The thought of an interview can be nerve-wracking, but the right preparation can make all the difference. Explore this comprehensive guide to Developmental Coordination Disorder Treatment interview questions and gain the confidence you need to showcase your abilities and secure the role.
Questions Asked in Developmental Coordination Disorder Treatment Interview
Q 1. Describe the diagnostic criteria for Developmental Coordination Disorder (DCD).
Developmental Coordination Disorder (DCD) diagnosis relies on observing significant delays in motor skill development compared to age-matched peers. It’s not simply clumsiness; it impacts daily activities and academic performance. The DSM-5 criteria require:
- Marked impairment in the development of motor coordination, as manifested by clumsiness, slowness, and inaccuracy of performance of motor skills.
- Motor skills deficits interfere with academic/vocational activities or activities of daily living.
- Onset is in the early developmental period.
- Impairment is not better explained by intellectual disability, neurological condition, or another medical condition.
Essentially, the child’s motor difficulties must be significant enough to impact their daily life and be present from early childhood, ruling out other potential causes.
Q 2. What are the common motor impairments observed in children with DCD?
Children with DCD exhibit a range of motor impairments, often impacting both fine and gross motor skills. Common observations include:
- Gross Motor Difficulties: Difficulty with running, jumping, hopping, skipping, catching, throwing, and balancing. For example, a child might struggle to ride a bike or participate in team sports.
- Fine Motor Difficulties: Challenges with writing, drawing, using scissors, buttoning clothes, and tying shoelaces. This can lead to difficulties in schoolwork and self-care.
- Coordination Problems: Poor hand-eye coordination, bilateral coordination (using both hands together), and timing difficulties.
- Postural Instability: Frequent falls, difficulty maintaining balance, and poor posture.
- Sequencing Difficulties: Problems with planning and carrying out complex motor sequences, such as assembling toys or following multi-step instructions.
The severity and combination of these impairments vary significantly between individuals.
Q 3. Explain the difference between apraxia and dyspraxia in the context of DCD.
While both apraxia and dyspraxia involve difficulties with motor planning and execution, they differ in their severity and underlying mechanisms. Dyspraxia, often used synonymously with DCD, encompasses a broader range of motor difficulties. It’s characterized by inconsistent performance, where the child may sometimes perform a task correctly and other times struggle. They may struggle with the organization and execution of movements.
Apraxia, on the other hand, is a more severe condition involving significant difficulty in planning and executing purposeful movement, even when muscle strength and coordination are not impaired. Apraxia is often associated with neurological damage or conditions and manifests as a significant deficit in motor planning, rather than just execution. It’s considered a more specific diagnosis within the spectrum of developmental motor problems.
In the context of DCD, dyspraxia is the more commonly used and applicable term, reflecting the developmental challenges with motor skills that are less severe than the profound motor planning deficits seen in apraxia.
Q 4. What assessment tools would you utilize to evaluate a child suspected of having DCD?
A thorough assessment of a child suspected of having DCD requires a multi-faceted approach involving various tools. Key assessments include:
- Developmental History: A detailed account of the child’s motor development from infancy, obtained through parent interviews and questionnaires.
- Observation of Motor Skills: Direct observation of the child performing various motor tasks, such as those found on standardized assessments.
- Standardized Motor Tests: These include tests like the Movement Assessment Battery for Children (MABC-2) or the Bruininks-Oseretsky Test of Motor Proficiency (BOT-2), which provide quantitative measures of motor skills across various domains.
- Parent/Teacher Questionnaires: These assess the child’s functional limitations in daily life and academic settings. Examples include the DCDQ ’07 (Developmental Coordination Disorder Questionnaire).
- Cognitive and Academic Assessments: To rule out other contributing factors and evaluate the impact of DCD on academic performance.
A comprehensive evaluation helps to build a clear picture of the child’s strengths and weaknesses, guiding the development of an effective treatment plan.
Q 5. Outline a comprehensive treatment plan for a child with DCD, incorporating various therapeutic approaches.
A comprehensive treatment plan for DCD should be individualized and tailored to the child’s specific needs and strengths. It should encompass a variety of therapeutic approaches, including:
- Occupational Therapy: This is a cornerstone of DCD treatment, focusing on improving motor skills through targeted activities and exercises. Techniques may include sensory integration activities, task-specific training, and adaptive strategies.
- Physical Therapy: Addresses gross motor skills, balance, coordination, and posture. It involves exercises to improve strength, endurance, and agility.
