Every successful interview starts with knowing what to expect. In this blog, we’ll take you through the top Musculoskeletal Rehabilitation interview questions, breaking them down with expert tips to help you deliver impactful answers. Step into your next interview fully prepared and ready to succeed.
Questions Asked in Musculoskeletal Rehabilitation Interview
Q 1. Describe the different types of musculoskeletal injuries.
Musculoskeletal injuries encompass a wide spectrum of conditions affecting the body’s supporting structures – bones, muscles, tendons, ligaments, and joints. These injuries range in severity from minor strains to severe fractures.
- Fractures: Breaks in the bone, ranging from hairline cracks to complete separations. Examples include a fractured femur (thigh bone) or a wrist fracture.
- Dislocations: When the bones of a joint are forced out of their normal alignment. A shoulder dislocation is a common example.
- Sprains: Injuries to ligaments, the tissues that connect bones to other bones. Ankle sprains are frequent occurrences.
- Strains: Injuries to muscles or tendons, the tissues that connect muscles to bones. A hamstring strain is a common sports injury.
- Contusions (Bruises): Soft tissue injuries caused by blunt force trauma, resulting in bleeding under the skin.
- Tendinopathies: Conditions affecting tendons, including tendinitis (inflammation) and tendinosis (degeneration).
- Bursitis: Inflammation of the bursae, fluid-filled sacs that cushion joints.
- Osteoarthritis: Degenerative joint disease characterized by cartilage breakdown and joint pain.
Understanding the specific type of injury is crucial for determining the appropriate treatment and rehabilitation plan. For instance, a fracture requires immobilization, whereas a strain might benefit from stretching and strengthening exercises.
Q 2. Explain the principles of joint mobilization.
Joint mobilization techniques involve manually applying specific forces to a joint to improve its range of motion, reduce pain, and restore normal joint mechanics. These techniques are based on understanding the biomechanics of joints and the principles of arthrokinematics (the movement of joint surfaces).
The principles of joint mobilization include:
- Grade I and II Mobilizations: Small amplitude oscillations within the pain-free range of motion, used to decrease pain and muscle guarding. Imagine gently rocking a slightly stiff door hinge to ease its movement.
- Grade III and IV Mobilizations: Larger amplitude oscillations or sustained stretches to the end range of motion, used to improve range of motion and address joint stiffness. Think of carefully stretching a tight rubber band to increase its flexibility.
- Specific Joint Techniques: The application of mobilization is highly specific to the joint being treated, considering its unique anatomy and biomechanics. For example, the mobilization techniques for the knee will differ significantly from those used for the cervical spine.
- Patient Assessment and Feedback: Throughout the mobilization process, patient feedback is crucial. The therapist adjusts the technique based on the patient’s response to pain and comfort levels. This ensures the treatment is safe and effective.
Proper training and experience are essential to perform joint mobilization safely and effectively. Improper application can lead to further injury.
Q 3. What are the common assessment tools used in musculoskeletal rehabilitation?
A comprehensive musculoskeletal assessment utilizes a variety of tools to gain a holistic understanding of the patient’s condition. These tools can be broadly categorized into subjective and objective measures.
- Subjective Assessments: These rely on the patient’s self-reported information, including pain scales (e.g., Visual Analog Scale or Numeric Rating Scale), patient history (mechanism of injury, past medical history), and functional limitations (activities of daily living).
- Objective Assessments: These involve direct observation and measurement by the clinician. Examples include:
- Range of Motion (ROM): Using a goniometer to measure the degree of joint movement.
- Muscle Strength Testing: Manual muscle testing (MMT) to assess muscle strength on a scale of 0-5.
- Palpation: Assessing tissue texture, temperature, and identifying trigger points.
- Special Tests: Specific tests designed to identify particular injuries or pathologies (e.g., Lachman’s test for anterior cruciate ligament injury).
- Functional Assessments: Evaluating the ability to perform tasks related to daily living, such as walking, climbing stairs, or lifting objects. Examples include the Timed Up and Go test or the Berg Balance Scale.
- Imaging Studies: X-rays, MRI, CT scans, and ultrasound to visualize bone, soft tissue, and joint structures.
The selection of assessment tools is dependent on the specific injury and patient presentation. A comprehensive approach incorporating both subjective and objective measures yields the most accurate diagnosis and informs appropriate treatment strategies.
Q 4. How do you differentiate between muscle strain and ligament sprain?
While both muscle strains and ligament sprains involve soft tissue injuries, they affect different structures and present with distinct characteristics.
- Muscle Strain: A muscle strain involves damage to the muscle fibers themselves or to the junction between the muscle and tendon. Patients typically report pain during muscle contraction or stretching, and often experience muscle weakness and tenderness to the touch. Pain is usually localized to the muscle belly.
- Ligament Sprain: A ligament sprain involves damage to the ligaments, which connect bones at a joint. Patients usually report pain with joint movement or weight-bearing. There may be joint instability, swelling, and bruising. The pain is typically localized to the joint.
Consider this analogy: imagine a rope (muscle) and the knot that ties two sticks together (ligament). A muscle strain is like a frayed section of the rope, while a ligament sprain is like damaging the knot itself.
A thorough history and physical examination, often supplemented by imaging studies (e.g., MRI), are necessary to differentiate between the two. Treatment will depend on the severity of the injury and may include rest, ice, compression, elevation (RICE), pain management, and targeted exercises.
Q 5. Explain the process of designing a rehabilitation program.
Designing a rehabilitation program is a meticulous process involving several crucial steps. It’s a personalized approach tailored to the patient’s specific needs and capabilities.
- Assessment: A comprehensive evaluation of the patient’s medical history, current condition, and functional limitations. This stage informs the overall goals and objectives of the program.
- Goal Setting: Establishing measurable, achievable, relevant, and time-bound (SMART) goals. These might involve improving range of motion, increasing muscle strength, restoring functional mobility, and reducing pain. For example, a goal might be “Increase knee flexion ROM from 90 degrees to 120 degrees within 4 weeks.”
- Intervention Selection: Choosing appropriate interventions based on the assessment and goals. This may include manual therapy, therapeutic exercises (strength training, range of motion exercises, flexibility exercises), modalities (e.g., ultrasound, TENS), patient education, and activity modifications.
- Program Implementation: Implementing the chosen interventions, monitoring the patient’s progress, and making adjustments as needed. Regular communication with the patient is crucial to ensure adherence and effectiveness.
