accurate and safe SHPB placement. The most commonly used techniques are fluoroscopy and ultrasound.
- Fluoroscopy: Fluoroscopy provides real-time X-ray imaging, allowing the physician to visualize the needle’s trajectory and the spread of contrast medium. This is often used in the retroperitoneal approach and provides excellent visualization of bony landmarks and vascular structures. Contrast is usually injected to verify the position of the needle tip within the SHP.
- Ultrasound: Ultrasound utilizes sound waves to generate real-time images of soft tissues. This technique is particularly helpful in identifying the common iliac arteries and other vascular structures and can be used in both approaches, offering a radiation-free alternative to fluoroscopy.
Sometimes, a combination of both fluoroscopy and ultrasound is used to maximize accuracy and safety. The choice of imaging modality often depends on the physician’s experience, available equipment, and patient-specific factors.
Q 6. What are the potential complications associated with SHPB?
While SHPB is generally a safe procedure, potential complications can arise. These complications can be broadly classified as:
- Vascular Injury: Puncture of the aorta or common iliac arteries is a serious, albeit rare, complication. This can lead to significant bleeding or hematoma formation.
- Nerve Injury: Injury to surrounding nerves, such as the lumbar plexus or sciatic nerve, can result in pain, paresthesia, or weakness.
- Visceral Injury: In the transperitoneal approach, injury to the bowel or other abdominal organs is a possibility.
- Infection: Infection at the injection site is a potential complication requiring prompt treatment with antibiotics.
- Hematoma: Bleeding at the injection site can lead to hematoma formation.
- Allergic Reactions: Allergic reactions to local anesthetics or contrast agents can occur.
The incidence of these complications is significantly reduced with meticulous technique, appropriate patient selection, and the use of image guidance.
Q 7. How do you manage potential complications during and after an SHPB procedure?
Management of complications during and after SHPB requires immediate attention and appropriate intervention. Here’s a breakdown:
- Vascular Injury: Immediate pressure should be applied at the puncture site, and the patient may require angiographic intervention to control bleeding.
- Nerve Injury: Depending on the severity, management might include supportive measures like analgesics, physical therapy, or in some cases surgical intervention.
- Visceral Injury: This would require immediate surgical intervention in most cases.
- Infection: Broad-spectrum antibiotics are usually prescribed, and the infection is closely monitored.
- Hematoma: Small hematomas usually resolve spontaneously, while larger hematomas may require drainage.
- Allergic Reactions: This would require immediate treatment with appropriate medications, potentially including epinephrine.
Post-procedural monitoring includes close observation for any signs of complications, including pain, bleeding, and infection. Patients are usually advised to rest and limit activity for a short period post-procedure. Regular follow-up appointments are important to monitor pain levels and assess the effectiveness of the block.
Q 8. Describe the post-procedural care for patients who have undergone SHPB.
Post-procedural care after a Superior Hypogastric Plexus Block (SHPB), often referred to as a superior hypogastric nerve block, focuses on pain management, monitoring for complications, and patient education. Immediate post-procedure care typically involves monitoring vital signs, assessing the injection site for bleeding or hematoma formation, and evaluating the patient’s pain levels. Patients are usually observed for a short period before discharge.
Pain management is crucial. This may involve administering analgesics, such as intravenous opioids or non-steroidal anti-inflammatory drugs (NSAIDs), tailored to the patient’s pain level and response. Regular pain assessments are essential. We encourage patients to report any pain, even if mild, so we can adjust the pain management plan accordingly.
Patients are given detailed instructions on wound care, potential side effects (such as urinary retention or hypotension), and when to seek immediate medical attention. They are provided with contact information for follow-up appointments and emergency situations. Discharge instructions also include advice on activities of daily living, emphasizing gradual resumption of normal activities to avoid re-injury or complications.