- Psychoeducational Interventions: Help the child develop strategies for managing challenges in school, social settings, and daily life. This might involve strategies for self-advocacy and organization.
- Behavioral Therapy: May be helpful to address any emotional or behavioral difficulties associated with DCD.
- Adaptive Equipment: Using assistive devices, such as weighted utensils or adapted writing tools, can improve functional performance.
- Parent/Teacher Training: Educating parents and teachers on how to support the child’s motor development and adapt their environment.
Regular monitoring and adjustment of the treatment plan are crucial to ensure its effectiveness.
Q 6. How do you adapt treatment strategies based on a child’s age and developmental stage?
Treatment strategies must be adapted based on the child’s age and developmental stage. Younger children might benefit from play-based interventions focusing on fundamental motor skills, while older children might require more task-specific training focused on academic or vocational needs. For example:
- Preschoolers: Play-based activities focusing on fundamental movement skills, sensory integration, and improving body awareness.
- School-aged Children: Focus on handwriting skills, sports-specific training, and strategies for managing classroom demands.
- Adolescents: Emphasis on activities relevant to their interests, such as driving skills, vocational training, and strategies for self-management and independence.
The complexity and intensity of the interventions are adjusted according to the child’s developmental level and the identified areas of difficulty.
Q 7. Describe your experience using sensory integration techniques in DCD treatment.
Sensory integration techniques are frequently incorporated into DCD treatment. Many children with DCD experience difficulties processing sensory information, which can affect their motor performance. Sensory integration therapy aims to improve the child’s ability to organize and use sensory information for effective motor planning and execution.
My experience shows that sensory integration can be particularly beneficial for children who exhibit significant sensory sensitivities or poor postural control. Activities may include:
- Proprioceptive activities: Activities that involve weight-bearing and resistance, such as climbing, crawling, and using weighted blankets, improve body awareness and stability.
- Vestibular activities: Activities that stimulate the inner ear, such as swinging, spinning, and rocking, improve balance and coordination.
- Tactile activities: Using various textures and materials to improve tactile discrimination and hand function.
The effectiveness of sensory integration is carefully monitored, and interventions are adapted based on the child’s response. While not a cure-all, it’s a valuable tool in the overall treatment plan, often enhancing the effectiveness of other therapeutic approaches. For instance, a child with poor tactile discrimination might struggle with fine motor tasks; sensory integration activities could improve tactile awareness and subsequently, their fine motor skills.
Q 8. What are the potential co-occurring conditions associated with DCD?
Developmental Coordination Disorder (DCD) often co-occurs with other conditions. Think of it like this: DCD is a difficulty with motor skills, but it can exist alongside other challenges that impact a child’s overall development. These co-occurring conditions can significantly influence the presentation and treatment of DCD.
- Learning Disabilities: Many children with DCD also have difficulties with reading, writing, or math (dyslexia, dysgraphia, dyscalculia). The motor difficulties can impact handwriting and fine motor tasks essential for academic success.
- Attention-Deficit/Hyperactivity Disorder (ADHD): Inattention, impulsivity, and hyperactivity are common in both DCD and ADHD. The overlap can make diagnosis and treatment more complex, requiring a comprehensive assessment.
- Speech and Language Impairments: Difficulties with articulation, expressive language, or receptive language are frequently seen alongside DCD, potentially impacting communication and social interaction.
- Social and Emotional Challenges: Children with DCD may experience low self-esteem, anxiety, or depression due to frustrations with their motor skills. These emotional challenges can further impact their participation in school and social activities.
- Autism Spectrum Disorder (ASD): While not always co-occurring, there can be overlap in motor challenges and social communication difficulties.
Recognizing these co-occurring conditions is crucial for developing a holistic treatment plan that addresses all aspects of the child’s needs. We often collaborate with other professionals, such as occupational therapists, speech therapists, and educational psychologists, to provide comprehensive care.
Q 9. How do you collaborate with parents and other professionals involved in a child’s care?
Collaboration is the cornerstone of effective DCD treatment. I believe in a team approach, working closely with parents and other professionals to ensure the child receives the best possible care. My collaboration strategy involves:
- Regular communication with parents: I maintain open communication channels, providing regular updates on the child’s progress, discussing challenges, and collaboratively setting goals. Parents are invaluable sources of information about their child’s strengths and weaknesses in various environments.