- Progression: Gradually increasing the intensity and duration of exercises as the patient recovers. This avoids re-injury and ensures continued progress.
- Discharge Planning: Developing a plan for the patient to transition from formal rehabilitation to self-management. This may involve home exercise programs, strategies for injury prevention, and guidance on returning to work or recreational activities.
Throughout this entire process, ongoing assessment and feedback are vital. The program must be flexible and adaptive to respond to the patient’s individual needs and progress.
Q 6. Describe your experience with different therapeutic modalities (e.g., ultrasound, TENS).
I have extensive experience using various therapeutic modalities in musculoskeletal rehabilitation. My experience includes:
- Ultrasound: I utilize ultrasound therapy for its thermal and non-thermal effects. Thermal ultrasound increases tissue temperature, promoting relaxation and reducing pain and muscle spasm. Non-thermal ultrasound may enhance tissue healing. I use ultrasound judiciously and always consider contraindications such as pregnancy, areas with reduced sensation, and over malignant tissue.
- Transcutaneous Electrical Nerve Stimulation (TENS): TENS is employed to manage pain by stimulating sensory nerves, thereby blocking pain signals from reaching the brain. I adjust the parameters of TENS (frequency, pulse width, intensity) based on the patient’s response and the specific pain condition. TENS is particularly effective for acute and chronic pain management.
- Other Modalities: My experience also encompasses other modalities such as electrical muscle stimulation (EMS) for muscle strengthening and re-education, laser therapy for tissue repair, and iontophoresis for drug delivery to the affected area.
It’s important to note that modalities are not used in isolation but integrated into a comprehensive rehabilitation program that addresses the underlying cause of the musculoskeletal condition. They should always be considered as adjunctive therapies, complementing other interventions like therapeutic exercise and manual therapy.
Q 7. How do you assess a patient’s functional limitations?
Assessing functional limitations requires a multifaceted approach combining observation, standardized assessments, and patient self-report. It goes beyond just measuring ROM or muscle strength; it’s about evaluating the ability to perform tasks relevant to the patient’s daily life.
- Observation: Carefully observing the patient’s movement patterns during various activities, such as walking, sitting, standing, and stair climbing. This helps identify compensations and movement limitations.
- Standardized Assessments: Utilizing validated functional assessment tools, such as the Timed Up and Go test (measures mobility and balance), the Berg Balance Scale (assesses balance), and the Functional Independence Measure (FIM) (measures the level of independence in daily activities). These tools provide objective measurements of functional performance.
- Patient Self-Report: Utilizing questionnaires and interviews to assess the patient’s ability to perform activities of daily living (ADLs), such as dressing, bathing, eating, and toileting. These self-reports help to understand the impact of the musculoskeletal condition on the patient’s quality of life.
- Activity Analysis: A systematic approach to analyzing the demands of specific activities, such as lifting or carrying objects, to identify the underlying factors contributing to the functional limitation.
By integrating these approaches, a clear picture of the patient’s functional limitations emerges, guiding the design of an individualized rehabilitation program focused on restoring function and independence. For instance, if a patient struggles with stair climbing, the rehabilitation program would focus on improving lower extremity strength, balance, and coordination to address this specific limitation.
Q 8. What are the common contraindications for therapeutic exercises?
Contraindications for therapeutic exercises are situations where an exercise or activity could potentially worsen a condition or cause harm. These vary widely depending on the specific injury or disease, but some common examples include:
- Acute inflammation: Intense exercise in the presence of significant inflammation (e.g., severe swelling, redness, heat) can increase tissue damage. For example, aggressive range of motion exercises in a severely sprained ankle could delay healing.
- Severe pain: Exercise should not exacerbate pain to the point of causing significant discomfort or further injury. We need to find a balance where the exercise is challenging, but not overwhelmingly painful. A patient with severe sciatica, for instance, might need to initially focus on pain-relieving strategies before undertaking more strenuous exercises.
- Cardiovascular instability: Patients with unstable heart conditions should have their exercise program carefully monitored and adjusted to accommodate their limitations. Vigorous exercise might be contraindicated.
- Uncontrolled infections: Systemic infections can impair healing and make exercise counterproductive.
- Bone fragility (osteoporosis): High-impact exercises may increase the risk of fractures in individuals with osteoporosis, requiring modifications toward weight-bearing activities with lower impact.
- Neurological deficits: Patients with significant neurological impairments, such as those with stroke or spinal cord injury, require carefully tailored exercises to prevent further damage. The intensity and type of exercise are modified based on the individual’s neurological status and risk for falls.
Determining contraindications always requires a thorough assessment of the patient’s condition, considering their medical history, current symptoms, and response to treatment. It often requires collaboration with other healthcare professionals.
Q 9. Explain the concept of pain management in musculoskeletal rehabilitation.
Pain management in musculoskeletal rehabilitation is crucial for successful recovery. It’s not simply about eliminating pain, but about managing it effectively to allow for safe and progressive exercise and functional improvements. We utilize a multimodal approach that considers the biological, psychological, and social aspects of pain.
Strategies include:
- Pharmacological interventions: Pain medications such as NSAIDs (non-steroidal anti-inflammatory drugs), analgesics, and in some cases, opioids, may be prescribed by the physician to control acute pain.
- Therapeutic modalities: Heat, ice, ultrasound, electrical stimulation, and laser therapy can be used to reduce inflammation, pain, and muscle spasm. For example, ice is often used after an acute injury to reduce swelling.
- Manual therapy: Techniques such as massage, mobilization, and manipulation can address musculoskeletal restrictions and alleviate pain.
- Therapeutic exercise: Graded exercise programs that progressively challenge the patient’s pain threshold are key. We might start with gentle range of motion exercises and gradually progress to strengthening and functional activities. For example, a patient with low back pain might begin with gentle stretches and progress to core strengthening exercises.
- Patient education: Understanding the source of their pain and how it relates to their injury is crucial for patient compliance and buy-in. Education on self-management techniques, such as proper posture and body mechanics, also plays a major role.
- Psychological interventions: Addressing psychological factors like anxiety, depression, and fear-avoidance beliefs is important, as these can significantly impact pain perception and recovery. Cognitive behavioral therapy (CBT) might be helpful.
The goal is to progressively reduce reliance on medication and other passive pain-relief strategies while empowering the patient to manage their pain through active participation in their rehabilitation.