For example, a patient might be advised to avoid strenuous activity for a few days post-procedure and to monitor their urine output. If they experience significant pain, increased swelling at the injection site, or difficulty urinating, they are instructed to contact the clinic immediately.
Q 9. What are the typical medications used during and after an SHPB procedure?
Medication choices during and after an SHPB are carefully selected to achieve both analgesia and procedural sedation where appropriate. Local anesthetic agents, such as bupivacaine or ropivacaine, are the cornerstone of the SHPB itself. They provide localized nerve blockade.
Sedatives such as midazolam or propofol may be used for patient comfort during the procedure, especially if it’s being performed without general anesthesia. Post-procedurally, NSAIDs, such as ibuprofen or naproxen, are frequently used to manage inflammation and pain. Opioid analgesics, such as morphine or fentanyl, might be necessary for severe pain, but we strive to minimize opioid use due to potential side effects. The choice of medications will always depend on individual patient factors like allergies, medical history, and comorbidities. We frequently use a multimodal approach to pain management, combining different classes of drugs to optimize pain relief while reducing side effects. For example, a patient might receive a combination of local anesthetic, NSAID, and a low dose opioid for a period post-surgery.
Q 10. How do you assess the effectiveness of an SHPB?
Assessing the effectiveness of an SHPB involves a multi-faceted approach. Firstly, we rely heavily on subjective patient feedback – a reduction in pain levels reported by the patient is a primary indicator of success. We use validated pain scales like the Numerical Rating Scale (NRS) or Visual Analog Scale (VAS) both pre and post-procedure, and at regular follow-up appointments to track changes.
Secondly, we observe objective clinical improvements. This might include an improvement in the patient’s ability to perform daily activities, reduced need for opioid analgesics, or improvement in bowel or bladder function if these were affected by the underlying condition.
Thirdly, we often use imaging techniques, like fluoroscopy during the procedure itself to confirm needle placement and ensure the local anesthetic is reaching the target nerves. While imaging doesn’t directly assess pain relief, it helps us understand procedural accuracy and potentially explain variations in outcomes. For example, if a patient reports limited pain relief, we may review the fluoroscopy images to identify any potential technical issues during the procedure.
Q 11. What are the alternative treatment options for patients who are not suitable candidates for SHPB?
Alternative treatment options for patients unsuitable for SHPB vary significantly depending on the underlying condition causing their pain. These options might include medical management with oral analgesics, such as NSAIDs or opioids, physical therapy, cognitive behavioral therapy (CBT), and neuromodulation techniques like spinal cord stimulation.
Surgical interventions, such as nerve ablation or surgical resection of the affected tissues, are possibilities in some cases but often represent a last resort due to the invasiveness. In cases of chronic pelvic pain, other minimally invasive approaches like celiac plexus blocks or transforaminal epidural injections may be considered. The best alternative will be determined through a thorough evaluation of each patient’s individual circumstances and medical history to determine the best treatment plan.
Q 12. Discuss the role of pre-procedural patient education in SHPB.
Pre-procedural patient education is paramount for a successful SHPB experience. It involves providing the patient with a clear understanding of the procedure, its benefits, risks, and potential complications. This helps ensure informed consent and reduces patient anxiety.
We explain the procedure in simple terms, using anatomical diagrams and analogies whenever possible, to ensure the patient grasps the concept and location of the target nerves. We discuss the expected outcomes, realistic expectations, and address any myths or misconceptions the patient might have.
We also thoroughly cover potential side effects, such as urinary retention, hypotension, or bleeding, and what to expect in the post-procedure period. Encouraging patients to ask questions and addressing their concerns creates a trusting relationship and fosters a positive procedural experience. A well-educated patient is more likely to cooperate during the procedure and adhere to post-procedural instructions, leading to better outcomes.
Q 13. Explain the importance of informed consent in the context of SHPB.
Informed consent is absolutely crucial in the context of SHPB, as with all medical interventions. It signifies that the patient has a thorough understanding of the procedure, its risks and benefits, and alternative treatment options. The patient must also comprehend that there are no guarantees of success, and the potential for complications exists.