- Collaborative goal setting: Parents, the child (when appropriate), and I work together to establish realistic and achievable goals. This shared understanding ensures everyone is on the same page and promotes buy-in from the child and family.
- Multidisciplinary team meetings: When necessary, I convene meetings with other professionals involved in the child’s care, such as occupational therapists, teachers, and psychologists. This allows us to share information, coordinate interventions, and ensure a consistent approach.
- Providing education and support: I provide parents with information about DCD, strategies to support their child at home, and resources for additional support. This empowers parents to actively participate in their child’s therapy and overall development.
For example, in one case, I worked closely with a child’s teacher to modify classroom activities to better suit his motor skills, making tasks less physically demanding and providing extra time for completion. This collaboration resulted in a significant improvement in his academic performance and self-confidence.
Q 10. Explain your approach to incorporating technology in DCD therapy.
Technology plays an increasingly important role in DCD therapy. It offers engaging and motivating ways to improve motor skills and enhance the therapeutic process. I use technology in several ways:
- Interactive games and apps: Many apps provide engaging activities that target specific motor skills, such as hand-eye coordination, balance, and fine motor control. These apps often provide immediate feedback and progress tracking, keeping the child motivated.
- Virtual reality (VR) therapy: VR offers immersive and playful experiences that can be used to improve gross motor skills, balance, and spatial awareness. The gamified nature of VR often makes therapy more enjoyable and effective.
- Biofeedback devices: These devices can help children become more aware of their body movements and improve their control. For example, a device might monitor muscle tension during writing, providing feedback to help the child relax and improve their handwriting.
- Teletherapy: Technology allows for remote therapy sessions, which can be beneficial for children in remote areas or those with transportation challenges.
However, it’s crucial to remember that technology should be a supplement to, not a replacement for, hands-on therapy. The human interaction and individualized attention provided by a therapist remain essential.
Q 11. How do you measure the effectiveness of your DCD treatment interventions?
Measuring the effectiveness of DCD interventions requires a multi-faceted approach. We use a combination of methods to assess progress, ensuring a comprehensive understanding of the child’s improvement:
- Standardized assessments: These are formal tests designed to measure specific motor skills, such as the Movement Assessment Battery for Children (MABC-2). These assessments provide objective data on the child’s progress over time.
- Observation and qualitative data: I regularly observe the child’s performance during therapy sessions, noting improvements in skills, participation, and engagement. This helps to gain a more holistic understanding of their progress beyond standardized test scores.
- Parent and teacher reports: Feedback from parents and teachers provides valuable insights into the child’s functional skills in different environments. These reports offer a broader perspective on the impact of therapy on the child’s daily life.
- Goal attainment scaling (GAS): This method allows us to set individualized goals and track progress towards those goals. It provides a flexible and personalized way to measure the effectiveness of interventions.
By combining these methods, we gain a rich understanding of the child’s progress, allowing us to adjust our treatment approach as needed to optimize outcomes.
Q 12. Describe a challenging case involving DCD and how you overcame the obstacles.
One particularly challenging case involved a 9-year-old girl with severe DCD who also had significant anxiety. Her motor skills were significantly delayed, and her anxiety made it difficult for her to participate in therapy. She would often freeze or refuse to attempt new tasks.
To overcome these obstacles, I implemented a gradual desensitization approach. We started with very simple activities that she felt comfortable with, gradually increasing the challenge as her confidence grew. I incorporated play-based therapy and positive reinforcement to make the sessions enjoyable and motivating. I also worked closely with her parents and a child psychologist to address her anxiety. The psychologist helped her develop coping strategies for managing her anxiety, and we coordinated our interventions to ensure a consistent approach.
Over time, she started to show noticeable progress in her motor skills and her anxiety decreased significantly. The key was patience, a tailored approach, and strong collaboration with the family and other professionals involved. Seeing her progress and increased confidence was incredibly rewarding.
Q 13. What are the long-term goals of DCD treatment?
The long-term goals of DCD treatment extend far beyond just improving motor skills. Our aim is to empower children to participate fully in all aspects of their lives, leading fulfilling and independent lives.
- Improved motor skills: While essential, this is just one component. We strive to help children achieve age-appropriate motor skills in all areas (gross and fine motor skills).
- Enhanced self-esteem and confidence: Addressing the emotional impact of DCD is paramount. We aim to build the child’s self-esteem and confidence through success in therapy and adaptation of tasks.