Q 10. How do you adapt rehabilitation programs to individual patient needs?
Adapting rehabilitation programs is central to effective musculoskeletal rehabilitation. A ‘one-size-fits-all’ approach is ineffective. We need to create individualized plans that consider each patient’s unique circumstances.
Factors we consider include:
- Medical history: Pre-existing conditions, surgeries, and medications all influence exercise prescription.
- Diagnosis and injury severity: The type and severity of injury will dictate the type, intensity, and duration of exercises.
- Functional limitations: Assessments of the patient’s daily living activities help target specific areas needing improvement.
- Pain levels: Exercises should be adjusted based on the patient’s pain response, ensuring they remain within a comfortable yet challenging range.
- Age and fitness levels: Older adults or those with low fitness levels will require modified exercise programs.
- Patient preferences and goals: Patient involvement in the planning process is crucial. Their preferences and what they hope to achieve should guide the program.
For instance, a young athlete recovering from a knee injury will have a different program than an elderly individual recovering from a hip fracture. The athlete might focus on high-intensity exercises to regain peak performance, whereas the elderly individual might need a gentler program focusing on improving mobility and reducing fall risk. The program’s evolution continuously considers the patient’s progress and response to treatment.
Q 11. Describe your experience with patient education and compliance.
Patient education and ensuring compliance are critical for successful outcomes in musculoskeletal rehabilitation. I believe in a collaborative approach that empowers patients to actively participate in their recovery.
My approach involves:
- Clear and concise explanations: I use simple language, avoiding jargon, to explain the patient’s condition, the treatment plan, and the rationale behind the exercises.
- Visual aids: Diagrams, videos, and demonstrations enhance understanding and retention.
- Practical demonstrations: I show patients how to perform exercises correctly, providing feedback and adjustments as needed.
- Home exercise programs: I create detailed written or video instructions for home exercises to reinforce progress between sessions.
- Regular check-ins: I maintain open communication, actively soliciting feedback and addressing concerns.
- Goal setting: Collaboratively setting realistic and achievable goals fosters motivation and adherence.
- Addressing barriers: I identify and address any barriers to compliance, such as lack of equipment, support, or understanding.
For example, I recently worked with a patient with chronic neck pain. By explaining the mechanics of their posture and demonstrating proper ergonomic techniques at work, and providing them with home exercises, I fostered compliance and saw a marked improvement in their condition. Consistent feedback and ongoing education were key to their success.
Q 12. What are the different stages of tissue healing?
Tissue healing proceeds in overlapping phases, and it’s crucial to understand these phases to tailor rehabilitation effectively:
- Inflammatory phase (0-7 days): Characterized by pain, swelling, redness, and heat. The body’s initial response is to contain damage and remove debris. Rest, ice, compression, and elevation (RICE) are key during this phase.
- Proliferative phase (7-21 days): Fibroblasts produce collagen, creating new tissue. Gentle range of motion exercises can begin to prevent scar tissue formation. The goal here is to promote healing and start gradually increasing tissue flexibility.
- Remodeling phase (21 days – 2 years): Collagen fibers are reorganized to increase strength and flexibility. Progressive loading exercises are introduced to strengthen the tissues. This phase can be lengthy, with ongoing tissue remodeling for up to two years.
It’s important to remember that these phases overlap, and the duration of each phase varies depending on the type and severity of injury. The rehabilitation program needs to adapt at each stage to support the healing process and avoid premature stress on the injured tissues.
Q 13. Explain the importance of proper body mechanics.
Proper body mechanics refers to using your body in the most efficient and safe way to perform any activity. Maintaining good body mechanics minimizes strain on your joints, muscles, and ligaments, reducing the risk of injury and promoting optimal performance.
Key principles of proper body mechanics include:
- Posture: Maintaining good posture—whether standing, sitting, or lifting—reduces strain on the spine and other joints. This includes keeping your back straight, shoulders relaxed, and core engaged.
- Lifting techniques: When lifting heavy objects, bend at your knees and hips, keeping your back straight, and lift with your legs. Avoid twisting your body.
- Ergonomics: Setting up your workspace correctly – proper chair height, monitor placement, and keyboard position – can prevent musculoskeletal strain.
- Body awareness: Being conscious of how you’re moving and making adjustments to minimize strain is a crucial aspect.
Improper body mechanics can lead to various musculoskeletal problems, including back pain, neck pain, carpal tunnel syndrome, and other overuse injuries. Incorporating proper body mechanics in daily activities significantly contributes to long-term musculoskeletal health and injury prevention.
Q 14. How do you incorporate patient goals into a rehabilitation plan?
Incorporating patient goals is essential to create a motivating and effective rehabilitation plan. It makes the process patient-centered and meaningful.
My approach involves:
- Early goal setting: During initial assessments, I actively discuss the patient’s personal goals, understanding their aspirations and expectations for recovery.
- Collaborative goal setting: We work together to establish realistic, measurable, achievable, relevant, and time-bound (SMART) goals. This ensures that the goals are both challenging and attainable.
- Goal prioritization: If the patient has multiple goals, we prioritize them to create a structured approach to the rehabilitation process.
- Regular goal review: Throughout the rehabilitation process, we regularly review progress toward established goals, adjusting them as needed based on the patient’s progress and changing circumstances.
- Functional goals: Goals focus on the patient’s ability to perform daily activities, return to work or hobbies, and improve overall quality of life.
For example, a patient might set a goal of being able to walk a mile without pain within a certain timeframe. Or they may want to be able to carry groceries or play with their grandchildren without difficulty. By focusing on these individual goals, the rehabilitation plan becomes personalized and the patient feels more engaged and motivated.
Q 15. What are the signs and symptoms of a rotator cuff tear?
Rotator cuff tears involve damage to the group of four muscles and their tendons that stabilize the shoulder joint. Symptoms vary depending on the severity of the tear.
- Pain: Often felt in the shoulder, sometimes radiating down the arm. Pain can be worse at night or with overhead activities.
- Weakness: Difficulty lifting or rotating the arm, particularly in activities like reaching for objects overhead or behind the back.
- Stiffness: Reduced range of motion in the shoulder joint, making it hard to fully move your arm in any direction.
- Clicking or popping: A noticeable sound or sensation in the shoulder during movement.
- Swelling: Though not always present, some swelling might occur around the shoulder joint.