Obtaining informed consent is a process, not merely a form to be signed. We engage in a comprehensive discussion with the patient, answering all their questions and ensuring they understand the information provided. We use plain language, avoiding medical jargon whenever possible, and encourage them to express any concerns or uncertainties. The patient should feel comfortable asking questions and clarifying anything they don’t understand before proceeding with the procedure. Documentation of this conversation and confirmation of understanding is critical from both a legal and ethical standpoint.
Q 14. What are the common patient-reported outcomes used to assess the efficacy of SHPB?
Common patient-reported outcomes (PROs) used to assess the efficacy of SHPB are designed to capture the patient’s subjective experience of pain and functional improvements. These PROs often include validated pain scales (NRS, VAS), measures of quality of life (e.g., SF-36), and assessments of specific functional limitations related to the underlying condition.
For instance, in patients with chronic pelvic pain, we might use questionnaires that evaluate the impact of pain on sexual function, bowel habits, and daily activities. By tracking these PROs over time, we can objectively measure the extent to which the SHPB has improved the patient’s quality of life and their functional capacity. The use of PROs is crucial because it provides valuable insights into the patient’s perspective and experience, which might not be fully captured by objective clinical measures alone. For example, a patient may experience a clinically significant reduction in pain scores on a numerical rating scale, but this may not fully reflect their experience, and quality of life questionnaires can supplement the information.
Q 15. How do you differentiate between successful and unsuccessful SHPB based on clinical findings?
Determining the success of a Superior Hypogastric Plexus Block (SHPB) relies heavily on clinical findings, not just imaging. A successful block manifests as a significant reduction or complete resolution of chronic pelvic pain, typically within hours to days. This improvement is subjective, reported by the patient, and objective, measured by pain scales like the Visual Analog Scale (VAS) or Numerical Rating Scale (NRS).
Successful SHPB: Patients report substantial pain relief, often described as a ‘numbness’ or ‘heaviness’ in the pelvic region. Objective measures, such as decreased pain scores on validated scales, support this subjective improvement. Improved quality of life indicators, such as better sleep and increased mobility, also strongly suggest success. For example, a patient reporting a VAS score of 8/10 pre-block dropping to 2/10 post-block, coupled with improved sleep and ability to walk without pain, indicates a successful procedure.
Unsuccessful SHPB: Persistent or only minimally improved pain despite the block suggests failure. The patient may report little to no change in their pain levels or pain score. Sometimes, the pain might even worsen temporarily due to the procedure itself, but this should resolve. If the pain relief is temporary, lasting only a few hours, it can indicate incomplete block or incorrect needle placement. For instance, a VAS score remaining at 7/10 post-block suggests an unsuccessful procedure requiring reevaluation of technique or alternative treatment.