- Increased independence: We strive to help children become more independent in daily activities, such as dressing, eating, and writing. This promotes autonomy and reduces reliance on others.
- Improved social participation: We address potential social challenges by improving communication skills and building social skills. This allows them to form positive relationships and participate fully in social settings.
- Academic success: We collaborate with schools to adapt activities and provide support to enhance academic performance.
Ultimately, our aim is to help children reach their full potential and live happy, productive lives, despite the challenges posed by DCD.
Q 14. How do you address social and emotional challenges faced by children with DCD?
Social and emotional challenges are often intertwined with DCD. Children may experience frustration, low self-esteem, anxiety, or depression due to their motor difficulties. Addressing these challenges is crucial for overall well-being and treatment success.
- Cognitive Behavioral Therapy (CBT): This approach helps children identify and challenge negative thoughts and behaviors related to their motor skills. It teaches them coping mechanisms to manage frustration and anxiety.
- Social skills training: This helps children improve their communication and interaction skills, increasing their ability to form positive relationships with peers and adults.
- Play therapy: This uses play as a medium to help children express their emotions and develop coping strategies. It provides a safe and fun environment for exploring challenges.
- Parent training: Educating parents on strategies to support their child’s emotional well-being is essential. This includes teaching them how to provide positive reinforcement, manage challenging behaviors, and create a supportive home environment.
It’s important to remember that addressing social and emotional challenges is an integral part of comprehensive DCD treatment. Ignoring these aspects can hinder progress and impact the child’s overall quality of life. We often collaborate with psychologists or other mental health professionals to provide specialized support in these areas.
Q 15. What are the potential limitations of different DCD treatment approaches?
Different DCD treatment approaches, while beneficial, have inherent limitations. For example, occupational therapy, a cornerstone of DCD intervention, can be limited by factors like the child’s motivation, the intensity and duration of therapy provided (availability and affordability play a role), and the family’s ability to support carryover activities at home. Similarly, physical therapy, focusing on gross motor skills, might not adequately address the fine motor challenges often seen in DCD. Specific interventions, like computer-aided programs for improving motor skills, can be costly and require access to technology and consistent internet connectivity. Furthermore, the effectiveness of any intervention varies significantly depending on the individual child’s specific needs, the severity of their DCD, and their response to treatment. A child’s developmental stage and co-existing conditions also influence the effectiveness of interventions. Finally, consistent adherence to treatment plans is crucial for success, and challenges with this adherence can limit outcomes.
For instance, a child with DCD might struggle with the repetitive practice required in motor skill training, leading to frustration and reduced participation. Or, a family’s inability to facilitate home-based exercises due to time constraints or other commitments might significantly impact progress. Therefore, a holistic approach that considers all these factors is essential for optimal results.
Career Expert Tips:
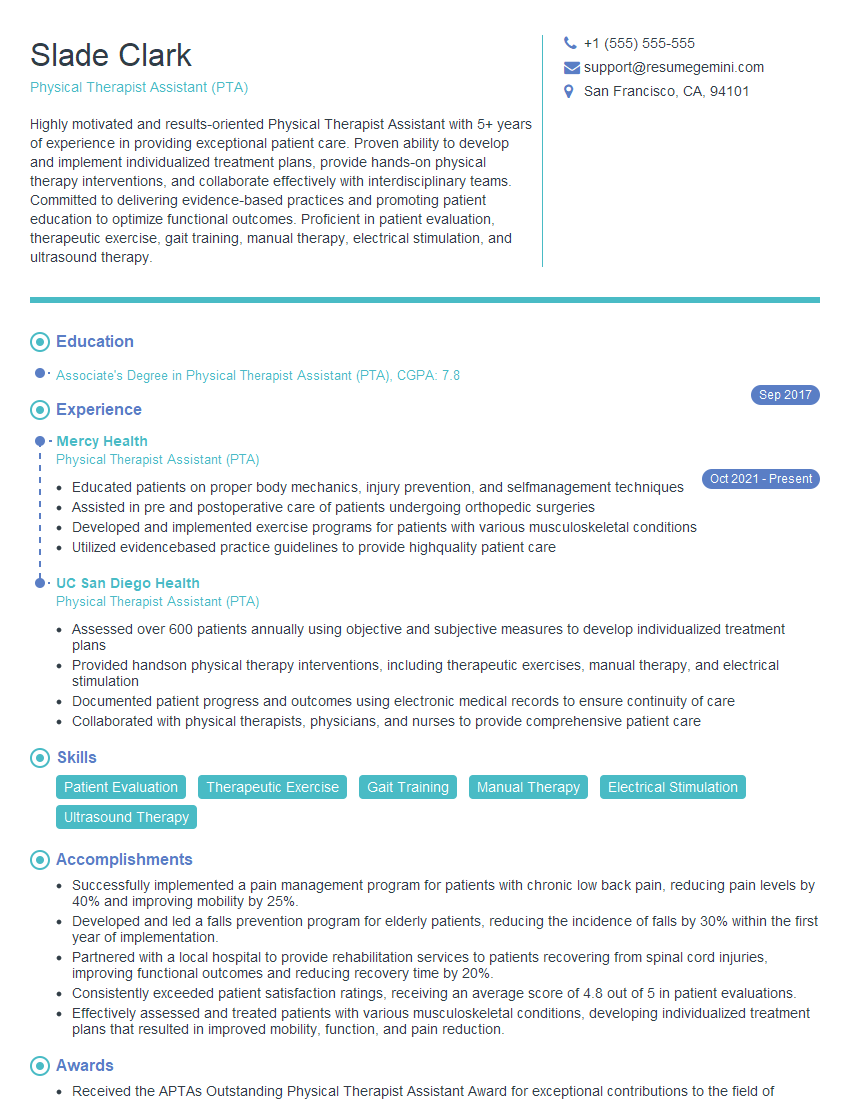
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Explain the role of family involvement in DCD management.