For example, a patient might describe difficulty combing their hair or reaching for items on a high shelf. The pain might be a dull ache or a sharp stabbing pain, depending on the extent of the tear.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you assess and treat carpal tunnel syndrome?
Carpal tunnel syndrome is a condition caused by compression of the median nerve as it passes through the carpal tunnel in the wrist. Assessment typically involves a combination of:
- Physical exam: I’d assess for tenderness, swelling, and diminished sensation in the thumb, index, middle, and radial half of the ring finger. Tests like Phalen’s maneuver (holding wrists in flexion) or Tinel’s sign (tapping over the median nerve) may elicit tingling or pain.
- Nerve conduction studies (NCS) and electromyography (EMG): These are objective tests used to measure the speed of nerve conduction and the electrical activity of muscles. They help confirm the diagnosis and rule out other conditions.
Treatment starts conservatively with:
- Splinting: To keep the wrist in a neutral position, reducing pressure on the median nerve.
- Medication: Non-steroidal anti-inflammatory drugs (NSAIDs) or corticosteroids to reduce pain and inflammation.
- Therapy: Exercises to improve range of motion and strengthen wrist muscles.
If conservative treatment fails, surgical intervention (carpal tunnel release) might be considered to relieve the pressure on the median nerve. It’s crucial to remember that early intervention is key to achieving better outcomes.
Q 17. Describe your experience with lower back pain management.
Lower back pain is a very common problem. My approach to management is comprehensive and individualized. It always begins with a thorough history and physical examination to identify the underlying cause. This includes assessing posture, range of motion, muscle strength, and neurological function.
Treatment strategies often involve:
- Education: Explaining the nature of the pain, potential causes, and self-management techniques.
- Manual therapy: Techniques like spinal manipulation, soft tissue mobilization, and stretching to improve joint mechanics and reduce muscle tension.
- Exercise therapy: A tailored program focusing on core strengthening, postural correction, and flexibility exercises. This might include exercises like planks, bridges, and back extensions.
- Modalities: Using modalities like heat, ice, ultrasound, or electrical stimulation to manage pain and inflammation.
- Patient education on posture and ergonomics: Improving workstation setup, lifting techniques, and overall body mechanics is critical for long-term management.
In cases of severe or persistent pain, I may refer the patient for imaging studies (X-rays, MRI) to rule out more serious conditions like disc herniation or spinal stenosis. In some cases, medication such as analgesics or muscle relaxants might be considered. I believe in empowering patients to actively participate in their recovery through education and a collaborative approach.
Q 18. Explain the difference between osteoarthritis and rheumatoid arthritis.
Osteoarthritis (OA) and rheumatoid arthritis (RA) are both forms of arthritis, but they differ significantly in their cause and characteristics.
- Osteoarthritis (OA): This is a degenerative joint disease, primarily caused by the breakdown of cartilage. It’s often associated with aging, overuse, or injury. OA typically affects specific joints, such as knees, hips, and hands. It’s characterized by gradual onset of pain and stiffness, with pain often worsening after activity and improving with rest. Joint swelling is usually minimal.
- Rheumatoid arthritis (RA): This is an autoimmune disease, where the body’s immune system attacks the joints. It’s usually symmetric, meaning that it affects the same joint on both sides of the body (e.g., both knees, both hands). RA can cause significant inflammation and joint destruction, leading to pain, swelling, stiffness, and deformity. The onset is often more rapid than OA and symptoms are worse in the morning or after periods of inactivity.
In essence, OA is a ‘wear-and-tear’ disease, while RA is an inflammatory disease. Imaging studies can help differentiate between them, with OA showing evidence of cartilage loss and bone spurs, while RA may show joint inflammation and erosion.
Q 19. How do you manage a patient with osteoporosis?
Osteoporosis is a condition characterized by decreased bone mass and density, leading to increased risk of fractures. Management involves a multifaceted approach:
- Medication: Bisphosphonates, denosumab, or teriparatide are commonly prescribed to increase bone density and reduce fracture risk. The specific choice depends on individual factors and risk assessment.
- Lifestyle modifications: This is crucial and includes:
- Weight-bearing exercise: Walking, jogging, and weight training help stimulate bone formation.
- Dietary changes: Adequate calcium and vitamin D intake are essential for bone health. A balanced diet rich in fruits, vegetables, and protein is recommended.
- Smoking cessation: Smoking significantly increases the risk of osteoporosis and fractures.
- Alcohol moderation: Excessive alcohol consumption can negatively impact bone health.
- Fall prevention: Measures to reduce the risk of falls are essential, such as improving home safety, addressing balance issues, and adapting footwear.
- Regular monitoring: Bone density scans (DXA) are used to track the effectiveness of treatment and assess the risk of fractures.
A personalized plan, tailored to the individual’s needs and risk factors, is critical for effective management.
Q 20. What are the common complications associated with musculoskeletal injuries?
Musculoskeletal injuries can have several potential complications, depending on the type and severity of the injury:
- Chronic pain: Persistent pain that can significantly impact daily life, leading to reduced quality of life.
- Joint stiffness and limited range of motion: Scar tissue formation and muscle shortening can restrict joint mobility.
- Muscle weakness and atrophy: Reduced muscle strength and size due to disuse or nerve damage.
- Arthritis: Damage to the joint cartilage can lead to the development of osteoarthritis in the future.
- Infection: Open wounds are at risk of infection, which can have serious implications.
- Complex regional pain syndrome (CRPS): A chronic pain condition that can develop after an injury.
- Malunion or nonunion: Fractures that heal improperly, leading to deformity or instability.
- Neurological complications: Nerve damage can cause numbness, tingling, weakness, or pain in the affected area.
These complications highlight the importance of early intervention, proper rehabilitation, and appropriate management of musculoskeletal injuries to minimize long-term consequences.
Q 21. How do you document patient progress in rehabilitation?
Accurate and thorough documentation of patient progress is critical in musculoskeletal rehabilitation. I use a combination of methods:
- Subjective reports: Recording the patient’s self-reported pain levels (using scales like the visual analog scale or numerical rating scale), functional limitations, and overall progress using standardized questionnaires (e.g., Oswestry Disability Index for back pain).
- Objective measurements: Quantifiable data such as range of motion (measured with a goniometer), muscle strength testing (using a handheld dynamometer), functional tests (e.g., timed up-and-go test), and gait analysis.
- Progress notes: Regularly documenting the patient’s response to treatment, changes in symptoms, and adjustments to the treatment plan. This might include notes on the type of exercises performed, their tolerance, and any adverse effects.