Career Expert Tips:
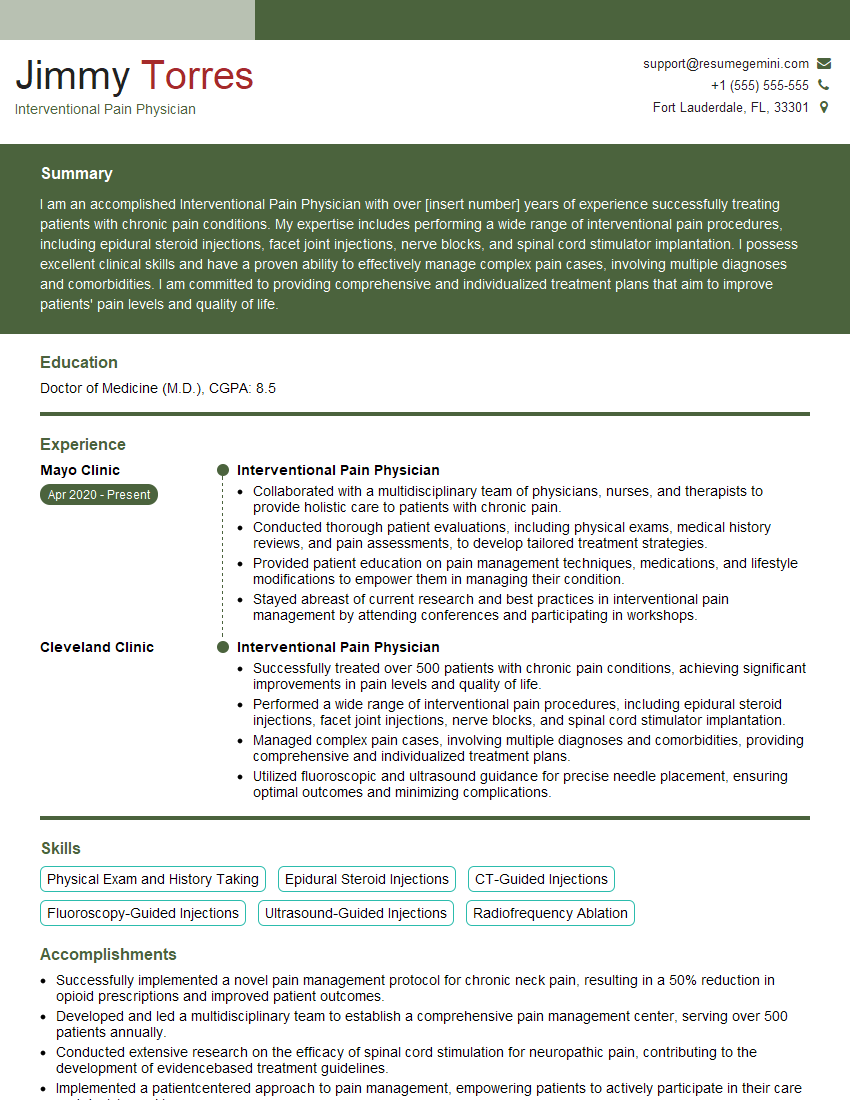
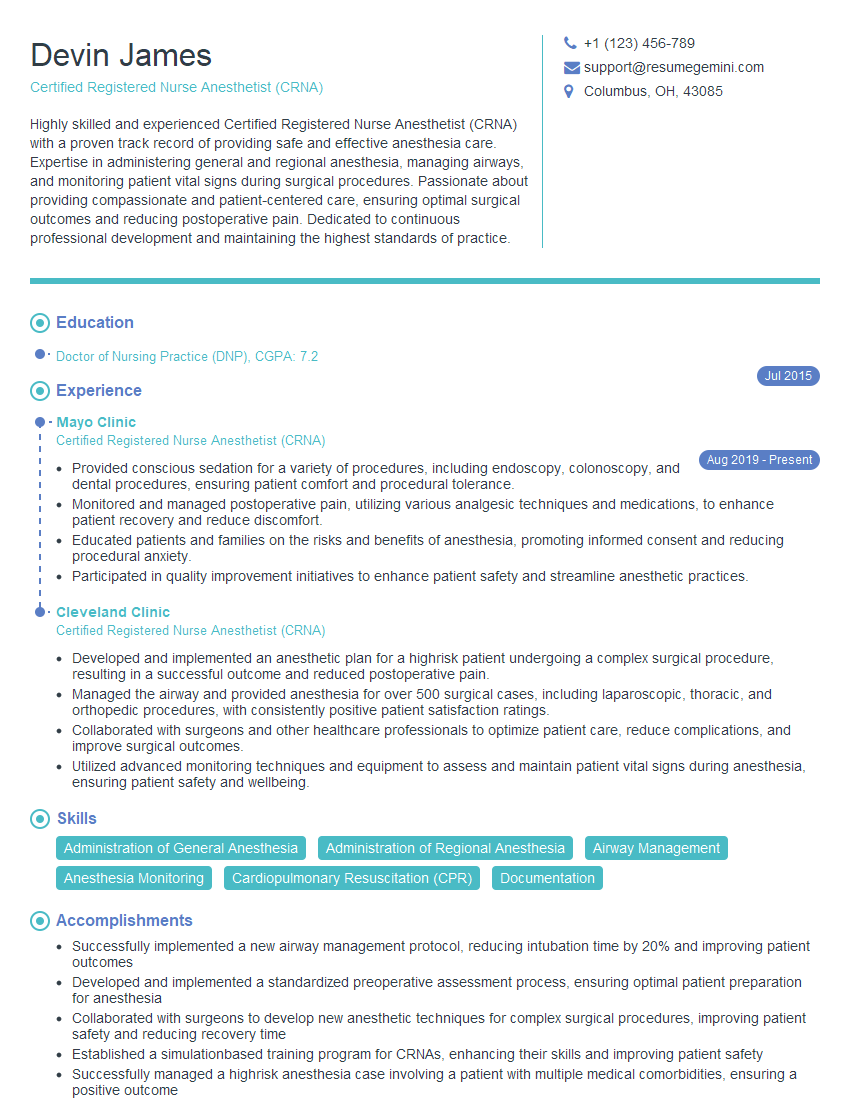
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What are the potential long-term effects of SHPB?
While generally safe, long-term effects of SHPB are relatively rare but can include persistent paresthesia (numbness or tingling), bowel or bladder dysfunction (though usually temporary and mild), and, in extremely rare instances, injury to adjacent structures.
Persistent Paresthesia: This is one of the most commonly reported long-term effects and may present as altered sensation in the lower extremities or perineal region. This usually resolves spontaneously within weeks to months but can be persistent in some individuals.
Bowel or Bladder Dysfunction: Changes in bowel or bladder function, such as urinary retention or constipation, are generally temporary. However, in rare cases, prolonged dysfunction may occur. Thorough pre-procedure evaluation, careful technique, and proper patient selection can minimize this risk.
Rare Complications: In exceptionally rare cases, nerve damage, hematoma formation, or infection may occur, typically due to unforeseen complications during the procedure. These are rare with skilled practitioners adhering to sterile techniques and meticulous attention to anatomical detail. It’s crucial to emphasize that these long-term effects are not common and are often manageable.
Q 17. How do you address patient concerns and anxieties regarding SHPB?