Family involvement is absolutely crucial for successful DCD management. Parents and caregivers are the child’s primary support system, and their active participation is critical for consistent implementation of treatment strategies. They act as vital partners in the therapy process, implementing the techniques and strategies learned during therapy sessions at home and in daily activities. This consistent reinforcement strengthens the child’s motor skills and builds confidence. Furthermore, families can play a key role in identifying environmental barriers and modifying the home environment to better support their child’s needs. They can help advocate for accommodations at school or in other settings. Regular communication between the therapist, the child, and the family is vital. A successful plan often involves structured discussions on goal setting, progress tracking, and strategies to navigate challenges at home and school.
For example, parents can help create a designated workspace free from distractions for homework or practice activities. They can break down complex tasks into smaller, manageable steps, encouraging the child with positive reinforcement. Open communication fosters understanding and encourages collaboration throughout the journey.
Q 17. How do you promote a child’s independence and self-esteem during DCD therapy?
Promoting independence and self-esteem is a central focus of DCD therapy. We achieve this by focusing on achievable goals, celebrating even small successes, and building the child’s self-efficacy. We start by setting realistic, incremental goals which build the child’s confidence. For example, instead of aiming for perfect handwriting immediately, we might start by focusing on improving letter formation or grip. Positive reinforcement, verbal praise, and encouragement are vital to build self-esteem. We also emphasize the child’s strengths and abilities, shifting the focus from deficits to capabilities. We encourage self-advocacy by involving them in the goal-setting process and empowering them to communicate their needs to teachers and peers.
We might use adaptive strategies, such as assistive technology or modifications to tasks, to enable the child to successfully complete activities, thereby boosting their confidence. For example, providing a weighted pencil to improve grip or using a speech-to-text program to reduce writing difficulties. The overall goal is to empower the child and build their belief in their own abilities.
Q 18. Discuss the importance of adapting the environment to support a child with DCD.
Adapting the environment is paramount for children with DCD. The environment should be organized, predictable, and supportive. This reduces the cognitive load associated with navigating daily activities and allows the child to focus on motor tasks rather than environmental challenges. Modifications can be simple yet effective. For instance, removing clutter, ensuring sufficient space for movement, providing tactile cues (e.g., colored tapes on the floor for walking lines), and adjusting the height of furniture. At school, accommodations might involve providing extra time for tasks, reducing the amount of written work, or allowing the use of assistive technology. In the classroom, designated spaces that are calm and less stimulating can help reduce sensory overload and improve focus. Visual aids, such as checklists and schedules, also contribute to the child’s organization and understanding of expectations.
For example, a child might struggle with navigating a crowded cafeteria. Adapting the environment might involve providing a designated quieter seating area where the child can eat lunch peacefully and avoid sensory overload. This strategy reduces stress and makes the experience more positive and less overwhelming.
Q 19. What are some strategies for improving handwriting skills in children with DCD?