- Photographs and videos: Visual documentation can be helpful in tracking progress in areas such as posture, gait, and range of motion.
This comprehensive approach ensures that the patient’s progress is accurately reflected, allowing for timely adjustments to the treatment plan and providing a detailed record for future reference. I maintain meticulous records in compliance with HIPAA regulations and professional standards.
Q 22. Explain the use of biofeedback in musculoskeletal rehabilitation.
Biofeedback is a powerful tool in musculoskeletal rehabilitation. It involves providing patients with real-time information about their physiological responses, such as muscle activity (electromyography or EMG), temperature, or heart rate. This allows them to gain conscious control over these responses, improving their ability to manage pain and dysfunction.
For example, a patient with chronic back pain might use EMG biofeedback to learn how to relax their paraspinal muscles, which often tense up in response to pain. Visual or auditory feedback from the EMG device shows them when their muscles are relaxing, reinforcing this behaviour. Another example includes using temperature biofeedback to help patients improve blood flow to an injured limb, accelerating healing. The process typically involves placing sensors on the skin near the affected area, and then providing the feedback through a visual display (like a bar graph) or an auditory tone. The patient learns to consciously modulate their physiological response to achieve a desired outcome, like muscle relaxation or increased temperature.
Q 23. Describe your experience with neuromuscular re-education techniques.
Neuromuscular re-education focuses on retraining the nervous system to improve muscle control and coordination. My experience encompasses a wide range of techniques, including:
- Proprioceptive Neuromuscular Facilitation (PNF): I frequently use PNF techniques, such as rhythmic initiation and hold-relax, to improve muscle strength, flexibility, and coordination. For instance, with a patient recovering from a knee injury, PNF can help restore normal gait patterns by improving quadriceps activation and hamstring flexibility.
- Functional electrical stimulation (FES): I have employed FES in cases of muscle weakness or paralysis. FES uses electrical impulses to stimulate muscles, helping to maintain muscle mass and improve function. I’ve successfully used it with patients recovering from stroke or spinal cord injuries to help restore some movement and function in affected limbs.
- Mirror therapy: This technique uses visual feedback to improve motor control and reduce pain. Patients observe the movement of their unaffected limb reflected in a mirror, which stimulates the brain to relearn the movement in the affected limb. I’ve found it effective for patients with complex regional pain syndrome (CRPS) or stroke.
These techniques aren’t used in isolation; I carefully tailor the program to the individual patient’s needs, goals, and condition, often combining several approaches for optimal results.
Q 24. What is your approach to managing patients with chronic pain?
Managing chronic pain requires a holistic approach that goes beyond simply addressing the physical symptoms. My strategy combines:
- Thorough assessment: This includes a comprehensive evaluation of the patient’s physical, psychological, and social factors contributing to their pain.
- Patient education: Educating patients about their condition, pain mechanisms, and the treatment plan is crucial for their involvement and adherence.
- Graded exercise therapy: Carefully progressed exercise programs are central to improving function and reducing pain. This ensures the patient doesn’t get discouraged or re-injured.
- Cognitive Behavioral Therapy (CBT): CBT techniques help patients develop coping mechanisms to manage their pain and improve their overall well-being. This is especially important for chronic pain, which often has a significant psychological impact.
- Pharmacological management: In some cases, medication may be necessary, but I always advocate for a multimodal approach, minimizing reliance on medication alone.
- Interdisciplinary collaboration: I often collaborate with other healthcare professionals, such as psychologists and physicians, to provide comprehensive care.
For example, a patient with fibromyalgia might benefit from a combination of gentle aerobic exercise, CBT to manage their emotional response to pain, and medication to help sleep. The key is personalization; no two patients are alike, and treatment plans must adapt to the individual needs.
Q 25. How do you prioritize patient care in a busy clinical setting?
Prioritizing patient care in a busy setting requires efficient time management and skillful decision-making. My approach involves:
- Triaging patients: Prioritizing patients based on the urgency of their needs – those with acute injuries or severe pain often require immediate attention.
- Streamlined assessments: Efficient and targeted assessments focus on the most relevant information, avoiding unnecessary delays.
- Delegation: When appropriate, I delegate tasks to other members of the healthcare team, like assistants or other therapists, to optimize workflow.
- Effective communication: Clear and concise communication with patients, their families, and other healthcare professionals is essential for coordinated care and minimizes misunderstandings.
- Time-blocking: Scheduling appointments and allocating specific time slots for various tasks helps manage the workload and prevents overbooking.
- Continuous self-reflection: Regularly reviewing my workflow helps identify areas for improvement and optimize efficiency.
I also actively participate in continuing education to improve my skills and stay updated with evidence-based practices, thus ensuring I provide optimal care within the time constraints of a busy clinical environment.
Q 26. Describe your experience with different types of assistive devices.
My experience with assistive devices is extensive and includes:
- Orthotics: I’ve fitted and prescribed various orthotics, including ankle-foot orthoses (AFOs), knee braces, and custom-fabricated foot orthoses, to improve gait, stability, and reduce pain. For instance, I’ve prescribed AFOs to patients with drop foot and custom foot orthoses to alleviate plantar fasciitis.
- Prosthetics: While I don’t directly fabricate prosthetics, I collaborate with prosthetists to ensure proper fitting and functional training for amputee patients. This often includes gait training and instruction on prosthetic use.
- Mobility aids: I regularly assess patient needs for mobility aids like canes, walkers, and wheelchairs, ensuring proper fitting and training on safe and effective use.
- Adaptive equipment: I also work with adaptive equipment, such as reachers, dressing aids, and adaptive utensils, to promote independence in daily activities for patients with limited mobility or dexterity.
My experience ensures I can effectively assess patient needs, recommend appropriate devices, and provide necessary training to maximize their functional outcomes and improve their quality of life.
Q 27. Explain your understanding of evidence-based practice in musculoskeletal rehabilitation.
Evidence-based practice (EBP) is central to my work. It means integrating the best available research evidence with clinical expertise and patient values to make informed decisions about patient care. This involves:
- Identifying clinical questions: Clearly defining the specific problem or question I need to address for a particular patient.
- Searching for relevant research: Using reliable databases to locate high-quality studies that address the clinical question. This often involves understanding the methodology and critical appraisal of research.
- Critically appraising the evidence: Assessing the quality, validity, and applicability of the research to my patient population.