Addressing patient concerns and anxieties is paramount in providing optimal care. I begin by actively listening to their fears and validating their feelings. I use clear and simple language to explain the procedure, emphasizing that I will manage their discomfort. Pain management is discussed extensively – what type of anesthesia is being used, what kind of pain to expect, and available pain relief options post-procedure.
I use analogies to make the complex anatomy easier to understand. For example, I might compare the superior hypogastric plexus to a major highway for nerve signals and explain how blocking this pathway can alleviate pain. I also discuss realistic expectations about the procedure’s success and potential side effects. Showing empathy is critical; I reassure patients that their concerns are valid and answer their questions thoroughly and patiently. Open communication and building trust before, during, and after the procedure is vital for managing patient anxieties. Providing educational materials about SHPB beforehand can also significantly reduce anxieties.
Q 18. Describe your experience with different types of needles and catheters used in SHPB.
Needle and catheter selection for SHPB depends on various factors, including patient anatomy, target location, and operator preference. I have experience with a range of needles, from 22-gauge to 18-gauge needles, typically using longer needles for a transgluteal approach.
Needles: The choice depends on the anticipated depth of insertion. For example, smaller-gauge needles (22-25 gauge) may be used for initial localization, while larger-gauge needles (18-20 gauge) might be needed for catheter placement. The needle type, such as a stimulating needle, is chosen to confirm correct placement. Stimulation of the nerves leads to pain replication or muscle contraction.