Improving handwriting skills in children with DCD requires a multi-faceted approach. We begin by assessing the child’s current writing abilities, identifying specific areas of difficulty (e.g., grip, letter formation, spacing). We then use a combination of techniques. This can include practicing pre-writing skills such as finger exercises to strengthen fine motor control, focusing on proper pencil grip using adapted tools (e.g., tripod grip aids), and practicing letter formation through various activities like tracing, copying, and drawing. We incorporate visual aids like dotted lines or templates to guide letter formation. We also break down complex writing tasks into smaller, more manageable steps. Technology can also play a role, using assistive technologies like specialized software or keyboarding programs. Regular, short, and focused practice sessions are more effective than longer, less frequent sessions. Positive reinforcement and encouragement throughout the process are essential to maintain motivation.
For instance, starting with large-scale activities like practicing forming letters in sand or playdough can improve motor control before transitioning to pencil and paper exercises. Positive feedback on even small improvements is crucial to the child’s self-confidence and progress.
Q 20. How do you teach motor planning skills to children with DCD?
Teaching motor planning skills involves breaking down complex movements into smaller, sequential steps. We use visual aids, verbal instructions, and hands-on guidance. We might use a task analysis approach, where we break down a task, such as tying shoelaces, into individual steps. We then provide visual cues or instructions for each step. We use games and activities that involve planning and sequencing movements, such as building blocks, following instructions, and performing actions in a specific order. Role-playing and imitation are also valuable tools, allowing the child to observe and mimic sequences of movements. We emphasize verbal rehearsal, encouraging the child to think through the steps before performing the movement. Consistent practice and feedback are key to improving motor planning.
For example, when teaching a child to button a shirt, we might start by having them practice manipulating a single button and buttonhole, gradually increasing the complexity of the task. Visual aids showing the steps or using a doll to demonstrate the task can also greatly benefit a child’s understanding and performance.
Q 21. Describe your experience with using assistive technology to aid children with DCD.
Assistive technology plays a significant role in supporting children with DCD. I have extensive experience using various technologies to improve their academic, social, and daily living skills. These include, but are not limited to, ergonomic writing tools (weighted pencils, adapted grips), speech-to-text software, graphic organizers for planning, and word prediction programs for writing. I’ve found that assistive technology not only helps children complete tasks more efficiently but also increases their confidence and independence. The selection of assistive technology is highly individualized, based on the child’s specific needs and challenges. It’s critical to thoroughly assess the child’s abilities and limitations before recommending any particular technology. Training and support are essential to ensure that the child and their family can effectively use the technology. We often work collaboratively with assistive technology specialists to find optimal solutions.
For example, a child struggling with handwriting might benefit from a speech-to-text program that allows them to dictate their essays or stories. This removes the physical barrier of writing and allows them to focus on expressing their ideas. Another example would be using a tablet and stylus, combined with specific apps, which provide adaptive tools for writing and drawing.
Q 22. How do you address the challenges of transferring learned skills from therapy to daily life?
Generalizing skills learned in therapy to everyday life, a phenomenon known as ‘generalization,’ is a significant challenge in DCD treatment. It’s like learning to ride a bike in a controlled environment – a smooth, flat track – and then expecting to effortlessly navigate bumpy, uneven terrain. We address this by using a technique called ‘generalization planning.’ This involves carefully designing therapy sessions to mirror real-world situations.
Contextual Practice: We gradually introduce distractions and varying environments during therapy. For example, if we’re working on handwriting, we might start with a quiet room and then move to a slightly noisy classroom setting.
Task Variation: We vary the tasks, materials, and instructions. If a child is practicing tying shoes, we’ll use different types of laces and shoes.
Reinforcement and Feedback: Consistent positive reinforcement and feedback are crucial, both during therapy and when practicing skills at home. We empower parents to understand and continue this support at home, giving them clear instructions and strategies.
Self-Monitoring Techniques: We teach children to self-monitor their progress and identify situations where they might need additional support. This could involve using checklists or keeping a journal.
Collaboration with other professionals: We collaborate with teachers, occupational therapists, and other support staff to create a consistent approach across settings. This ensures that what’s learned in therapy is reinforced at school and home.
For instance, a child learning to organize their school backpack in therapy might then practice this same skill at home, starting with a structured approach and progressively reducing support as their independence grows.
Q 23. What is your experience with different types of feedback mechanisms in DCD treatment?
Feedback is vital in DCD treatment. It’s the navigational system guiding improvement. I utilize a variety of feedback methods, tailoring them to the individual child’s needs and learning style.