- Integrating evidence with clinical expertise and patient values: Considering my own experience, the patient’s preferences, and the available resources in formulating a treatment plan. This requires effective communication with the patient to understand their perspective and ensure shared decision-making.
- Evaluating outcomes: Monitoring the effectiveness of the treatment plan and making adjustments as needed. This involves ongoing assessment and feedback, reflecting the iterative nature of EBP.
By consistently adhering to EBP principles, I ensure that my practice is informed by the best available science, leading to the most effective and safe care for my patients.
Q 28. How do you handle challenging or uncooperative patients?
Handling challenging or uncooperative patients requires patience, empathy, and strong communication skills. My approach involves:
- Understanding the root cause: I attempt to understand the underlying reasons for the patient’s behavior. This may involve exploring their anxieties, fears, past experiences, or unmet needs.
- Active listening: Paying close attention to the patient’s concerns and validating their feelings. This shows respect and encourages open communication.
- Collaborative goal setting: Working with the patient to develop realistic and achievable goals that they feel invested in. This increases their sense of control and ownership of the process.
- Modifying the treatment plan: Being flexible and adapting the treatment plan to accommodate the patient’s preferences and limitations. This shows willingness to work with them, rather than against them.
- Seeking support: When necessary, I seek support from other healthcare professionals, such as psychologists or social workers, to address any psychological or social barriers to care.
- Setting clear boundaries: While aiming for collaboration, it’s crucial to set clear professional boundaries to ensure a safe and effective therapeutic relationship.
It is important to remember that every patient is an individual, and sometimes, despite my best efforts, a positive therapeutic relationship may not be possible. In such instances, a referral to another practitioner may be necessary.
Key Topics to Learn for Musculoskeletal Rehabilitation Interview
- Biomechanics of Movement: Understanding joint kinematics, kinetics, and muscle mechanics is fundamental. Consider how these principles apply to various pathologies.
- Assessment and Examination Techniques: Master the skills of subjective and objective assessment, including range of motion measurements, muscle strength testing, and special tests. Practice explaining your reasoning behind chosen assessments.
- Pathology and Treatment of Musculoskeletal Conditions: Develop a strong understanding of common conditions like osteoarthritis, rheumatoid arthritis, rotator cuff tears, and low back pain. Be prepared to discuss various treatment approaches, including manual therapy, exercise prescription, and modalities.
- Exercise Prescription and Program Design: Learn how to design safe and effective exercise programs tailored to individual patient needs and goals, considering factors like age, comorbidities, and functional limitations. Be ready to justify your exercise choices.