Catheters: Various catheters are used, typically those with multiple side holes to deliver medication effectively across the plexus. These can be longer or shorter, depending on the individual anatomy. The material and flexibility are also important considerations for successful placement and patient comfort. For example, a flexible, smaller-diameter catheter is generally more comfortable for the patient during the post-procedure period. Proper catheter placement is crucial for sustained pain relief. Post-procedural imaging is used to confirm proper catheter position.
Q 19. What are the advantages and disadvantages of using different imaging modalities for SHPB?
Imaging modalities play a crucial role in guiding SHPB placement, enhancing safety, and improving outcomes. Fluoroscopy is the most commonly used technique, providing real-time visualization of needle and catheter advancement. Ultrasound guidance is also increasingly employed and provides advantages in certain scenarios.
Fluoroscopy: Offers excellent visualization of bony landmarks, allowing precise needle placement. However, it involves ionizing radiation, raising concerns about potential long-term effects. This needs to be balanced against the benefits.
Ultrasound: Offers radiation-free guidance, ideal for pregnant women or patients requiring repeated blocks. However, ultrasound visualization can be challenging in obese patients or those with significant bowel gas. It may provide less precise visualization of nerves compared to fluoroscopy. The choice depends on individual patient characteristics and the practitioner’s experience with both techniques. A hybrid approach, using both, is sometimes utilized.
Q 20. How do you manage bleeding complications during an SHPB procedure?
Bleeding complications are rare but need immediate attention. Careful technique during the procedure, including using the smallest gauge needle possible and applying pressure after needle removal, minimizes the risk. However, if bleeding does occur, immediate pressure is applied to the insertion site.
Management Steps: If bleeding is significant or continues despite pressure, the patient’s vital signs are monitored closely, and potentially, more invasive procedures may be necessary. This may involve local hematoma evacuation or, rarely, surgical intervention. Monitoring hematocrit and hemoglobin levels post-procedure can also assess any significant blood loss.
Prevention: Careful patient selection, obtaining complete blood count pre-procedure, careful needle placement, and gentle manipulation minimize bleeding risk. The use of smaller-gauge needles can significantly minimize the trauma to the tissues. Prophylactic measures such as the use of topical hemostatic agents are also sometimes employed, depending on the patient’s bleeding risk.
Q 21. How do you manage infection risk during and after an SHPB procedure?
Infection risk is a concern in any invasive procedure. Strict adherence to sterile techniques is crucial in preventing infection. This includes meticulous hand hygiene, using sterile gloves, drapes, and equipment. The patient is educated about signs and symptoms of infection, such as fever, localized redness, swelling, or purulent drainage.
Prevention and Management: Prophylactic antibiotics are sometimes used, especially in high-risk patients, and the insertion site is cleaned thoroughly before and after the procedure. Any post-procedure signs of infection are managed promptly with appropriate antibiotic therapy, based on culture and sensitivity testing. Patient education about proper wound care and the need to contact the physician if any signs of infection develop is crucial to successful outcome.
Q 22. Describe your experience with using nerve stimulators during SHPB.
Nerve stimulators are invaluable during Superior Hypogastric Plexus Blocks (SHPB) because they allow for precise targeting of the superior hypogastric plexus, minimizing the risk of injecting the anesthetic solution into unintended locations. Imagine trying to find a specific nerve in the pelvis without a map; the stimulator acts as that map. It works by delivering small electrical pulses that stimulate the nerves, causing a characteristic muscle contraction or sensory response. We then adjust the needle position until we achieve the desired response, ensuring the anesthetic is placed correctly. This technique significantly improves the accuracy of the block and maximizes its efficacy while reducing complications.