Intrinsic Feedback: This involves the child’s own sensory experience. For instance, feeling the weight of a pen and the texture of paper while writing.
Extrinsic Feedback: This comes from external sources. It can be:
Knowledge of Results (KR): This tells the child whether they succeeded or failed (e.g., ‘That’s a great throw!’).
Knowledge of Performance (KP): This explains how they performed (e.g., ‘Remember to keep your elbow straight when throwing’). KP is particularly helpful as it provides valuable insights.
Verbal Feedback: I use clear, concise language, focusing on specific aspects to improve, avoiding overwhelming criticism.
Visual Feedback: Using videos, mirrors, or diagrams to show children their movements can be powerfully insightful. They can literally see what they need to adjust.
Augmentative Feedback: This includes technologies like motion sensors or apps which provide real-time data on performance, allowing children to see their progress objectively.
I often combine different types of feedback to create a holistic approach, focusing on positive reinforcement and progressively fading support as the child’s skills improve.
Q 24. How do you differentiate between DCD and other conditions with similar symptoms?
Differentiating DCD from other conditions presenting similar symptoms requires careful assessment. It’s crucial to consider several factors. DCD is characterized by difficulties with motor skills that are not explained by intellectual disability, neurological conditions, or other medical conditions.
Comprehensive Assessment: We use standardized tests evaluating motor skills, including fine motor skills (e.g., handwriting, buttoning), gross motor skills (e.g., jumping, running, catching), and coordination.
Developmental History: We gather detailed information about the child’s developmental milestones, identifying any significant delays or difficulties.
Medical History: We review medical records to rule out other conditions that could explain the motor difficulties, such as cerebral palsy or muscular dystrophy.
Cognitive Assessment: We perform cognitive tests to evaluate intellectual functioning and ensure there isn’t an underlying intellectual disability contributing to the motor issues.
Observation: Direct observation of the child’s motor performance is essential. We note things like postural control, movement fluidity, and the ability to adapt to different tasks.
For instance, a child with ADHD may also show clumsiness, but this is often accompanied by inattention and hyperactivity. In contrast, a child with DCD may have difficulty with fine motor tasks despite having normal attention and concentration.
Q 25. Describe your understanding of the impact of DCD on academic performance.
DCD significantly impacts academic performance, often affecting multiple areas. Difficulties with handwriting, drawing, and using tools in classrooms can cause frustration and affect participation in activities. The impact is not always obvious and can manifest in many ways.
Written Work: Slow writing speed, illegible handwriting, and difficulties with spelling and drawing can lead to incomplete assignments and lower grades.
Participation: Difficulties with fine motor skills can impact participation in activities requiring manual dexterity, leading to social isolation.
Organization and Planning: Difficulties with planning and sequencing movements can affect organization, leading to a lack of preparation and poor time management.
Self-Esteem: The persistent challenges can significantly affect a child’s self-esteem, leading to negative self-perception and reduced motivation.
Physical Education: Difficulties in P.E. can lead to exclusion and feelings of inadequacy, impacting overall social and emotional wellbeing.
Addressing these academic challenges requires a multi-faceted approach, including occupational therapy, assistive technologies (like ergonomic writing tools), and tailored classroom support and adaptations.
Q 26. What are the ethical considerations in treating a child with DCD?
Ethical considerations in DCD treatment are paramount. The focus is always on the child’s well-being and their rights.
Informed Consent: Obtaining informed consent from parents or guardians is crucial, ensuring they fully understand the treatment plan and its potential risks and benefits.
Confidentiality: Maintaining confidentiality about the child’s diagnosis and treatment is essential, protecting their privacy.
Beneficence and Non-maleficence: The treatment should always aim to benefit the child and avoid harm. This means carefully selecting interventions and monitoring for any adverse effects.
Justice: Ensuring equal access to quality DCD treatment, regardless of the child’s background or socioeconomic status, is vital.
Cultural Sensitivity: Consideration of the child’s cultural background and beliefs is critical in designing a treatment plan that respects their values and family dynamics.
For example, the family’s involvement in therapy is crucial, not just for support but also for respecting their cultural perspectives on child-rearing and rehabilitation.
Q 27. How do you incorporate evidence-based practices into your DCD treatment plans?
Evidence-based practice is at the core of my approach. This means utilizing interventions supported by high-quality research. I carefully review scientific literature to determine effective strategies and adapt them to each individual child’s specific needs.