- Patient Education and Communication: Effective communication is crucial. Practice explaining complex medical information in a clear and understandable way. Consider how to motivate patients and build rapport.
- Rehabilitation Techniques: Familiarize yourself with various manual therapy techniques, therapeutic exercise modalities, and assistive devices. Be prepared to discuss the rationale behind your chosen interventions.
- Evidence-Based Practice: Understand the importance of using current research to guide your clinical decision-making. Be ready to discuss relevant studies and how they inform your practice.
- Ethical and Legal Considerations: Review professional standards of practice, informed consent, and documentation requirements.
Next Steps
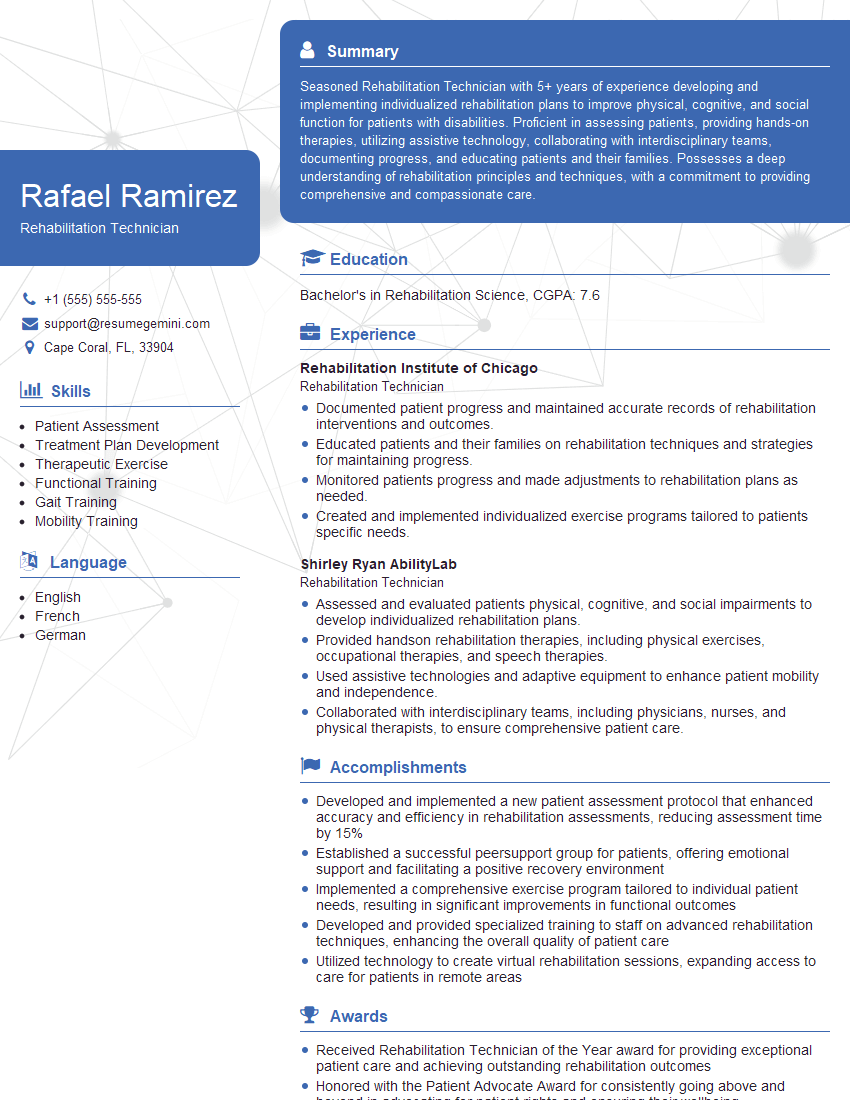
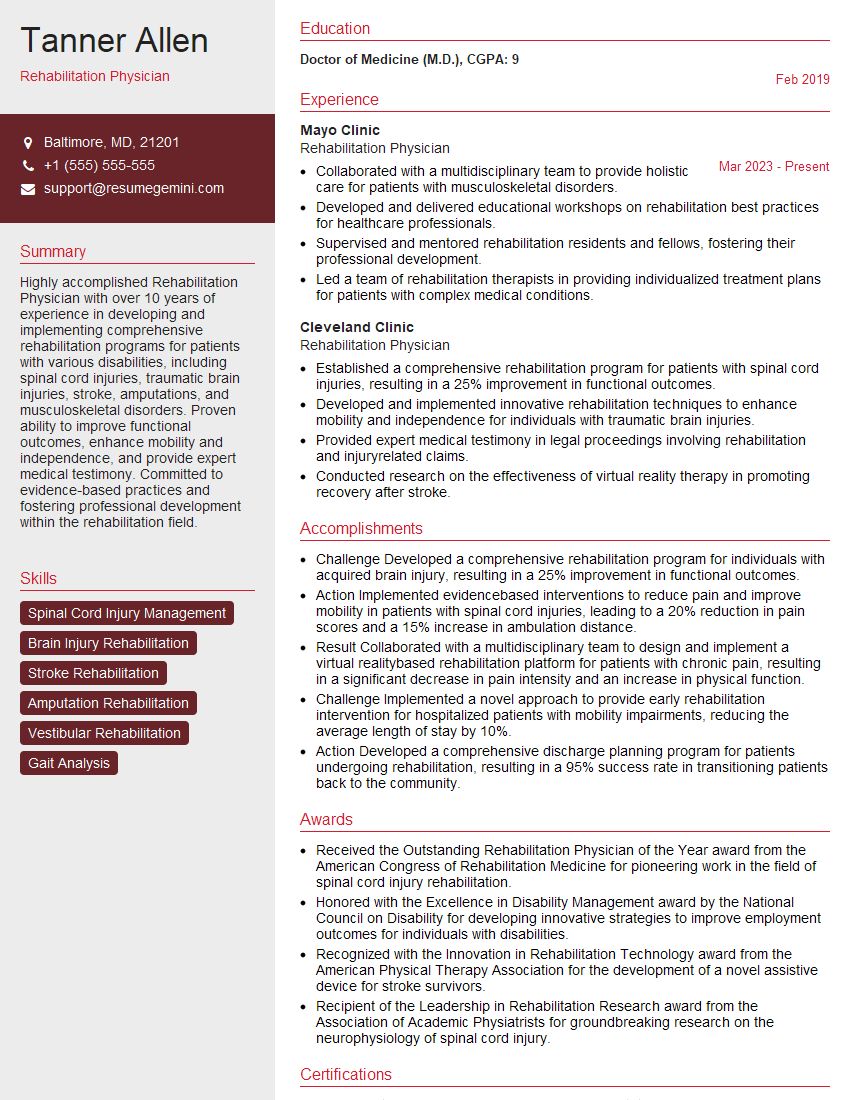
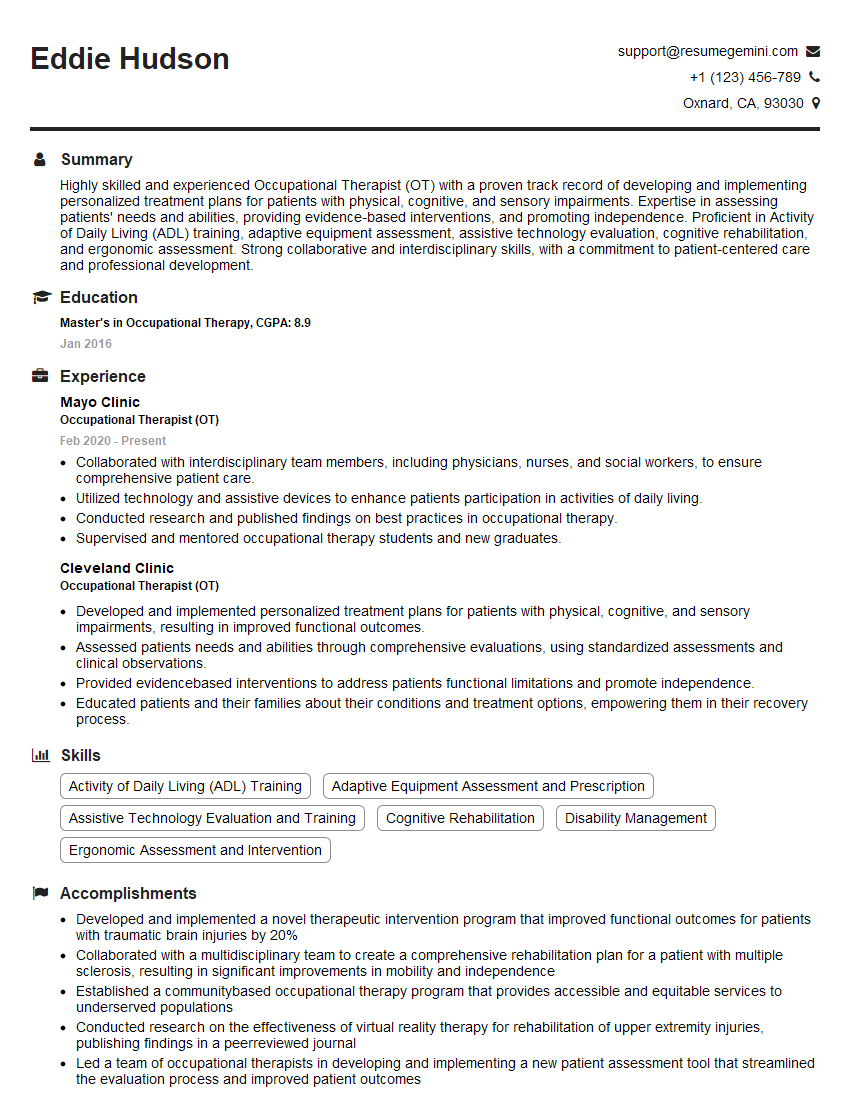
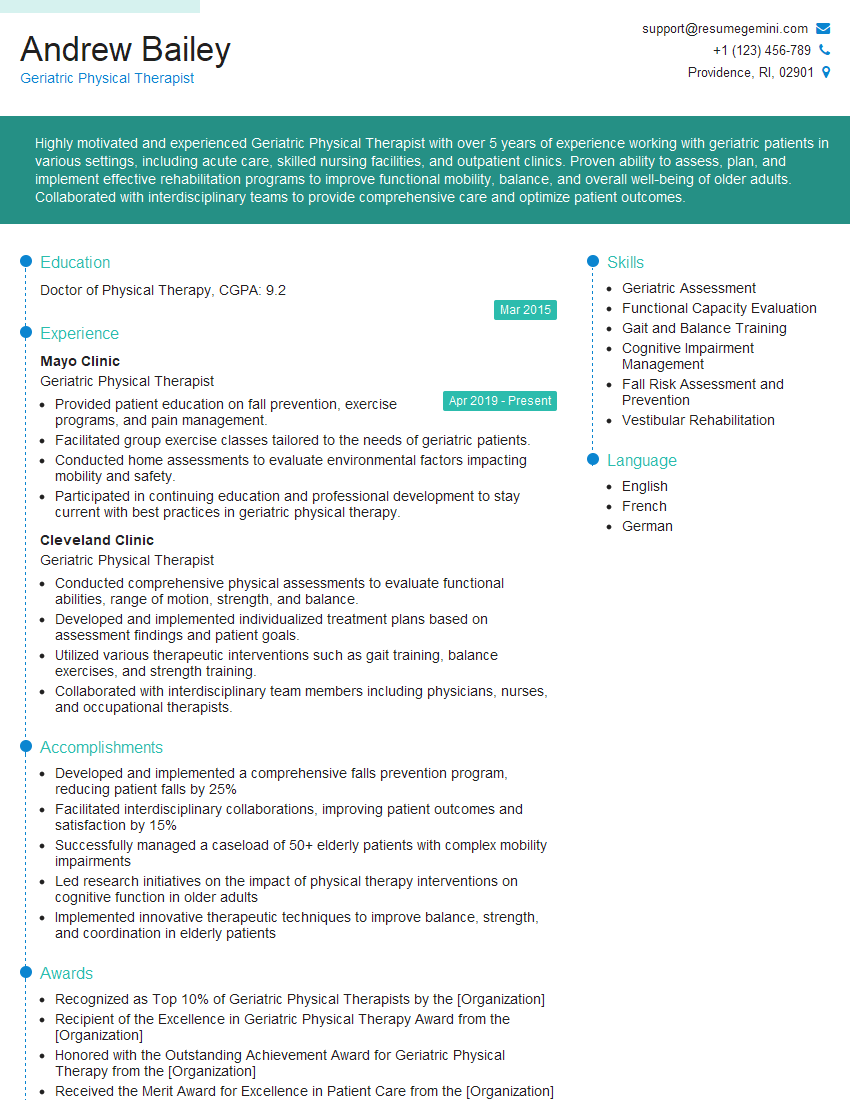
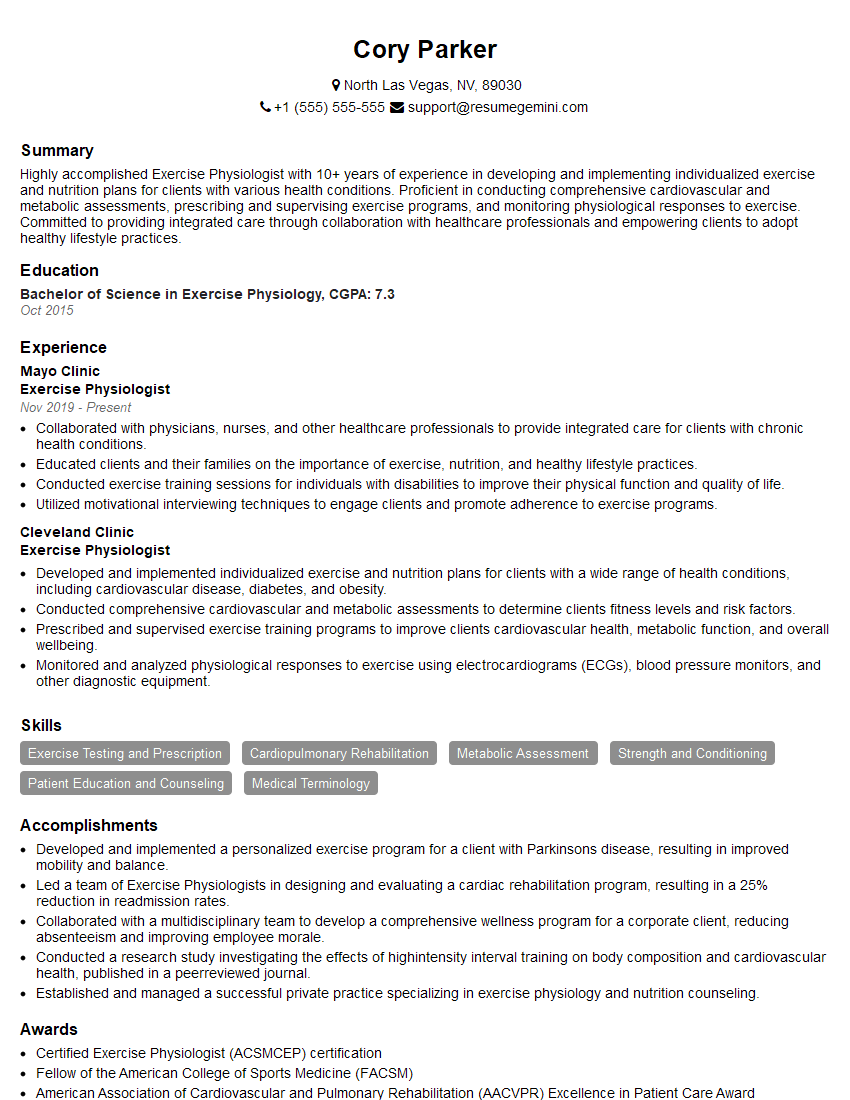
Mastering Musculoskeletal Rehabilitation opens doors to a rewarding career with diverse opportunities for growth and specialization. A strong resume is your key to unlocking these prospects. Crafting an ATS-friendly resume is essential to ensure your application gets noticed. ResumeGemini is a trusted resource that can help you build a professional and impactful resume tailored to the specific requirements of Musculoskeletal Rehabilitation roles. Examples of resumes tailored to this field are available to guide you. Invest time in building a compelling resume to highlight your skills and experience effectively – it’s your first impression and sets the stage for a successful interview.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.