My experience encompasses using various stimulators, from simple monopolar devices to more sophisticated models with impedance monitoring. I find that real-time feedback from the stimulator, coupled with fluoroscopy in some cases, is crucial in navigating the complex pelvic anatomy and achieving successful placement. For instance, in one case, a patient presented with chronic pelvic pain and a failed initial attempt at SHPB. Using a nerve stimulator with impedance monitoring, we were able to identify the optimal location, which led to significant pain relief.
Q 23. Explain the use of local anesthetics and steroids in SHPB.
Local anesthetics and steroids play distinct but complementary roles in SHPB. Local anesthetics, such as bupivacaine or ropivacaine, provide immediate pain relief by temporarily blocking nerve conduction. Think of it as a temporary ‘off’ switch for the pain signals. This immediate effect is crucial for post-procedure pain management and assessing the success of the block. Steroids, such as dexamethasone or methylprednisolone, are added to the anesthetic mixture to reduce inflammation, a major contributor to chronic pelvic pain. They act more slowly, providing long-term benefits by suppressing the inflammatory process and thus extending the analgesic effect. The combination of these two agents provides both immediate pain relief and a longer-lasting anti-inflammatory effect, leading to more sustained pain reduction.
The selection of the specific anesthetic and steroid depends on factors such as the patient’s medical history, the severity of pain, and the anticipated duration of analgesia. For example, a patient with a history of allergic reactions may require an alternative anesthetic, and a patient with severe inflammatory conditions might benefit from a higher dose of steroid.
Q 24. What is the role of multidisciplinary pain management in the context of SHPB?
Multidisciplinary pain management is essential for optimal outcomes in SHPB. SHPB is rarely a standalone treatment; it’s most effective as part of a comprehensive approach. A multidisciplinary team typically includes anesthesiologists (like myself), pain specialists, physical therapists, psychologists, and other healthcare professionals as needed. Each team member addresses a different aspect of the patient’s condition, leading to holistic care. For example, physical therapists might teach patients exercises to strengthen their pelvic floor muscles, while psychologists can help patients manage the psychological aspects of chronic pain.
My approach always involves collaboration. We assess the patient’s overall condition, considering not only their pain but also their psychological well-being, functional limitations, and other related medical conditions. We then create a personalized treatment plan that might involve SHPB, medication management, physical therapy, and psychological support, all guided by the patient’s individual needs and preferences.
Q 25. How do you determine the appropriate volume and concentration of local anesthetic for SHPB?
Determining the appropriate volume and concentration of local anesthetic for SHPB is crucial to ensure both efficacy and safety. There’s no single ‘correct’ answer; it depends on several factors, including the patient’s body weight, the extent of the pain, and the patient’s overall medical status. Typically, volumes range from 10-20ml, and concentrations commonly include 0.25%–0.5% bupivacaine or ropivacaine. However, I always tailor the approach to each individual.
I carefully consider the patient’s medical history to rule out any contraindications to the chosen local anesthetic and steroid. Pre-procedural assessment of renal and hepatic function, along with cardiovascular health, plays a crucial role in determining the appropriate dose. For example, I might use a lower volume and concentration in elderly patients or in those with pre-existing kidney or liver conditions. The goal is to achieve optimal analgesia while minimizing potential side effects.
Q 26. What are the factors that influence the duration of analgesia after SHPB?
The duration of analgesia after SHPB is variable and influenced by many factors. These factors include the type and concentration of local anesthetic used, the volume injected, the presence and concentration of corticosteroids, the patient’s individual characteristics, the underlying cause and severity of pain, and the presence of any concurrent medical conditions. A larger volume or concentration of the anesthetic generally leads to longer lasting pain relief. The addition of a corticosteroid can further extend the duration of relief by reducing inflammation.
Patient factors such as age, body mass index (BMI), and overall health can also impact the duration. For instance, older patients or those with significant comorbidities may experience shorter-lasting effects compared to younger, healthier individuals. The underlying cause of pain also plays a role; for example, pain from nerve damage may respond differently to SHPB compared to pain from inflammation.
Q 27. Describe a challenging case involving SHPB that you have managed and the outcome.