Task-Specific Training: This involves breaking down complex motor skills into smaller, manageable components and providing repetitive practice. Research shows this is effective for improving specific motor skills.
Motor Learning Principles: I incorporate principles of motor learning, such as providing clear instructions, feedback, and opportunities for practice and feedback in a structured manner. This is crucial for efficient skill acquisition.
Neuroplasticity: I leverage the brain’s capacity for change by emphasizing repetition and practice to promote neural rewiring and improve motor control. This reinforces the idea that practice enhances skill and modifies the brain’s neural connections.
Adaptive Equipment: Where appropriate, I suggest assistive devices like ergonomic writing tools or adaptive sports equipment to assist with task completion. This makes the process easier and more efficient.
Regular Monitoring and Evaluation: I regularly monitor the child’s progress using standardized assessments and adjust the treatment plan as needed, ensuring the approach remains relevant and effective.
A systematic approach to tracking progress, using standardized assessments paired with qualitative observations, is pivotal to ensure the effectiveness of the chosen intervention and allows for necessary adaptations based on ongoing assessment.
Q 28. Describe your approach to working with children with severe DCD.
Children with severe DCD require a highly individualized and intensive approach. The key is breaking down tasks into their smallest components and providing extensive, adapted support.
Intensive Therapy: Frequent and longer therapy sessions might be necessary, focusing on foundational skills. This often necessitates a collaborative approach with other professionals, such as occupational therapists.
Adaptive Strategies and Assistive Technologies: Utilizing adaptive equipment and assistive technologies is crucial to facilitate participation in everyday activities. This could involve specialized writing tools or communication apps.
Environmental Modifications: Adapting the child’s environment to reduce demands on their motor skills is important. This might involve adjusting classroom furniture or using assistive technology in the home.
Functional Goals: Focus is shifted towards achieving functional goals that enhance the child’s independence and quality of life. This could include improving self-care skills or participation in school and social activities.
Family Support: Extensive family support and education are essential. This helps the family adapt to the child’s needs and collaborate in supporting therapeutic progress beyond therapy sessions.
For example, a child struggling with severe DCD might benefit from using a specialized computer keyboard and adaptive software to participate in writing tasks. It’s about understanding and meeting the child’s unique challenges at every step.
Key Topics to Learn for Developmental Coordination Disorder Treatment Interview
- Developmental Diagnosis & Assessment: Understanding the diagnostic criteria for DCD, different assessment tools (e.g., Movement ABC, Bruininks-Oseretsky Test of Motor Proficiency), and interpreting assessment results to inform treatment planning.
- Theoretical Frameworks: Familiarity with relevant theoretical models explaining DCD, such as the dynamic systems theory and its implications for intervention strategies. Understanding the role of sensory processing and motor learning in DCD.
- Intervention Strategies: Knowledge of various therapeutic approaches, including occupational therapy, physiotherapy, and adapted physical activity programs. Understanding the principles of task-specific training, repetition, and feedback in intervention.
- Practical Application: Designing and implementing individualized treatment plans based on assessment findings. Adapting interventions to meet the specific needs and goals of diverse clients with DCD. Experience with modifying activities and environments to promote successful participation.
- Collaboration & Communication: Understanding the importance of collaboration with parents, educators, and other professionals. Effective communication strategies for explaining DCD and its treatment to families and other stakeholders.
- Evidence-Based Practice: Ability to critically evaluate research related to DCD interventions and apply evidence-based practices in clinical settings. Understanding the importance of outcome measurement and monitoring progress.
- Adaptive Strategies & Assistive Technology: Knowledge of adaptive strategies and assistive technologies that can support individuals with DCD in various settings (school, home, community).
- Addressing Co-occurring Conditions: Understanding the prevalence of co-occurring conditions (e.g., ADHD, learning disabilities) and how to address these in treatment planning.
Next Steps
Mastering Developmental Coordination Disorder treatment is crucial for a rewarding and impactful career in pediatric therapy or related fields. A strong understanding of DCD’s complexities and effective intervention strategies significantly enhances your value to potential employers. To maximize your job prospects, creating an ATS-friendly resume is essential. ResumeGemini is a trusted resource that can help you build a compelling resume highlighting your skills and experience in Developmental Coordination Disorder treatment. Examples of resumes tailored to this specialization are available to guide you. Invest time in crafting a professional and effective resume – it’s your first impression on potential employers.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.