One particularly challenging case involved a 45-year-old female patient with chronic pelvic pain of unclear etiology. She had undergone multiple prior procedures with limited success, and her pain was significantly impacting her quality of life. Initial attempts at SHPB were unsuccessful likely due to anatomical variations. I used fluoroscopy guidance combined with nerve stimulation to carefully visualize the plexus and targeted the injection. Even with precise placement, initial pain relief was minimal.
This case highlighted the importance of a multidisciplinary approach. After careful re-evaluation with the pain team, we discovered that she had significant underlying psychological factors contributing to her pain experience. We incorporated psychological support into her treatment plan, which included cognitive behavioral therapy. Combining this psychological intervention with repeated targeted SHPB injections (with adjustments to volume and steroid concentration) led to substantial improvement in her pain levels and a marked increase in her quality of life. This emphasized that successful pain management often requires a holistic approach that addresses both the physical and psychological aspects of chronic pain.
Q 28. How do you stay updated on the latest advancements and best practices in SHPB?
Staying current in the field of SHPB involves a multi-pronged approach. I regularly attend national and international conferences focused on pain management and interventional techniques. These meetings often feature the latest research findings and case studies. I also actively participate in continuing medical education (CME) courses and workshops specifically dedicated to advanced interventional pain management. Peer-reviewed journals, such as Anesthesiology and Pain Medicine, are key sources of information on new research, techniques, and best practices.
Moreover, I maintain active memberships in professional organizations like the American Society of Anesthesiologists (ASA) and the American Academy of Pain Medicine (AAPM). These memberships provide access to ongoing educational resources, publications, and opportunities for professional collaboration with leading experts in the field. Staying involved in these communities ensures I’m well-versed in the latest advancements and best practices, ultimately improving the care I provide to my patients.
Key Topics to Learn for Superior Hypogastric Nerve Blocks Interview
- Anatomy and Neuroanatomy: Thorough understanding of the superior hypogastric plexus, its branches, and their relationship to surrounding structures. Consider variations in anatomy and potential pitfalls during the procedure.
- Indications and Contraindications: Master the clinical scenarios where SHNB is indicated and the situations where it is contraindicated. Be prepared to discuss the rationale behind these decisions.
- Technique and Approaches: Familiarize yourself with different approaches to performing SHNB (e.g., fluoroscopic guidance, ultrasound guidance). Understand the steps involved in each technique and potential complications.
- Needle Placement and Verification: Understand the critical aspects of achieving accurate needle placement and methods for verifying successful nerve blockade (e.g., sensory testing, fluoroscopy). Be prepared to discuss strategies for managing difficulties.
- Potential Complications and Management: Be ready to discuss potential complications (e.g., hematoma, infection, nerve injury) and the appropriate management strategies for each.
- Post-Procedure Care and Patient Monitoring: Understand the importance of post-procedure monitoring and the necessary steps to ensure patient safety and comfort.
- Anesthesia Considerations: Discuss the types of anesthetic agents used, their dosages, and their pharmacokinetic and pharmacodynamic properties in the context of SHNB.
- Comparison with Alternative Treatments: Be prepared to discuss the advantages and disadvantages of SHNB compared to other treatment options for similar conditions.
- Case Studies and Problem Solving: Review clinical cases and scenarios to develop your problem-solving skills related to patient selection, technique optimization, and complication management.
Next Steps
Mastering Superior Hypogastric Nerve Blocks significantly enhances your expertise in interventional pain management, opening doors to specialized roles and advanced career opportunities. A strong resume is crucial for showcasing your skills effectively. Building an ATS-friendly resume is vital for maximizing your job prospects. ResumeGemini is a trusted resource to help you craft a professional and impactful resume that highlights your expertise in SHNB. Examples of resumes tailored to Superior Hypogastric Nerve Blocks are available to guide you. Take the next step towards your dream career today!
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.